 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
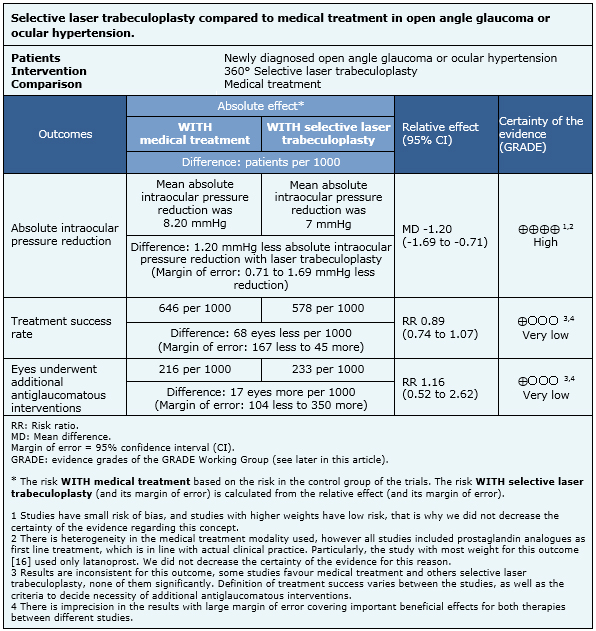
Selective laser trabeculoplasty is a relatively new therapeutic alternative for the management of open angle glaucoma and ocular hypertension. On the other hand, medical treatment has robust data supporting its efficacy and has progressed in last decades with the introduction of prostaglandin analogues. To compare these two therapies, we searched Epistemonikos database, which is maintained by screening 30 databases, and identified four systematic reviews including four randomized and one non-randomized clinical trial. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded that selective laser trabeculoplasty leads to a smaller absolute intraocular pressure reduction than medical treatment. However, it is not clear if there are differences in treatment success rate or need of additional antiglaucomatous interventions, because the quality of the evidence is low.
Open angle glaucoma and ocular hypertension are initially asymptomatic conditions that frequently course with additional optic nerve damage that may lead to progressive loss of visual field and irreversible blindness at an end stage if they are not treated appropriately. In clinical practice medical treatment is usually preferred as first line therapy, but laser trabeculoplasty or surgery are also valid options in selected patients as suggested by The American Academy of Ophthalmology [1].
Laser trabeculoplasty was first introduced in 1979, using argon laser [2]. A decade later, the procedure demonstrated to be as effective as timolol for intraocular pressure reduction in the initial management of open angle glaucoma or ocular hypertension [3]. Few years later prostaglandin analogues were introduced and demonstrated to produce greater intraocular pressure reduction than timolol [4], with the advantage of requiring only once daily dosing. However, adherence to medical treatment remains an important problem as shown by recent reports of 25% of missed doses even when patients knew they were being monitored [5].
In this context, selective laser trabeculoplasty [6] could offer many theoretical advantages over argon laser trabeculoplasty such as easier application, and lower energy parameters that could reduce coagulative damage in trabecular meshwork. The latter has used as an argument to justify that the procedure can be repeated while the recommendation for argon laser trabeculoplasty is against repeatability. There is evidence that the effectiveness of both interventions is similar [7], and despite only weak evidence of repeatability for selective laser trabeculoplasty [8], it is being used in clinical practice as a repeatable procedure without reports of intraocular pressure decompensation as previously seen with argon laser trabeculoplasty [9],[10].
Taking into account the introduction of new and better medications as well as selective laser trabeculoplasty a procedure that is easier to apply and potentially repeatable, we consider this effectiveness comparison of selective laser trabeculoplasty vs medical treatment for intraocular pressure reduction in open-angle glaucoma or ocular hypertension of great interest.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found four systematic reviews [7],[11],[12],[13] that include four randomized clinical trials [14],[15],[16],[17] and one non randomized prospective study [18]. In this table and the summary in general, we only considered the randomized trials. Three of the four systematic reviews did a meta-analysis [7],[11],[19]. |
|
What types of patients were included |
All of the randomized clinical trials included patients with ocular hypertension or primary open angle glaucoma. Two of them included also patients with secondary open angle glaucoma, particularly pseudoexfoliation glaucoma [14],[17] and pigment dispersion syndrome [17]. Only one study included patients with mixed mechanism open angle glaucoma with a narrow angle, if laser peripheral iridotomy was performed more than three months ago, but this study did not report the number of patients included with this diagnosis [14]. All the studies included newly or recently diagnosed patients. Two of them also included patients previously controlled with medical treatment [14],[17]. There is no distinction by sex. Only two studies restricted age as inclusion criteria: one of them considered only patients under the age of 80 [16]; the other included patients between 25 and 82 years [14]. All the studies excluded patients with previous laser procedure or ocular surgery disturbing the aqueous outflow. Three of the randomized clinical trials considered pregnancy as exclusion criteria [14],[15],[16]. Studies included patients that belong to multiple ethnic groups: Chinese population [15], African or afro-Caribbean [17], white [14],[17] or non-white [14]. Only one study established an upper limit of intraocular pressure, including patients with pressures between 24 and 34 mmHg in the higher eye, and 20 mmHg or more in the contralateral eye [14]. |
|
What types of interventions were included |
All the studies compared selective laser trabeculoplasty with medical treatment. Regarding laser trabeculoplasty, all randomized clinical trials used similar procedures, with energy ranging from 0,2 to 1,7 mJ per application, adjusted according to patients characteristics and response, and applied over 360 degrees (approximately 100 non-overlapping laser spots). Regarding the extent of trabecular meshwork treated, one study [17] randomized patients into four groups, one receiving medical treatment, and other three groups treated with selective laser trabeculoplasty in different extent of trabecular meshwork: 360º, 180º and 90º respectively. This differs from the other three randomized clinical trials [14],[15],[16], which applied selective laser trabeculoplasty over 360º of trabecular meshwork. Only treatments performed over 360 degrees were considered for this summary. Medical treatment modality varied across studies. Two of the randomized clinical trials [16],[17] used exclusively latanoprost, a prostaglandin analogue. One study used [15] a variable combination of medicines including latanoprost, beta-blocker, pilocarpine and dorzolamide. The other randomized clinical trial [14] applied a flexible algorithm of treatment with sequential steps starting with prostaglandin analogues, then adding or substituting to beta-blocker, then brimonidine, and finally dorzolamide, brinzolamide or a fixed-combination dorzolamide-timolol. Follow up also varied across studies: one of them [15] followed patients for five years; two studies [14],[17] did for one year; and other study [16] for four to six months. |
|
What types of outcomes |
The systematic reviews included here, analysed the following outcomes: absolute intraocular pressure reduction [7],[19], treatment success rate [7],[19] and need of additional antiglaucomatous interventions [19]. There is heterogeneity in treatment success definition: one primary study [16] defined it as achieving an intraocular pressure reduction of 20% or more; other study [17] used two definitions, considering intraocular pressure reduction of 20% and 30% from baseline; one study [14] defined treatment success when achieving a target intraocular pressure reduction calculated by using a formula; other [15] defined it indirectly considering treatment failure when intraocular pressure was greater than 21 mmHg in follow up. Different adverse effects were evaluated by three of the randomized clinical trials [14],[15],[17]: ocular pain or discomfort [17], anterior chamber reaction [15], peripheral anterior synechiae [14], uveitis [14],[17], post-laser intraocular pressure spike [15],[17] and increase in trabecular meshwork pigmentation [15]. |
This information is based on four randomized clinical trials including 271 eyes of 201 patients. All studies measured absolute intraocular pressure reduction and treatment success rate. Three of them [14],[15],[17] evaluated the need of additional antiglaucomatous interventions. The summary of finding is the following:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
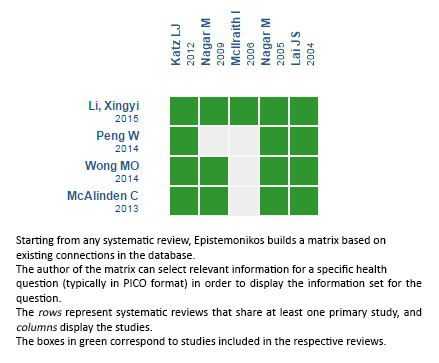
Follow the link to access the interactive version: Selective laser trabeculoplasty versus medical treatment for open angle glaucoma and ocular hypertension
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Selective laser trabeculoplasty is a relatively new therapeutic alternative for the management of open angle glaucoma and ocular hypertension. On the other hand, medical treatment has robust data supporting its efficacy and has progressed in last decades with the introduction of prostaglandin analogues. To compare these two therapies, we searched Epistemonikos database, which is maintained by screening 30 databases, and identified four systematic reviews including four randomized and one non-randomized clinical trial. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded that selective laser trabeculoplasty leads to a smaller absolute intraocular pressure reduction than medical treatment. However, it is not clear if there are differences in treatment success rate or need of additional antiglaucomatous interventions, because the quality of the evidence is low.
 Autores:
Efraín Pérez[1,3], Gabriel Rada[2,3,4,5,6], Eugenio Maul[3,7]
Autores:
Efraín Pérez[1,3], Gabriel Rada[2,3,4,5,6], Eugenio Maul[3,7]

Citación: Pérez E, Rada G, Maul E. Selective laser trabeculoplasty compared with medical treatment for the initial management of open angle glaucoma or ocular hypertension. Medwave 2015;15(Suppl 3):e6337 doi: 10.5867/medwave.2015.6337
Fecha de publicación: 16/12/2015

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 American Academy of Ophthalmology Glaucoma P. Preferred Practice Pattern Guidelines. Primary Open-Angle Glaucoma. American Academy of Ophthalmology; 2010:1-57.
American Academy of Ophthalmology Glaucoma P. Preferred Practice Pattern Guidelines. Primary Open-Angle Glaucoma. American Academy of Ophthalmology; 2010:1-57.  Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma. A pilot study. Arch Ophthalmol. 1979 Feb;97(2):319-22. | PubMed |
Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma. A pilot study. Arch Ophthalmol. 1979 Feb;97(2):319-22. | PubMed | The Glaucoma Laser Trial (GLT). 2. Results of argon laser trabeculoplasty versus topical medicines. The Glaucoma Laser Trial Research Group. Ophthalmology. 1990 Nov;97(11):1403-13. | PubMed |
The Glaucoma Laser Trial (GLT). 2. Results of argon laser trabeculoplasty versus topical medicines. The Glaucoma Laser Trial Research Group. Ophthalmology. 1990 Nov;97(11):1403-13. | PubMed | Camras CB. Comparison of latanoprost and timolol in patients with ocular hypertension and glaucoma: a six-month masked, multicenter trial in the United States. The United States Latanoprost Study Group. Ophthalmology. 1996 Jan;103(1):138-47. | PubMed |
Camras CB. Comparison of latanoprost and timolol in patients with ocular hypertension and glaucoma: a six-month masked, multicenter trial in the United States. The United States Latanoprost Study Group. Ophthalmology. 1996 Jan;103(1):138-47. | PubMed | Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009 Feb;116(2):191-9. | CrossRef | PubMed |
Okeke CO, Quigley HA, Jampel HD, Ying GS, Plyler RJ, Jiang Y, et al. Adherence with topical glaucoma medication monitored electronically the Travatan Dosing Aid study. Ophthalmology. 2009 Feb;116(2):191-9. | CrossRef | PubMed | Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res. 1995 Apr;60(4):359-71. | PubMed |
Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res. 1995 Apr;60(4):359-71. | PubMed | Wong MO, Lee JW, Choy BN, Chan JC, Lai JS. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol. 2015 Jan-Feb;60(1):36-50. | CrossRef | PubMed |
Wong MO, Lee JW, Choy BN, Chan JC, Lai JS. Systematic review and meta-analysis on the efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol. 2015 Jan-Feb;60(1):36-50. | CrossRef | PubMed | Avery N, Ang GS, Nicholas S, Wells A. Repeatability of primary selective laser trabeculoplasty in patients with primary open-angle glaucoma. Int Ophthalmol. 2013 Oct;33(5):501-6. | CrossRef | PubMed |
Avery N, Ang GS, Nicholas S, Wells A. Repeatability of primary selective laser trabeculoplasty in patients with primary open-angle glaucoma. Int Ophthalmol. 2013 Oct;33(5):501-6. | CrossRef | PubMed | Russo V, Barone A, Cosma A, Stella A, Delle Noci N. Selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with uncontrolled open-angle glaucoma. Eur J Ophthalmol. 2009 May-Jun;19(3):429-34. | PubMed |
Russo V, Barone A, Cosma A, Stella A, Delle Noci N. Selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with uncontrolled open-angle glaucoma. Eur J Ophthalmol. 2009 May-Jun;19(3):429-34. | PubMed | Samples JR, Singh K, Lin SC, Francis BA, Hodapp E, Jampel HD, Smith SD. Laser trabeculoplasty for open-angle glaucoma: a report by the american academy of ophthalmology. Ophthalmology. 2011 Nov;118(11):2296-302.
| CrossRef | PubMed |
Samples JR, Singh K, Lin SC, Francis BA, Hodapp E, Jampel HD, Smith SD. Laser trabeculoplasty for open-angle glaucoma: a report by the american academy of ophthalmology. Ophthalmology. 2011 Nov;118(11):2296-302.
| CrossRef | PubMed | Li X, Wang W, Zhang X. Meta-analysis of selective laser trabeculoplasty versus topical medication in the treatment of open-angle glaucoma. BMC Ophthalmol. 2015 Aug 19;15:107. | CrossRef | PubMed |
Li X, Wang W, Zhang X. Meta-analysis of selective laser trabeculoplasty versus topical medication in the treatment of open-angle glaucoma. BMC Ophthalmol. 2015 Aug 19;15:107. | CrossRef | PubMed | McAlinden C. Selective laser trabeculoplasty (SLT) vs other treatment modalities for glaucoma: systematic review. Eye (Lond). 2014 Mar;28(3):249-58. | CrossRef | PubMed |
McAlinden C. Selective laser trabeculoplasty (SLT) vs other treatment modalities for glaucoma: systematic review. Eye (Lond). 2014 Mar;28(3):249-58. | CrossRef | PubMed | Zhang W, Zhou T, Wu T, Gao X, Peng Y, Xu C, Chen Q,et al. Retrograde Intrarenal Surgery Versus Percutaneous Nephrolithotomy Versus Extracorporeal Shockwave Lithotripsy for Treatment of Lower Pole Renal Stones: A Meta-Analysis and Systematic Review. J Endourol. 2015 Jul;29(7):745-59. | CrossRef | PubMed |
Zhang W, Zhou T, Wu T, Gao X, Peng Y, Xu C, Chen Q,et al. Retrograde Intrarenal Surgery Versus Percutaneous Nephrolithotomy Versus Extracorporeal Shockwave Lithotripsy for Treatment of Lower Pole Renal Stones: A Meta-Analysis and Systematic Review. J Endourol. 2015 Jul;29(7):745-59. | CrossRef | PubMed | Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2012 Sep;21(7):460-8. | CrossRef | PubMed |
Katz LJ, Steinmann WC, Kabir A, Molineaux J, Wizov SS, Marcellino G, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma. 2012 Sep;21(7):460-8. | CrossRef | PubMed | Lai JS, Chua JK, Tham CC, Lam DS. Five-year follow up of selective laser trabeculoplasty in Chinese eyes. Clin Experiment phthalmol. 2004 Aug;32(4):368-72.
| PubMed |
Lai JS, Chua JK, Tham CC, Lam DS. Five-year follow up of selective laser trabeculoplasty in Chinese eyes. Clin Experiment phthalmol. 2004 Aug;32(4):368-72.
| PubMed | Nagar M, Luhishi E, Shah N. Intraocular pressure control and fluctuation: the effect of treatment with selective laser trabeculoplasty. Br J Ophthalmol. 2009 Apr;93(4):497-501. | CrossRef | PubMed |
Nagar M, Luhishi E, Shah N. Intraocular pressure control and fluctuation: the effect of treatment with selective laser trabeculoplasty. Br J Ophthalmol. 2009 Apr;93(4):497-501. | CrossRef | PubMed | Nagar M, Ogunyomade A, O'Brart DP, Howes F, Marshall J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005 Nov;89(11):1413-7. | PubMed |
Nagar M, Ogunyomade A, O'Brart DP, Howes F, Marshall J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005 Nov;89(11):1413-7. | PubMed | McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006 Apr;15(2):124-30. | PubMed |
McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006 Apr;15(2):124-30. | PubMed | Peng W, Zhong X, Yu M. [Meta-analysis of randomized controlled trials comparing selective laser trabeculoplasty with prostaglandin analogue in the primary treatment of open-angle glaucoma or ocular hypertention]. Zhonghua Yan Ke Za Zhi. 2014 May;50(5):343-8. | PubMed |
Peng W, Zhong X, Yu M. [Meta-analysis of randomized controlled trials comparing selective laser trabeculoplasty with prostaglandin analogue in the primary treatment of open-angle glaucoma or ocular hypertention]. Zhonghua Yan Ke Za Zhi. 2014 May;50(5):343-8. | PubMed | Bhargava JS, Patel B, Foss AJ, Avery AJ, King AJ. Views of glaucoma patients on aspects of their treatment: an assessment of patient preference by conjoint analysis. Invest Ophthalmol Vis Sci. 2006 Jul;47(7):2885-8.
| PubMed |
Bhargava JS, Patel B, Foss AJ, Avery AJ, King AJ. Views of glaucoma patients on aspects of their treatment: an assessment of patient preference by conjoint analysis. Invest Ophthalmol Vis Sci. 2006 Jul;47(7):2885-8.
| PubMed | Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M; Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002 Oct;120(10):1268-79. | PubMed |
Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M; Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002 Oct;120(10):1268-79. | PubMed | Ting NS, Li Yim JF, Ng JY. Different strategies and cost-effectiveness in the treatment of primary open angle glaucoma. Clinicoecon Outcomes Res. 2014 Dec 4;6:523-30. | CrossRef | PubMed |
Ting NS, Li Yim JF, Ng JY. Different strategies and cost-effectiveness in the treatment of primary open angle glaucoma. Clinicoecon Outcomes Res. 2014 Dec 4;6:523-30. | CrossRef | PubMed | Stein JD, Kim DD, Peck WW, Giannetti SM, Hutton DW. Cost-effectiveness of medications compared with laser trabeculoplasty inpatients with newly diagnosed open-angle glaucoma. Arch Ophthalmol. 2012 Apr;130(4):497-505. | CrossRef | PubMed |
Stein JD, Kim DD, Peck WW, Giannetti SM, Hutton DW. Cost-effectiveness of medications compared with laser trabeculoplasty inpatients with newly diagnosed open-angle glaucoma. Arch Ophthalmol. 2012 Apr;130(4):497-505. | CrossRef | PubMed | No authors listed [The Japan Glaucoma Society Guidelines for Glaucoma (2nd edition)]. Nippon Ganka Gakkai Zasshi. 2006 Oct;110 10):778-814 | PubMed |
No authors listed [The Japan Glaucoma Society Guidelines for Glaucoma (2nd edition)]. Nippon Ganka Gakkai Zasshi. 2006 Oct;110 10):778-814 | PubMed | Tuulonen A, Airaksinen PJ, Erola E, Forsman E, Friberg K, Kaila M, et al. The Finnish evidence-based guideline for open-angle glaucoma. Acta Ophthalmol Scand. 2003 Feb;81(1):3-18. | PubMed |
Tuulonen A, Airaksinen PJ, Erola E, Forsman E, Friberg K, Kaila M, et al. The Finnish evidence-based guideline for open-angle glaucoma. Acta Ophthalmol Scand. 2003 Feb;81(1):3-18. | PubMed | Nhmrc. Guidelines for the Screening, Prognosis, Diagnosis, Management and Prevention of Glaucoma [on line]. | Link |
Nhmrc. Guidelines for the Screening, Prognosis, Diagnosis, Management and Prevention of Glaucoma [on line]. | Link | Canadian Ophthalmological Society Glaucoma Clinical Practice Guideline Expert Committee; Canadian Ophthalmological Society. Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of glaucoma in the adult eye. Can J Ophthalmol. 2009;44 Suppl 1:S7-93.
| CrossRef | PubMed |
Canadian Ophthalmological Society Glaucoma Clinical Practice Guideline Expert Committee; Canadian Ophthalmological Society. Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of glaucoma in the adult eye. Can J Ophthalmol. 2009;44 Suppl 1:S7-93.
| CrossRef | PubMed |