 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
INTRODUCTION
Lidocaine is widely used in anesthesia due to its multiple properties, including its role as analgesic. However, it is not entirely clear which are the real benefits of its use in the perioperative setting.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified 15 systematic reviews including 53 studies overall, all of them randomized controlled trials. We concluded the use of intravenous perioperative lidocaine probably results in a clinically irrelevant difference in pain and length of hospital stay, but it probably prevents postoperative nausea and vomiting.
There are different alternatives used as adjuvants in the various anesthetics techniques, with the objective of diminishing postoperative symptoms and accelerating recovery. It has been proposed that lidocaine, a local anesthetic belonging to the group of the aminoamides which acts by inhibiting sodium channels, would have analgesics effects, among others, that would make it a good alternative in the surgical setting. Nevertheless, it is not yet clear whether its effects bring a real benefit for patients, and also if it is a safe intervention.
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We identified 15 systematic reviews [1],[2],[3],[4],[5],[6],[7],[8],[9], One of the reviews [10] presented data from one trial that was not included in any other review (Harvey 2006), in a way in which it was not possible to reanalyze it. The reference to this trial is not included in the review, it was not possible to identify it by other means and the author did not reply after to our contact. |
|
What types of patients were included* |
Twenty five trials included adults from 18 to 75 years old [16],[17], Seven trials only included women [18],[21],[42],[44],[49],[50],[52], three included only men [26],[53],[60], the remaining 43 trials did not restrict by sex. Fourteen trials included ASA I-II patients [16],[18],[19],[28],[34],[36],[41], In 24 trials the patients underwent abdominal surgery; of these, 13 only included digestive surgery [17],[22],[24],[27],[28],[39],[41], Twenty-two trials excluded patients with chronic pain conditions, chronic pain treatments or pain treatment in the last week with any analgesic drug [19],[21],[22],[24],[25],[28],[34],[35],[39],[41],[42], |
|
What types of interventions were included* |
All of the trials used intravenous systemic lidocaine. Forty seven trials started lidocaine intraoperatively; of these, forty six initiated it before skin incision [16],[17],[18],[19],[20],[21],[22], Forty two trials used a lidocaine bolus (1 mg/kg to 3 mg/kg) followed by an infusion (20 μg/kg/min to 4 mg/min); from these, 17 maintained the infusion only during the intraoperative period [18], Four trials started lidocaine postoperatively; one as a bolus (1.5 mg/kg) and then continued with an infusion (2 mg/kg/h) for two hours [43]; of the remaining three, one used lidocaine infusion (60 mg/h) for 24 hours [54] and two a PCA without referring an end time [45],[46]. One trial started lidocaine preoperatively [58] with a bolus (1.5 mg/kg) followed by an infusion (2 mg/kg/h) only during the intraoperative period. It was not possible to extract data related to the characteristics from one trial [70] because it was included in only one systematic review [15], and the author did not reply after attempting to contact him. One trial was included in a systematic review with preliminary data before being published [35]. All of the trials compared lidocaine against placebo or no treatment. |
|
What types of outcomes |
The outcome were grouped by the systematics reviews as follows: Postoperative pain, intraoperative and postoperative analgesic consumption, chronic pain, opioid related adverse effects, postoperative nausea and vomiting, postoperative ileus and functional gastrointestinal recovery (evaluated by time to first flatus, feces, or bowel movement), length of hospital stay and length of post-anesthesia care unit stay, surgical complications, adverse events, mortality, cognitive outcomes, patient satisfaction, cessation of the intervention, systemic lidocaine toxicity, plasma levels of cytokines. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
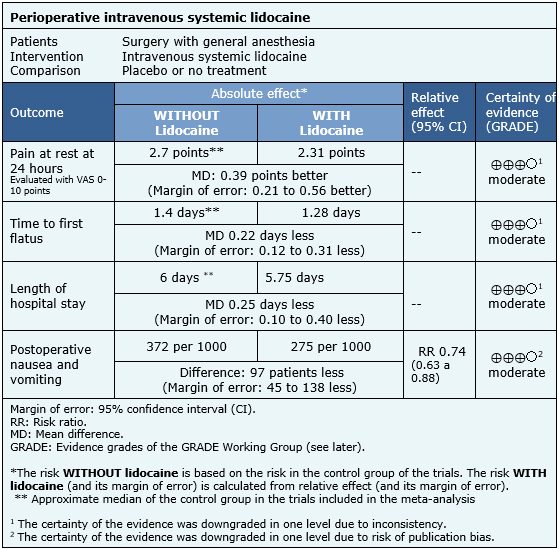
The information about the effects of the intravenous systemic lidocaine is based on 37 randomized trials including 2253 patients [16],[17],[18],[20],[21],[22],[23],[24],[25],[27],[28],[31],[32],[33],[35],[39],[40],[41],[42],[44],[48],[49],[51],[52],[53],[54],[57],[58],[59],[60],[61],[62],[63],[65],[66],[68],[69]. Twenty five trials reported the outcome pain at rest at 24 hours [16],[17],[18],[20],[22],[24],[25],[27],[28],[31],[35],[39],[41],[42],[44],[52],[53],[57],[58],[59],[60],[61],[65],[68],[69], 16 reported time to first flatus [18],[22],[24],[25],[28],[41],[51],[53],[54],[57],[59],[60],[63],[65],[68],[69], 24 measured length of hospital stay [18],[20],[22],[23],[24],[25],[27],[28],[32],[33],[39],[40],[41],48],[51],[53],[54],[57],[58],[59],[60],[61],[62],[69] and 24 reported postoperative nausea and vomiting [16],[17],[18],[20],[21],[24],[25],[27],[28],[31],[35],[39],[41],[44],[49],[57],[58],[59],[60],[63],[65],[66],[68],[69].
The summary of findings is the following:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
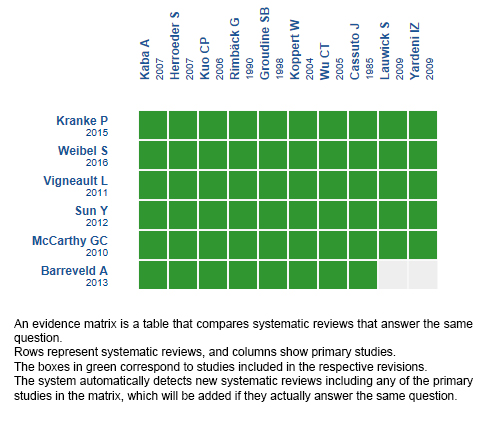
Follow the link to access the interactive version: Intravenous lidocaine versus placebo or no treatment on perioperative analgesia
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Lidocaine is widely used in anesthesia due to its multiple properties, including its role as analgesic. However, it is not entirely clear which are the real benefits of its use in the perioperative setting.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified 15 systematic reviews including 53 studies overall, all of them randomized controlled trials. We concluded the use of intravenous perioperative lidocaine probably results in a clinically irrelevant difference in pain and length of hospital stay, but it probably prevents postoperative nausea and vomiting.
 Autores:
María Magdalena González[1,2], Fernando Altermatt[2,3]
Autores:
María Magdalena González[1,2], Fernando Altermatt[2,3]

Citación: González M, Altermatt F. Is intravenous lidocaine effective for decreasing pain and speeding up recovery after surgery?. Medwave 2017 Nov-Dic;17(9):e7121 doi: 10.5867/medwave.2017.09.7121
Fecha de envío: 29/11/2017
Fecha de aceptación: 26/12/2017
Fecha de publicación: 29/12/2017
Origen: Este artículo es producto del Epistemonikos Evidence Synthesis Project de la Fundación Epistemonikos, en colaboración con Medwave para su publicación.
Tipo de revisión: Con revisión por pares sin ciego por parte del equipo metodológico del Epistemonikos Evidence Synthesis Project.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Weibel S, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart
LH, Poepping DM, Afshari A, Kranke P. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016 Jun;116(6):770-83.
| CrossRef | PubMed |
Weibel S, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart
LH, Poepping DM, Afshari A, Kranke P. Efficacy and safety of intravenous lidocaine for postoperative analgesia and recovery after surgery: a systematic review with trial sequential analysis. Br J Anaesth. 2016 Jun;116(6):770-83.
| CrossRef | PubMed | Wallström A, Frisman GH. Facilitating early recovery of bowel motility after colorectal surgery: a systematic review. J Clin Nurs. 2014 Jan;23(1-2):24-44. | CrossRef | PubMed |
Wallström A, Frisman GH. Facilitating early recovery of bowel motility after colorectal surgery: a systematic review. J Clin Nurs. 2014 Jan;23(1-2):24-44. | CrossRef | PubMed | Vigneault L, Turgeon AF, Côté D, Lauzier F, Zarychanski R, Moore L, McIntyre LA, Nicole PC, Fergusson DA. Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anaesth. 2011 Jan;58(1):22-37. | CrossRef | PubMed |
Vigneault L, Turgeon AF, Côté D, Lauzier F, Zarychanski R, Moore L, McIntyre LA, Nicole PC, Fergusson DA. Perioperative intravenous lidocaine infusion for postoperative pain control: a meta-analysis of randomized controlled trials. Can J Anaesth. 2011 Jan;58(1):22-37. | CrossRef | PubMed | Ventham NT, Kennedy ED, Brady RR, Paterson HM, Speake D, Foo I, Fearon KC. Efficacy of Intravenous Lidocaine for Postoperative Analgesia Following Laparoscopic Surgery: A Meta-Analysis. World J Surg. 2015 Sep;39(9):2220-34. | CrossRef | PubMed |
Ventham NT, Kennedy ED, Brady RR, Paterson HM, Speake D, Foo I, Fearon KC. Efficacy of Intravenous Lidocaine for Postoperative Analgesia Following Laparoscopic Surgery: A Meta-Analysis. World J Surg. 2015 Sep;39(9):2220-34. | CrossRef | PubMed | Traut U, Brügger L, Kunz R, Pauli-Magnus C, Haug K, Bucher HC, Koller MT. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD004930. | CrossRef | PubMed |
Traut U, Brügger L, Kunz R, Pauli-Magnus C, Haug K, Bucher HC, Koller MT. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008 Jan 23;(1):CD004930. | CrossRef | PubMed | Sun Y, Li T, Wang N, Yun Y, Gan TJ. Perioperative systemic lidocaine for postoperative analgesia and recovery after abdominal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2012 Nov;55(11):1183-94. Erratum in: Dis Colon Rectum. 2013 Feb;52(2):271. | CrossRef | PubMed |
Sun Y, Li T, Wang N, Yun Y, Gan TJ. Perioperative systemic lidocaine for postoperative analgesia and recovery after abdominal surgery: a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2012 Nov;55(11):1183-94. Erratum in: Dis Colon Rectum. 2013 Feb;52(2):271. | CrossRef | PubMed | McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs. 2010 Jun 18;70(9):1149-63. | CrossRef | PubMed |
McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs. 2010 Jun 18;70(9):1149-63. | CrossRef | PubMed | Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008 Nov;95(11):1331-8. | CrossRef | PubMed |
Marret E, Rolin M, Beaussier M, Bonnet F. Meta-analysis of intravenous lidocaine and postoperative recovery after abdominal surgery. Br J Surg. 2008 Nov;95(11):1331-8. | CrossRef | PubMed | Kranke P, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart LH, Poepping DM, Weibel S. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 2015 Jul 16;(7):CD009642. | CrossRef | PubMed |
Kranke P, Jokinen J, Pace NL, Schnabel A, Hollmann MW, Hahnenkamp K, Eberhart LH, Poepping DM, Weibel S. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery. Cochrane Database Syst Rev. 2015 Jul 16;(7):CD009642. | CrossRef | PubMed | Khan JS, Yousuf M, Victor JC, Sharma A, Siddiqui N. An estimation for an appropriate end time for an intraoperative intravenous lidocaine infusion in bowel surgery: a comparative meta-analysis. J Clin Anesth. 2016 Feb;28:95-104. | CrossRef | PubMed |
Khan JS, Yousuf M, Victor JC, Sharma A, Siddiqui N. An estimation for an appropriate end time for an intraoperative intravenous lidocaine infusion in bowel surgery: a comparative meta-analysis. J Clin Anesth. 2016 Feb;28:95-104. | CrossRef | PubMed | Joshi GP, Bonnet F, Kehlet H; PROSPECT collaboration. Evidence-based postoperative pain management after laparoscopic colorectal surgery. Colorectal Dis. 2013 Feb;15(2):146-55. | CrossRef | PubMed |
Joshi GP, Bonnet F, Kehlet H; PROSPECT collaboration. Evidence-based postoperative pain management after laparoscopic colorectal surgery. Colorectal Dis. 2013 Feb;15(2):146-55. | CrossRef | PubMed | Gholipour Baradari A, Habibi MR, Habibi V, Nouraei SM. Administration of lidocaine to prevent cognitive deficit in patients undergoing coronary artery bypass grafting and valve plasty: a systematic review and meta-analysis. Expert Rev Clin Pharmacol. 2017 Feb;10(2):179-185. | CrossRef | PubMed |
Gholipour Baradari A, Habibi MR, Habibi V, Nouraei SM. Administration of lidocaine to prevent cognitive deficit in patients undergoing coronary artery bypass grafting and valve plasty: a systematic review and meta-analysis. Expert Rev Clin Pharmacol. 2017 Feb;10(2):179-185. | CrossRef | PubMed | Chang YC, Liu CL, Liu TP, Yang PS, Chen MJ, Cheng SP. Effect of Perioperative Intravenous Lidocaine Infusion on Acute and Chronic Pain after Breast Surgery: A Meta-Analysis of Randomized Controlled Trials. Pain Pract. 2017 Mar;17(3):336-343. | CrossRef | PubMed |
Chang YC, Liu CL, Liu TP, Yang PS, Chen MJ, Cheng SP. Effect of Perioperative Intravenous Lidocaine Infusion on Acute and Chronic Pain after Breast Surgery: A Meta-Analysis of Randomized Controlled Trials. Pain Pract. 2017 Mar;17(3):336-343. | CrossRef | PubMed | Barreveld A, Witte J, Chahal H, Durieux ME, Strichartz G. Preventive analgesia by local anesthetics: the reduction of postoperative pain by peripheral nerve blocks and intravenous drugs. Anesth Analg. 2013 May;116(5):1141-61. | CrossRef | PubMed | PMC |
Barreveld A, Witte J, Chahal H, Durieux ME, Strichartz G. Preventive analgesia by local anesthetics: the reduction of postoperative pain by peripheral nerve blocks and intravenous drugs. Anesth Analg. 2013 May;116(5):1141-61. | CrossRef | PubMed | PMC | Dong M, Tian B, Gao S, Yang D, Ren X. A systemic review of the preventative effect of peri-operative intervention to the post mastectomy pain syndrome. Journal of Modern Oncology. 2016;2:248-253. | CrossRef |
Dong M, Tian B, Gao S, Yang D, Ren X. A systemic review of the preventative effect of peri-operative intervention to the post mastectomy pain syndrome. Journal of Modern Oncology. 2016;2:248-253. | CrossRef | Baral BK, Bhattarai BK, Rahman TR, Singh SN, Regmi R. Perioperative intravenous lidocaine infusion on postoperative pain relief in patients undergoing upper abdominal surgery. Nepal Med Coll J. 2010 Dec;12(4):215-20. | PubMed |
Baral BK, Bhattarai BK, Rahman TR, Singh SN, Regmi R. Perioperative intravenous lidocaine infusion on postoperative pain relief in patients undergoing upper abdominal surgery. Nepal Med Coll J. 2010 Dec;12(4):215-20. | PubMed | Cassuto J, Wallin G, Högström S, Faxén A, Rimbäck G. Inhibition of postoperative pain by continuous low-dose intravenous infusion of lidocaine. Anesth Analg. 1985 Oct;64(10):971-4. | PubMed |
Cassuto J, Wallin G, Högström S, Faxén A, Rimbäck G. Inhibition of postoperative pain by continuous low-dose intravenous infusion of lidocaine. Anesth Analg. 1985 Oct;64(10):971-4. | PubMed | Choi SJ, Kim MH, Jeong HY, Lee JJ. Effect of intraoperative lidocaine on anesthetic consumption, and bowel function, pain intensity, analgesic consumption and hospital stay after breast surgery. Korean J Anesthesiol. 2012 May;62(5):429-34. | CrossRef | PubMed | PMC |
Choi SJ, Kim MH, Jeong HY, Lee JJ. Effect of intraoperative lidocaine on anesthetic consumption, and bowel function, pain intensity, analgesic consumption and hospital stay after breast surgery. Korean J Anesthesiol. 2012 May;62(5):429-34. | CrossRef | PubMed | PMC | Cui W, Li Y, Li S, Wang R, Li J. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil-based anaesthesia. Eur J Anaesthesiol. 2010 Jan;27(1):41-6. | CrossRef | PubMed |
Cui W, Li Y, Li S, Wang R, Li J. Systemic administration of lidocaine reduces morphine requirements and postoperative pain of patients undergoing thoracic surgery after propofol-remifentanil-based anaesthesia. Eur J Anaesthesiol. 2010 Jan;27(1):41-6. | CrossRef | PubMed | Farag E, Ghobrial M, Sessler DI, Dalton JE, Liu J, Lee JH, Zaky S, Benzel E, Bingaman W, Kurz A. Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology. 2013 Oct;119(4):932-40. | CrossRef | PubMed |
Farag E, Ghobrial M, Sessler DI, Dalton JE, Liu J, Lee JH, Zaky S, Benzel E, Bingaman W, Kurz A. Effect of perioperative intravenous lidocaine administration on pain, opioid consumption, and quality of life after complex spine surgery. Anesthesiology. 2013 Oct;119(4):932-40. | CrossRef | PubMed | Grady MV, Mascha E, Sessler DI, Kurz A. The effect of perioperative intravenous lidocaine and ketamine on recovery after abdominal hysterectomy. Anesth Analg. 2012 Nov;115(5):1078-84. | CrossRef | PubMed |
Grady MV, Mascha E, Sessler DI, Kurz A. The effect of perioperative intravenous lidocaine and ketamine on recovery after abdominal hysterectomy. Anesth Analg. 2012 Nov;115(5):1078-84. | CrossRef | PubMed | Herroeder S, Pecher S, Schönherr ME, Kaulitz G, Hahnenkamp K, Friess H, Böttiger BW, Bauer H, Dijkgraaf MG, Durieux ME, Hollmann MW. Systemic lidocaine shortens length of hospital stay after colorectal surgery: a double-blinded, randomized, placebo-controlled trial. Ann Surg. 2007 Aug;246(2):192-200. Erratum in: Ann Surg. 2009 Apr;249(4):701. Dijkgraaf, Omarcel G W [corrected to Dijkgraaf, Marcel G W]. | PubMed | PMC |
Herroeder S, Pecher S, Schönherr ME, Kaulitz G, Hahnenkamp K, Friess H, Böttiger BW, Bauer H, Dijkgraaf MG, Durieux ME, Hollmann MW. Systemic lidocaine shortens length of hospital stay after colorectal surgery: a double-blinded, randomized, placebo-controlled trial. Ann Surg. 2007 Aug;246(2):192-200. Erratum in: Ann Surg. 2009 Apr;249(4):701. Dijkgraaf, Omarcel G W [corrected to Dijkgraaf, Marcel G W]. | PubMed | PMC | Insler SR, O'Connor M, Samonte AF, Bazaral MG. Lidocaine and the inhibition of postoperative pain in coronary artery bypass patients. J Cardiothorac Vasc Anesth. 1995 Oct;9(5):541-6. | PubMed |
Insler SR, O'Connor M, Samonte AF, Bazaral MG. Lidocaine and the inhibition of postoperative pain in coronary artery bypass patients. J Cardiothorac Vasc Anesth. 1995 Oct;9(5):541-6. | PubMed | Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Joris JL. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology. 2007 Jan;106(1):11-8; discussion 5-6. | PubMed |
Kaba A, Laurent SR, Detroz BJ, Sessler DI, Durieux ME, Lamy ML, Joris JL. Intravenous lidocaine infusion facilitates acute rehabilitation after laparoscopic colectomy. Anesthesiology. 2007 Jan;106(1):11-8; discussion 5-6. | PubMed | Kang H, Kim BG. Intravenous lidocaine for effective pain relief after inguinal herniorrhaphy: a prospective, randomized, double-blind, placebo-controlled study. J Int Med Res. 2011;39(2):435-45. | PubMed |
Kang H, Kim BG. Intravenous lidocaine for effective pain relief after inguinal herniorrhaphy: a prospective, randomized, double-blind, placebo-controlled study. J Int Med Res. 2011;39(2):435-45. | PubMed | Kasten GW, Owens E. Evaluation of lidocaine as an adjunct to fentanyl anesthesia for coronary artery bypass graft surgery. Anesth Analg. 1986 May;65(5):511-5. | PubMed |
Kasten GW, Owens E. Evaluation of lidocaine as an adjunct to fentanyl anesthesia for coronary artery bypass graft surgery. Anesth Analg. 1986 May;65(5):511-5. | PubMed | Kim TH, Kang H, Hong JH, Park JS, Baek CW, Kim JY, Jung YH, Kim HK. Intraperitoneal and intravenous lidocaine for effective pain relief after laparoscopic appendectomy: a prospective, randomized, double-blind, placebo-controlled study. Surg Endosc. 2011 Oct;25(10):3183-90. | CrossRef |
Kim TH, Kang H, Hong JH, Park JS, Baek CW, Kim JY, Jung YH, Kim HK. Intraperitoneal and intravenous lidocaine for effective pain relief after laparoscopic appendectomy: a prospective, randomized, double-blind, placebo-controlled study. Surg Endosc. 2011 Oct;25(10):3183-90. | CrossRef | Kuo CP, Jao SW, Chen KM, Wong CS, Yeh CC, Sheen MJ, Wu CT. Comparison of the effects of thoracic epidural analgesia and i.v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006 Nov;97(5):640-6. | PubMed |
Kuo CP, Jao SW, Chen KM, Wong CS, Yeh CC, Sheen MJ, Wu CT. Comparison of the effects of thoracic epidural analgesia and i.v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006 Nov;97(5):640-6. | PubMed | Lee EH, Lee HM, Chung CH, Chin JH, Choi DK, Chung HJ, Sim JY, Choi IC. Impact of intravenous lidocaine on myocardial injury after off-pump coronary artery surgery. Br J Anaesth. 2011 Apr;106(4):487-93. | CrossRef | PubMed |
Lee EH, Lee HM, Chung CH, Chin JH, Choi DK, Chung HJ, Sim JY, Choi IC. Impact of intravenous lidocaine on myocardial injury after off-pump coronary artery surgery. Br J Anaesth. 2011 Apr;106(4):487-93. | CrossRef | PubMed | Kim WJ , Lee EH , Sim JY , Choi IC. Impact of intravenous lidocaine on myocardial injury during off pump coronary artery surgery. Journal of Cardiothoracic and Vascular Anesthesia. 2010. | Link |
Kim WJ , Lee EH , Sim JY , Choi IC. Impact of intravenous lidocaine on myocardial injury during off pump coronary artery surgery. Journal of Cardiothoracic and Vascular Anesthesia. 2010. | Link | McKay A, Gottschalk A, Ploppa A, Durieux ME, Groves DS. Systemic lidocaine decreased the perioperative opioid analgesic requirements but failed to reduce discharge time after ambulatory surgery. Anesth Analg. 2009 Dec;109(6):1805-8. | CrossRef | PubMed |
McKay A, Gottschalk A, Ploppa A, Durieux ME, Groves DS. Systemic lidocaine decreased the perioperative opioid analgesic requirements but failed to reduce discharge time after ambulatory surgery. Anesth Analg. 2009 Dec;109(6):1805-8. | CrossRef | PubMed | Mitchell SJ, Pellett O, Gorman DF. Cerebral protection by lidocaine during cardiac operations. Ann Thorac Surg. 1999 Apr;67(4):1117-24. | PubMed |
Mitchell SJ, Pellett O, Gorman DF. Cerebral protection by lidocaine during cardiac operations. Ann Thorac Surg. 1999 Apr;67(4):1117-24. | PubMed | Mitchell SJ, Merry AF, Frampton C, Davies E, Grieve D, Mills BP, Webster CS, Milsom FP, Willcox TW, Gorman DF. Cerebral protection by lidocaine during cardiac operations: a follow-up study. Ann Thorac Surg. 2009 Mar;87(3):820-5. | CrossRef | PubMed |
Mitchell SJ, Merry AF, Frampton C, Davies E, Grieve D, Mills BP, Webster CS, Milsom FP, Willcox TW, Gorman DF. Cerebral protection by lidocaine during cardiac operations: a follow-up study. Ann Thorac Surg. 2009 Mar;87(3):820-5. | CrossRef | PubMed | Omar AM. Can systemic lidocaine be used in controlled hypotension? A double-blinded
randomized controlled study in patients undergoing functional endoscopic sinus surgery.
Egyptian Journal of Anaesthesia. 2013 Oct;29(4):295-300. | CrossRef |
Omar AM. Can systemic lidocaine be used in controlled hypotension? A double-blinded
randomized controlled study in patients undergoing functional endoscopic sinus surgery.
Egyptian Journal of Anaesthesia. 2013 Oct;29(4):295-300. | CrossRef | Slovack M, Taylor B, Bryce R, Ong D. Does intravenous lidocaine infusion during video-assisted thoracoscopic surgery reduce postoperative analgesia? A randomized controlled study. Can J Anaesth. 2015 Jun;62(6):676-7. | CrossRef | PubMed |
Slovack M, Taylor B, Bryce R, Ong D. Does intravenous lidocaine infusion during video-assisted thoracoscopic surgery reduce postoperative analgesia? A randomized controlled study. Can J Anaesth. 2015 Jun;62(6):676-7. | CrossRef | PubMed | Soltani HA , Nasr M , Siadat ZD. Effects of Lidocaine on Reducing the Need for Anesthetic Drugs during Ophthalmologic Surgeries. Journal of Isfahan Medical School. 2013 Apr;31(224):41-49. | Link |
Soltani HA , Nasr M , Siadat ZD. Effects of Lidocaine on Reducing the Need for Anesthetic Drugs during Ophthalmologic Surgeries. Journal of Isfahan Medical School. 2013 Apr;31(224):41-49. | Link | Terkawi AS, Durieux ME, Gottschalk A, Brenin D, Tiouririne M. Effect of intravenous lidocaine on postoperative recovery of patients undergoing mastectomy: a double-blind, placebo-controlled randomized trial. Reg Anesth Pain Med. 2014 Nov-Dec;39(6):472-7. | CrossRef | PubMed |
Terkawi AS, Durieux ME, Gottschalk A, Brenin D, Tiouririne M. Effect of intravenous lidocaine on postoperative recovery of patients undergoing mastectomy: a double-blind, placebo-controlled randomized trial. Reg Anesth Pain Med. 2014 Nov-Dec;39(6):472-7. | CrossRef | PubMed | Terkawi AS, Sharma S, Durieux ME, Thammishetti S, Brenin D, Tiouririne M. Perioperative lidocaine infusion reduces the incidence of post-mastectomy chronic pain: a double-blind, placebo-controlled randomized trial. Pain Physician. 2015 Mar-Apr;18(2):E139-46. | PubMed |
Terkawi AS, Sharma S, Durieux ME, Thammishetti S, Brenin D, Tiouririne M. Perioperative lidocaine infusion reduces the incidence of post-mastectomy chronic pain: a double-blind, placebo-controlled randomized trial. Pain Physician. 2015 Mar-Apr;18(2):E139-46. | PubMed | Tikuiis R, Miliauskas P, Samalavičius NE, urauskas A, Samalavičius R,
Zabulis V. Intravenous lidocaine for post-operative pain relief after hand-assisted laparoscopic colon surgery: a randomized, placebo-controlled clinical trial. Tech Coloproctol. 2014 Apr;18(4):373-80. | CrossRef | PubMed | PMC |
Tikuiis R, Miliauskas P, Samalavičius NE, urauskas A, Samalavičius R,
Zabulis V. Intravenous lidocaine for post-operative pain relief after hand-assisted laparoscopic colon surgery: a randomized, placebo-controlled clinical trial. Tech Coloproctol. 2014 Apr;18(4):373-80. | CrossRef | PubMed | PMC | Wang D, Wu X, Li J, Xiao F, Liu X, Meng M. The effect of lidocaine on early postoperative cognitive dysfunction after coronary artery bypass surgery. Anesth Analg. 2002 Nov;95(5):1134-41, table of contents. | PubMed |
Wang D, Wu X, Li J, Xiao F, Liu X, Meng M. The effect of lidocaine on early postoperative cognitive dysfunction after coronary artery bypass surgery. Anesth Analg. 2002 Nov;95(5):1134-41, table of contents. | PubMed | Yang SY, Kang H, Choi GJ, Shin HY, Baek CW, Jung YH, Choi YS. Efficacy of intraperitoneal and intravenous lidocaine on pain relief after laparoscopic cholecystectomy. J Int Med Res. 2014 Apr;42(2):307-19. | CrossRef | PubMed |
Yang SY, Kang H, Choi GJ, Shin HY, Baek CW, Jung YH, Choi YS. Efficacy of intraperitoneal and intravenous lidocaine on pain relief after laparoscopic cholecystectomy. J Int Med Res. 2014 Apr;42(2):307-19. | CrossRef | PubMed | Yardeni IZ, Beilin B, Mayburd E, Levinson Y, Bessler H. The effect of perioperative intravenous lidocaine on postoperative pain and immune function. Anesth Analg. 2009 Nov;109(5):1464-9. | CrossRef | PubMed |
Yardeni IZ, Beilin B, Mayburd E, Levinson Y, Bessler H. The effect of perioperative intravenous lidocaine on postoperative pain and immune function. Anesth Analg. 2009 Nov;109(5):1464-9. | CrossRef | PubMed | Birch K, Jørgensen J, Chraemmer-Jørgensen B, Kehlet H. Effect of i.v. lignocaine on pain and the endocrine metabolic responses after surgery. Br J Anaesth. 1987 Jun;59(6):721-4. | PubMed |
Birch K, Jørgensen J, Chraemmer-Jørgensen B, Kehlet H. Effect of i.v. lignocaine on pain and the endocrine metabolic responses after surgery. Br J Anaesth. 1987 Jun;59(6):721-4. | PubMed | Bryson GL, Charapov I, Krolczyk G, Taljaard M, Reid D. Intravenous lidocaine does not reduce length of hospital stay following abdominal hysterectomy. Can J Anaesth. 2010 Aug;57(8):759-66. | CrossRef | PubMed |
Bryson GL, Charapov I, Krolczyk G, Taljaard M, Reid D. Intravenous lidocaine does not reduce length of hospital stay following abdominal hysterectomy. Can J Anaesth. 2010 Aug;57(8):759-66. | CrossRef | PubMed | Cepeda MS, Delgado M, Ponce M, Cruz CA, Carr DB. Equivalent outcomes during postoperative patient-controlled intravenous analgesia with lidocaine plus morphine versus morphine alone. Anesth Analg. 1996 Jul;83(1):102-6. | PubMed |
Cepeda MS, Delgado M, Ponce M, Cruz CA, Carr DB. Equivalent outcomes during postoperative patient-controlled intravenous analgesia with lidocaine plus morphine versus morphine alone. Anesth Analg. 1996 Jul;83(1):102-6. | PubMed | Chia YY, Tan PH, Wang KY, Liu K. Lignocaine plus morphine in bolus patient-controlled intravenous analgesia lacks post-operative morphine-sparing effect. Eur J Anaesthesiol. 1998 Nov;15(6):664-8. | PubMed |
Chia YY, Tan PH, Wang KY, Liu K. Lignocaine plus morphine in bolus patient-controlled intravenous analgesia lacks post-operative morphine-sparing effect. Eur J Anaesthesiol. 1998 Nov;15(6):664-8. | PubMed | De Kock M, Lavandhomme P, Scholtes JL. Intraoperative and postoperative analgesia using intravenous opioid, clonidine and lignocaine. Anaesth Intensive Care. 1994 Feb;22(1):15-21. | PubMed |
De Kock M, Lavandhomme P, Scholtes JL. Intraoperative and postoperative analgesia using intravenous opioid, clonidine and lignocaine. Anaesth Intensive Care. 1994 Feb;22(1):15-21. | PubMed | De Oliveira GS Jr, Duncan K, Fitzgerald P, Nader A, Gould RW, McCarthy RJ. Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: a randomized double-blinded placebo-controlled trial. Obes Surg. 2014 Feb;24(2):212-8. | CrossRef | PubMed |
De Oliveira GS Jr, Duncan K, Fitzgerald P, Nader A, Gould RW, McCarthy RJ. Systemic lidocaine to improve quality of recovery after laparoscopic bariatric surgery: a randomized double-blinded placebo-controlled trial. Obes Surg. 2014 Feb;24(2):212-8. | CrossRef | PubMed | De Oliveira GS Jr, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg. 2012 Aug;115(2):262-7. | CrossRef | PubMed |
De Oliveira GS Jr, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg. 2012 Aug;115(2):262-7. | CrossRef | PubMed | El-Tahan MR, Warda OM, Diab DG, Ramzy EA, Matter MK. A randomized study of
the effects of perioperative i.v. lidocaine on hemodynamic and hormonal responses
for cesarean section. J Anesth. 2009;23(2):215-21. | CrossRef | PubMed |
El-Tahan MR, Warda OM, Diab DG, Ramzy EA, Matter MK. A randomized study of
the effects of perioperative i.v. lidocaine on hemodynamic and hormonal responses
for cesarean section. J Anesth. 2009;23(2):215-21. | CrossRef | PubMed | Grady P, Clark N, Lenahan J, Oudekerk C, Hawkins R, Nezat G, Pellegrini JE. Effect of intraoperative intravenous lidocaine on postoperative pain and return of bowel function after laparoscopic abdominal gynecologic procedures. AANA J. 2012 Aug;80(4):282-8. | PubMed |
Grady P, Clark N, Lenahan J, Oudekerk C, Hawkins R, Nezat G, Pellegrini JE. Effect of intraoperative intravenous lidocaine on postoperative pain and return of bowel function after laparoscopic abdominal gynecologic procedures. AANA J. 2012 Aug;80(4):282-8. | PubMed | Grigoras A, Lee P, Sattar F, Shorten G. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain. 2012 Sep;28(7):567-72. | CrossRef | PubMed |
Grigoras A, Lee P, Sattar F, Shorten G. Perioperative intravenous lidocaine decreases the incidence of persistent pain after breast surgery. Clin J Pain. 2012 Sep;28(7):567-72. | CrossRef | PubMed | Groudine SB, Fisher HA, Kaufman RP Jr, Patel MK, Wilkins LJ, Mehta SA, Lumb PD. Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg. 1998 Feb;86(2):235-9. | PubMed |
Groudine SB, Fisher HA, Kaufman RP Jr, Patel MK, Wilkins LJ, Mehta SA, Lumb PD. Intravenous lidocaine speeds the return of bowel function, decreases postoperative pain, and shortens hospital stay in patients undergoing radical retropubic prostatectomy. Anesth Analg. 1998 Feb;86(2):235-9. | PubMed | Harvey KP, Adair JD, Isho M, Robinson R. Can intravenous lidocaine decrease postsurgical ileus and shorten hospital stay in elective bowel surgery? A pilot study and literature review. Am J Surg. 2009 Aug;198(2):231-6. | CrossRef | PubMed |
Harvey KP, Adair JD, Isho M, Robinson R. Can intravenous lidocaine decrease postsurgical ileus and shorten hospital stay in elective bowel surgery? A pilot study and literature review. Am J Surg. 2009 Aug;198(2):231-6. | CrossRef | PubMed | Ismail SA. Effects of systemic lidocaine infusion during lumbar discectomy under total intravenous anesthesia. Egyptian Journal of Anaesthesia. 2008 Jan;24(1):39-46. | Link |
Ismail SA. Effects of systemic lidocaine infusion during lumbar discectomy under total intravenous anesthesia. Egyptian Journal of Anaesthesia. 2008 Jan;24(1):39-46. | Link | Juárez-Pichardo JS, Ávila-López A, Serrano-Herrera MA. Preventive postoperative analgesia with dexmetomidine iv compared to lidocaine iv in cholecystectomy. Rev Mex Anest. 2009 Apr-Jun;32(2):81-88. | Link |
Juárez-Pichardo JS, Ávila-López A, Serrano-Herrera MA. Preventive postoperative analgesia with dexmetomidine iv compared to lidocaine iv in cholecystectomy. Rev Mex Anest. 2009 Apr-Jun;32(2):81-88. | Link | Kim HO, Lee SR, Choi WJ, Kim H. Early oral feeding following laparoscopic colorectal cancer surgery. ANZ J Surg. 2014 Jul-Aug;84(7-8):539-44. | CrossRef | PubMed |
Kim HO, Lee SR, Choi WJ, Kim H. Early oral feeding following laparoscopic colorectal cancer surgery. ANZ J Surg. 2014 Jul-Aug;84(7-8):539-44. | CrossRef | PubMed | Kim TH, Kang H, Choi YS, Park JM, Chi KC, Shin HY, Hong JH. Pre- and intraoperative lidocaine injection for preemptive analgesics in laparoscopic gastrectomy: a prospective, randomized, double-blind, placebo-controlled study. J Laparoendosc Adv Surg Tech A. 2013 Aug;23(8):663-8. | CrossRef | PubMed |
Kim TH, Kang H, Choi YS, Park JM, Chi KC, Shin HY, Hong JH. Pre- and intraoperative lidocaine injection for preemptive analgesics in laparoscopic gastrectomy: a prospective, randomized, double-blind, placebo-controlled study. J Laparoendosc Adv Surg Tech A. 2013 Aug;23(8):663-8. | CrossRef | PubMed | Koppert W, Weigand M, Neumann F, Sittl R, Schuettler J, Schmelz M, Hering W. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004 Apr;98(4):1050-5, table of contents. | PubMed |
Koppert W, Weigand M, Neumann F, Sittl R, Schuettler J, Schmelz M, Hering W. Perioperative intravenous lidocaine has preventive effects on postoperative pain and morphine consumption after major abdominal surgery. Anesth Analg. 2004 Apr;98(4):1050-5, table of contents. | PubMed | Lauwick S, Kim DJ, Mistraletti G, Carli F. Functional walking capacity as an outcome measure of laparoscopic prostatectomy: the effect of lidocaine infusion. Br J Anaesth. 2009 Aug;103(2):213-9. | CrossRef | PubMed |
Lauwick S, Kim DJ, Mistraletti G, Carli F. Functional walking capacity as an outcome measure of laparoscopic prostatectomy: the effect of lidocaine infusion. Br J Anaesth. 2009 Aug;103(2):213-9. | CrossRef | PubMed | Martin F, Cherif K, Gentili ME, Enel D, Abe E, Alvarez JC, Mazoit JX, Chauvin M, Bouhassira D, Fletcher D. Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptive pain threshold after total hip arthroplasty. Anesthesiology. 2008 Jul;109(1):118-23. | CrossRef | PubMed | PMC |
Martin F, Cherif K, Gentili ME, Enel D, Abe E, Alvarez JC, Mazoit JX, Chauvin M, Bouhassira D, Fletcher D. Lack of impact of intravenous lidocaine on analgesia, functional recovery, and nociceptive pain threshold after total hip arthroplasty. Anesthesiology. 2008 Jul;109(1):118-23. | CrossRef | PubMed | PMC | Mathew JP, Mackensen GB, Phillips-Bute B, Grocott HP, Glower DD, Laskowitz DT, Blumenthal JA, Newman MF; Neurologic Outcome Research Group (NORG) of the Duke Heart Center. Randomized, double-blinded, placebo controlled study of neuroprotection with lidocaine in cardiac surgery. Stroke. 2009 Mar;40(3):880-7. | CrossRef | PubMed | PMC |
Mathew JP, Mackensen GB, Phillips-Bute B, Grocott HP, Glower DD, Laskowitz DT, Blumenthal JA, Newman MF; Neurologic Outcome Research Group (NORG) of the Duke Heart Center. Randomized, double-blinded, placebo controlled study of neuroprotection with lidocaine in cardiac surgery. Stroke. 2009 Mar;40(3):880-7. | CrossRef | PubMed | PMC | Rimbäck G, Cassuto J, Tollesson PO. Treatment of postoperative paralytic ileus by intravenous lidocaine infusion. Anesth Analg. 1990 Apr;70(4):414-9. | PubMed |
Rimbäck G, Cassuto J, Tollesson PO. Treatment of postoperative paralytic ileus by intravenous lidocaine infusion. Anesth Analg. 1990 Apr;70(4):414-9. | PubMed | Rinne T, Kaukinen S. Does lidocaine protect the heart during coronary revascularisation? Acta Anaesthesiol Scand. 1998 Sep;42(8):936-40. | PubMed |
Rinne T, Kaukinen S. Does lidocaine protect the heart during coronary revascularisation? Acta Anaesthesiol Scand. 1998 Sep;42(8):936-40. | PubMed | Saadawy IM, Kaki AM, Abd El Latif AA, Abd-Elmaksoud AM, Tolba OM. Lidocaine vs. magnesium: effect on analgesia after a laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2010 May;54(5):549-56. | CrossRef | PubMed |
Saadawy IM, Kaki AM, Abd El Latif AA, Abd-Elmaksoud AM, Tolba OM. Lidocaine vs. magnesium: effect on analgesia after a laparoscopic cholecystectomy. Acta Anaesthesiol Scand. 2010 May;54(5):549-56. | CrossRef | PubMed | Striebel HW, Klettke U. [Is intravenous lidocaine infusion suitable for postoperative pain management?]. Schmerz. 1992 Dec;6(4):245-50. German. | PubMed |
Striebel HW, Klettke U. [Is intravenous lidocaine infusion suitable for postoperative pain management?]. Schmerz. 1992 Dec;6(4):245-50. German. | PubMed | Wallin G, Cassuto J, Högström S, Lindén I, Faxén A, Rimbäck G, Hedner T. Effects of lidocaine infusion on the sympathetic response to abdominal surgery. Anesth Analg. 1987 Oct;66(10):1008-13. | PubMed |
Wallin G, Cassuto J, Högström S, Lindén I, Faxén A, Rimbäck G, Hedner T. Effects of lidocaine infusion on the sympathetic response to abdominal surgery. Anesth Analg. 1987 Oct;66(10):1008-13. | PubMed | Wu CT, Borel CO, Lee MS, Yu JC, Liou HS, Yi HD, Yang CP. The interaction effect of perioperative cotreatment with dextromethorphan and intravenous lidocaine on pain relief and recovery of bowel function after laparoscopic cholecystectomy. Anesth Analg. 2005 Feb;100(2):448-53. | PubMed |
Wu CT, Borel CO, Lee MS, Yu JC, Liou HS, Yi HD, Yang CP. The interaction effect of perioperative cotreatment with dextromethorphan and intravenous lidocaine on pain relief and recovery of bowel function after laparoscopic cholecystectomy. Anesth Analg. 2005 Feb;100(2):448-53. | PubMed | Wuethrich PY, Romero J, Burkhard FC, Curatolo M. No benefit from perioperative intravenous lidocaine in laparoscopic renal surgery: a randomised, placebo-controlled study. Eur J Anaesthesiol. 2012 Nov;29(11):537-43. | CrossRef | PubMed |
Wuethrich PY, Romero J, Burkhard FC, Curatolo M. No benefit from perioperative intravenous lidocaine in laparoscopic renal surgery: a randomised, placebo-controlled study. Eur J Anaesthesiol. 2012 Nov;29(11):537-43. | CrossRef | PubMed | Yin LZ. The effect of multimodal analgesia in chronic postoperative pain after modified radical mastectomy. Capital Medical University. 2013. | Link |
Yin LZ. The effect of multimodal analgesia in chronic postoperative pain after modified radical mastectomy. Capital Medical University. 2013. | Link | Dunn LK, Durieux ME. Perioperative Use of Intravenous Lidocaine. Anesthesiology. 2017 Apr;126(4):729-737. | CrossRef | PubMed |
Dunn LK, Durieux ME. Perioperative Use of Intravenous Lidocaine. Anesthesiology. 2017 Apr;126(4):729-737. | CrossRef | PubMed | Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J. Acute pain management: scientific evidence, fourth edition, 2015. Med J Aust. 2016 May 2;204(8):315-7. | PubMed |
Schug SA, Palmer GM, Scott DA, Halliwell R, Trinca J. Acute pain management: scientific evidence, fourth edition, 2015. Med J Aust. 2016 May 2;204(8):315-7. | PubMed | Govindarajan R. Efficacy of Intravenous Lidocaine in the Operative Management of Thyroid Surgery With Intraoperative Nerve Monitoring. Clinical trials [Online] | Link |
Govindarajan R. Efficacy of Intravenous Lidocaine in the Operative Management of Thyroid Surgery With Intraoperative Nerve Monitoring. Clinical trials [Online] | Link | Shah A. Efficacy of Intravenous Lidocaine in the Operative Management of Thyroid Surgery With Intraoperative Nerve Monitoring. Clinical trials [Online] | Link |
Shah A. Efficacy of Intravenous Lidocaine in the Operative Management of Thyroid Surgery With Intraoperative Nerve Monitoring. Clinical trials [Online] | Link | Plattner V. E L I C O : Evaluation de la Lidocaïne par voie Intraveineuse en chirurgie Carcinologique ORL Essai thérapeutique randomisé, contrôlé, en double aveugle, versus placebo évaluant l'épargne morphinique et la douleur chronique postopératoire. Clinical trials [Online] | Link |
Plattner V. E L I C O : Evaluation de la Lidocaïne par voie Intraveineuse en chirurgie Carcinologique ORL Essai thérapeutique randomisé, contrôlé, en double aveugle, versus placebo évaluant l'épargne morphinique et la douleur chronique postopératoire. Clinical trials [Online] | Link | Herzog J. Randomized, double-blind, prospective, placebo-controlled trial of the effect of intravenous lidocaine infusion for postoperative pain management and bowel function in robot assisted laparoscopic colon surgery. Clinical trials [Online] | Link |
Herzog J. Randomized, double-blind, prospective, placebo-controlled trial of the effect of intravenous lidocaine infusion for postoperative pain management and bowel function in robot assisted laparoscopic colon surgery. Clinical trials [Online] | Link | Sahmeddini MA. Comparison the effect of intraoperative ketamine and systemic lidocaine on post operative pain management of opioid dependent patients undergoing orthopedic surgeries. Clinical trials [Online] | Link |
Sahmeddini MA. Comparison the effect of intraoperative ketamine and systemic lidocaine on post operative pain management of opioid dependent patients undergoing orthopedic surgeries. Clinical trials [Online] | Link | Choi YJ. Effect of oxynorm on postoperative pain and recovery from anesthesia in patients undergoing thyroidectomy. Clinical trials [Online] | Link |
Choi YJ. Effect of oxynorm on postoperative pain and recovery from anesthesia in patients undergoing thyroidectomy. Clinical trials [Online] | Link | Yoo Y. The Impact of Intraoperative Systemic Lidocaine Infusion on Chronic Postoperative Pain After Video-assisted Thoracic Surgery (VATS). Clinical trials [Online] | Link |
Yoo Y. The Impact of Intraoperative Systemic Lidocaine Infusion on Chronic Postoperative Pain After Video-assisted Thoracic Surgery (VATS). Clinical trials [Online] | Link | Anesthesia research. Systemic administration of Lidocain for oncological gynaecological surgery: the effect on postoperative pain and consumption of Morphine. Clinical trials [Online] | Link |
Anesthesia research. Systemic administration of Lidocain for oncological gynaecological surgery: the effect on postoperative pain and consumption of Morphine. Clinical trials [Online] | Link | Karlnoski R. Systemic Intraoperative Lidocaine Infusion for Postoperative Pain Management in Obese Patients: A Randomized, Placebo-Controlled Pilot Study. Clinical trials [Online] | Link |
Karlnoski R. Systemic Intraoperative Lidocaine Infusion for Postoperative Pain Management in Obese Patients: A Randomized, Placebo-Controlled Pilot Study. Clinical trials [Online] | Link | Head of Department Anesthesiology. Pilot study: Targeting the inflammatory response and the induction of acute pain after breast cancer surgery with perioperative infusion of lidocaine. Clinical trials [Online] | Link |
Head of Department Anesthesiology. Pilot study: Targeting the inflammatory response and the induction of acute pain after breast cancer surgery with perioperative infusion of lidocaine. Clinical trials [Online] | Link | Hajduk J. Intravenous Lidocaine to Decrease Postoperative Pain in Pediatric Patients Undergoing Tonsillectomy: A Randomized, Double Blind, Placebo Controlled Trial. Clinical trials [Online] | Link |
Hajduk J. Intravenous Lidocaine to Decrease Postoperative Pain in Pediatric Patients Undergoing Tonsillectomy: A Randomized, Double Blind, Placebo Controlled Trial. Clinical trials [Online] | Link | Tiouririne M. IRB-HSR# 13957: IV Lidocaine for Patients Undergoing Primary Breast Cancer Surgery: Effects on Postoperative Recovery and Cancer Recurrence. Clinical trials [Online] | Link |
Tiouririne M. IRB-HSR# 13957: IV Lidocaine for Patients Undergoing Primary Breast Cancer Surgery: Effects on Postoperative Recovery and Cancer Recurrence. Clinical trials [Online] | Link | Mahajan C. Effect of magnesium and lignocaine on postcraniotomy pain: a comparative, randomised, double-blinded, placebo-controlled study. Clinical trials [Online] | Link |
Mahajan C. Effect of magnesium and lignocaine on postcraniotomy pain: a comparative, randomised, double-blinded, placebo-controlled study. Clinical trials [Online] | Link | Trivedi D. The Effect of Perioperative Intravenous Lidocaine on Postoperative Outcomes After
Cardiac Surgery. Clinical trials [Online] | Link |
Trivedi D. The Effect of Perioperative Intravenous Lidocaine on Postoperative Outcomes After
Cardiac Surgery. Clinical trials [Online] | Link | Lintérêt de la Xylocaine® et de la kétamine per et postopératoire sur la prise en charge de la douleur postopératoire aigue et chronique après colectomie par Laparoscopie. Clinical trials [Online] | Link |
Lintérêt de la Xylocaine® et de la kétamine per et postopératoire sur la prise en charge de la douleur postopératoire aigue et chronique après colectomie par Laparoscopie. Clinical trials [Online] | Link | Logvinov I. Perioperative Intravenous Lidocaine Infusion for Patients Undergoing Laparoscopic and Open Pancreatectomies. Clinical trials [Online] | Link |
Logvinov I. Perioperative Intravenous Lidocaine Infusion for Patients Undergoing Laparoscopic and Open Pancreatectomies. Clinical trials [Online] | Link | El-Tahan M. Perioperative Systemic Lidocaine for Enhanced Bowel Recovery After Laparoscopic Bariatric Surgery: A Dose Dependent Study. Clinical trials [Online] | Link |
El-Tahan M. Perioperative Systemic Lidocaine for Enhanced Bowel Recovery After Laparoscopic Bariatric Surgery: A Dose Dependent Study. Clinical trials [Online] | Link | Chuxiong P. Effect of Intravenous Lidocaine on Postoperative Pain Management After Laparoscopy Cholecystectomy. Clinical trials [Online] | Link |
Chuxiong P. Effect of Intravenous Lidocaine on Postoperative Pain Management After Laparoscopy Cholecystectomy. Clinical trials [Online] | Link | Ni J. Effect of intravenous lidocaine for postoperative catheter-related bladder discomfort in patients undergoing gynecological laparotomy. Clinical trials [Online] | Link |
Ni J. Effect of intravenous lidocaine for postoperative catheter-related bladder discomfort in patients undergoing gynecological laparotomy. Clinical trials [Online] | Link | Deem S. Intravenous Lidocaine in the Perioperative Setting and the Effects on Postoperative Pain and Bowel Function Following Cystectomy: A Pilot Study. Clinical trials [Online] | Link |
Deem S. Intravenous Lidocaine in the Perioperative Setting and the Effects on Postoperative Pain and Bowel Function Following Cystectomy: A Pilot Study. Clinical trials [Online] | Link | Lebuffe G. The Interest of the Xylocaine® and Ketamine on the Per and Postoperative Management of Acute and Chronic Postoperative Pain After Colectomy by Laparoscopy. Clinical trials [Online] | Link |
Lebuffe G. The Interest of the Xylocaine® and Ketamine on the Per and Postoperative Management of Acute and Chronic Postoperative Pain After Colectomy by Laparoscopy. Clinical trials [Online] | Link | Rehberg B, Tramèr M, Iselin-Chavez I, Elia N. Efficacy and harm of non-opioid analgesics that are used concomitantly with opioids in the perioperative period: systematic review of systematic reviews. Prospero [Online] | Link |
Rehberg B, Tramèr M, Iselin-Chavez I, Elia N. Efficacy and harm of non-opioid analgesics that are used concomitantly with opioids in the perioperative period: systematic review of systematic reviews. Prospero [Online] | Link | Moppett I. Intraoperative, intravenous lidocaine for prevention of adverse outcomes following surgery: systematic review and meta-analysis. Prospero [Online] | Link |
Moppett I. Intraoperative, intravenous lidocaine for prevention of adverse outcomes following surgery: systematic review and meta-analysis. Prospero [Online] | Link | Li Y. The effectiveness of lidocaine for preventing postoperative cognitive dysfunction: a systematic review and meta-analysis. Prospero [Online] | Link |
Li Y. The effectiveness of lidocaine for preventing postoperative cognitive dysfunction: a systematic review and meta-analysis. Prospero [Online] | Link | Ventham N. IV lidocaine and return of gut function in colorectal surgery. Prospero [Online] | Link |
Ventham N. IV lidocaine and return of gut function in colorectal surgery. Prospero [Online] | Link |