 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: orthognathic surgery, long term antibiotic prophylaxis, short term antibiotic prophylaxis, Epistemonikos, GRADE.
INTRODUCTION
Orthognathic surgery, being an invasive surgical procedure, may present significant postoperative morbidities for the patient. Among the most frequently described complications is surgical site infection. The administration of prophylactic antibiotics prior to this type of procedure is a common practice, however, the cost-benefit of the use of antibiotics, the type of antibiotics, the route of administration, the dosage, and the regimen to be used have not been clearly defined and are still considered a controversial issue. In this summary of evidence, we will compare long-term antibiotic prophylaxis with short-term prophylaxis.
METHODS
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified five systematic reviews including nine studies overall, of which all nine were randomized trials. We conclude that administering a long-term prophylactic antibiotic regimen probably decreases the risk of surgical site infection and that it may increase the risk of hospital stay longer than two days, nevertheless, regarding this last point, the certainty of the evidence is low.
Orthognathic surgery corresponds to a set of surgical techniques that allow the correction of the anomalies of the maxillofacial complex through the realignment of the maxillary and mandibular bones; allowing the improvement of the functionality, facial harmony, and aesthetics. Some of the postoperative complications include hemorrhage, temporary or permanent neurological alterations and infections. In relation to this last complication, the use of antibiotic prophylaxis is frequent, and is defined as the use of antibiotics to prevent infection at the surgical site [1]. However, there is no clear consensus regarding the type of antibiotic, dose, route of administration or regimen to use.
Additionally, prophylactic antibiotic schedules can be classified according to the time of administration:
In this summary of evidence, the long-term and short-term prophylactic antibiotic regimen will be comparatively evaluated, with the intention of clarifying which of these would be more effective in reducing postoperative complications.
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We identified five systematic reviews [1], [2], [3], [4], [5] including nine studies overall [6], [7], [8], [9], [10], [11], [12], [13], [14], of which all were randomized trials. |
|
What types of patients were included* |
All trials included patients that underwent orthognathic surgery, without distinction in the subtype of surgery. The trials included men and women with ages ranging from 15 to 48 years [6], [7], [8], [9], [10], [11], [12], [13], [14]. |
|
What types of interventions were included* |
All trials evaluated long antibiotic prophylaxis regimens compared with short prophylaxis regimens. Long-term prophylactic regimens considered administration of antibiotics before the operation, on the day of the surgery, and for several additional postoperative days: two days [7], [13],12 three days 12], five days [6], [11], seven days [10], [14]. This information was not reported in two trials [8], [9]. Short-term prophylactic antibiotic regimens considered preoperative and during the same day (up to 24 hrs.) antibiotic administration [6], [7], [8], [9], [10], [11], [12], [13], [14]. Three trials used placebo within the regimen [6], [7], [13]. The antibiotics used by each trial were:
The routes of drug administration used were Two trials did not report the regimen, antibiotic or route of administration used [8], [9]. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
|
* Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
The information on the effects of antibiotic prophylaxis in a long-term regimen is based on nine randomized trials [6], [7], [8], [9], [10], [11], [12], [13], [14], involving 472 patients.Nine trials measured the outcome surgical site infection [6], [7], [8], [9], [10], [11], [12], [13], [14] (472 patients) and only one trial measured the outcome hospital stay longer than two days (171 patients) [8].
The summary of findings is as follows:
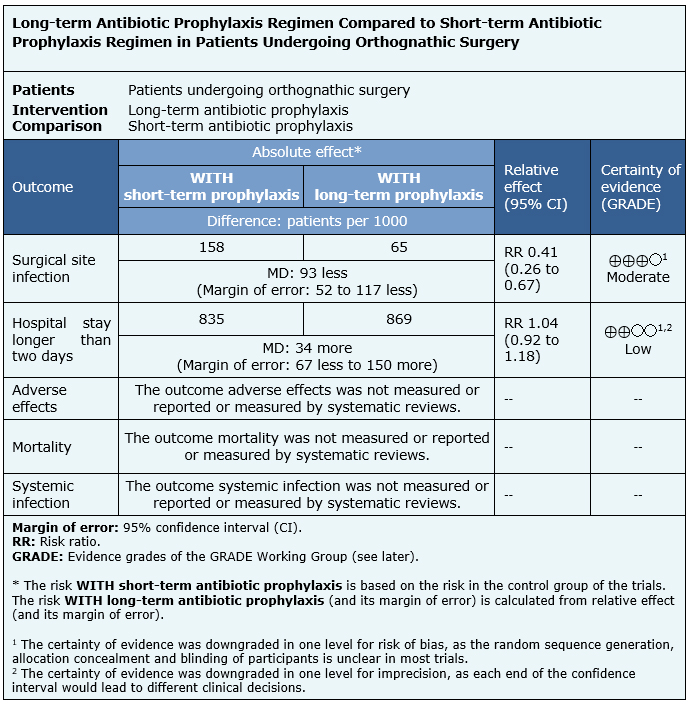
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
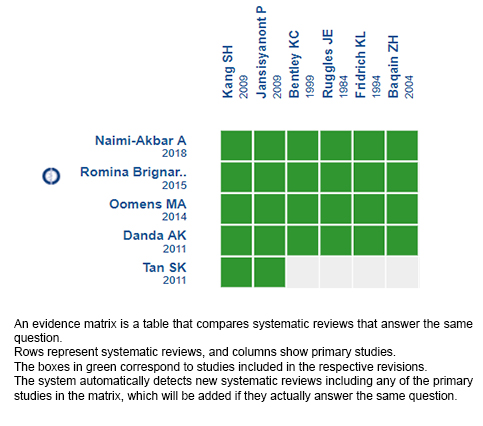
Follow the link to access the interactive version: Long-term antibiotic prophylaxis regimen compared to short-term antibiotic prophylaxis regimen in patients undergoing orthognathic surgery.
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Orthognathic surgery, being an invasive surgical procedure, may present significant postoperative morbidities for the patient. Among the most frequently described complications is surgical site infection. The administration of prophylactic antibiotics prior to this type of procedure is a common practice, however, the cost-benefit of the use of antibiotics, the type of antibiotics, the route of administration, the dosage, and the regimen to be used have not been clearly defined and are still considered a controversial issue. In this summary of evidence, we will compare long-term antibiotic prophylaxis with short-term prophylaxis.
METHODS
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified five systematic reviews including nine studies overall, of which all nine were randomized trials. We conclude that administering a long-term prophylactic antibiotic regimen probably decreases the risk of surgical site infection and that it may increase the risk of hospital stay longer than two days, nevertheless, regarding this last point, the certainty of the evidence is low.
 Autores:
Matthias Wallach [1], Javier Cuéllar[1], Francisca Verdugo-Paiva[2,3], Ana Alarcón[1,4]
Autores:
Matthias Wallach [1], Javier Cuéllar[1], Francisca Verdugo-Paiva[2,3], Ana Alarcón[1,4]

Citación: Wallach M, Cuéllar J, Verdugo-Paiva F, Alarcón A. Long-term antibiotic prophylaxis regimen compared to short-term antibiotic prophylaxis regimen in patients undergoing orthognathic surgery. Medwave 2020;20(11):e8071 doi: 10.5867/medwave.2020.11.8071
Fecha de envío: 11/6/2020
Fecha de aceptación: 3/8/2020
Fecha de publicación: 11/12/2020
Origen: Este artículo es producto del Epistemonikos Evidence Synthesis Project de la Fundación Epistemonikos, en colaboración con Medwave para su publicación.
Tipo de revisión: Con revisión por pares sin ciego por parte del equipo metodológico del Centro Evidencia UC en colaboración con Epistemonikos Evidence Synthesis Project.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Brignardello‐Petersen, R., Carrasco‐Labra, A., Araya, I., Yanine, N., Jara, L. C., & Villanueva, J. Antibiotic prophylaxis for preventing infectious complications in orthognathic surgery. Cochrane Database of systematic reviews; (2015), (1).
Brignardello‐Petersen, R., Carrasco‐Labra, A., Araya, I., Yanine, N., Jara, L. C., & Villanueva, J. Antibiotic prophylaxis for preventing infectious complications in orthognathic surgery. Cochrane Database of systematic reviews; (2015), (1).  Danda, A. K., & Ravi, P. Effectiveness of postoperative antibiotics in orthognathic surgery: a meta-analysis. Journal of Oral and Maxillofacial Surgery; (2011) , 69(10), 2650-2656.
Danda, A. K., & Ravi, P. Effectiveness of postoperative antibiotics in orthognathic surgery: a meta-analysis. Journal of Oral and Maxillofacial Surgery; (2011) , 69(10), 2650-2656.  Naimi-Akbar, A., Hultin, M., Klinge, A., Klinge, B., Tranaeus, S., & Lund, B. Antibiotic prophylaxis in orthognathic surgery: A complex systematic review. PloS one; (2018), 13(1), e0191161.
Naimi-Akbar, A., Hultin, M., Klinge, A., Klinge, B., Tranaeus, S., & Lund, B. Antibiotic prophylaxis in orthognathic surgery: A complex systematic review. PloS one; (2018), 13(1), e0191161.  Oomens, M. A. E. M., Verlinden, C. R. A., Goey, Y., & Forouzanfar, T. Prescribing antibiotic prophylaxis in orthognathic surgery: a systematic review. International journal of oral and maxillofacial surgery; (2014), 43(6), 725-731.
Oomens, M. A. E. M., Verlinden, C. R. A., Goey, Y., & Forouzanfar, T. Prescribing antibiotic prophylaxis in orthognathic surgery: a systematic review. International journal of oral and maxillofacial surgery; (2014), 43(6), 725-731.  Tan, S. K., Lo, J., & Zwahlen, R. A. Perioperative antibiotic prophylaxis in orthognathic surgery: a systematic review and meta-analysis of clinical trials. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology; (2011), 112(1), 19-27.
Tan, S. K., Lo, J., & Zwahlen, R. A. Perioperative antibiotic prophylaxis in orthognathic surgery: a systematic review and meta-analysis of clinical trials. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology; (2011), 112(1), 19-27.  Baqain, Z. H., Hyde, N., Patrikidou, A., & Harris, M. Antibiotic prophylaxis for orthognathic surgery: a prospective, randomised clinical trial. British Journal of Oral and Maxillofacial Surgery; (2004), 42(6), 506-510.
Baqain, Z. H., Hyde, N., Patrikidou, A., & Harris, M. Antibiotic prophylaxis for orthognathic surgery: a prospective, randomised clinical trial. British Journal of Oral and Maxillofacial Surgery; (2004), 42(6), 506-510.  Bentley, K. C., Head, T. W., & Aiello, G. A. Antibiotic prophylaxis in orthognathic surgery: a 1-day versus 5-day regimen. Journal of oral and maxillofacial surgery; (1999), 57(3), 226-230.
Bentley, K. C., Head, T. W., & Aiello, G. A. Antibiotic prophylaxis in orthognathic surgery: a 1-day versus 5-day regimen. Journal of oral and maxillofacial surgery; (1999), 57(3), 226-230.  Davis, C. M., Gregoire, C. E., Davis, I., & Steeves, T. W. Prevalence of surgical site infections following orthognathic surgery: a double-blind, randomized controlled trial on a 3-day versus 1-day postoperative antibiotic regimen. Journal of Oral and Maxillofacial Surgery; (2017), 75(4), 796-804.
Davis, C. M., Gregoire, C. E., Davis, I., & Steeves, T. W. Prevalence of surgical site infections following orthognathic surgery: a double-blind, randomized controlled trial on a 3-day versus 1-day postoperative antibiotic regimen. Journal of Oral and Maxillofacial Surgery; (2017), 75(4), 796-804.  Eshghpour, M., Khajavi, A., Bagheri, M., & Banihashemi, E. Value of prophylactic postoperative antibiotic therapy after bimaxillary orthognathic surgery: a clinical trial. Iranian journal of otorhinolaryngology; (2014), 26(77), 207.
Eshghpour, M., Khajavi, A., Bagheri, M., & Banihashemi, E. Value of prophylactic postoperative antibiotic therapy after bimaxillary orthognathic surgery: a clinical trial. Iranian journal of otorhinolaryngology; (2014), 26(77), 207.  Fridrich, K. L., Partnoy, B. E., & Zeitler, D. L. Prospective analysis of antibiotic prophylaxis for orthognathic surgery. The International journal of adult orthodontics and orthognathic surgery; (1994), 9(2), 129-131.
Fridrich, K. L., Partnoy, B. E., & Zeitler, D. L. Prospective analysis of antibiotic prophylaxis for orthognathic surgery. The International journal of adult orthodontics and orthognathic surgery; (1994), 9(2), 129-131.  Jansisyanont, P., Sessirisombat, S., Sastravaha, P., & Bamroong, P. Antibiotic prophylaxis for orthognathic surgery: a prospective, comparative, randomized study between amoxicillin-clavulanic acid and penicillin. Journal of the Medical Association of Thailand; (2011), 91(11), 1726.
Jansisyanont, P., Sessirisombat, S., Sastravaha, P., & Bamroong, P. Antibiotic prophylaxis for orthognathic surgery: a prospective, comparative, randomized study between amoxicillin-clavulanic acid and penicillin. Journal of the Medical Association of Thailand; (2011), 91(11), 1726.  Kang, S. H., Yoo, J. H., & Yi, C. K. The efficacy of postoperative prophylactic antibiotics in orthognathic surgery: a prospective study in Le Fort I osteotomy and bilateral intraoral vertical ramus osteotomy. Yonsei medical journal; (2009), 50(1), 55-59.
Kang, S. H., Yoo, J. H., & Yi, C. K. The efficacy of postoperative prophylactic antibiotics in orthognathic surgery: a prospective study in Le Fort I osteotomy and bilateral intraoral vertical ramus osteotomy. Yonsei medical journal; (2009), 50(1), 55-59.  Ruggles, J. E., & Hann, J. R. Antibiotic prophylaxis in intraoral orthognathic surgery. Journal of Oral and Maxillofacial Surgery; (1984), 42(12), 797-801.
Ruggles, J. E., & Hann, J. R. Antibiotic prophylaxis in intraoral orthognathic surgery. Journal of Oral and Maxillofacial Surgery; (1984), 42(12), 797-801.  Samman N, Cheung LK. Antibiotic prophylaxis for orthognathic surgery: a prospective trial of four penicillin regimes. Journal of cranio-maxillo-facial surgery. 1996;24(Suppl 1).
Samman N, Cheung LK. Antibiotic prophylaxis for orthognathic surgery: a prospective trial of four penicillin regimes. Journal of cranio-maxillo-facial surgery. 1996;24(Suppl 1).  American Association of Oral and Maxillofacial Surgeons (AAOMS). Parameters of care: Clinical Practice Guidelines for Oral and Maxillofacial Surgery. Surgical Correction of Skeletal Deformities. 2017.
American Association of Oral and Maxillofacial Surgeons (AAOMS). Parameters of care: Clinical Practice Guidelines for Oral and Maxillofacial Surgery. Surgical Correction of Skeletal Deformities. 2017.  British Association of Oral and Maxillofacial Surgeons (BAOMS). Commissioning Guide: Orthognathic Procedures. 2013.
British Association of Oral and Maxillofacial Surgeons (BAOMS). Commissioning Guide: Orthognathic Procedures. 2013.