 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
ABOUT THE UPDATE: This article updates the June 2014 Living FRISBEE (Living FRISBEE: Living FRIendly Summary of the Body of Evidence using Epistemonikos). It incorporates a new systematic review identifying one study not included in previous reviews. The new evidence leads to substantial changes in the existing evidence.
ASBTRACT: Pentoxifylline is an inhibitor of tumor necrosis factor, and has been proposed as treatment for alcoholic hepatitis. However, it is not clear if it is effective, or if it adds benefit to the treatment with corticosteroids. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified three systematic reviews including eight randomized controlled trials addressing the question of this article. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded pentoxifylline probably leads to little or no difference in mortality in alcoholic hepatitis.
This article is an update of the Living FRISBEE (Living FRISBEE: Living FRIendly Summary of the Body of Evidence using Epistemonikos) published in June 2014 (doi: 10.5867/medwave.2014.06.6002), based on the publication of a new systematic review including an additional randomized trial larger than all previous studies combined.
The new evidence incorporated in this summary leads to a change in the direction of the effect (from benefit to no benefit) with the corresponding modifications in key messages and considerations for decision-making.
Alcoholic hepatitis is associated to high morbidity and mortality. During the course of the disease an inflammatory process occurs. Corticosteroids have been used because of their antiinflammatory properties, but they are associated to important adverse effects. The oral tumor necrosis factor inhibitor pentoxifylline has been postulated as an alternative for the treatment of alcoholic hepatitis. However, its effects are not clear.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found three systematic reviews [1],[2],[3] including eight randomized controlled trials reported in 13 references [4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14],[15],[16]. |
|
What types of patients were included |
All studies included patients with severe alcoholic hepatitis, generally based on a Maddrey score > 32. Only three studies required histological confirmation of alcoholic hepatitis as inclusion criteria [4],[11],[16]. One study included patients with advanced cirrhosis, with only some patients presenting severe alcoholic hepatitis [4]. Only data on the latter were used in the analysis. |
|
What types of interventions were included |
Pentoxifylline dose was 400 mg t.i.d. in six studies [4],[5],[7],[12],[15],[16]. One study administered 1200 mg q.d. [11] and one study did not report dosification [10]. Duration of treatment was 10 days in one study [11], 28 days in six [5],[9],[10],[14],[15],[16] and 6 months in one [12]. In four studies standard treatment did not include corticosteroids [5],[9],[10],[11] and in three studies both groups received an identical schedule of corticosteroids [4],[14],[16. One trial evaluated both alternatives (pentoxifylline versus placebo, and pentoxifylline plus corticosteroids versus corticosteroids) in different study arms [15]. All of the studies using corticosteroids administered prednisolone. |
|
What types of outcomes |
All of the studies measured short-term mortality, and three also measured long-term mortality (three to six months) [4],[14],[16. Other outcomes assessed in the different systematic reviews were: hepatic mortality, renal dysfunction (hepatorrenal syndrome, serum creatinine elevation), bilirubin plasma levels, and tumor necrosis factor plasma levels. |
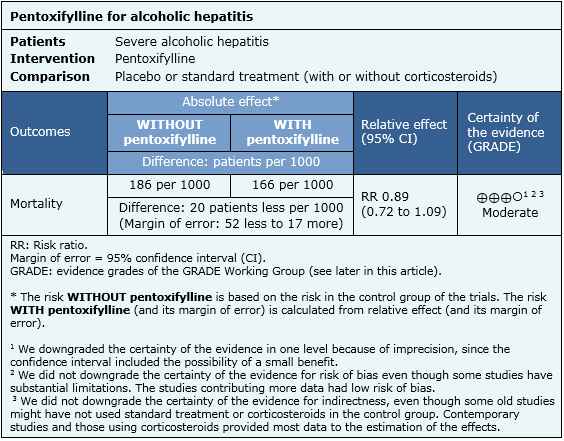
Information on the effects of pentoxifylline for alcoholic hepatitis is based on eight randomized controlled studies involving 1,653 patients. All of the studies reported mortality. The summary of findings is the following:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
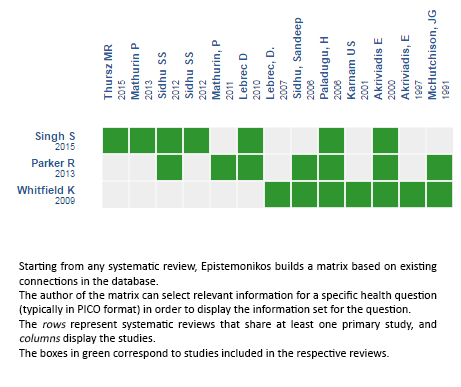
Follow the link to access the interactive version: Pentoxyfilline (alone or added to corticosteroids) for acute alcoholic hepatitis
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

ABOUT THE UPDATE: This article updates the June 2014 Living FRISBEE (Living FRISBEE: Living FRIendly Summary of the Body of Evidence using Epistemonikos). It incorporates a new systematic review identifying one study not included in previous reviews. The new evidence leads to substantial changes in the existing evidence.
ASBTRACT: Pentoxifylline is an inhibitor of tumor necrosis factor, and has been proposed as treatment for alcoholic hepatitis. However, it is not clear if it is effective, or if it adds benefit to the treatment with corticosteroids. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified three systematic reviews including eight randomized controlled trials addressing the question of this article. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded pentoxifylline probably leads to little or no difference in mortality in alcoholic hepatitis.
 Autores:
Gabriel Rada[1,2,3,4,5], Matías Arteaga[1,3], Roberto Candia[2,3,6]
Autores:
Gabriel Rada[1,2,3,4,5], Matías Arteaga[1,3], Roberto Candia[2,3,6]

Citación: Rada G, Arteaga M, Candia R. Is pentoxifylline effective in alcoholic hepatitis? –First update. Medwave 2016;16(Suppl2):e6469 doi: 10.5867/medwave.2016.6469
Fecha de publicación: 14/6/2016

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Parker R, Armstrong MJ, Corbett C, Rowe IA, Houlihan DD. Systematic review: pentoxifylline for the treatment of severe alcoholic hepatitis. Aliment Pharmacol Ther. 2013 May;37(9):845-54. | CrossRef | PubMed |
Parker R, Armstrong MJ, Corbett C, Rowe IA, Houlihan DD. Systematic review: pentoxifylline for the treatment of severe alcoholic hepatitis. Aliment Pharmacol Ther. 2013 May;37(9):845-54. | CrossRef | PubMed | Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009 Oct 7;(4):CD007339. | CrossRef | PubMed |
Whitfield K, Rambaldi A, Wetterslev J, Gluud C. Pentoxifylline for alcoholic hepatitis. Cochrane Database Syst Rev. 2009 Oct 7;(4):CD007339. | CrossRef | PubMed | Singh S, Murad MH, Chandar AK, Bongiorno CM, Singal AK, Atkinson SR, et al. Comparative Effectiveness of Pharmacological Interventions for Severe Alcoholic Hepatitis: A Systematic Review and Network Meta-analysis. Gastroenterology. 2015 Oct;149(4):958-70.e12. | CrossRef | PubMed |
Singh S, Murad MH, Chandar AK, Bongiorno CM, Singal AK, Atkinson SR, et al. Comparative Effectiveness of Pharmacological Interventions for Severe Alcoholic Hepatitis: A Systematic Review and Network Meta-analysis. Gastroenterology. 2015 Oct;149(4):958-70.e12. | CrossRef | PubMed | Lebrec D, Thabut D, Oberti F, Perarnau JM, Condat B, Barraud H, et al. Pentoxifylline does not decrease short-term mortality but does reduce complications in patients with advanced cirrhosis. Gastroenterology. 2010 May;138(5):1755-62. | CrossRef | PubMed |
Lebrec D, Thabut D, Oberti F, Perarnau JM, Condat B, Barraud H, et al. Pentoxifylline does not decrease short-term mortality but does reduce complications in patients with advanced cirrhosis. Gastroenterology. 2010 May;138(5):1755-62. | CrossRef | PubMed | Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology. 2000 Dec;119(6):1637-48. | PubMed |
Akriviadis E, Botla R, Briggs W, Han S, Reynolds T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology. 2000 Dec;119(6):1637-48. | PubMed | Sidhu SS, Goyal O, Singla P, Gupta D, Sood A, Chhina RS, et al. Corticosteroid plus pentoxifylline is not better than corticosteroid alone for improving survival in severe alcoholic hepatitis (COPE trial). Dig Dis Sci. 2012 Jun;57(6):1664-71. | CrossRef | PubMed |
Sidhu SS, Goyal O, Singla P, Gupta D, Sood A, Chhina RS, et al. Corticosteroid plus pentoxifylline is not better than corticosteroid alone for improving survival in severe alcoholic hepatitis (COPE trial). Dig Dis Sci. 2012 Jun;57(6):1664-71. | CrossRef | PubMed | Mathurin P, Louvet A, Dao T, Nahon P, Diaz E, Carbonell E, et al. Addition of pentoxifylline to prednisolone for severe alcoholic hepatitis does not improve 6-month survival: Results of the CORPENTOX trial. Annual Meeting of the American Association for the Study of Liver Diseases: The Liver Meeting (62nd : California); 20112011. | Link |
Mathurin P, Louvet A, Dao T, Nahon P, Diaz E, Carbonell E, et al. Addition of pentoxifylline to prednisolone for severe alcoholic hepatitis does not improve 6-month survival: Results of the CORPENTOX trial. Annual Meeting of the American Association for the Study of Liver Diseases: The Liver Meeting (62nd : California); 20112011. | Link | Sidhu S, Singla M, Bhatia KL. Pentoxifylline reduces disease severity and prevents renal impairment in severe acute alcoholic hepatitis: A double blind, placebo controlled trial. Hepatology. 2006 2006;44(4 Suppl 1):373A-4A. | Link |
Sidhu S, Singla M, Bhatia KL. Pentoxifylline reduces disease severity and prevents renal impairment in severe acute alcoholic hepatitis: A double blind, placebo controlled trial. Hepatology. 2006 2006;44(4 Suppl 1):373A-4A. | Link | Paladugu H, Sawant P, Dalvi L, Kudalkar J. Role of pentoxifylline in treatment of severe acute alcoholic hepatitis – a randomized controlled trial. Journal of Gastroenterology and Hepatology. 2006 2006;21(supp s6):A459. | CrossRef |
Paladugu H, Sawant P, Dalvi L, Kudalkar J. Role of pentoxifylline in treatment of severe acute alcoholic hepatitis – a randomized controlled trial. Journal of Gastroenterology and Hepatology. 2006 2006;21(supp s6):A459. | CrossRef | McHutchison, JG, Runyon, BA, Draguesku, JO, Comineelli, F, Person, JL, J, Castracane. Pentoxifylline may prevent renal impairment (hepatorenal syndrome) in severe acute alcoholic hepatitis. Hepatology. 1991;14(4 (Pt 2)):96.
McHutchison, JG, Runyon, BA, Draguesku, JO, Comineelli, F, Person, JL, J, Castracane. Pentoxifylline may prevent renal impairment (hepatorenal syndrome) in severe acute alcoholic hepatitis. Hepatology. 1991;14(4 (Pt 2)):96.  Lebrec D, Thabut D, Oberti F, Perarnau JM, Condat B, Barraud H, et al. Pentoxifylline for the treatment of patients with advanced cirrhosis. A randomized, placebo-controlled, double-blind trial. 58th Annual Meeting of the American Association for the Study of Liver Diseases; 20072007. p. 249A. | Link |
Lebrec D, Thabut D, Oberti F, Perarnau JM, Condat B, Barraud H, et al. Pentoxifylline for the treatment of patients with advanced cirrhosis. A randomized, placebo-controlled, double-blind trial. 58th Annual Meeting of the American Association for the Study of Liver Diseases; 20072007. p. 249A. | Link | Akriviadis, E, Botla, R, Briggs, W, Han, S, Reynolds, T, Shakil, O. Improved short-term survival with pentoxifylline treatment in severe acute alcoholic hepatitis. Hepatology. 1997;26(4):250A
Akriviadis, E, Botla, R, Briggs, W, Han, S, Reynolds, T, Shakil, O. Improved short-term survival with pentoxifylline treatment in severe acute alcoholic hepatitis. Hepatology. 1997;26(4):250A  Sidhu SS, Goyal O, Singla M, Bhatia KL, Chhina RS, Sood A. Pentoxifylline in severe alcoholic hepatitis: a prospective, randomised trial. J Assoc Physicians India. 2012 May;60:20-2. | PubMed |
Sidhu SS, Goyal O, Singla M, Bhatia KL, Chhina RS, Sood A. Pentoxifylline in severe alcoholic hepatitis: a prospective, randomised trial. J Assoc Physicians India. 2012 May;60:20-2. | PubMed | Thursz MR, Richardson P, Allison M, Austin A, Bowers M, Day CP, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med. 2015 Apr 23;372(17):1619-28. | CrossRef | PubMed |
Thursz MR, Richardson P, Allison M, Austin A, Bowers M, Day CP, et al. Prednisolone or pentoxifylline for alcoholic hepatitis. N Engl J Med. 2015 Apr 23;372(17):1619-28. | CrossRef | PubMed | Mathurin P, Louvet A, Duhamel A, Nahon P, Carbonell N, Boursier J, et al. Prednisolone with vs without pentoxifylline and survival of patients with severe alcoholic hepatitis: a randomized clinical trial. JAMA. 2013 Sep 11;310(10):1033-41. | CrossRef | PubMed |
Mathurin P, Louvet A, Duhamel A, Nahon P, Carbonell N, Boursier J, et al. Prednisolone with vs without pentoxifylline and survival of patients with severe alcoholic hepatitis: a randomized clinical trial. JAMA. 2013 Sep 11;310(10):1033-41. | CrossRef | PubMed |