 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
INTRODUCTION
The timing of surgical repair in patients with congenital diaphragmatic hernia has been a controversial topic over the years, and there is still no agreement as to whether immediate repair or late surgery with preoperative stabilization is preferable.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
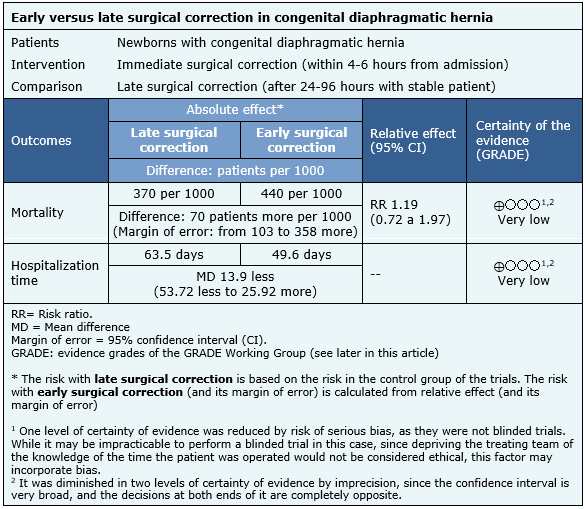
We identified four systematic reviews including 38 studies overall, of which two were randomized trials. We concluded it is not clear whether immediate surgical repair in congenital diaphragmatic hernia increases mortality or decreases hospitalization days compared to late repair because the certainty of evidence is very low.
Congenital diaphragmatic hernia presents with a prevalence of 2 to 4 per 10,000 live births and is associated with high mortality and high costs. Despite significant advances in neonatal and surgical care, management of newborns with congenital diaphragmatic hernia remains a challenge. As for timing of surgical repair, since the 1980s most investigators have advocated delayed surgery, post-preoperative stabilization, using a variety of ventilatory strategies. If late surgery is beneficial compared to immediate repair is still a controversial issue; a convincing improvement in survival has not yet been documented after this strategy is implemented. Patients who survive the neonatal period require long-term follow-up as they are more likely to develop important morbidity, such as chronic lung disease, gastroesophageal reflux, growth restriction, neurological and sensory abnormalities. Due to the high mortality and associated morbidity, it is important to find the best possible alternative to lower these rates.
In congenital diaphragmatic hernia, there is a defect in the diaphragm that allows the passage of intra-abdominal organs (small intestine, stomach, spleen, liver, etc.) to the thoracic cavity; this occupation determines compression of the thoracic organs during its development, which causes hypoplasia and pulmonary hypertension, which affect the normal transition of the cardiorespiratory system at the time of birth. One of the most important prognostic factors in these patients is the presence of pulmonary hypertension, also called persistent fetal circulation. Immediate repair may be beneficial in avoiding persistent pulmonary compression, making ventilation easier for these patients in theory. On the other hand, delayed surgery would allow the patient to make a more adequate transition to extra uterine life, allowing time for hemodynamic adaptation to better cope with the impact of early surgery that could aggravate preexisting pulmonary hypertension. Our purpose is to review available evidence about the optimum timing of repair.
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] which together include 38 primary studies [5],[6],[7],[8], |
|
What types of patients were included* |
The two randomized trials [5],[6] included newborn patients with congenital diaphragmatic hernia which were symptomatic at birth; one of these with the additional requirement that they were symptomatic at within the 12 hours from birth [6]. |
|
What types of interventions were included* |
The two trials [5],[6] evaluated immediate surgical repair, and compared it with late repair.One trial [5] defined immediate repair to the surgery performed within the first 4 hours of admission to the center, and late repair to that performed at least after 24 hours, at the time when the patient was considered stable. The other trial [6] defined immediate repair to the surgery performed within the first 6 hours of admission to the center, and late repair to that performed after 96 hours, when there was no evidence of pulmonary hypertension. |
|
What types of outcomes |
The studies measured multiple outcomes, however, those that were grouped in the identified reviews were:
|
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
The information on the effects of immediate versus late surgical repair in patients with congenital diaphragmatic hernia is based on two randomized trials [5],[6] including 84 patients in total. Both trials reported the outcome mortality and hospitalization time in survivors. One trial [6] further measured the use of extracorporeal membrane oxygenation, the type of procedure used and the complications associated with the interventions. The summary of findings is as follows:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
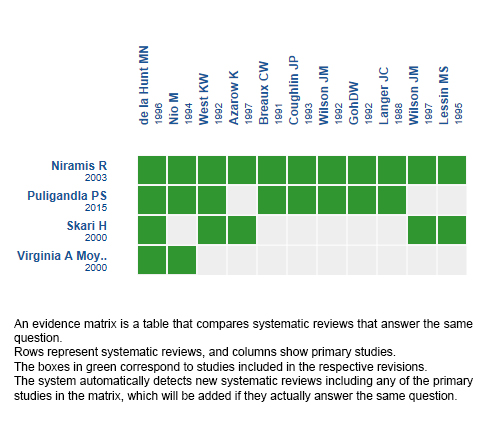
Follow the link to access the interactive version: Late versus early surgical correction for congenital diaphragmatic hernia.
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
The timing of surgical repair in patients with congenital diaphragmatic hernia has been a controversial topic over the years, and there is still no agreement as to whether immediate repair or late surgery with preoperative stabilization is preferable.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified four systematic reviews including 38 studies overall, of which two were randomized trials. We concluded it is not clear whether immediate surgical repair in congenital diaphragmatic hernia increases mortality or decreases hospitalization days compared to late repair because the certainty of evidence is very low.
 Autores:
Alexandra Yunes[1,2], Matías Luco[2,3], Juan Carlos Pattillo[2,4]
Autores:
Alexandra Yunes[1,2], Matías Luco[2,3], Juan Carlos Pattillo[2,4]

Citación: Yunes A, Luco M, Pattillo J. Early versus late surgical correction in congenital diaphragmatic hernia. Medwave 2017 Nov-Dic;17(8):e7081 doi: 10.5867/medwave.2017.09.7081
Fecha de envío: 27/5/2017
Fecha de aceptación: 23/10/2017
Fecha de publicación: 15/11/2017
Origen: Este artículo es producto del Epistemonikos Evidence Synthesis Project de la Fundación Epistemonikos, en colaboración con Medwave para su publicación.
Tipo de revisión: Con revisión por pares sin ciego por parte del equipo metodológico del Epistemonikos Evidence Synthesis Project.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Moyer V, Moya F, Tibboel R, Losty P, Nagaya M, Lally KP. Late versus early surgical correction for congenital diaphragmatic hernia in newborn infants. Cochrane Database Syst Rev. 2000;(3):CD001695. | PubMed |
Moyer V, Moya F, Tibboel R, Losty P, Nagaya M, Lally KP. Late versus early surgical correction for congenital diaphragmatic hernia in newborn infants. Cochrane Database Syst Rev. 2000;(3):CD001695. | PubMed | 1. Puligandla PS, Grabowski J, Austin M, Hedrick H, Renaud E, Arnold M, Williams RF, Graziano K, Dasgupta R, McKee M, Lopez ME, Jancelewicz T, Goldin A, Downard CD, Islam S. Management of congenital diaphragmatic hernia: A systematic review from the APSA outcomes and evidence based practice committee. J Pediatr Surg. 2015 Nov;50(11):1958-70.
| CrossRef | PubMed |
1. Puligandla PS, Grabowski J, Austin M, Hedrick H, Renaud E, Arnold M, Williams RF, Graziano K, Dasgupta R, McKee M, Lopez ME, Jancelewicz T, Goldin A, Downard CD, Islam S. Management of congenital diaphragmatic hernia: A systematic review from the APSA outcomes and evidence based practice committee. J Pediatr Surg. 2015 Nov;50(11):1958-70.
| CrossRef | PubMed | Skari H, Bjornland K, Haugen G, Egeland T, Emblem R. Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg. 2000 Aug;35(8):1187-97. | PubMed |
Skari H, Bjornland K, Haugen G, Egeland T, Emblem R. Congenital diaphragmatic hernia: a meta-analysis of mortality factors. J Pediatr Surg. 2000 Aug;35(8):1187-97. | PubMed | Niramis R. Technology assessment for management of congenital diaphragmatic hernia: immediate versus delayed surgery. J Med Assoc Thai. 2003 Aug;86 Suppl 3:S727-33. | PubMed |
Niramis R. Technology assessment for management of congenital diaphragmatic hernia: immediate versus delayed surgery. J Med Assoc Thai. 2003 Aug;86 Suppl 3:S727-33. | PubMed | de la Hunt MN, Madden N, Scott JE, Matthews JN, Beck J, Sadler C, Barrett AM, Boddy SA, Bray RJ, Cusick E, Gardner L, Hargrave SA, Hinton W, Rangecroft L, Spicer R, Stafford M, Thomas D, Vallis CJ, Wagget J. Is delayed surgery really better for congenital diaphragmatic hernia?: a prospective randomized clinical trial. J Pediatr Surg. 1996 Nov;31(11):1554-6. | PubMed |
de la Hunt MN, Madden N, Scott JE, Matthews JN, Beck J, Sadler C, Barrett AM, Boddy SA, Bray RJ, Cusick E, Gardner L, Hargrave SA, Hinton W, Rangecroft L, Spicer R, Stafford M, Thomas D, Vallis CJ, Wagget J. Is delayed surgery really better for congenital diaphragmatic hernia?: a prospective randomized clinical trial. J Pediatr Surg. 1996 Nov;31(11):1554-6. | PubMed | 1. Nio M, Haase G, Kennaugh J, Bui K, Atkinson JB. A prospective randomized trial of delayed versus immediate repair of congenital diaphragmatic hernia. J Pediatr Surg. 1994 May;29(5):618-21. | PubMed |
1. Nio M, Haase G, Kennaugh J, Bui K, Atkinson JB. A prospective randomized trial of delayed versus immediate repair of congenital diaphragmatic hernia. J Pediatr Surg. 1994 May;29(5):618-21. | PubMed | 1. Azarow K, Messineo A, Pearl R, Filler R, Barker G, Bohn D. Congenital diaphragmatic hernia--a tale of two cities: the Toronto experience. J Pediatr Surg. 1997 Mar;32(3):395-400. | PubMed |
1. Azarow K, Messineo A, Pearl R, Filler R, Barker G, Bohn D. Congenital diaphragmatic hernia--a tale of two cities: the Toronto experience. J Pediatr Surg. 1997 Mar;32(3):395-400. | PubMed | Hollinger LE, Lally PA, Tsao K, Wray CJ, Lally KP; Congenital Diaphragmatic Hernia Study Group.. A risk-stratified analysis of delayed congenital diaphragmatic hernia repair: does timing of operation matter? Surgery. 2014 Aug;156(2):475-82. | CrossRef | PubMed |
Hollinger LE, Lally PA, Tsao K, Wray CJ, Lally KP; Congenital Diaphragmatic Hernia Study Group.. A risk-stratified analysis of delayed congenital diaphragmatic hernia repair: does timing of operation matter? Surgery. 2014 Aug;156(2):475-82. | CrossRef | PubMed | 1. Lally KP, Paranka MS, Roden J, Georgeson KE, Wilson JM, Lillehei CW, Breaux CW Jr, Poon M, Clark RH, Atkinson JB. Congenital diaphragmatic hernia. Stabilization and repair on ECMO. Ann Surg. 1992 Nov;216(5):569-73. | PubMed | PMC |
1. Lally KP, Paranka MS, Roden J, Georgeson KE, Wilson JM, Lillehei CW, Breaux CW Jr, Poon M, Clark RH, Atkinson JB. Congenital diaphragmatic hernia. Stabilization and repair on ECMO. Ann Surg. 1992 Nov;216(5):569-73. | PubMed | PMC | 1. Steimle CN, Meric F, Hirschl RB, Bozynski M, Coran AG, Bartlett RH. Effect of extracorporeal life support on survival when applied to all patients with congenital diaphragmatic hernia. J Pediatr Surg. 1994 Aug;29(8):997-1001. | PubMed |
1. Steimle CN, Meric F, Hirschl RB, Bozynski M, Coran AG, Bartlett RH. Effect of extracorporeal life support on survival when applied to all patients with congenital diaphragmatic hernia. J Pediatr Surg. 1994 Aug;29(8):997-1001. | PubMed | Coughlin JP, Drucker DE, Cullen ML, Klein MD. Delayed repair of congenital diaphragmatic hernia. Am Surg. 1993 Feb;59(2):90-3. | PubMed |
Coughlin JP, Drucker DE, Cullen ML, Klein MD. Delayed repair of congenital diaphragmatic hernia. Am Surg. 1993 Feb;59(2):90-3. | PubMed | Partridge EA, Peranteau WH, Rintoul NE, Herkert LM, Flake AW, Adzick NS, Hedrick HL. Timing of repair of congenital diaphragmatic hernia in patients supported by extracorporeal membrane oxygenation (ECMO). J Pediatr Surg. 2015 Feb;50(2):260-2. | CrossRef | PubMed |
Partridge EA, Peranteau WH, Rintoul NE, Herkert LM, Flake AW, Adzick NS, Hedrick HL. Timing of repair of congenital diaphragmatic hernia in patients supported by extracorporeal membrane oxygenation (ECMO). J Pediatr Surg. 2015 Feb;50(2):260-2. | CrossRef | PubMed | Langer JC, Filler RM, Bohn DJ, Shandling B, Ein SH, Wesson DE, Superina RA. Timing of surgery for congenital diaphragmatic hernia: is emergency operation necessary? J Pediatr Surg. 1988 Aug;23(8):731-4. | PubMed |
Langer JC, Filler RM, Bohn DJ, Shandling B, Ein SH, Wesson DE, Superina RA. Timing of surgery for congenital diaphragmatic hernia: is emergency operation necessary? J Pediatr Surg. 1988 Aug;23(8):731-4. | PubMed | Wilson JM, Lund DP, Lillehei CW, Vacanti JP. Congenital diaphragmatic hernia--a tale of two cities: the Boston experience. J Pediatr Surg. 1997 Mar;32(3):401-5. | PubMed |
Wilson JM, Lund DP, Lillehei CW, Vacanti JP. Congenital diaphragmatic hernia--a tale of two cities: the Boston experience. J Pediatr Surg. 1997 Mar;32(3):401-5. | PubMed | Lessin MS, Thompson IM, Deprez MF, Cullen ML, Whittlesey GC, Klein MD. Congenital diaphragmatic hernia with or without extracorporeal membrane oxygenation: are we making progress? J Am Coll Surg. 1995 Jul;181(1):65-71. | PubMed |
Lessin MS, Thompson IM, Deprez MF, Cullen ML, Whittlesey GC, Klein MD. Congenital diaphragmatic hernia with or without extracorporeal membrane oxygenation: are we making progress? J Am Coll Surg. 1995 Jul;181(1):65-71. | PubMed | Sigalet DL, Tierney A, Adolph V, Perreault T, Finer N, Hallgren R, Laberge JM. Timing of repair of congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation support. J Pediatr Surg. 1995 Aug;30(8):1183-7. | PubMed |
Sigalet DL, Tierney A, Adolph V, Perreault T, Finer N, Hallgren R, Laberge JM. Timing of repair of congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation support. J Pediatr Surg. 1995 Aug;30(8):1183-7. | PubMed | Reickert CA, Hirschl RB, Atkinson JB, Dudell G, Georgeson K, Glick P, Greenspan J, Kays D, Klein M, Lally KP, Mahaffey S, Ryckman F, Sawin R, Short BL, Stolar CJ, Thompson A, Wilson JM. Congenital diaphragmatic hernia survival and use of extracorporeal life support at selected level III nurseries with multimodality support. Surgery. 1998 Mar;123(3):305-10. | PubMed |
Reickert CA, Hirschl RB, Atkinson JB, Dudell G, Georgeson K, Glick P, Greenspan J, Kays D, Klein M, Lally KP, Mahaffey S, Ryckman F, Sawin R, Short BL, Stolar CJ, Thompson A, Wilson JM. Congenital diaphragmatic hernia survival and use of extracorporeal life support at selected level III nurseries with multimodality support. Surgery. 1998 Mar;123(3):305-10. | PubMed | Finer NN, Tierney A, Etches PC, Peliowski A, Ainsworth W. Congenital diaphragmatic hernia: developing a protocolized approach. J Pediatr Surg. 1998 Sep;33(9):1331-7. | PubMed |
Finer NN, Tierney A, Etches PC, Peliowski A, Ainsworth W. Congenital diaphragmatic hernia: developing a protocolized approach. J Pediatr Surg. 1998 Sep;33(9):1331-7. | PubMed | Fallon SC, Cass DL, Olutoye OO, Zamora IJ, Lazar DA, Larimer EL, Welty SE, Moise AA, Demny AB, Lee TC. Repair of congenital diaphragmatic hernias on Extracorporeal Membrane Oxygenation (ECMO): does early repair improve patient survival? J Pediatr Surg. 2013 Jun;48(6):1172-6. | CrossRef | PubMed |
Fallon SC, Cass DL, Olutoye OO, Zamora IJ, Lazar DA, Larimer EL, Welty SE, Moise AA, Demny AB, Lee TC. Repair of congenital diaphragmatic hernias on Extracorporeal Membrane Oxygenation (ECMO): does early repair improve patient survival? J Pediatr Surg. 2013 Jun;48(6):1172-6. | CrossRef | PubMed | Vazquez WD, Cheu HW. Hemorrhagic complications and repair of congenital diaphragmatic hernias: does timing of the repair make a difference? Data from the Extracorporeal Life Support Organization. J Pediatr Surg. 1994;29(8):1002–5 [discussion 1005–6].
Vazquez WD, Cheu HW. Hemorrhagic complications and repair of congenital diaphragmatic hernias: does timing of the repair make a difference? Data from the Extracorporeal Life Support Organization. J Pediatr Surg. 1994;29(8):1002–5 [discussion 1005–6].  Breaux CW, Rouse TM, Cain WS, et al. Improvement in survival of patients with congenital diaphragmatic hernia utilizing a strategy of delayed repair after medical and/or extracorporeal membrane oxygenation stabilization. J Pediatr Surg. 1991;26(3):333–6 [discussion 336–8].
Breaux CW, Rouse TM, Cain WS, et al. Improvement in survival of patients with congenital diaphragmatic hernia utilizing a strategy of delayed repair after medical and/or extracorporeal membrane oxygenation stabilization. J Pediatr Surg. 1991;26(3):333–6 [discussion 336–8].  Wilson JM, Lund DP, Lillehei CW, et al. Delayed repair and preoperative ECMO does not improve survival in high-risk congenital diaphragmatic hernia. J Pediatr Surg. 1992;27(3):368–72 [discussion 373–5].
Wilson JM, Lund DP, Lillehei CW, et al. Delayed repair and preoperative ECMO does not improve survival in high-risk congenital diaphragmatic hernia. J Pediatr Surg. 1992;27(3):368–72 [discussion 373–5].  GohDW, Drake DP, Brereton RJ, et al. Delayed surgery for congenital diaphragmatic hernia. Br J Surg. 1992;79(7):644–6.
GohDW, Drake DP, Brereton RJ, et al. Delayed surgery for congenital diaphragmatic hernia. Br J Surg. 1992;79(7):644–6.  Connors RH, Tracy T, Bailey PV, et al. Congenital diaphragmatic hernia repair on ECMO. J Pediatr Surg. 1990;25(10):1043–6 [discussion 1046–7].
Connors RH, Tracy T, Bailey PV, et al. Congenital diaphragmatic hernia repair on ECMO. J Pediatr Surg. 1990;25(10):1043–6 [discussion 1046–7].  Rozmiarek AJ, Qureshi FG, Cassidy L, et al. Factors influencing survival in newborns with congenital diaphragmatic hernia: the relative role of timing of surgery. J Pediatr Surg. 2004;39(6):821–4 [discussion 821–4].
Rozmiarek AJ, Qureshi FG, Cassidy L, et al. Factors influencing survival in newborns with congenital diaphragmatic hernia: the relative role of timing of surgery. J Pediatr Surg. 2004;39(6):821–4 [discussion 821–4].  DassingerMS, Copeland DR, Gossett J, et al. Early repair of congenital diaphragmatic hernia on extracorporeal membrane oxygenation. J Pediatr Surg. 2010;45(4):693–7.
DassingerMS, Copeland DR, Gossett J, et al. Early repair of congenital diaphragmatic hernia on extracorporeal membrane oxygenation. J Pediatr Surg. 2010;45(4):693–7.  Congenital Diaphragmatic Hernia Study Group, Bryner BS, West BT, et al. Congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: does timing of repair matter?. J Pediatr Surg. 2009;44(6):1165–71 [discussion 1171–2].
Congenital Diaphragmatic Hernia Study Group, Bryner BS, West BT, et al. Congenital diaphragmatic hernia requiring extracorporeal membrane oxygenation: does timing of repair matter?. J Pediatr Surg. 2009;44(6):1165–71 [discussion 1171–2].  West KW, Bengston K, Rescorla FJ, et al. Delayed surgical repair and ECMO improves survival in congenital diaphragmatic hernia. Ann Surg. 1992;216:454-460.
West KW, Bengston K, Rescorla FJ, et al. Delayed surgical repair and ECMO improves survival in congenital diaphragmatic hernia. Ann Surg. 1992;216:454-460.  Kamata S, Usui N, Ishikawa S, Okuyama H, Kitayama Y, Sawai T, Imura K, Okada A. Prolonged preoperative stabilization using high-frequency oscillatory ventilation does not improve the outcome in neonates with congenital diaphragmatic hernia. Pediatr Surg Int. 1998 Oct;13(8):542-6. | PubMed |
Kamata S, Usui N, Ishikawa S, Okuyama H, Kitayama Y, Sawai T, Imura K, Okada A. Prolonged preoperative stabilization using high-frequency oscillatory ventilation does not improve the outcome in neonates with congenital diaphragmatic hernia. Pediatr Surg Int. 1998 Oct;13(8):542-6. | PubMed | Shanbhogue LK, Tam PK, Ninan G, Lloyd DA. Preoperative stabilisation in congenital diaphragmatic hernia. Arch Dis Child. 1990 Oct;65(10 Spec No):1043-4. | PubMed | PMC |
Shanbhogue LK, Tam PK, Ninan G, Lloyd DA. Preoperative stabilisation in congenital diaphragmatic hernia. Arch Dis Child. 1990 Oct;65(10 Spec No):1043-4. | PubMed | PMC | Charlton AJ, Bruce J, Davenport M. Timing of surgery in congenital diaphragmatic hernia. Low mortality after pre-operative stabilisation. Anaesthesia. 1991 Oct;46(10):820-3. | PubMed |
Charlton AJ, Bruce J, Davenport M. Timing of surgery in congenital diaphragmatic hernia. Low mortality after pre-operative stabilisation. Anaesthesia. 1991 Oct;46(10):820-3. | PubMed | Reickert CA, Hirschl RB, Schumacher R, Geiger JD, Cox C, Teitelbaum DH, Polley TZ Jr, Harmon CM, Lelli JL, Coran AG. Effect of very delayed repair of congenital diaphragmatic hernia on survival and extracorporeal life support use. Surgery. 1996 Oct;120(4):766-72; discussion 772-3. | PubMed |
Reickert CA, Hirschl RB, Schumacher R, Geiger JD, Cox C, Teitelbaum DH, Polley TZ Jr, Harmon CM, Lelli JL, Coran AG. Effect of very delayed repair of congenital diaphragmatic hernia on survival and extracorporeal life support use. Surgery. 1996 Oct;120(4):766-72; discussion 772-3. | PubMed | Cartlidge PH, Mann NP, Kapila L. Preoperative stabilisation in congenital diaphragmatic hernia. Arch Dis Child. 1986 Dec;61(12):1226-8. | PubMed | PMC |
Cartlidge PH, Mann NP, Kapila L. Preoperative stabilisation in congenital diaphragmatic hernia. Arch Dis Child. 1986 Dec;61(12):1226-8. | PubMed | PMC | Wiener ES. Congenital posterolateral diaphragmatic hernia: new dimensions in management. Surgery. 1982 Oct;92(4):670-81. | PubMed |
Wiener ES. Congenital posterolateral diaphragmatic hernia: new dimensions in management. Surgery. 1982 Oct;92(4):670-81. | PubMed | McNamara JJ, Eraklis AJ, Gross RE. Congenital posterolateral diaphragmatic hernia in the newborn. J Thorac Cardiovasc Surg. 1968 Jan;55(1):55-9. | PubMed |
McNamara JJ, Eraklis AJ, Gross RE. Congenital posterolateral diaphragmatic hernia in the newborn. J Thorac Cardiovasc Surg. 1968 Jan;55(1):55-9. | PubMed | Hazebroek FW, Tibboel D, Bos AP, Pattenier AW, Madern GC, Bergmeijer JH, Molenaar JC. Congenital diaphragmatic hernia: impact of preoperative stabilization. A prospective pilot study in 13 patients. J Pediatr Surg. 1988 Dec;23(12):1139-46. | PubMed |
Hazebroek FW, Tibboel D, Bos AP, Pattenier AW, Madern GC, Bergmeijer JH, Molenaar JC. Congenital diaphragmatic hernia: impact of preoperative stabilization. A prospective pilot study in 13 patients. J Pediatr Surg. 1988 Dec;23(12):1139-46. | PubMed | Nakayama DK, Motoyama EK, Tagge EM. Effect of preoperative stabilization on respiratory system compliance and outcome in newborn infants with congenital diaphragmatic hernia. J Pediatr. 1991 May;118(5):793-9. | PubMed |
Nakayama DK, Motoyama EK, Tagge EM. Effect of preoperative stabilization on respiratory system compliance and outcome in newborn infants with congenital diaphragmatic hernia. J Pediatr. 1991 May;118(5):793-9. | PubMed | Reyes C, Chang LK, Waffarn F, et al. Delayed repair of congenital diaphragmatic hernia with early high-frequency oscillatory ventilation during preoperative stabilization. J Pediatr Surg. 1998;33(7):1010–4 [discussion 1014–6].
Reyes C, Chang LK, Waffarn F, et al. Delayed repair of congenital diaphragmatic hernia with early high-frequency oscillatory ventilation during preoperative stabilization. J Pediatr Surg. 1998;33(7):1010–4 [discussion 1014–6].  Miguet D, Claris O, Lapillonne A, Bakr A, Chappuis JP, Salle BL. Preoperative stabilization using high-frequency oscillatory ventilation in the management of congenital diaphragmatic hernia. Crit Care Med. 1994 Sep;22(9 Suppl): S77-82. | PubMed |
Miguet D, Claris O, Lapillonne A, Bakr A, Chappuis JP, Salle BL. Preoperative stabilization using high-frequency oscillatory ventilation in the management of congenital diaphragmatic hernia. Crit Care Med. 1994 Sep;22(9 Suppl): S77-82. | PubMed | Adolph V, Flageole H, Perreault T, Johnston A, Nguyen L, Youssef S, Guttman F, Laberge JM. Repair of congenital diaphragmatic hernia after weaning from extracorporeal membrane oxygenation. J Pediatr Surg. 1995 Feb;30(2):349-52. | PubMed |
Adolph V, Flageole H, Perreault T, Johnston A, Nguyen L, Youssef S, Guttman F, Laberge JM. Repair of congenital diaphragmatic hernia after weaning from extracorporeal membrane oxygenation. J Pediatr Surg. 1995 Feb;30(2):349-52. | PubMed | Wung JT, Sahni R, Moffitt ST, Lipsitz E, Stolar CJ. Congenital diaphragmatic hernia: survival treated with very delayed surgery, spontaneous respiration, and no chest tube. J Pediatr Surg. 1995 Mar;30(3):406-9. | PubMed |
Wung JT, Sahni R, Moffitt ST, Lipsitz E, Stolar CJ. Congenital diaphragmatic hernia: survival treated with very delayed surgery, spontaneous respiration, and no chest tube. J Pediatr Surg. 1995 Mar;30(3):406-9. | PubMed | Frenckner B, Ehrén H, Granholm T, Lindén V, Palmér K. Improved results in patients who have congenital diaphragmatic hernia using preoperative stabilization, extracorporeal membrane oxygenation, and delayed surgery. J Pediatr Surg. 1997 Aug;32(8):1185-9. | PubMed |
Frenckner B, Ehrén H, Granholm T, Lindén V, Palmér K. Improved results in patients who have congenital diaphragmatic hernia using preoperative stabilization, extracorporeal membrane oxygenation, and delayed surgery. J Pediatr Surg. 1997 Aug;32(8):1185-9. | PubMed | Snoek, K. G., Reiss, I. K., Greenough, A., Capolupo, I., Urlesberger, B., Wessel, L., & Tibboel, D. (2016). Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: The CDH EURO consortium consensus-2015 update. Neonatology, 110(1), 66-74.
Snoek, K. G., Reiss, I. K., Greenough, A., Capolupo, I., Urlesberger, B., Wessel, L., & Tibboel, D. (2016). Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: The CDH EURO consortium consensus-2015 update. Neonatology, 110(1), 66-74.