 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
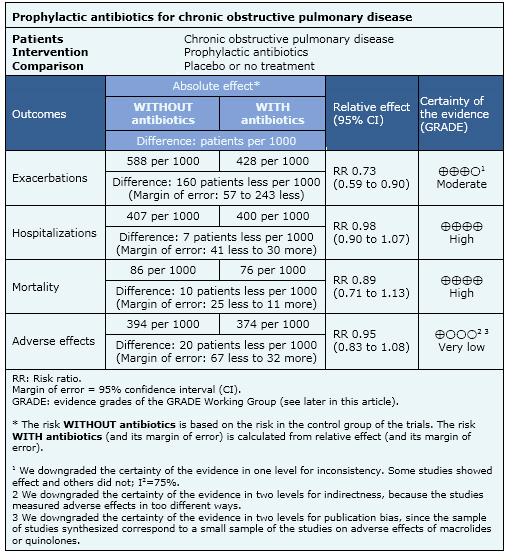
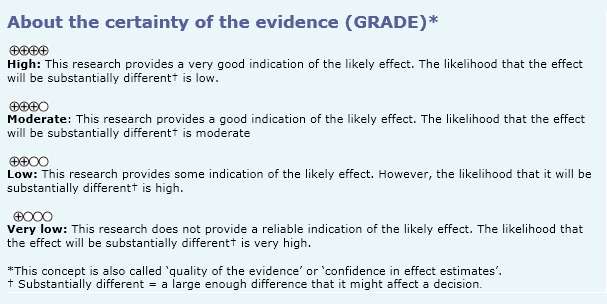
Bacterial infections are one of the main causes of chronic obstructive pulmonary disease exacerbation, so the use of prophylactic antibiotics, especially macrolides, has been proposed in these patients. However, it is unclear whether antibiotics use is worth the risk and cost. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified five systematic reviews including eight randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded prophylactic antibiotics probably decrease exacerbations in chronic obstructive pulmonary disease, but have no effect on hospitalizations or mortality.
Exacerbations contribute substantially to morbidity and mortality in patients with chronic obstructive pulmonary disease. Since bacterial infections play a major etiologic role it has been proposed prolonged use of prophylactic antibiotics may reduce exacerbations. Apart from their antimicrobial role, it has been postulated that some antibiotics such as macrolides may also have an anti-inflammatory effect. On the other hand, the use of prophylactic antibiotics is associated with costs and adverse effects at both individual and population level.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5], considering 10 primary studies [6],[7],[8],[9],[10],[11],[12],[13],[14],[15], including eight randomized controlled trials [6],[7],[8],[9],[10],[12],[13],[14]. This table and the summary in general are based on the latter. |
|
What types of patients were included |
All studies included patients with FEV1/FVC <70% with moderate to very severe disease. Three studies included patients with a history of exacerbations in the previous months [6],[10],[13]. |
|
What types of interventions were included |
The antibiotic used was a macrolide in seven studies; azithromycin [6],[8],[10], clarithromycin [7] and erythromycin 9],[12],[14]; and a quinolone in only one study (moxifloxacin) [13]. Prophylactic antibiotics were administered continuously in five studies [6],[7],[9],[12],[14] and intermittently or pulsed in the other three [8],[10],[13]. Concomitant therapy was the following: inhaled corticosteroids alone in two studies [7],[12], theophylline plus inhaled anticholinergics in one study [14], inhaled corticosteroids plus inhaled anticholinergics and beta2 agonists in one study [6], inhaled corticosteroids plus inhaled beta2 agonists, inhaled anticholinergics and theophylline in one study [9], and concomitant therapy was not reported in three studies [8],[10],[13]. Seven studies used a placebo for comparison [6],[7],[9],[12],[13],[14]. |
|
What types of outcomes |
Different systematic reviews performed meta-analysis of the following outcomes:
|
Information on the effects of prophylactic antibiotics in chronic obstructive pulmonary disease is based on eight randomized trials that included 3,315 patients. It was possible to obtain information on exacerbations in seven studies [6],[7],[8],[9],[12],[13],[14], on hospitalizations in three [6],[8],[13], on mortality in four [6],[8],[10],[13] and on adverse effects in seven [6],[7],[8],[9],[12],[13],[14].
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
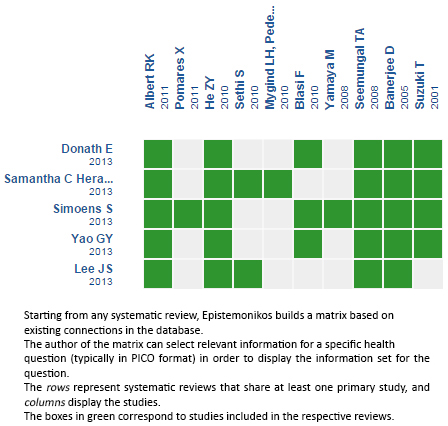
Follow the link to access the interactive version: Prophylactic antibiotic therapy for chronic obstructive pulmonary disease
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Bacterial infections are one of the main causes of chronic obstructive pulmonary disease exacerbation, so the use of prophylactic antibiotics, especially macrolides, has been proposed in these patients. However, it is unclear whether antibiotics use is worth the risk and cost. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified five systematic reviews including eight randomized trials. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded prophylactic antibiotics probably decrease exacerbations in chronic obstructive pulmonary disease, but have no effect on hospitalizations or mortality.
 Autores:
Alex Arenas[1,2], Gabriel Rada[1,2,3,4,5]
Autores:
Alex Arenas[1,2], Gabriel Rada[1,2,3,4,5]

Citación: Arenas A, Rada G. Are prophylactic antibiotics useful in chronic obstructive pulmonary disease? . Medwave 2015;15(Suppl 3):e6309 doi: 10.5867/medwave.2015.6309
Fecha de publicación: 10/11/2015

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Donath E, Chaudhry A, Hernandez-Aya LF, Lit L. A meta-analysis on the prophylactic use of macrolide antibiotics for the prevention of disease exacerbations in patients with Chronic Obstructive Pulmonary Disease. Respir Med. 2013 Sep;107(9):1385-92. | CrossRef | PubMed |
Donath E, Chaudhry A, Hernandez-Aya LF, Lit L. A meta-analysis on the prophylactic use of macrolide antibiotics for the prevention of disease exacerbations in patients with Chronic Obstructive Pulmonary Disease. Respir Med. 2013 Sep;107(9):1385-92. | CrossRef | PubMed | Lee JS, Park DA, Hong Y, Jo KW, Lee SW, Huh JW, et al. Systematic review and meta-analysis of prophylactic antibiotics in COPD and/or chronic bronchitis. Int J Tuberc Lung Dis. 2013 Feb;17(2):153-62. | CrossRef | PubMed |
Lee JS, Park DA, Hong Y, Jo KW, Lee SW, Huh JW, et al. Systematic review and meta-analysis of prophylactic antibiotics in COPD and/or chronic bronchitis. Int J Tuberc Lung Dis. 2013 Feb;17(2):153-62. | CrossRef | PubMed | Herath SC, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2013 Nov 28;11:CD009764. | CrossRef | PubMed |
Herath SC, Poole P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2013 Nov 28;11:CD009764. | CrossRef | PubMed | Simoens S, Laekeman G, Decramer M. Preventing COPD exacerbations with macrolides: a review and budget impact analysis. Respir Med. 2013
May;107(5):637-48. | CrossRef | PubMed |
Simoens S, Laekeman G, Decramer M. Preventing COPD exacerbations with macrolides: a review and budget impact analysis. Respir Med. 2013
May;107(5):637-48. | CrossRef | PubMed | Yao GY, Ma YL, Zhang MQ, Gao ZC. Macrolide therapy decreases chronic obstructive pulmonary disease exacerbation: a meta-analysis. Respiration. 2013;86(3):254-60. | CrossRef | PubMed |
Yao GY, Ma YL, Zhang MQ, Gao ZC. Macrolide therapy decreases chronic obstructive pulmonary disease exacerbation: a meta-analysis. Respiration. 2013;86(3):254-60. | CrossRef | PubMed | Albert RK, Connett J, Bailey WC, Casaburi R, Cooper JA Jr, Criner GJ,et al. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011 Aug 25;365(8):689-98.
| CrossRef | PubMed |
Albert RK, Connett J, Bailey WC, Casaburi R, Cooper JA Jr, Criner GJ,et al. Azithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011 Aug 25;365(8):689-98.
| CrossRef | PubMed | Banerjee D, Khair OA, Honeybourne D. The effect of oral clarithromycin on health status and sputum bacteriology in stable COPD. Respir Med. 2005 Feb;99(2):208-15. | PubMed |
Banerjee D, Khair OA, Honeybourne D. The effect of oral clarithromycin on health status and sputum bacteriology in stable COPD. Respir Med. 2005 Feb;99(2):208-15. | PubMed | Blasi F, Bonardi D, Aliberti S, Tarsia P, Confalonieri M, Amir O, et al. Long-term azithromycin use in patients with chronic obstructive pulmonary disease and tracheostomy. Pulm Pharmacol Ther. 2010 Jun;23(3):200-7. | CrossRef | PubMed |
Blasi F, Bonardi D, Aliberti S, Tarsia P, Confalonieri M, Amir O, et al. Long-term azithromycin use in patients with chronic obstructive pulmonary disease and tracheostomy. Pulm Pharmacol Ther. 2010 Jun;23(3):200-7. | CrossRef | PubMed | He ZY, Ou LM, Zhang JQ, Bai J, Liu GN, Li MH, Deng JM, MacNee W, Zhong XN. Effect of 6 months of erythromycin treatment on inflammatory cells in induced sputum and exacerbations in chronic obstructive pulmonary disease. Respiration. 2010;80(6):445-52. | CrossRef | PubMed |
He ZY, Ou LM, Zhang JQ, Bai J, Liu GN, Li MH, Deng JM, MacNee W, Zhong XN. Effect of 6 months of erythromycin treatment on inflammatory cells in induced sputum and exacerbations in chronic obstructive pulmonary disease. Respiration. 2010;80(6):445-52. | CrossRef | PubMed | Mygind LH, Pedersen C, Vestbo J, Christensen JJ, Frimodt-Moller N, Kristiansen IS, et al. A randomised, placebo-controlled 3 years study of prophylactic azithromycin in 575 patients with chronic obstructive pulmonary disease. European Respiratory Society Annual Congress. 2010 2010. | Link |
Mygind LH, Pedersen C, Vestbo J, Christensen JJ, Frimodt-Moller N, Kristiansen IS, et al. A randomised, placebo-controlled 3 years study of prophylactic azithromycin in 575 patients with chronic obstructive pulmonary disease. European Respiratory Society Annual Congress. 2010 2010. | Link | Pomares X, Montón C, Espasa M, Casabon J, Monsó E, Gallego M. Long-term azithromycin therapy in patients with severe COPD and repeated exacerbations. Int J Chron Obstruct Pulmon Dis. 2011;6:449-56. | CrossRef | PubMed |
Pomares X, Montón C, Espasa M, Casabon J, Monsó E, Gallego M. Long-term azithromycin therapy in patients with severe COPD and repeated exacerbations. Int J Chron Obstruct Pulmon Dis. 2011;6:449-56. | CrossRef | PubMed | Seemungal TA, Wilkinson TM, Hurst JR, Perera WR, Sapsford RJ, Wedzicha JA. Long-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med. 2008 Dec 1;178(11):1139-47. | CrossRef | PubMed |
Seemungal TA, Wilkinson TM, Hurst JR, Perera WR, Sapsford RJ, Wedzicha JA. Long-term erythromycin therapy is associated with decreased chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med. 2008 Dec 1;178(11):1139-47. | CrossRef | PubMed | Sethi S, Jones PW, Theron MS, Miravitlles M, Rubinstein E, Wedzicha JA, Wilson R; PULSE Study group. Pulsed moxifloxacin for the prevention of exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. Respir Res. 2010 Jan 28;11:10. | CrossRef | PubMed |
Sethi S, Jones PW, Theron MS, Miravitlles M, Rubinstein E, Wedzicha JA, Wilson R; PULSE Study group. Pulsed moxifloxacin for the prevention of exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. Respir Res. 2010 Jan 28;11:10. | CrossRef | PubMed | Suzuki T, Yanai M, Yamaya M, Satoh-Nakagawa T, Sekizawa K, Ishida S, Sasaki H. Erythromycin and common cold in COPD. Chest. 2001 Sep;120(3):730-3. | PubMed |
Suzuki T, Yanai M, Yamaya M, Satoh-Nakagawa T, Sekizawa K, Ishida S, Sasaki H. Erythromycin and common cold in COPD. Chest. 2001 Sep;120(3):730-3. | PubMed | Yamaya M, Azuma A, Tanaka H, Takizawa H, Chida K, Taguchi Y, et al. Inhibitory effects of macrolide antibiotics on exacerbations and hospitalization in chronic obstructive pulmonary disease in Japan: a retrospective multicenter analysis. J Am Geriatr Soc. 2008 Jul;56(7):1358-60. | CrossRef | PubMed |
Yamaya M, Azuma A, Tanaka H, Takizawa H, Chida K, Taguchi Y, et al. Inhibitory effects of macrolide antibiotics on exacerbations and hospitalization in chronic obstructive pulmonary disease in Japan: a retrospective multicenter analysis. J Am Geriatr Soc. 2008 Jul;56(7):1358-60. | CrossRef | PubMed | Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P, et al. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015 Apr;147(4):894-942. | CrossRef | PubMed |
Criner GJ, Bourbeau J, Diekemper RL, Ouellette DR, Goodridge D, Hernandez P, et al. Prevention of acute exacerbations of COPD: American College of Chest Physicians and Canadian Thoracic Society Guideline. Chest. 2015 Apr;147(4):894-942. | CrossRef | PubMed | Hansen M, Thorning S, Aronson J, Beller E, Glasziou P, Hoffmann T, et al. Adverse events in patients taking macrolide antibiotics versus placebo for any indication (Protocol). Cochrane Database of Systematic Reviews. 2015;8:8. | CrossRef |
Hansen M, Thorning S, Aronson J, Beller E, Glasziou P, Hoffmann T, et al. Adverse events in patients taking macrolide antibiotics versus placebo for any indication (Protocol). Cochrane Database of Systematic Reviews. 2015;8:8. | CrossRef |