 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
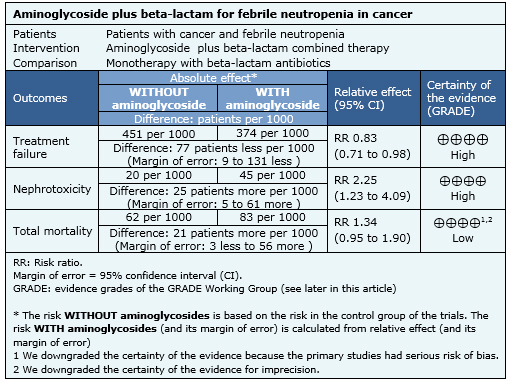
It is still controversial if the combined use of beta-lactam antibiotics and aminoglycosides has advantages over broad-spectrum beta-lactam monotherapy for the empirical treatment of cancer patients with febrile neutropenia. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified three systematic reviews including 14 pertinent randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded the combination of beta-lactam antibiotics and aminoglycosides probably does not lead to a reduced mortality in febrile neutropenic cancer patients and it might increase nephrotoxicity.
Patients with cancer have predisposition to infections that increase morbidity and mortality. Many factors contribute to this risk, including neutropenia and the anatomic barrier disruption due to the underlying disease or its treatment. This has led to the use of empirical antibiotics when infection is suspected in patients with fever, before isolating the pathogen or determining its sensitivity.
The combination of beta-lactams and aminoglycosides has been one of the most widely used treatment options. It aims to increase antimicrobial spectrum, and a synergistic effect has been proposed too, preventing the appearance of intra-treatment resistance. Currently, there are alternatives for beta-lactam monotherapy with wide coverage over gram positive and negative bacteria, which can be used to replace combinations. Furthermore, the addition of aminoglycosides increases adverse effects risk, mainly renal toxicity.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found three systematic reviews [1],[2],[3], including 14 randomized controlled trials reported in 17 references [4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14], |
|
What types of patients were included |
Eleven studies [6],[7],[10],[11],[14],[15],[16],[17],[18], Six studies [6],[7],[8],[9],[14],[18] included patients with hematologic malignancy, one study [10] included patients with solid tumors and six studies [4],[11],[15],[17],[19],[20], included both. In three studies [4],[8],[14] patients with bone marrow transplantation were included. Most of the studies considered patients with moderate neutropenia (<1000 leukocytes/mm3) and five studies [4],[6],[8],[9],[11] included patients with severe neutropenia. |
|
What types of interventions were included |
All included studies compared combination therapy (beta-lactam plus aminoglycosides) versus monotherapy with the same beta-lactam. All studies used a beta-lactam with antipseudomonic activity (piperaciline-tazobactam, cefepime, ceftazidime, cefoperazone and imipenem) and 12 of 14 studies [4],[6],[7],[10],[11],[14],[15],[16],[17], |
|
What types of outcomes |
The main outcomes were overall mortality, mortality related to infection, treatment failure and nephrotoxicity. |
The information about the effects of the association between aminoglycosides and beta-lactams in cancer patients with febrile neutropenia is based on 14 randomized controlled trials that included 2670 patients. Fourteen studies reported treatment failure, ten studies overall mortality [4],[6],[7],[9],[14],[15],[16],[18],[19],[20], seven studies measured mortality related to infection [4],[6],[9],[14],[15],[16],[18],[20] and eight studies reported nephrotoxicity [6],[7],[10],[11],[14],[17],[18],[19].

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
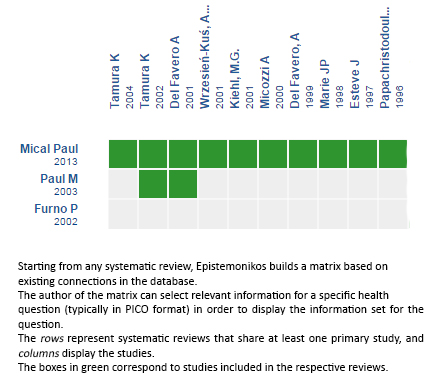
Follow the link to access the interactive version: Beta‐lactam versus the same beta‐lactam plus aminoglycoside for febrile neutropenic cancer patients
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

It is still controversial if the combined use of beta-lactam antibiotics and aminoglycosides has advantages over broad-spectrum beta-lactam monotherapy for the empirical treatment of cancer patients with febrile neutropenia. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified three systematic reviews including 14 pertinent randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded the combination of beta-lactam antibiotics and aminoglycosides probably does not lead to a reduced mortality in febrile neutropenic cancer patients and it might increase nephrotoxicity.
 Autores:
Valeria Contreras[1,2], Sebastián Sepúlveda[1,2], Ana Heredia[2,3]
Autores:
Valeria Contreras[1,2], Sebastián Sepúlveda[1,2], Ana Heredia[2,3]

Citación: Contreras V, Sepúlveda S, Heredia A. Is the addition of aminoglycosides to beta-lactams in cancer patients with febrile neutropenia needed?. Medwave 2015;16(Suppl 1):e6379 doi: 10.5867/medwave.2016.6379
Fecha de publicación: 24/2/2016

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Furno P, Bucaneve G, Del Favero A. Monotherapy or aminoglycoside-containing combinations for empirical antibiotic treatment of febrile neutropenic patients: a meta-analysis. Lancet Infect Dis. 2002 Apr;2(4):231-42. | PubMed |
Furno P, Bucaneve G, Del Favero A. Monotherapy or aminoglycoside-containing combinations for empirical antibiotic treatment of febrile neutropenic patients: a meta-analysis. Lancet Infect Dis. 2002 Apr;2(4):231-42. | PubMed | Paul M, Dickstein Y, Schlesinger A, Grozinsky-Glasberg S, Soares-Weiser K, Leibovici L. Beta-lactam versus beta-lactam-aminoglycoside combination therapy in cancer patients with neutropenia. Cochrane Database Syst Rev. 2013 Jun 29;6:CD003038. | CrossRef | PubMed |
Paul M, Dickstein Y, Schlesinger A, Grozinsky-Glasberg S, Soares-Weiser K, Leibovici L. Beta-lactam versus beta-lactam-aminoglycoside combination therapy in cancer patients with neutropenia. Cochrane Database Syst Rev. 2013 Jun 29;6:CD003038. | CrossRef | PubMed | Paul M, Soares-Weiser K, Leibovici L. Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for fever with neutropenia: systematic review and meta-analysis. BMJ. 2003 May 24;326(7399):1111. | PubMed |
Paul M, Soares-Weiser K, Leibovici L. Beta lactam monotherapy versus beta lactam-aminoglycoside combination therapy for fever with neutropenia: systematic review and meta-analysis. BMJ. 2003 May 24;326(7399):1111. | PubMed | Del Favero A, Menichetti F, Martino P, Bucaneve G, Micozzi A, Gentile G, et al. A multicenter, double-blind, placebo-controlled trial comparing piperacillin-tazobactam with and without amikacin as empiric therapy for febrile neutropenia. Clin Infect Dis. 2001 Oct 15;33(8):1295-301. | PubMed |
Del Favero A, Menichetti F, Martino P, Bucaneve G, Micozzi A, Gentile G, et al. A multicenter, double-blind, placebo-controlled trial comparing piperacillin-tazobactam with and without amikacin as empiric therapy for febrile neutropenia. Clin Infect Dis. 2001 Oct 15;33(8):1295-301. | PubMed | Del Favero A, Menichetti F, Micozzi A, Bucaneve G, Martino P. Double-blind, randomized clinical trial comparing monotherapy with piperacillin-tazobactam vs. piperacillin-tazobactam plus amikacin as empiric therapy for febrile neutropenic cancer patients. 39th Interscience Conference on Antimicrobial Agents and Chemotherapy, San Francisco, CA; 1999: 722. | Link |
Del Favero A, Menichetti F, Micozzi A, Bucaneve G, Martino P. Double-blind, randomized clinical trial comparing monotherapy with piperacillin-tazobactam vs. piperacillin-tazobactam plus amikacin as empiric therapy for febrile neutropenic cancer patients. 39th Interscience Conference on Antimicrobial Agents and Chemotherapy, San Francisco, CA; 1999: 722. | Link | Doyen C, Tepatondele JM, Wauters G, Michaux JL. A randomized therapeutic trial for ceftazidime versus ceftazidime and amikacin in febrile granulopenic patients. International Congress of Chemotherapy (13th : 1983: Vienna: Spitzy KH); 1983: 26-9. | Link |
Doyen C, Tepatondele JM, Wauters G, Michaux JL. A randomized therapeutic trial for ceftazidime versus ceftazidime and amikacin in febrile granulopenic patients. International Congress of Chemotherapy (13th : 1983: Vienna: Spitzy KH); 1983: 26-9. | Link | Esteve J, Nomdedeu B, Mensa J, Guardia R, Marco F, Montserrat E. Piperacillin/tazobactam vs. piperacillin/tazobactam plus amikacin as empiric therapy for fever in neutropenic patients. Blood. 1997;90(Suppl 1):229b. | Link |
Esteve J, Nomdedeu B, Mensa J, Guardia R, Marco F, Montserrat E. Piperacillin/tazobactam vs. piperacillin/tazobactam plus amikacin as empiric therapy for fever in neutropenic patients. Blood. 1997;90(Suppl 1):229b. | Link | Kiehl MG, Bischoff M, Basara N, Guenzelmann S, Fauser A. A prospective randomized trial comparing the efficacy and safety of piperacillin/tazobactam versus piperacillin/tazobactam plus netilmicin in the treatment of febrile neutropenia in allogeneic stem cell recipients. Abstracts Of The Interscience Conference On Antimicrobial Agents & Chemotherapy. 2001 2001(41):267. | Link |
Kiehl MG, Bischoff M, Basara N, Guenzelmann S, Fauser A. A prospective randomized trial comparing the efficacy and safety of piperacillin/tazobactam versus piperacillin/tazobactam plus netilmicin in the treatment of febrile neutropenia in allogeneic stem cell recipients. Abstracts Of The Interscience Conference On Antimicrobial Agents & Chemotherapy. 2001 2001(41):267. | Link | Kinsey SE, Machin SJ, Goldstone AH. Ceftazidime monotherapy is as effective as ceftazidime combined with gentamicin in the treatment of febrile neutropenic patients. J Hosp Infect. 1990 Apr;15 Suppl A:49-53. | PubMed |
Kinsey SE, Machin SJ, Goldstone AH. Ceftazidime monotherapy is as effective as ceftazidime combined with gentamicin in the treatment of febrile neutropenic patients. J Hosp Infect. 1990 Apr;15 Suppl A:49-53. | PubMed | Kojima A, Shinkai T, Soejima Y, Okamoto H, Eguchi K, Sasaki Y, et al. A randomized prospective study of imipenem-cilastatin with or without amikacin as an empirical antibiotic treatment for febrile neutropenic patients. Am J Clin Oncol. 1994 Oct;17(5):400-4. | PubMed |
Kojima A, Shinkai T, Soejima Y, Okamoto H, Eguchi K, Sasaki Y, et al. A randomized prospective study of imipenem-cilastatin with or without amikacin as an empirical antibiotic treatment for febrile neutropenic patients. Am J Clin Oncol. 1994 Oct;17(5):400-4. | PubMed | Marie JP, Pico J, Lapierre V, Maulard C, Pappo M, Chiche D, et al. Comparative trial of ceftazidime alone, ceftazidime + amikacin and ceftazidime + vancomycin as empiric therapy of febrile cancer patients with induced prolonged neutropenia. Médecine et Maladies Infectieuses. 1991 7;21(7):386-8.
Marie JP, Pico J, Lapierre V, Maulard C, Pappo M, Chiche D, et al. Comparative trial of ceftazidime alone, ceftazidime + amikacin and ceftazidime + vancomycin as empiric therapy of febrile cancer patients with induced prolonged neutropenia. Médecine et Maladies Infectieuses. 1991 7;21(7):386-8.  Marie JP, Vekhoff A, Pico JL, Guy H, Andremont A, Richet H. Neutropenic infections: a review of the French Febrile Aplasia Study Group trials in 608 febrile neutropenic patients. J Antimicrob Chemother. 1998 Jun;41 Suppl D:57-64. | PubMed |
Marie JP, Vekhoff A, Pico JL, Guy H, Andremont A, Richet H. Neutropenic infections: a review of the French Febrile Aplasia Study Group trials in 608 febrile neutropenic patients. J Antimicrob Chemother. 1998 Jun;41 Suppl D:57-64. | PubMed | Micozzi A, Bucaneve G, Menichetti F, Martino P, Del Favero A, Program GI. Double blind, randomized, clinical trial comparing monotherapy with piperacillin-tazobactam versus piperacillin-tazobactam plus amikacin as empiric therapy for febrile neutropenic cancer patients. Supportive care in cancer. 2000;8 (Suppl:160). | Link |
Micozzi A, Bucaneve G, Menichetti F, Martino P, Del Favero A, Program GI. Double blind, randomized, clinical trial comparing monotherapy with piperacillin-tazobactam versus piperacillin-tazobactam plus amikacin as empiric therapy for febrile neutropenic cancer patients. Supportive care in cancer. 2000;8 (Suppl:160). | Link | Nováková IR, Donnelly JP, de Pauw BE. Ceftazidime with or without amikacin for the empiric treatment of localized infections in febrile, granulocytopenic patients. Ann Hematol. 1991 Oct;63(4):195-200. | PubMed |
Nováková IR, Donnelly JP, de Pauw BE. Ceftazidime with or without amikacin for the empiric treatment of localized infections in febrile, granulocytopenic patients. Ann Hematol. 1991 Oct;63(4):195-200. | PubMed | Papachristodoulou A, Vaslamatzis M, Xynogalos S, Papacharalambous A, Alexopoulos CG. Ceftazidime (CFZ) monotherapy as empirical initial treatment of febrile neutropenia cancer patients (Pts). Ann of Oncol. 1996;7(suppl 5):146. | CrossRef |
Papachristodoulou A, Vaslamatzis M, Xynogalos S, Papacharalambous A, Alexopoulos CG. Ceftazidime (CFZ) monotherapy as empirical initial treatment of febrile neutropenia cancer patients (Pts). Ann of Oncol. 1996;7(suppl 5):146. | CrossRef | Piccart M, Klastersky J, Meunier F, Lagast H, Van Laethem Y, Weerts D. Single-drug versus combination empirical therapy for gram-negative bacillary infections in febrile cancer patients with and without granulocytopenia. Antimicrob Agents Chemother. 1984 Dec;26(6):870-5. | PubMed |
Piccart M, Klastersky J, Meunier F, Lagast H, Van Laethem Y, Weerts D. Single-drug versus combination empirical therapy for gram-negative bacillary infections in febrile cancer patients with and without granulocytopenia. Antimicrob Agents Chemother. 1984 Dec;26(6):870-5. | PubMed | Rolston KV, Berkey P, Bodey GP, Anaissie EJ, Khardori NM, Joshi JH, et al. A comparison of imipenem to ceftazidime with or without amikacin as empiric therapy in febrile neutropenic patients. Arch Intern Med. 1992 Feb;152(2):283-91. | PubMed |
Rolston KV, Berkey P, Bodey GP, Anaissie EJ, Khardori NM, Joshi JH, et al. A comparison of imipenem to ceftazidime with or without amikacin as empiric therapy in febrile neutropenic patients. Arch Intern Med. 1992 Feb;152(2):283-91. | PubMed | Tamura K, Imajo K, Akiyama N, Suzuki K, Urabe A, Ohyashiki K, et al. Randomized trial of cefepime monotherapy or cefepime in combination with amikacin as empirical therapy for febrile neutropenia. Clin Infect Dis. 2004 Jul 15;39 Suppl 1:S15-24. | PubMed |
Tamura K, Imajo K, Akiyama N, Suzuki K, Urabe A, Ohyashiki K, et al. Randomized trial of cefepime monotherapy or cefepime in combination with amikacin as empirical therapy for febrile neutropenia. Clin Infect Dis. 2004 Jul 15;39 Suppl 1:S15-24. | PubMed | Tamura K, Matsuoka H, Tsukada J, Masuda M, Ikeda S, Matsuishi E, et al. Cefepime or carbapenem treatment for febrile neutropenia as a single agent is as effective as a combination of 4th-generation cephalosporin + aminoglycosides: comparative study. Am J Hematol. 2002 Dec;71(4):248-55. | PubMed |
Tamura K, Matsuoka H, Tsukada J, Masuda M, Ikeda S, Matsuishi E, et al. Cefepime or carbapenem treatment for febrile neutropenia as a single agent is as effective as a combination of 4th-generation cephalosporin + aminoglycosides: comparative study. Am J Hematol. 2002 Dec;71(4):248-55. | PubMed | Wrzesień-Kuś A, Jamroziak K, Wierzbowska A, Robak T. Cefepime in monotherapy or in combination with amikacine as the empirical treatment of febrile neutropenic patients. Acta Haematologica Polonica. 2001;32(2):165-72. | Link |
Wrzesień-Kuś A, Jamroziak K, Wierzbowska A, Robak T. Cefepime in monotherapy or in combination with amikacine as the empirical treatment of febrile neutropenic patients. Acta Haematologica Polonica. 2001;32(2):165-72. | Link |