 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: High flow nasal cannula, Respiration, Artificial, Respiratory Therapy, Oxygen, Oxygen Inhalation Therapy, bronchiolitis, high flow oxygen delivery system
Introduction
Oxygen therapy through a high-flow nasal cannula is thought to improve the work of breathing and the comfort of patients with acute bronchiolitis. It is widely used in hospital wards and critical care of pediatric patients. However, there is uncertainty on the magnitude of the effect on critical and important outcomes in these patients.
Objectives
The objective of this review is to evaluate the available evidence on the use of oxygen administered through high-flow cannula versus low-flow oxygen for the treatment of acute bronchiolitis in children under two years of age.
Methodology
We carried out a systematic review and a meta-analysis following the PRISMA standards for reporting. The search was carried out in electronic databases by two researchers independently. The evidence was summarized using the GRADE methodology.
Results
Six randomized and non-randomized clinical trials were included, including 1867 individuals younger than 24 months of age with acute bronchiolitis in pediatric emergency, hospitalization, and intensive care services. Mortality was not reported in the included studies. Treatment failure occurred in 108/933 in the high flow group and 233/934 in the low flow group (relative risk: 0.46; 95% confidence interval: 0.35 to 0.62), which shows 11.7% less treatment failure (95% confidence interval between 7.9% and 14.5% less) in the high flow group with a number needed to treat of 7.5 (95% confidence interval 6 to 10) with moderate certainty in the evidence.
Conclusion
The use of humidified and heated oxygen with high flow compared to oxygen at low flow is probably associated with decreased treatment failure in children younger than two years with acute bronchiolitis. There is uncertainty about the effect on hospitalization days and clinical progression.
Main messages
|
Bronchiolitis is the most common lower respiratory tract infection in infants and represents an important cause of hospitalization in this age group. It is estimated that 11 to 12% of infants are affected in the first year of life, and 1 to 2% of them require hospitalization [1]. Of those admitted to emergency rooms and hospitalization, 10% of previously healthy children and 36% of those with comorbidities will require admission to a pediatric intensive care unit. This group of children has an associated mortality of 1% [2],[3].
Treatment by traditional low-flow oxygen therapy with a mask or nasal cannula has limitations due to the application of dry oxygen and the impossibility of using high flow [4],[5].
When this therapeutic approach is ineffective, noninvasive ventilation strategies are used, mainly through continuous positive airway pressure.
The application of noninvasive ventilation presents difficulties in small infants, especially those weighing less than 7 kg. In addition to the technical limitations related to the interface used, the flows generated, and the equipment available, continuous positive airway pressure/noninvasive ventilation can be challenging, requires highly trained nursing and medical staff, is not always tolerated by patients and, therefore, in the past, has been restricted to the intensive care unit [6],[7].
Heated humidified high-flow nasal cannula oxygen therapy provides heated and humidified gas at high flow rates to improve breathing and patient comfort. The addition of heat and high levels of humidification allows high flows of air and oxygen, achieving concentrations close to 100%. This requires systems with appropriate oxygen mixers and flowmeters. These high-flow oxygenation systems are convenient, simple, and have the advantage of not interfering with feeding [8],[9].
In pediatric wards, high-flow oxygen therapy through a nasal cannula has become a widely used new method to provide respiratory support for respiratory diseases in infants and newborns. Clinical studies in infants with acute bronchiolitis show benefits in some surrogate outcomes (respiratory frequency, days of hospitalization, among others) [10].
We set out to conduct a systematic review to synthesize the available evidence on the use of high-flow nasal cannula oxygen compared to low-flow oxygen for the treatment of acute bronchiolitis in children under two years of age.
A multidisciplinary team, free of conflicts of interest, was formed to conduct a systematic review of the use of high-flow cannulae versus oxygen administered through low-flow systems to treat acute bronchiolitis in the population of children under two years of age.
This study was conducted following PRISMA (Preferred Reported Items in Systematic Reviews and Meta-analysis) guidelines for the conduct and publication of systematic reviews [11].
The protocol was previously published in the PROSPERO International Prospective Register of Systematic Reviews. Registration number: CRD42020169993 [12].
Research question
Should heated humidified high-flow nasal cannula be used versus conventional low-flow oxygen therapy to treat acute bronchiolitis in children under two years of age?
PICO question
P: patients younger than 24 months with a presumptive diagnosis of acute bronchiolitis.
I: nasal cannula with high-flow oxygen.
C: low-flow oxygen.
O: mortality, treatment failure (defined as the need for noninvasive ventilation or intubation), severity score, length of hospitalization, treatment-related adverse events.
Data sources
Two reviewers independently conducted a sensitive search in the following bibliographic databases: PubMed, EMBASE, LILACS, Cochrane Library, Epistemonikos, and Tripdatabase. A search was also made of other sources and repositories of health technology assessment agencies and national and international agencies. An evidence matrix was performed to identify among the primary studies that made up the different systematic reviews initially selected, works that had not emerged from other search strategies. Additional searches of the references were also carried out through Crossref.
This is the example search strategy in Medline/PubMed, which included the following terms:
#1 MeSH descriptor Oxygen Inhalation Therapy explode all trees #2 intubation rates*.
#3 (#1 AND #2) #4 ((high flow (nasal or prong or cannula)) or (nasal near oxygen)):ti,ab #5 (#3 OR #4).
No language restriction was performed. In addition, to identify additional literature, Google Scholar was searched, and experts were contacted. These searches were conducted according to the platform type, and free language terms were used in the search. The searches were conducted until July 1, 2020.
More details about the complete search can be found in Annex 1.
Selection of studies
We searched for randomized controlled trials, non-randomized, prospective, and analytical studies that included a control group in children under 24 months of age with a presumptive diagnosis of acute bronchiolitis. The intervention was high-flow oxygen nasal cannula, and the comparator was some form of low-flow oxygen administration.
The following outcomes were considered in order of clinical relevance: death (critical, 9), treatment failure, defined as the need for mechanical ventilation or noninvasive ventilation (mechanical ventilation or noninvasive ventilation) (critical, 7), days of hospitalization (important, 6), severity scores (important, 4), adverse events (not important, 3).
Data collection
Studies were selected by two reviewers independently based on inclusion and exclusion criteria. Differences were defined by agreement between the reviewers. References of identified systematic reviews were also reviewed. Two reviewers independently extracted the evidence of the selected outcomes in electronic spreadsheets designed for this purpose.
Risk of bias
Risk of bias assessment was performed through the risk of bias tool suggested by Cochrane (RoB-2) [13]. Two operators independently assessed the risk of bias in the trials (Annex 2 and Figure 2). For each trial and outcome, the reviewers rated them as follows:
Risk of bias domains: Bias arising from the randomization process; bias due to deviations from the intended intervention; bias due to missing outcome data; bias in outcome measurement; bias in the selection of outcome reports, including deviations from the recorded protocol; and bias arising from early termination in benefit.
Differences between operators were defined by a third party where necessary.
Measures of effect and statistical analysis
Analysis of the results was performed using relative risk for binary outcomes and mean difference for continuous outcomes, together with their 95% confidence interval. The Mantel and Haenszel random-effects model was used for meta-analysis.
R (RStudio Version 1.3.1073 © 2009-2020 RStudio, PBC) was used for meta-analytic calculations, risk of bias, publication bias, and the production of traffic light, summary, forest plot, and funnel plots.
Certainty of evidence
The GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach was used to assess the certainty in the body of evidence for each comparison. The GRADE tool was used to create the summary tables of findings, and the information on the studies and outcomes included was extracted in spreadsheets. Subsequently, the selected studies were synthesized, and the evidence profiles were constructed with the help of the GRADE website [14],[15].
We rated the certainty for each comparison and outcome as high, moderate, low, low, or very low, based on the risk assessment domains of bias, inconsistency, indirect evidence, publication bias, and imprecision.
The GRADE evidence profiles are available in Table 2 and Annex 2.
Analysis of sample power and optimal intervention size
To detect appropriate sample power, calculation of the optimal intervention size was performed, using R (RStudio Version 1.3.1073 © 2009-2020 RStudio, PBC), assuming an effect d (the hypothetical or plausible overall effect size of an intervention in the study compared with control) of SMD 0.15, a number k of studies of 5, the number of patients in intervention and control branches of 200 (n1 and n2) and an α level of 0.05 and moderate heterogeneity, with a power of 81.75%.
Subgroup analysis and publication bias
Subgroup analyses were performed according to the risk of bias of the included studies (low versus high risk of bias: LOW_ROB versus HIGH_ROB). The presence of publication bias was analyzed through the performance of a funnel plot and the Eggers test statistic [16].
Figure 1. PRISMA flow diagram.
Participants were in all cases under 24 months of age, while two studies only included children under 12 months of age and in another study only children under six months of age. The clinical setting was in all cases the inpatient, emergency, and pediatric critical care area. The intervention used was a nasal cannula with humidified and heated oxygen at high flow with a flow rate of 1 to 2 L/kg/min, with a maximum in all cases of 20 L. The comparator was low-flow oxygen with nasal cannula or a mask with 100% oxygen. A summary of the studies included in this review [17],[18],[19],[20],[21],[22] can be found in Table 1.
Table 1. Summary of studies included in the quantitative synthesis.
The excluded studies and the reasons for their exclusion [23],[24],[25],[26],[27],[28],[29] are described in Annex 2.
The overall risk of bias of the included studies was high in four of them, due to problems in blinding of participants and reporting of included outcomes, whereas, in two, Franklin et al. 2018 [19] and Kepreotes et al. 2017 [17], it was low (Figure 2).
Figure 2. Risk of bias of included studies.
Death outcome
Most of the studies included in this review did not report the outcome of death. One of them, Kepreotes et al. 2017 [17], reported that there were no deaths during the follow-up period.
Treatment failure outcome
Treatment failure (need for noninvasive, invasive ventilation, or orotracheal intubation) occurred in 108/933 in the humidified high-flow nasal cannula group and 233/934 in the low-flow group (relative risk: 0.46; 95% confidence interval: 0.35 to 0.62). This means in absolute numbers 11.7% less treatment failure (95% confidence interval between 7.9% and 14.5% less) in the high-flow humidified nasal cannula group (Table 2).
The certainty in the evidence regarding this outcome was moderate due to the high risk of bias in the included studies (Figure 3).
Figure 3. Forest plot of high-flow oxygen cannula versus low-flow oxygen
Outcome days of hospitalization
Patients treated with humidified high-flow nasal cannula versus those treated with low-flow had a mean difference in inpatient days of −0.55 (between 1.92 days less and 0.85 days more) (Figure 4).
The certainty of the evidence for this outcome was very low due to imprecision (wide confidence intervals including risks and benefits), heterogeneity (high I2, overlapping confidence intervals), and risk of bias in the included studies.
Figure 4. Forest plot of high-flow oxygen cannula versus low-flow oxygen
Disentanglement severity scores
The severity scores used varied widely among studies. While Hilliard et al. [18] reported no change in severity scores, Franklin et al. [19], Ergul et al. [21], and Milani et al. [22] used clinical parameters such as respiratory rate and effort, and feeding ability, which were then reported as individual outcomes in response to treatment.
Kepreotes and colleagues [17], on the other hand, initially assessed children through the Health Initial Severity Assessment of Bronchiolitis score, which also includes different clinical parameters such as cyanosis and oxygen saturation, using these parameters to assess treatment failure and time to treatment failure.
Finally, Bueno Campaña et al. [20] used the Respiratory Distress Assessment Instrument (RDAI), which measures the presence of wheezing, crackles, and rib retraction. The change in this score before and after treatment was used to measure the efficacy of the assigned treatment. In this study, no difference was found between the means of the two groups (p = 0.24): mean difference −1.22 (95% confidence interval: 2.99 to 0.55).
Treatment-related adverse events outcome
The included studies reported no intervention- or comparator-related adverse events.
Other analyses
For the outcome of treatment failure, heterogeneity was low among the included studies, and the direction and size of the effect were maintained after subgroup analysis between low and high risk of bias (Annex).
Regarding the outcome days of hospitalization, heterogeneity between studies was high I2 = 99% and was maintained after sensitivity analysis between studies with high and low risk of bias (Annex 2).
The publication bias analysis shows asymmetry in the funnel plots (Annex 2, Figures 3 and 4) and Eggers test at the limit of statistical significance intercept: −1.31 (95% confidence interval: −2.27 to −0.45), p = 0.06. However, the number of studies is less than 10, not enough to suspect publication bias.
The absolute and relative estimates of effect and the significance of the outcomes can be seen in Table 2.
This meta-analysis was conducted with high-quality standards, following regulations for conducting and reporting systematic reviews, together with PRISMA meta-analysis. We included the best available evidence through an exhaustive review of the literature and assessment of the risk of bias within the included studies and the publication bias among the studies. In addition, the evidence summary was performed using the GRADE methodology to determine the effect estimates and the degree of certainty of the body of literature included in the review.
The evidence analyzed shows that the use of oxygen through humidified and heated high-flow cannula is probably associated with an absolute reduction of 11.7% in treatment failure in infants with acute bronchiolitis under 24 months of age, with 7.5 patients needing to be treated with the intervention to reduce one event (number needed to treat 7.5; 95% confidence interval: 6 to 10).
Regarding days of hospitalization, there is uncertainty in the magnitude of the effect of humidified high-flow nasal cannula compared to standard treatment, so high-flow oxygen therapy may not be associated with a change in days of hospitalization. This is supported by low certainty of the evidence due to imprecision and risk of bias in the included studies.
We were unable to properly assess mortality since, in the studies reviewed, mortality remained below 1%. In the follow-up cohorts of patients with acute bronchiolitis, mortality was not reported; therefore, there is no evidence available on the effect of high-flow oxygen on death in the treatment of acute bronchiolitis in this age group.
However, severity scores were not included because they could not be adequately assessed, given that there is significant imprecision in the timing of their use, in the types of scores assessed, and in their proper reporting.
No intervention- or control-related adverse events were reported.
The use of high-flow humidified and heated oxygen compared with low-flow oxygen is likely associated with decreased treatment failure in children under two years of age with acute bronchiolitis.
There is uncertainty in the magnitude of the effect on hospital days and clinical progression scores.
The available evidence is insufficient to assess the effect of the intervention on mortality in the population evaluated.
Notes
Authorship contributions
FT: conceptualization, methodology, data validation, formal analysis, preparation and writing, editing and supervision. IA: conceptualization, methodology, formal analysis and supervision. GV: conceptualization, methodology, data validation and editing. VS: methodology and supervision. PH: formal analysis, preparation and writing, and editing. GC: preparation and writing and editing.
Competing interests
The authors completed the ICMJE conflict of interest statement and declared that they received no funding for the completion of this article; have no financial relationships with organizations that may have an interest in the published article in the last three years; and have no other relationships or activities that may influence the publication of the article. Forms can be requested by contacting the responsible author or the Editorial Board of the Journal.
Funding
The authors declare that they had no external sources of financing for the present study.
Ethics
The present study did not require evaluation by an ethics committee since it is a systematic review and uses secondary data sources.
Annex with supplementary material
Supplementary material, search strategy, tables, and graphs not present in this manuscript are available at the following link.
Registration of the study protocol
PROSPERO, CRD42020169993.
Language of submission
Spanish.

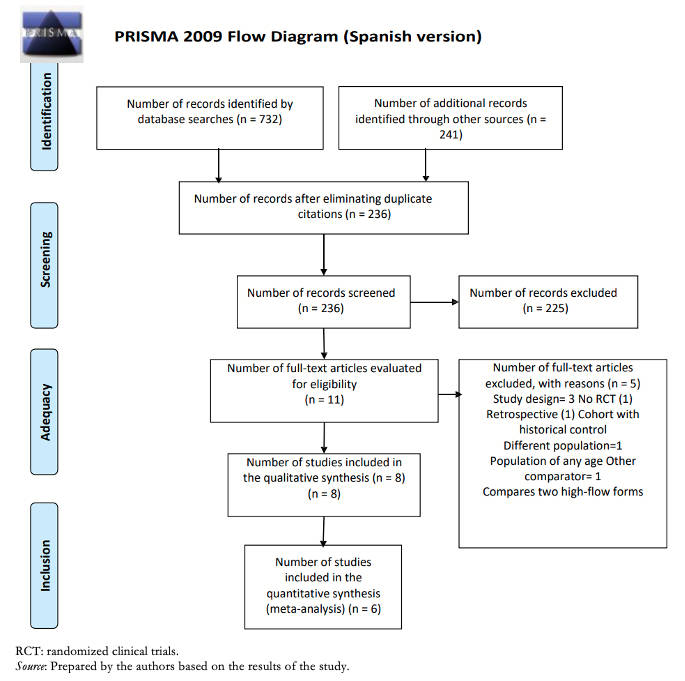 Figure 1. PRISMA flow diagram.
Figure 1. PRISMA flow diagram.

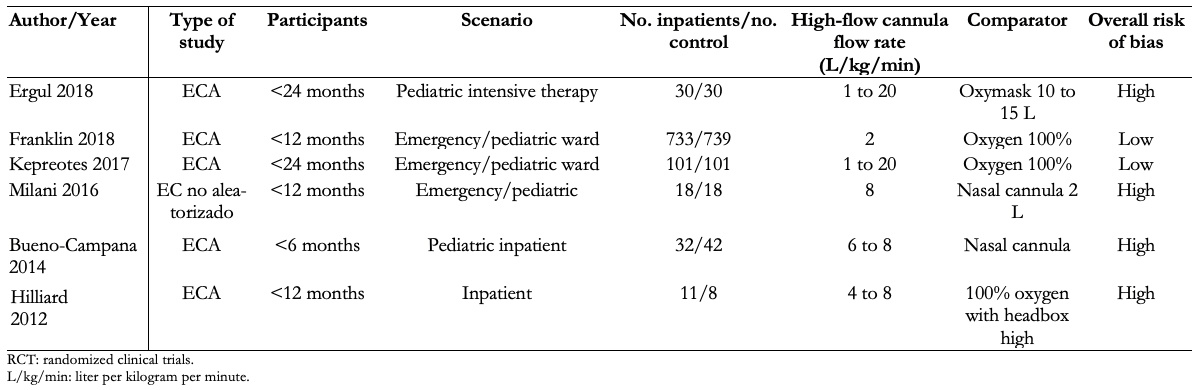 Table 1. Summary of studies included in the quantitative synthesis.
Table 1. Summary of studies included in the quantitative synthesis.

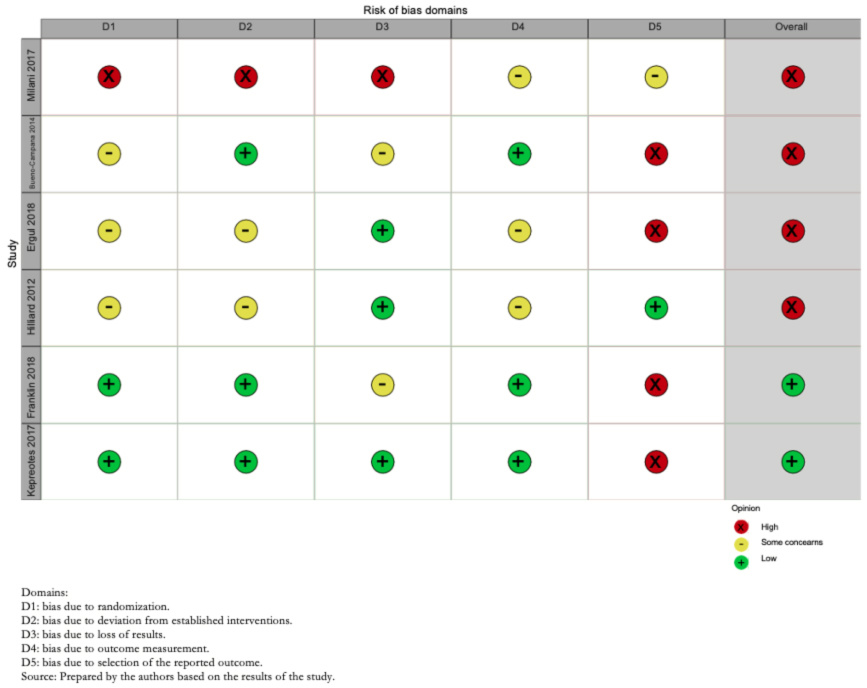 Figure 2. Risk of bias of included studies.
Figure 2. Risk of bias of included studies.

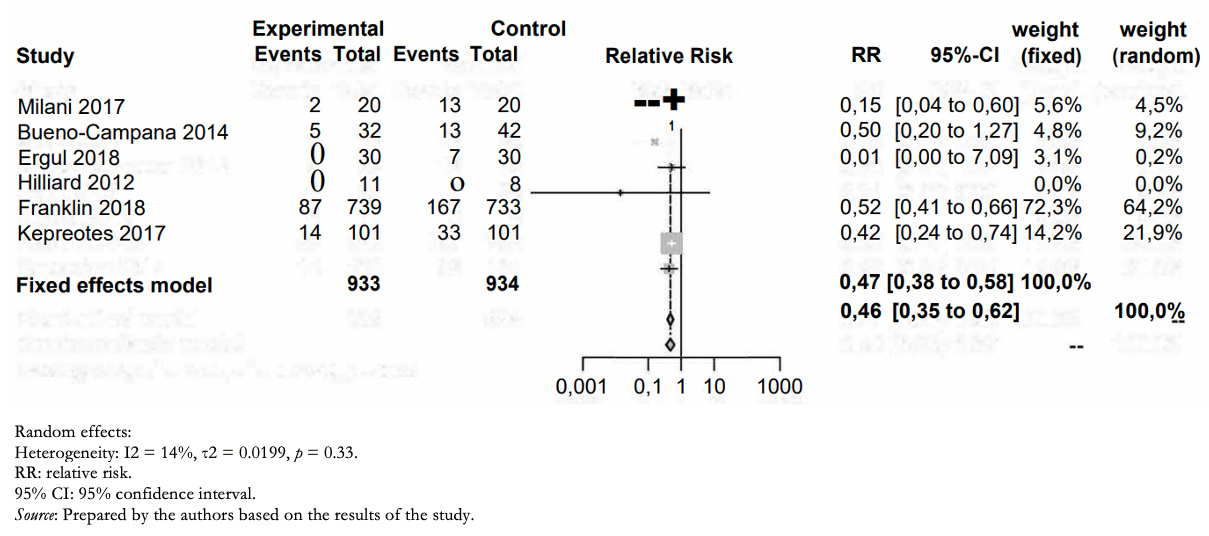 Figure 3. Forest plot of high-flow oxygen cannula versus low-flow oxygen
Figure 3. Forest plot of high-flow oxygen cannula versus low-flow oxygen

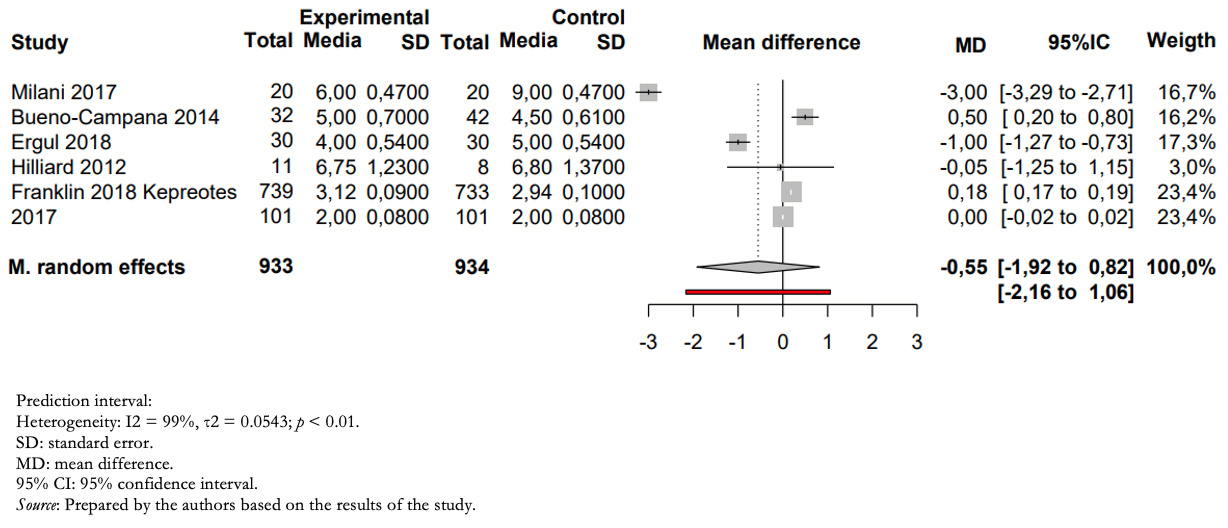 Figure 4. Forest plot of high-flow oxygen cannula versus low-flow oxygen
Figure 4. Forest plot of high-flow oxygen cannula versus low-flow oxygen

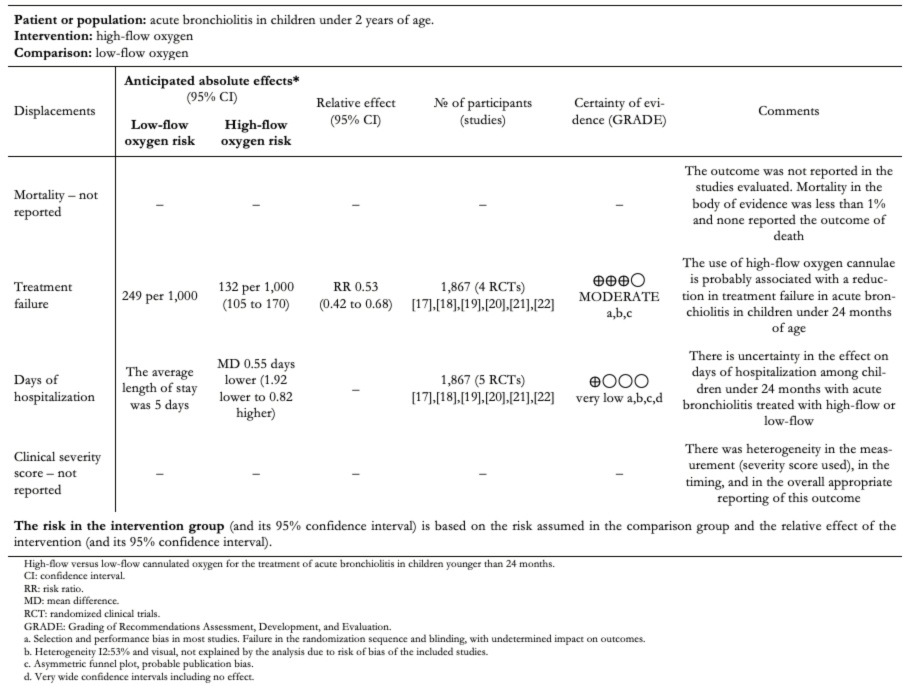 Table 2. Summary of findings.
Table 2. Summary of findings.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introduction
Oxygen therapy through a high-flow nasal cannula is thought to improve the work of breathing and the comfort of patients with acute bronchiolitis. It is widely used in hospital wards and critical care of pediatric patients. However, there is uncertainty on the magnitude of the effect on critical and important outcomes in these patients.
Objectives
The objective of this review is to evaluate the available evidence on the use of oxygen administered through high-flow cannula versus low-flow oxygen for the treatment of acute bronchiolitis in children under two years of age.
Methodology
We carried out a systematic review and a meta-analysis following the PRISMA standards for reporting. The search was carried out in electronic databases by two researchers independently. The evidence was summarized using the GRADE methodology.
Results
Six randomized and non-randomized clinical trials were included, including 1867 individuals younger than 24 months of age with acute bronchiolitis in pediatric emergency, hospitalization, and intensive care services. Mortality was not reported in the included studies. Treatment failure occurred in 108/933 in the high flow group and 233/934 in the low flow group (relative risk: 0.46; 95% confidence interval: 0.35 to 0.62), which shows 11.7% less treatment failure (95% confidence interval between 7.9% and 14.5% less) in the high flow group with a number needed to treat of 7.5 (95% confidence interval 6 to 10) with moderate certainty in the evidence.
Conclusion
The use of humidified and heated oxygen with high flow compared to oxygen at low flow is probably associated with decreased treatment failure in children younger than two years with acute bronchiolitis. There is uncertainty about the effect on hospitalization days and clinical progression.
 Autores:
Fernando Tortosa [1,2,3], Ariel Izcovich [4], Gabriela Carrasco[2], Gabriela Varone[3,5], Pedro Haluska[3], Verónica Sanguine[6]
Autores:
Fernando Tortosa [1,2,3], Ariel Izcovich [4], Gabriela Carrasco[2], Gabriela Varone[3,5], Pedro Haluska[3], Verónica Sanguine[6]

Citación: Tortosa F, Izcovich A, Carrasco G, Varone G, Haluska P, Sanguine V. High-flow oxygen nasal cannula for treating acute bronchiolitis in infants: A systematic review and meta-analysis. Medwave 2021;21(04):e8190 doi: 10.5867/medwave.2021.04.8190
Fecha de envío: 25/11/2020
Fecha de aceptación: 29/3/2021
Fecha de publicación: 12/5/2021
Origen: No solicitado.
Tipo de revisión: Revisión por pares externa, por tres árbitros a doble ciego.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 García Figueruelo A, Urbano Villaescusa J, Botrán Prieto M, Solana García MJ, Mencía Bartolomé S, López-Herce Cid J. Use of high-flow nasal cannula for non-invasive ventilation in children. An Pediatr (Barc). septiembre de 2011;75(3):182-7. | CrossRef | PubMed |
García Figueruelo A, Urbano Villaescusa J, Botrán Prieto M, Solana García MJ, Mencía Bartolomé S, López-Herce Cid J. Use of high-flow nasal cannula for non-invasive ventilation in children. An Pediatr (Barc). septiembre de 2011;75(3):182-7. | CrossRef | PubMed | Hough JL, Pham TMT, Schibler A. Delivery of high flow nasal prong oxygen: the effect CPAP exposed. Pediatric Critical Care Medicine Conference: 6th World Congress on Pediatric Critical Care. 2011; Vol. 12 (3 Suppl 1):A7.
Hough JL, Pham TMT, Schibler A. Delivery of high flow nasal prong oxygen: the effect CPAP exposed. Pediatric Critical Care Medicine Conference: 6th World Congress on Pediatric Critical Care. 2011; Vol. 12 (3 Suppl 1):A7.  Mikalsen IB, Davis P, Øymar K. High flow nasal cannula in children: a literature review. Scand J Trauma Resusc Emerg Med. 2016 Jul 12;24:93. | CrossRef | PubMed |
Mikalsen IB, Davis P, Øymar K. High flow nasal cannula in children: a literature review. Scand J Trauma Resusc Emerg Med. 2016 Jul 12;24:93. | CrossRef | PubMed | Tejera J, Pujadas M, Alonso B, Pírez C. Aplicación de oxigenoterapia de alto flujo en niños con bronquiolitis e insuficiencia respiratoria en piso de internación: Primera experiencia a nivel nacional. Archivos de Pediatría del Uruguay. 2013;84:28-33. [Internet] | Link |
Tejera J, Pujadas M, Alonso B, Pírez C. Aplicación de oxigenoterapia de alto flujo en niños con bronquiolitis e insuficiencia respiratoria en piso de internación: Primera experiencia a nivel nacional. Archivos de Pediatría del Uruguay. 2013;84:28-33. [Internet] | Link | Unger S, Cunningham S. Effect of oxygen supplementation on length of stay for
infants hospitalized with acute viral bronchiolitis. Pediatrics. 2008
Mar;121(3):470-5. | CrossRef | PubMed |
Unger S, Cunningham S. Effect of oxygen supplementation on length of stay for
infants hospitalized with acute viral bronchiolitis. Pediatrics. 2008
Mar;121(3):470-5. | CrossRef | PubMed | Oñoro G, Pérez Suárez E, Iglesias Bouzas MI, Serrano A, Martínez De Azagra A, et al. Bronquiolitis grave. Cambios epidemiológicos
y de soporte respiratorio [Severe bronchiolitis. Changes in epidemiology and
respiratory support]. An Pediatr (Barc). 2011 Jun;74(6):371-6. | CrossRef | PubMed |
Oñoro G, Pérez Suárez E, Iglesias Bouzas MI, Serrano A, Martínez De Azagra A, et al. Bronquiolitis grave. Cambios epidemiológicos
y de soporte respiratorio [Severe bronchiolitis. Changes in epidemiology and
respiratory support]. An Pediatr (Barc). 2011 Jun;74(6):371-6. | CrossRef | PubMed | American Academy of Pediatrics Subcommittee on Diagnosis and Management of
Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006
Oct;118(4):1774-93. | CrossRef | PubMed |
American Academy of Pediatrics Subcommittee on Diagnosis and Management of
Bronchiolitis. Diagnosis and management of bronchiolitis. Pediatrics. 2006
Oct;118(4):1774-93. | CrossRef | PubMed | Abboud PA, Roth PJ, Skiles CL, Stolfi A, Rowin ME. Predictors of failure in
infants with viral bronchiolitis treated with high-flow, high-humidity nasal
cannula therapy*. Pediatr Crit Care Med. 2012 Nov;13(6):e343-9. | CrossRef | PubMed |
Abboud PA, Roth PJ, Skiles CL, Stolfi A, Rowin ME. Predictors of failure in
infants with viral bronchiolitis treated with high-flow, high-humidity nasal
cannula therapy*. Pediatr Crit Care Med. 2012 Nov;13(6):e343-9. | CrossRef | PubMed | Moreel L, Proesmans M. High flow nasal cannula as respiratory support in
treating infant bronchiolitis: a systematic review. Eur J Pediatr. 2020
May;179(5):711-718. | CrossRef | PubMed |
Moreel L, Proesmans M. High flow nasal cannula as respiratory support in
treating infant bronchiolitis: a systematic review. Eur J Pediatr. 2020
May;179(5):711-718. | CrossRef | PubMed | González Martínez F, González Sánchez MI, Rodríguez Fernández R. Impacto
clínico de la implantación de la ventilación por alto flujo de oxígeno en el
tratamiento de la bronquiolitis en una planta de hospitalización pediátrica
[Clinical impact of introducing ventilation with high flow oxygen in the
treatment of bronchiolitis in a paediatric ward]. An Pediatr (Barc). 2013
Apr;78(4):210-5. | CrossRef | PubMed |
González Martínez F, González Sánchez MI, Rodríguez Fernández R. Impacto
clínico de la implantación de la ventilación por alto flujo de oxígeno en el
tratamiento de la bronquiolitis en una planta de hospitalización pediátrica
[Clinical impact of introducing ventilation with high flow oxygen in the
treatment of bronchiolitis in a paediatric ward]. An Pediatr (Barc). 2013
Apr;78(4):210-5. | CrossRef | PubMed | Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting
systematic reviews and meta-analyses of studies that evaluate healthcare
interventions: explanation and elaboration. BMJ. 2009 Jul 21;339:b2700. | CrossRef | PubMed |
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting
systematic reviews and meta-analyses of studies that evaluate healthcare
interventions: explanation and elaboration. BMJ. 2009 Jul 21;339:b2700. | CrossRef | PubMed | Tortosa F, Varone G, Izcovich, A. Fernando Tortosa, Gabriela Varone, Ariel Izcovich. High flow oxygen nasal cannula versus low flow oxygen for the treatment of acute bronchiolitis in infants. PROSPERO 2020 CRD42020169993. [Internet] | Link |
Tortosa F, Varone G, Izcovich, A. Fernando Tortosa, Gabriela Varone, Ariel Izcovich. High flow oxygen nasal cannula versus low flow oxygen for the treatment of acute bronchiolitis in infants. PROSPERO 2020 CRD42020169993. [Internet] | Link | Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019 Aug 28;366:l4898. | CrossRef | PubMed |
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019 Aug 28;366:l4898. | CrossRef | PubMed | Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 26;336(7650):924-6. | CrossRef | PubMed |
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 26;336(7650):924-6. | CrossRef | PubMed | Dickersin K. Publication Bias: Recognizing the Problem, Understanding Its Origins and Scope, and Preventing Harm. En: Publication Bias in Meta‐Analysis. John Wiley & Sons, Ltd; 2005. p. 9-33. [Internet] | Link |
Dickersin K. Publication Bias: Recognizing the Problem, Understanding Its Origins and Scope, and Preventing Harm. En: Publication Bias in Meta‐Analysis. John Wiley & Sons, Ltd; 2005. p. 9-33. [Internet] | Link | Atkins D, Briss PA, Eccles M, Flottorp S, Guyatt GH, et al. Systems
for grading the quality of evidence and the strength of recommendations II:
pilot study of a new system. BMC Health Serv Res. 2005 Mar 23;5(1):25. | CrossRef | PubMed |
Atkins D, Briss PA, Eccles M, Flottorp S, Guyatt GH, et al. Systems
for grading the quality of evidence and the strength of recommendations II:
pilot study of a new system. BMC Health Serv Res. 2005 Mar 23;5(1):25. | CrossRef | PubMed | Kepreotes E, Whitehead B, Attia J, Oldmeadow C, Collison A, Searles A, et al. High-flow warm humidified oxygen versus
standard low-flow nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT):
an open, phase 4, randomised controlled trial. Lancet. 2017 Mar
4;389(10072):930-939. | CrossRef | PubMed |
Kepreotes E, Whitehead B, Attia J, Oldmeadow C, Collison A, Searles A, et al. High-flow warm humidified oxygen versus
standard low-flow nasal cannula oxygen for moderate bronchiolitis (HFWHO RCT):
an open, phase 4, randomised controlled trial. Lancet. 2017 Mar
4;389(10072):930-939. | CrossRef | PubMed | Hilliard TN, Archer N, Laura H, Heraghty J, Cottis H, Mills K, et al. Pilot study of vapotherm oxygen delivery in moderately severe bronchiolitis.
Arch Dis Child. 2012 Feb;97(2):182-3. | CrossRef | PubMed |
Hilliard TN, Archer N, Laura H, Heraghty J, Cottis H, Mills K, et al. Pilot study of vapotherm oxygen delivery in moderately severe bronchiolitis.
Arch Dis Child. 2012 Feb;97(2):182-3. | CrossRef | PubMed | Franklin D, Babl FE, Schlapbach LJ, Oakley E, Craig S, Neutze J, et al. A Randomized Trial of
High-Flow Oxygen Therapy in Infants with Bronchiolitis. N Engl J Med. 2018 Mar
22;378(12):1121-1131. | CrossRef | PubMed |
Franklin D, Babl FE, Schlapbach LJ, Oakley E, Craig S, Neutze J, et al. A Randomized Trial of
High-Flow Oxygen Therapy in Infants with Bronchiolitis. N Engl J Med. 2018 Mar
22;378(12):1121-1131. | CrossRef | PubMed | Bueno Campaña M, Olivares Ortiz J, Notario Muñoz C, Rupérez Lucas M,
Fernández Rincón A, Patiño Hernández O, et al. High flow therapy versus
hypertonic saline in bronchiolitis: randomised controlled trial. Arch Dis Child.
2014 Jun;99(6):511-5. | CrossRef | PubMed |
Bueno Campaña M, Olivares Ortiz J, Notario Muñoz C, Rupérez Lucas M,
Fernández Rincón A, Patiño Hernández O, et al. High flow therapy versus
hypertonic saline in bronchiolitis: randomised controlled trial. Arch Dis Child.
2014 Jun;99(6):511-5. | CrossRef | PubMed | Ergul AB, Calıskan E, Samsa H, Gokcek I, Kaya A, Zararsiz GE, et al. Using
a high-flow nasal cannula provides superior results to OxyMask delivery in
moderate to severe bronchiolitis: a randomized controlled study. Eur J Pediatr.
2018 Aug;177(8):1299-1307. | CrossRef | PubMed |
Ergul AB, Calıskan E, Samsa H, Gokcek I, Kaya A, Zararsiz GE, et al. Using
a high-flow nasal cannula provides superior results to OxyMask delivery in
moderate to severe bronchiolitis: a randomized controlled study. Eur J Pediatr.
2018 Aug;177(8):1299-1307. | CrossRef | PubMed | Milani GP, Plebani AM, Arturi E, Brusa D, Esposito S, Dell'Era L, et al. Using a high-flow nasal cannula provided
superior results to low-flow oxygen delivery in moderate to severe
bronchiolitis. Acta Paediatr. 2016 Aug;105(8):e368-72. | CrossRef | PubMed |
Milani GP, Plebani AM, Arturi E, Brusa D, Esposito S, Dell'Era L, et al. Using a high-flow nasal cannula provided
superior results to low-flow oxygen delivery in moderate to severe
bronchiolitis. Acta Paediatr. 2016 Aug;105(8):e368-72. | CrossRef | PubMed | Mayfield S, Bogossian F, O'Malley L, Schibler A. High-flow nasal cannula
oxygen therapy for infants with bronchiolitis: pilot study. J Paediatr Child
Health. 2014 May;50(5):373-8. | CrossRef | PubMed |
Mayfield S, Bogossian F, O'Malley L, Schibler A. High-flow nasal cannula
oxygen therapy for infants with bronchiolitis: pilot study. J Paediatr Child
Health. 2014 May;50(5):373-8. | CrossRef | PubMed | Maitland K, Kiguli S, Opoka RO, Olupot-Olupot P, Engoru C, Njuguna P, et al. Children's Oxygen Administration Strategies Trial (COAST): A
randomised controlled trial of high flow versus oxygen versus control in African
children with severe pneumonia. Wellcome Open Res. 2018 Jan 9;2:100. | CrossRef | PubMed |
Maitland K, Kiguli S, Opoka RO, Olupot-Olupot P, Engoru C, Njuguna P, et al. Children's Oxygen Administration Strategies Trial (COAST): A
randomised controlled trial of high flow versus oxygen versus control in African
children with severe pneumonia. Wellcome Open Res. 2018 Jan 9;2:100. | CrossRef | PubMed | Franklin D, Shellshear D, Babl FE, Schlapbach LJ, Oakley E, Borland ML, et al. Multicentre, randomised trial to investigate early nasal high-flow
therapy in paediatric acute hypoxaemic respiratory failure: a protocol for a
randomised controlled trial-a Paediatric Acute respiratory Intervention Study
(PARIS 2). BMJ Open. 2019 Dec 18;9(12):e030516. | CrossRef | PubMed |
Franklin D, Shellshear D, Babl FE, Schlapbach LJ, Oakley E, Borland ML, et al. Multicentre, randomised trial to investigate early nasal high-flow
therapy in paediatric acute hypoxaemic respiratory failure: a protocol for a
randomised controlled trial-a Paediatric Acute respiratory Intervention Study
(PARIS 2). BMJ Open. 2019 Dec 18;9(12):e030516. | CrossRef | PubMed | Daverio M, Da Dalt L, Panozzo M, Frigo AC, Bressan S. A two-tiered high-flow
nasal cannula approach to bronchiolitis was associated with low admission rate
to intensive care and no adverse outcomes. Acta Paediatr. 2019
Nov;108(11):2056-2062. | CrossRef | PubMed |
Daverio M, Da Dalt L, Panozzo M, Frigo AC, Bressan S. A two-tiered high-flow
nasal cannula approach to bronchiolitis was associated with low admission rate
to intensive care and no adverse outcomes. Acta Paediatr. 2019
Nov;108(11):2056-2062. | CrossRef | PubMed | Bressan S, Balzani M, Krauss B, Pettenazzo A, Zanconato S, Baraldi E. High-
flow nasal cannula oxygen for bronchiolitis in a pediatric ward: a pilot study.
Eur J Pediatr. 2013 Dec;172(12):1649-56. | CrossRef | PubMed |
Bressan S, Balzani M, Krauss B, Pettenazzo A, Zanconato S, Baraldi E. High-
flow nasal cannula oxygen for bronchiolitis in a pediatric ward: a pilot study.
Eur J Pediatr. 2013 Dec;172(12):1649-56. | CrossRef | PubMed | Monteverde E, Fernández A, Ferrero F, Barbaro C, De Lillo L, Lavitola M, et al. High-flow nasal cannula oxygen therapy in infants
with acute lower respiratory tract infection. An experience in hospitals of the
City of Buenos Aires. Arch Argent Pediatr. 2019 Oct 1;117(5):286-293. | CrossRef | PubMed |
Monteverde E, Fernández A, Ferrero F, Barbaro C, De Lillo L, Lavitola M, et al. High-flow nasal cannula oxygen therapy in infants
with acute lower respiratory tract infection. An experience in hospitals of the
City of Buenos Aires. Arch Argent Pediatr. 2019 Oct 1;117(5):286-293. | CrossRef | PubMed | Milési C, Essouri S, Pouyau R, Liet JM, Afanetti M, Portefaix A, et al. High flow nasal cannula (HFNC) versus nasal
continuous positive airway pressure (nCPAP) for the initial respiratory
management of acute viral bronchiolitis in young infants: a multicenter
randomized controlled trial (TRAMONTANE study). Intensive Care Med. 2017
Feb;43(2):209-216. | CrossRef | PubMed |
Milési C, Essouri S, Pouyau R, Liet JM, Afanetti M, Portefaix A, et al. High flow nasal cannula (HFNC) versus nasal
continuous positive airway pressure (nCPAP) for the initial respiratory
management of acute viral bronchiolitis in young infants: a multicenter
randomized controlled trial (TRAMONTANE study). Intensive Care Med. 2017
Feb;43(2):209-216. | CrossRef | PubMed |