 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
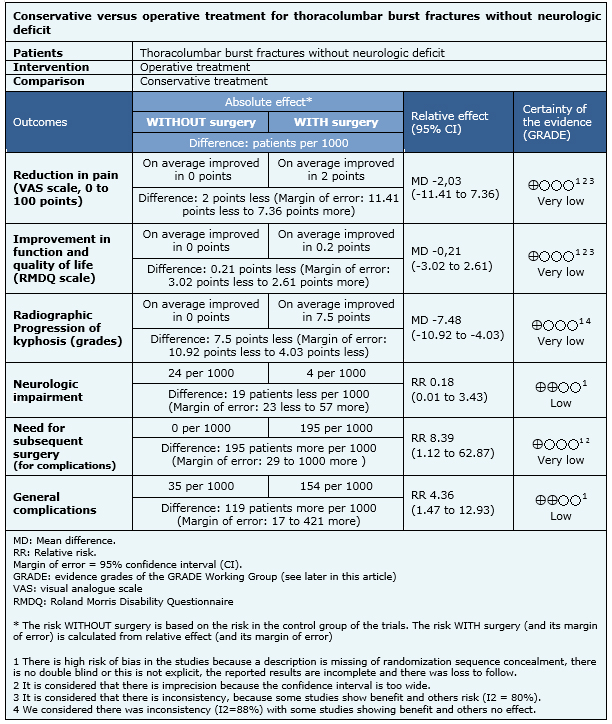
Thoracolumbar burst fractures account for up to 17% of major spinal fractures. Both conservative and operative treatments are widely used in clinical practice to manage thoracolumbar burst fractures. Previous studies showed good functional results with both treatments, but surgical approach has been associated with higher cost and risks of causing unnecessary adverse effects. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified six systematic reviews including four randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded that operative treatment may decrease the risk of neurologic impairment, but in turn, could increase the risk of general complications. It is unclear whether there are differences in pain reduction, improvement in function and quality of life, need for subsequent surgery or radiographic progression of kyphosis in both groups.
Thoracolumbar burst fractures account for 17% of major spinal fractures [1]. Burst fractures are produced by axial compression load resulting in failure of the anterior and middle columns of the spine. The incidence of neurological deficit caused by thoracolumbar burst fractures is estimated to be 50% to 60% [1],[2]. Although many injuries of the thoracolumbar spinal cord do not result in paralysis, they may leave an unstable spinal segment due to disruption of bone elements and soft tissues, which can cause late paralysis [1]. There are controversial opinions on the ideal treatment of patients with thoracolumbar burst fractures without neurological deficit. Both conservative and surgical treatments are widely used in clinical practice. Previous studies have shown that conservative treatment with early mobilization achieved good functional results, even in fractures with posterior column compromise. Surgical treatment has also shown favorable radiographic results and same functional results than the orthopedic treatment, but at a higher cost and with the risk of exposing patients to unnecessary adverse consequences.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found six systematic reviews [3],[4],[5],[6],[7],[8], including four randomized controlled trials [9],[10],[11],[12]. |
|
What types of patients were included |
All studies included adult patients (age 18-65 years) with no pathologic thoracolumbar burst fractures without neurological deficit [9],[10],[11],[12]. One study included patients with CT concordant with retropulsion of the vertebral body into the medullar canal [11], one study included patients with CT that ruled out dislocations, with pedicles and facet joints intact despite the fracture of the pedicle [10], one study included patients with CT concordant with residual spinal canal > 50% of normal [9], and one study did not discriminate by type of canal compromise [12]. |
|
What types of interventions were included |
All studies compared conservative versus surgical management independent of the type of treatment [9],[10],[11],[12]. As conservative treatment two studies used brace [9],[10], one used brace or cast [11] and one used corset [12]. As surgical treatment two studies used fixation with instrumentation [10],[11], one study used posterior stabilization with transpedicular graft or posterolateral fusion [12] and one study did not specify [9]. |
|
What types of outcomes |
Reduction of pain by visual analog scale (VAS), Oswestry back pain questionnaire, Short Form-36 and Greenough Low Back Outcome Score (GLBOS); improvement in function and quality of life by Roland Morris Disability Questionnaire (RMDQ); need for subsequent surgery; neurologic impairment and general complications were measured. Other outcomes measured were time to return to work, progression of spinal canal stenosis, radiographic progression of kyphosis (degrees), treatment costs and duration of hospitalization. |
|
We found three systematic reviews [5], [6], [7], including 14 studies reported in 21 references [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28]. Eight studies correspond to randomized controlled trials (15 references [9], [10], [11], [12], [13], [14], [16], [17], [19], [21], [22], [23], [24], [26], [27]). This table and the summary in general are based on the latter. One study [15] did not contribute data to any of the outcomes of interest. |
Information on conservative versus surgical treatment in thoracolumbar burst fractures without neurological deficit is based on four randomized controlled trials that included 201 patients. Three studies evaluated pain reduction by visual analog scale (VAS) [10],[11],[12], two studies assessed improvement in function and quality of life by Roland Morris Disability Questionnaire (RMDQ) [9],[10],[11],[12], all studies reported radiographic progression of kyphosis (degrees) and neurologic impairment [9],[10],[11],[12] and three studies evaluated subsequent surgery and general complications [10],[11],[12].
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
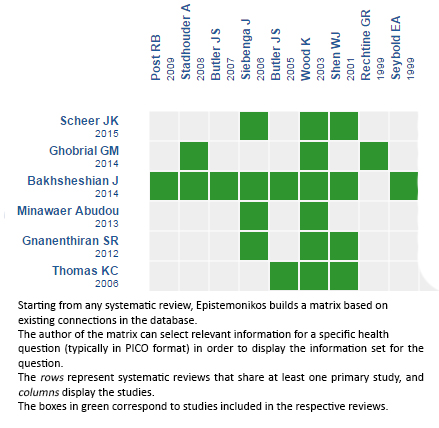
Follow the link to access the interactive version: Conservative versus operative treatment for thoracolumbar burst fractures without neurologic deficit
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Thoracolumbar burst fractures account for up to 17% of major spinal fractures. Both conservative and operative treatments are widely used in clinical practice to manage thoracolumbar burst fractures. Previous studies showed good functional results with both treatments, but surgical approach has been associated with higher cost and risks of causing unnecessary adverse effects. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified six systematic reviews including four randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded that operative treatment may decrease the risk of neurologic impairment, but in turn, could increase the risk of general complications. It is unclear whether there are differences in pain reduction, improvement in function and quality of life, need for subsequent surgery or radiographic progression of kyphosis in both groups.
 Autores:
Carolina Avilés[1,2], Sebastián Flores[1,2], Marcelo Molina[2,3]
Autores:
Carolina Avilés[1,2], Sebastián Flores[1,2], Marcelo Molina[2,3]

Citación: Avilés C, Flores S, Molina M. Conservative versus operative treatment for thoracolumbar burst fractures without neurologic deficit. Medwave 2016;16(Suppl 1):e6383 doi: 10.5867/medwave.2016.6383
Fecha de publicación: 15/3/2016

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983 Nov-Dec;8(8):817-31. | PubMed |
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983 Nov-Dec;8(8):817-31. | PubMed | McEvoy RD, Bradford DS. The management of burst fractures of the thoracic and lumbar spine. Experience in 53 patients. Spine (Phila Pa 1976). 1985 Sep;10(7):631-7. | PubMed |
McEvoy RD, Bradford DS. The management of burst fractures of the thoracic and lumbar spine. Experience in 53 patients. Spine (Phila Pa 1976). 1985 Sep;10(7):631-7. | PubMed | Abudou M, Chen X, Kong X, Wu T. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2013 Jun 6;6:CD005079. | CrossRef | PubMed |
Abudou M, Chen X, Kong X, Wu T. Surgical versus non-surgical treatment for thoracolumbar burst fractures without neurological deficit. Cochrane Database Syst Rev. 2013 Jun 6;6:CD005079. | CrossRef | PubMed | Scheer JK, Bakhsheshian J, Fakurnejad S, Oh T, Dahdaleh NS, Smith ZA. Evidence-Based Medicine of Traumatic Thoracolumbar Burst Fractures: A Systematic Review of Operative Management across 20 Years. Global Spine J. 2015 Feb;5(1):73-82. | CrossRef | PubMed |
Scheer JK, Bakhsheshian J, Fakurnejad S, Oh T, Dahdaleh NS, Smith ZA. Evidence-Based Medicine of Traumatic Thoracolumbar Burst Fractures: A Systematic Review of Operative Management across 20 Years. Global Spine J. 2015 Feb;5(1):73-82. | CrossRef | PubMed | Gnanenthiran SR, Adie S, Harris IA. Nonoperative versus operative treatment for thoracolumbar burst fractures without neurologic deficit: a meta-analysis. Clin Orthop Relat Res. 2012 Feb;470(2):567-77. | CrossRef | PubMed |
Gnanenthiran SR, Adie S, Harris IA. Nonoperative versus operative treatment for thoracolumbar burst fractures without neurologic deficit: a meta-analysis. Clin Orthop Relat Res. 2012 Feb;470(2):567-77. | CrossRef | PubMed | Ghobrial GM, Maulucci CM, Maltenfort M, Dalyai RT, Vaccaro AR, Fehlings MG, et al. Operative and nonoperative adverse events in the management of traumatic fractures of the thoracolumbar spine: a systematic review. Neurosurg Focus. 2014;37(1):E8. | CrossRef | PubMed |
Ghobrial GM, Maulucci CM, Maltenfort M, Dalyai RT, Vaccaro AR, Fehlings MG, et al. Operative and nonoperative adverse events in the management of traumatic fractures of the thoracolumbar spine: a systematic review. Neurosurg Focus. 2014;37(1):E8. | CrossRef | PubMed | Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006 May;4(5):351-8. | PubMed |
Thomas KC, Bailey CS, Dvorak MF, Kwon B, Fisher C. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006 May;4(5):351-8. | PubMed | Bakhsheshian J, Dahdaleh NS, Fakurnejad S, Scheer JK, Smith ZA. Evidence-based management of traumatic thoracolumbar burst fractures: a systematic review of nonoperative management. Neurosurg Focus. 2014;37(1):E1. | CrossRef | PubMed |
Bakhsheshian J, Dahdaleh NS, Fakurnejad S, Scheer JK, Smith ZA. Evidence-based management of traumatic thoracolumbar burst fractures: a systematic review of nonoperative management. Neurosurg Focus. 2014;37(1):E1. | CrossRef | PubMed | Hitchon PW, Torner JC, Haddad SF, Follett KA. Management options in thoracolumbar burst fractures. Surg Neurol. 1998 Jun;49(6):619-26; discussion 626-7. | PubMed |
Hitchon PW, Torner JC, Haddad SF, Follett KA. Management options in thoracolumbar burst fractures. Surg Neurol. 1998 Jun;49(6):619-26; discussion 626-7. | PubMed | Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 2001 May 1;26(9):1038-45. | PubMed |
Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 2001 May 1;26(9):1038-45. | PubMed | Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003 May;85-A(5):773-81 | PubMed |
Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003 May;85-A(5):773-81 | PubMed | Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, et al. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976). 2006 Dec 1;31(25):2881-90. | PubMed |
Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, et al. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976). 2006 Dec 1;31(25):2881-90. | PubMed | Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, et al. Diagnosis and management of thoracolumbar spine fractures. Instr Course Lect. 2004;53:359-73. | PubMed |
Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, et al. Diagnosis and management of thoracolumbar spine fractures. Instr Course Lect. 2004;53:359-73. | PubMed |