 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
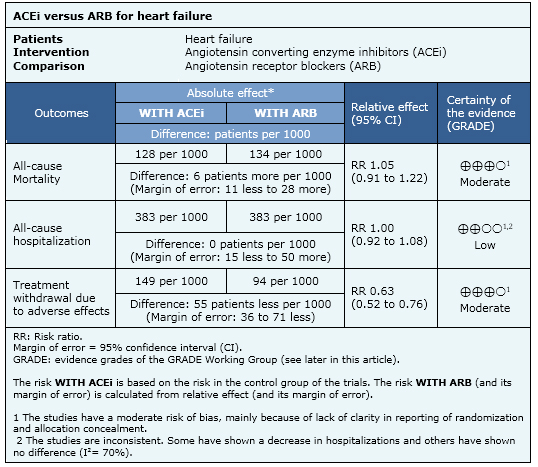
Angiotensin receptor blockers are usually considered as equivalent to angiotensin converting enzyme inhibitors for patients with heart failure and low-ejection fraction. Some guidelines even recommend the former as first line treatment given their better adverse effects profile. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified four systematic reviews including eight pertinent randomized controlled trials. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded angiotensin receptor blockers and angiotensin converting enzyme inhibitors probably have a similar effect on mortality, and they might be equivalent in reducing hospitalization risk too. Treatment withdrawal due to adverse effects is probably lower with angiotensin receptor blockers than with angiotensin converting enzyme inhibitors.
Angiotensin converting enzyme inhibitors decrease morbidity and mortality in patients with heart failure and systolic dysfunction. It is generally accepted angiotensin receptor blockers have similar benefits, but recommendations vary in the different guidelines, ranging from using them as first-line treatment to reserve them to patients intolerant to angiotensin converting enzyme inhibitors.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] including eight randomized controlled trials [5],[6],[7],[8],[9],[10],[11],[12]. |
|
What types of patients were included |
The average age between studies ranged from 56 to 74 years. All studies included patients with heart failure of any etiology, and the most common cause was ischemic. No study included NYHA functional class I patients. All studies restricted inclusion to low ejection fraction patients; two studies required ejection fraction lower than 45% [8],[9], five < 40% [5],[6],[7],[10],[11] and one < 35% [12]. |
|
What types of interventions were included |
The angiotensin converting enzyme inhibitors used in the studies was enalapril in five [5],[6],[8],[9],[12], captopril in two [7],[11] and lisinopril in one [10]. The Angiotensin receptor blocker used as comparator was losartan in four studies [7],[9],[11],[12], valsartan in two [8],[10], telmisartan in one [6] and candesartan in one [5]. |
|
What types of outcomes were measured |
All-cause mortality or cardiovascular death, all-cause hospitalization, treatment withdrawal, quality of life, exercise tolerance, neurohumoral biomarkers and echocardiographic parameters. |
The information on the effects of carvedilol is based on eight randomized controlled trials including 5201 patients. All studies reported mortality and three reported all-cause hospitalization, [5],[7],[11].

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
Follow the link to access the interactive version Angiotensin-receptor blockers versus angiotensin converting enzyme inhibitors for heart failure
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

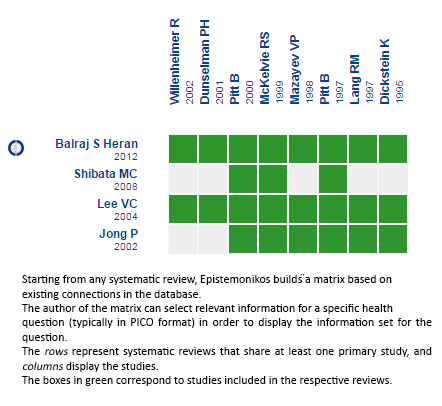 Matrix of evidence
Matrix of evidence
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Angiotensin receptor blockers are usually considered as equivalent to angiotensin converting enzyme inhibitors for patients with heart failure and low-ejection fraction. Some guidelines even recommend the former as first line treatment given their better adverse effects profile. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified four systematic reviews including eight pertinent randomized controlled trials. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded angiotensin receptor blockers and angiotensin converting enzyme inhibitors probably have a similar effect on mortality, and they might be equivalent in reducing hospitalization risk too. Treatment withdrawal due to adverse effects is probably lower with angiotensin receptor blockers than with angiotensin converting enzyme inhibitors.
 Autores:
Carmen Rain[1,5], Gabriel Rada[1,2,3,4,5]
Autores:
Carmen Rain[1,5], Gabriel Rada[1,2,3,4,5]

Citación: Rain C, Rada G. Is there any difference between angiotensin converting enzyme inhibitors and angiotensin receptor blockers for heart failure?. Medwave 2015 Jul;15(Suppl 1):e6177 doi: 10.5867/medwave.2015.6177
Fecha de publicación: 6/7/2015

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Lee VC, Rhew DC, Dylan M, Badamgarav E, Braunstein GD, Weingarten SR. Meta-analysis: angiotensin-receptor blockers in chronic heart failure and high-risk acute myocardial infarction. Ann Intern Med. 2004 Nov 2;141(9):693-704. | PubMed |
Lee VC, Rhew DC, Dylan M, Badamgarav E, Braunstein GD, Weingarten SR. Meta-analysis: angiotensin-receptor blockers in chronic heart failure and high-risk acute myocardial infarction. Ann Intern Med. 2004 Nov 2;141(9):693-704. | PubMed | Jong P, Demers C, McKelvie RS, Liu PP. Angiotensin receptor blockers in heart failure: meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2002 Feb 6;39(3):463-70. | PubMed |
Jong P, Demers C, McKelvie RS, Liu PP. Angiotensin receptor blockers in heart failure: meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2002 Feb 6;39(3):463-70. | PubMed | Shibata MC, Tsuyuki RT, Wiebe N. The effects of angiotensin-receptor blockers on mortality and morbidity in heart failure: a systematic review. Int J Clin Pract. 2008 Sep;62(9):1397-402. | CrossRef | PubMed |
Shibata MC, Tsuyuki RT, Wiebe N. The effects of angiotensin-receptor blockers on mortality and morbidity in heart failure: a systematic review. Int J Clin Pract. 2008 Sep;62(9):1397-402. | CrossRef | PubMed | Heran BS, Musini VM, Bassett K, Taylor RS, Wright JM. Angiotensin receptor blockers for heart failure. Cochrane Database Syst Rev. 2012 Apr 18;4:CD003040. | CrossRef | PubMed |
Heran BS, Musini VM, Bassett K, Taylor RS, Wright JM. Angiotensin receptor blockers for heart failure. Cochrane Database Syst Rev. 2012 Apr 18;4:CD003040. | CrossRef | PubMed | McKelvie RS, Yusuf S, Pericak D, Avezum A, Burns RJ, Probstfield J, et al. Comparison of
candesartan, enalapril, and their combination in congestive heart failure: randomized evaluation of strategies for left ventricular dysfunction (RESOLVD) pilot study. The RESOLVD Pilot Study Investigators. Circulation. 1999 Sep 7;100(10):1056-64. | PubMed |
McKelvie RS, Yusuf S, Pericak D, Avezum A, Burns RJ, Probstfield J, et al. Comparison of
candesartan, enalapril, and their combination in congestive heart failure: randomized evaluation of strategies for left ventricular dysfunction (RESOLVD) pilot study. The RESOLVD Pilot Study Investigators. Circulation. 1999 Sep 7;100(10):1056-64. | PubMed | Dunselman PH; Replacement of Angiotensin Converting Enzyme Inhibition (REPLACE) Investigators. Effects of the replacement of the angiotensin converting enzyme inhibitor enalapril by the angiotensin II receptor blocker telmisartan in patients with congestive heart failure. The replacement of angiotensin converting enzyme inhibition (REPLACE) investigators. Int J Cardiol. 2001 Feb;77(2-3):131-8; discussion 139-40. | PubMed |
Dunselman PH; Replacement of Angiotensin Converting Enzyme Inhibition (REPLACE) Investigators. Effects of the replacement of the angiotensin converting enzyme inhibitor enalapril by the angiotensin II receptor blocker telmisartan in patients with congestive heart failure. The replacement of angiotensin converting enzyme inhibition (REPLACE) investigators. Int J Cardiol. 2001 Feb;77(2-3):131-8; discussion 139-40. | PubMed | Pitt B, Segal R, Martinez FA, Meurers G, Cowley AJ, Thomas I, et al. Randomised trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE). Lancet. 1997 Mar 15;349(9054):747-52. | PubMed |
Pitt B, Segal R, Martinez FA, Meurers G, Cowley AJ, Thomas I, et al. Randomised trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE). Lancet. 1997 Mar 15;349(9054):747-52. | PubMed | Willenheimer R, Helmers C, Pantev E, Rydberg E, Löfdahl P, Gordon A. Safety and efficacy of valsartan versus enalapril in heart failure patients. Int J Cardiol. 2002 Oct;85(2-3):261-70. | PubMed |
Willenheimer R, Helmers C, Pantev E, Rydberg E, Löfdahl P, Gordon A. Safety and efficacy of valsartan versus enalapril in heart failure patients. Int J Cardiol. 2002 Oct;85(2-3):261-70. | PubMed | Lang RM, Elkayam U, Yellen LG, Krauss D, McKelvie RS, Vaughan DE, et al. Comparative effects of losartan and enalapril on exercise capacity and clinical status in patients with heart failure. The Losartan Pilot Exercise Study Investigators. J Am Coll Cardiol. 1997 Oct;30(4):983-91. | PubMed |
Lang RM, Elkayam U, Yellen LG, Krauss D, McKelvie RS, Vaughan DE, et al. Comparative effects of losartan and enalapril on exercise capacity and clinical status in patients with heart failure. The Losartan Pilot Exercise Study Investigators. J Am Coll Cardiol. 1997 Oct;30(4):983-91. | PubMed | Mazayev VP, Fomina IG, Kazakov EN, Sulimov VA, Zvereva TV, Lyusov VA, et al. Valsartan in heart
failure patients previously untreated with an ACE inhibitor. Int J Cardiol. 1998 Aug;65(3):239-46. | PubMed |
Mazayev VP, Fomina IG, Kazakov EN, Sulimov VA, Zvereva TV, Lyusov VA, et al. Valsartan in heart
failure patients previously untreated with an ACE inhibitor. Int J Cardiol. 1998 Aug;65(3):239-46. | PubMed | Pitt B, Poole-Wilson PA, Segal R, Martinez FA, Dickstein K, Camm AJ, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial--the Losartan Heart Failure Survival Study ELITE II. Lancet. 2000 May 6;355(9215):1582-7. | PubMed |
Pitt B, Poole-Wilson PA, Segal R, Martinez FA, Dickstein K, Camm AJ, et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial--the Losartan Heart Failure Survival Study ELITE II. Lancet. 2000 May 6;355(9215):1582-7. | PubMed | Dickstein K, Chang P, Willenheimer R, Haunsø S, Remes J, Hall C, et al. Comparison of the effects of losartan and enalapril on clinical status and exercise performance in patients with moderate or severe chronic heart failure. J Am Coll Cardiol. 1995 Aug;26(2):438-45. | PubMed |
Dickstein K, Chang P, Willenheimer R, Haunsø S, Remes J, Hall C, et al. Comparison of the effects of losartan and enalapril on clinical status and exercise performance in patients with moderate or severe chronic heart failure. J Am Coll Cardiol. 1995 Aug;26(2):438-45. | PubMed | Arnold JM, Liu P, Demers C, Dorian P, Giannetti N, Haddad H, et al. Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol. 2006 Jan;22(1):23-45. | PubMed |
Arnold JM, Liu P, Demers C, Dorian P, Giannetti N, Haddad H, et al. Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol. 2006 Jan;22(1):23-45. | PubMed | Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194. | CrossRef | PubMed |
Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194. | CrossRef | PubMed | McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed |
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327. | CrossRef | PubMed |
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327. | CrossRef | PubMed |