 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: Psychological trauma, Post-traumatic stress disorders, Acute traumatic stress disorders, Therapeutics
Stressful life situations can generate chronic symptomatology, so it is of great concern to analyze preventive strategies. Psychological debriefing is an intervention for acute trauma, which verbalizes perceptions, thoughts, and emotions experienced during a recent traumatic event. The evidence surrounding its efficacy is controversial. This article discusses the efficacy of psychological debriefing based on systematic reviews and clinical practice guidelines. In all, nine systematic reviews were included. Only one of them found that psychological debriefing effectively decreased psychological stress, while the remaining eight found no significant effects for outcomes such stress, depressive and anxious symptoms, or development and severity of post-traumatic stress disorder. Moreover, two clinical trials found that the intervention had a significantly deleterious effect. Another study found a worsening in the symptomatology associated with the event. Of the eight clinical practice guidelines incorporated, none recommended psychological debriefing as an intervention for acute trauma. Some phenomena could explain the lack of success of the intervention in the scientific evidence. The bioethical conditions related to the traumatic scenario hinder its research, and its lack of standardization makes its evaluation in clinical trials problematic. Other variables such as ethnicity, personality, culture, gender, and history of traumatic experiences have been little considered in research. Nevertheless, the intervention may hinder the adequate processing of traumatic memory and emotions. Current evidence is consistent in not recommending psychological debriefing as an intervention for acute trauma, so its management should avoid it. It is suggested to promote research on preventive interventions to develop chronic traumatic symptomatology.
|
Main messages
|
Some stressful life events can trigger mental symptoms and configure themselves as psychic trauma. This damaging situation has convened research on the prevention of chronic psychopathology, especially in the form of post-traumatic stress disorder. This latter condition develops in 14% [1] (or 37% in intentional events [2]) of acute trauma cases, in addition to about 40% of people who have acute stress disorder [3],[4]. In many cases, post-traumatic stress disorder is resolved without interventions. However, symptomatic persistence at ten years reaches one-third of cases and has profound clinical implications that may alter personal identity, as in complex trauma [5],[6],[7]. Little is known about the epidemiology of traumatic events in Latin America. Still, it is estimated that about 40% of the Chilean population has experienced acute trauma [6],[7],[8], whereas, in countries like Mexico, the figure is twice as high [9].
Most people have emotional, behavioral, physiological, and cognitive reactions following a traumatic experience – i.e., emotional lability, irritability, intrusive thoughts, and behavioral avoidance. Nevertheless, some patients show intense and dissociative sphere-related symptomatology and develop acute stress disorder [6]. Although with low sensitivity, this acute disorder has a sufficient positive predictive value for post-traumatic stress disorder [3]. The traumatic manifestations are nonspecific during the two weeks following the stressful event, and therefore, the interventions applied during this period must be broad. These include psychological debriefing, psychological first aid, and various forms of counseling [10].
Psychological debriefing is one of the most widespread interventions for acute psychological trauma [11],[12]. Briefly, the World Health Organization (WHO) notes that psychological debriefing involves an emotional opening, encouraging the person to make a brief but systematic account of perceptions, thoughts, and emotional reactions experienced during a recent stressful event [13]. Most studies that have tested psychological debriefing conceptualize the intervention in this direction. Several variants of psychological debriefing share a common background and address similar outcomes but with different structures. Within this field, we should distinguish psychological debriefing from practices such as "psychological first aid," which aims to provide a "human response" of support, listening, and help, without necessarily delving into detailed discussion and analysis of the distress-provoking event [14].
In psychological debriefing, two main currents can be recognized. The first is a cognitive intervention developed by Mitchell [15], whose original objective was to provide psychological support to people working in disaster areas. With a psychodynamic background, the second was developed by de Clercq and Lebigot [16]. Its purpose was to link affective and perceptual phenomena through a re-registration in the symbolic order. Mitchell’s technique has received more attention, probably because it is protocolized, allowing a more systematic evaluation. However, it has often been used as an isolated intervention outside the context of the intervention program developed by Mitchell [17].
The scientific evidence is controversial regarding the efficacy of psychological debriefing in reducing post-traumatic symptomatology and preventing post-traumatic stress disorder [18]. Some authors, such as Hawker et al. [19], have argued for the intervention. Others, such as Bisson et al. [20] and Hobbs et al. [21], claim deleterious effects on depression and anxiety and even an increase the occurrence of post-traumatic stress disorder. The inconsistency between findings has been attributed to deficits in the intervention itself, problems in the methodological designs and the definition of interventions and outcomes, and the difficulty of conducting clinical trials due to bioethical concerns [19].
This article reviews some therapeutic aspects of psychological debriefing, discussing its efficacy based on the evidence provided by systematic reviews and the main clinical practice guidelines for managing traumatic stress (Box 1).
|
Box 1. Search and selection of systematic reviews and clinical practice guidelines. We searched PubMed/Medline, PsycINFO, and Cochrane Library for systematic literature reviews with meta-analysis. The search terms used were "debriefing," "psychological debriefing," "post-traumatic stress disorders," and "acute traumatic stress disorders." "AND" and "OR" were used as Boolean operators. Publications in English and Spanish available until October 2021 that analyzed the efficacy of psychological debriefing were selected. If there were updates of systematic reviews that have been conducted on the same protocol, the results from the most updated version are mentioned. The web pages of the main societies and governmental divisions of traumatic stress, psychiatry, psychology, and mental health were searched according to the authors' criteria of this study to include clinical practice guidelines. Primary studies and narrative reviews were excluded. Source: Prepared by the authors of this study. |
Description of the intervention
Psychological debriefing is a brief intervention during the first days after the traumatic event. It can be a group session led by a moderator, where those affected by the traumatic episode discuss, through catharsis, the cognitions and affective and physical reactions linked to the event [15],[22]. It promotes the normalization of common responses to trauma and provides information on coping strategies and future assistance [19]. Although initially practiced with individuals working in rescue teams, it has also been implemented in single-session and multiple settings [23]. 'Critical Incident Stress Debriefing' is the first and most widely applied method, designed to be conducted between two and ten days after a traumatic event or up to four weeks after a mass disaster [15,24]. The original model is performed in a more extensive program called Critical Incident Stress Management, which includes other crisis intervention strategies (i.e., pre-trauma stress inoculation training, group psychological debriefing, counseling sessions, and follow-up) [15],[24].
Mitchell’s standardized 'Critical Incident Stress Debriefing' [26] consists of seven stages applied to small groups presenting significant traumatic events (Table 1).
Table 1. Phases of psychological debriefing.
This practice should only be performed by trained personnel. Its objectives are:
After the psychological debriefing, some follow-up activities can be conducted. Box 2 briefly describes the historical context of the development of the intervention.
|
Box 2. The historical context of psychological debriefing. During the development of avant-garde military psychiatry in the second decade of the 20th-century, military psychiatrist Thomas William Salmon [52] articulated the so-called "Salmon principles," aimed at recovering traumatized soldiers to continue in combat. These principles indicate the characteristics that psychological interventions for acute stress during catastrophes or wars should have, being applied in the design of psychological interventions within the First and Second World Wars: "proximity" (interventions close to the "front line"), "immediacy" (early interventions), "centrality" (coordinated interventions), "simplicity" (brief, simple and easily applicable interventions) and "expectation" (interventions that provide hope for recovery) [53]. Since the 1970s, Jeffrey T. Mitchell began to develop debriefing groups. However, it was only in 1983 that he formally introduced the concept of "debriefing" when he published an article describing a technique called 'Critical Incident Stress Debriefing' [15]. He presents it as a simple and effective intervention to help emergency workers cope with experienced events, allowing them to continue their work with minimal long-term effects, in line with Salmon’s earlier proposal. Interventions related to debriefing have emphasized the healing power of abreaction or catharsis, incorporating other elements that enable a change in the content of traumatic memories, such as reflection and elaboration [22]. Subsequent developments have enriched the intervention, which since the late 1980s has been known as "psychological debriefing" [51]. Psychological debriefing and some similar interventions are currently used by groups of people and work organizations to contain the traumatic event, understanding that the procedure would alleviate the distress associated with the trauma and promote appropriate processing [54]. Source: Prepared by the authors based on the theoretical literature review. |
The findings of systematic reviews with meta-analysis that intend to scrutinize the effects of psychological debriefing, as well as recommendations suggested by clinical practice guidelines, are described below (Table 2).
Systematic Reviews
Everly et al. (1999) [17] evaluated the effect of psychological debriefing on acute stress, incorporating ten studies (n = 698). They concluded that the technique would effectively alleviate symptoms associated with psychological stress in emergency health care workers.
Two reviews have analyzed the effects of psychological debriefing as a single session. Rose et al. [27] (2002) published the third update of a Cochrane review, which evaluated the effectiveness of a single session of psychological debriefing on post-traumatic symptomatology. Clinical trials conducted in adults who experienced psychological trauma within a month were included. In the 15 studies included, the intervention was applied between 24 hours and one month after the event. Compared to the control, the psychological debriefing did not prevent the development of post-traumatic stress disorder or reduce its severity. There was also no evidence of decreased levels of psychological stress, general psychological morbidity, depression, or anxiety. Of note are the individual findings observed in the clinical trials of Bisson et al. [20] and Hobbs et al. [21], both of which suggested a deleterious effect of the intervention. In the first case, adults who had suffered burns (n = 133) were analyzed. After 13 months, the group that received the single session of psychological debriefing exhibited significantly higher means of anxiety, depression, and subjective stress levels associated with the event and a higher frequency of post-traumatic stress disorder.
In the second study, adult victims of traffic accidents were included. The intervention group had a worse outcome in terms of post-traumatic symptomatology measured at four and 36 months. A second review that analyzed single-session psychological debriefing was published by van Emmerik et al. (2003) [18]. This review included seven randomized clinical trials that measured the effect of 'Critical Incident Stress Debriefing' and other interventions to treat acute psychological trauma. Interventions related to 'Critical Incident Stress Debriefing' failed to demonstrate a reduction of the severity of posttraumatic symptoms. No significant differences were found between 'Critical Incident Stress Debriefing' and other techniques in terms of symptomatic reduction.
Gillies et al. (2016) [10] conducted a review to evaluate the efficacy of different psychological therapies in trauma-exposed children and adolescents. Three clinical trials (n = 317) met the inclusion criteria, and all were at high risk of bias. The study found no significant intervention effect on global symptomatology associated with post-traumatic stress disorder, nor on specific symptom clusters, such as avoidance, hypervigilance, and intrusion. In terms of secondary outcomes, there was no significant effect on anxious or depressive levels. This review was an update of the 2012 Cochrane review [28]. For its part, the review by Wethington et al. (2008) [29] analyzed the effect of different psychological interventions on psychological harm linked to traumatic events. Only one study by Stallard et al. [30] evaluated psychological debriefing and found no statistically significant differences in the levels of depression, anxiety, and the frequency of post-traumatic stress disorder between groups. However, an increase in the rates of all three outcomes was observed in the intervention branch.
de Graaff et al. (2018) [31] studied the effect of 'Critical Incident Stress Debriefing' on the prevention of post-traumatic stress disorder following birth-associated traumatic experiences. Two clinical trials were included. The first one [32] recruited postpartum women (n = 1745), in whom 'Critical Incident Stress Debriefing' was applied between 48 and 72 hours postpartum, without finding significant differences in the incidence of posttraumatic stress disorder at two, six, and 12 months postpartum. The second clinical trial was conducted by Gamble et al. [33] but evaluated a counseling intervention that did not involve psychological debriefing per se.
The focus of the systematic review by Forneris et al. (2013) [34] was broader, considering studies that examined psychological and pharmacological interventions to prevent posttraumatic stress disorder. Three randomized clinical trials addressed psychological debriefing but did not demonstrate a decrease in the incidence or severity of post-traumatic stress disorder.
The review by Bastos et al. (2015) [35] included seven studies (n = 3596) and analyzed the effect of psychological debriefing to prevent postpartum psychological trauma. The included studies were generally of low quality, and no significant differences were seen between the intervention and standard postnatal care at six months. Therefore, the authors conclude that there is little or no evidence to recommend this technique. Similar results were reported by Maglione et al. (2021) [36], who analyzed the effect of different interventions for combat stress and post-traumatic stress disorder in military and first responders. Specifically, group debriefing and 'Critical Incident Stress Debriefing' did not demonstrate significant effects on posttraumatic symptomatology or the emergence of post-traumatic stress disorder.
In summary, only one of the nine systematic reviews included in this article mentioned a significant positive effect of psychological debriefing on acute stress [17]. In contrast, two clinical trials analyzed in the reviews found significant deleterious effects of the intervention [20],[21], while one found a numerical worsening of the outcomes studied [30].
Table 2. Synthesis of the main findings of the systematic reviews.
Clinical practice guidelines
Based on the evidence published on psychological debriefing, different governmental divisions and independent organizations related to mental health have developed clinical guidelines that issue recommendations for managing acute trauma.
In Chile, the Technical Guidance for the Management of Acute Stress Disorder (2019) does not mention psychological debriefing as an intervention to be considered [37], nor does the American Psychological Association guide [38]. For its part, in the 2013 guideline for treating stress-related conditions [13], the WHO comments that there is no demonstrated benefit that psychological debriefing, in single or multiple sessions, in adults, children or adolescents, prevents post-traumatic stress disorder after the potentially traumatic event. Of note, this guideline suggests that psychological first aid is a feasible alternative. The International Society for Traumatic Stress Studies' guidelines for the prevention and treatment of post-traumatic stress disorder [11] also indicates insufficient evidence to recommend psychological debriefing in adults. Likewise, it states that it is not recommended for children or adolescents since the intervention increases the risk of suffering post-traumatic symptoms in a clinically relevant way. Moreover, the clinical guideline for the management of post-traumatic stress disorder published by the National Institute for Health and Care Excellence (NICE) of the United Kingdom (2018) [12] encourages not to perform psychological debriefing in adults in light of clinically irrelevant benefits, as well as its detrimental potential on post-traumatic symptomatology. The Australian guideline also supports this recommendation for the Treatment of Acute and Posttraumatic Stress Disorder [39]. The US Department of Veterans Affairs and Department of Defense Guidance for the Management of Acute and Posttraumatic Stress Disorder [40] indicates that psychological debriefing is not beneficial and may be harmful in asymptomatic individuals. Also, it states that it is not a feasible way to reduce acute stress symptomatology or prevent progression to post-traumatic stress disorder. The same is noted by the American Psychiatric Association guideline [41] for the treatment of acute and post-traumatic stress disorder, where psychological debriefing or similar techniques involving a single session are not recommended, as they appear to be ineffective and may increase symptomatology. These recommendations are consistent with the Canadian clinical practice guideline for managing anxiety, post-traumatic stress, and obsessivecompulsive disorders [42].
In this article, the effectiveness of psychological debriefing as an intervention for acute trauma was analyzed from the evidence provided by systematic reviews and clinical practice guidelines. Nine systematic reviews and eight clinical guidelines were considered. Only one review found the effectiveness of the intervention [17]. However, the review contained primary studies with different methodological designs, including observational and quasi-experimental, so their conclusions are debatable and controversial. In all, no guidelines recommend psychological debriefing.
Some authors advocate that the intervention may have a positive role that has not been reflected in studies. There are multiple forms of psychological debriefing, more or less similar to 'Critical Incident Stress Debriefing,' that deviate from the original protocol. This aspect may cloud the systematic evaluation of its effectiveness from different dimensions: the technical qualification of those who apply it, the way of selecting the intervention group, the structure of the intervention, its temporality, and its application as a single intervention or in a larger management context [22],[43]. Therefore, it is expected to find different conclusions regarding efficacy, which ultimately depends on the specific way the intervention is conducted [43]. On the other hand, the samples studied are highly heterogeneous in terms of biodemographic characteristics and the nature of the trauma. The individual risk of developing chronic post-traumatic symptomatology is equally variable from this perspective. The original conception of 'Critical Incident Stress Debriefing' was considered for patients with occupational risk and not the general population [19].
Research in psychological interventions to prevent post-traumatic symptomatology must consider personality, culture, gender, ethnicity – and, of course – previous traumatic experiences. Patients with a history of previous events have an increased pre-traumatic risk and benefit more from acute psychological interventions. From this point of view, authors such as Hawker et al. [19] argue that the fundamental problem with the scientific evidence for psychological debriefing is the poor quality evidence. The researchers assert that standardized 'Critical Incident Stress Debriefing' contains similar elements to well-documented trauma-focused cognitive-behavioral therapy, such as recall of the traumatic experience, psychoeducation, cognitive restructuring, and the development of coping strategies. However, cognitive-behavioral therapy usually takes place weeks or months after the traumatic event, thus constituting a form of psychotherapy rather than crisis intervention [24]. This psychotherapy has shown greater effectiveness than supportive counseling or no intervention in decreasing the incidence of post-traumatic stress disorder and is recommended by the Chilean Ministry of Health guidelines for managing acute stress disorder [37].
Although some participants value psychological debriefing as a helpful intervention [24],[43], there is a lack of correspondence between perceived help, its efficacy in reducing acute symptomatology, and its preventive capacity. Perceived satisfaction is not an indicator of intervention efficacy, especially considering that some people may satisfy from performing potentially dangerous actions. Conversely, – and especially in cases where symptomatology is not configured as a clinical diagnosis – self-assessed benefit might be a good measure of effectiveness because patients' judgement may be more important than the presence of symptoms perceived by researchers [43].
Due to bioethical considerations concerning traumatic exposure, experimental design is problematic and underlies some methodological difficulties observed in studies examining psychological debriefing. The British Psychological Society [44] reviewed this subject, highlighting the ethical difficulty in conducting clinical trials (especially in disaster conditions), which may explain the poor success of psychological debriefing. Therefore, they recommend the implementation of mixed experimental methodological designs. On the other hand, some authors argue that the lack of effectiveness of 'Critical Incident Stress Debriefing' is associated with the negative interference that the intervention would cause on the natural processing of trauma [45],[46]. These interventions would prevent adequate habituation time and deepen sensitization to the traumatic stimulus [47] against the natural post-traumatic process. On this point, van Emmerick et al. [18] reported that participants who did not receive interventions would have superior symptomatic improvement than those who received 'Critical Incident Stress Debriefing.' Hence, natural recovery would allow a better outcome. However, they note that 'Critical Incident Stress Debriefing' was conceptualized as part of a broader management plan and not a single session.
The two systematic reviews that evaluated single-session psychological debriefing did not find a significant symptomatic reduction or capacity as a preventive intervention. One of them revealed that two of the included clinical trials showed a worsening in the outcomes measured [18],[27]. However, the isolated intervention does not correspond to the original 'Critical Incident Stress Debriefing' strategy, including cognitivebehavioral techniques such as pre-trauma stress inoculation and follow-up counseling. On this assumption, the Critical Incident Stress Management program would only be feasible in populations at high risk of exposure. Such groups, that differ in their general characteristics from published trials include firefighters, emergency health care personnel, and military personnel [45]. Hobbs et al. [21] evaluated debriefing as a single intervention in acute episodes through a clinical trial. The authors indicate that its lack of efficacy and potential for harm could be related: first, to a state of numbing or emotional stress and hindering the reception of the intervention; second, to a disruption of natural psychological processes in the face of trauma; and third, to the inadequacy of the single intervention in the face of major emotional disturbances. Therefore, they emphasize the application of psychological interventions not too close to the traumatic event and identifying the population at risk of chronicity. Indeed, it has been pointed out that promoting early detailed verbalization of the traumatic event may vividly encode the traumatic memory, reinforcing feelings of hopelessness [19]. However, Mitchell and collaborators [48] emphasize that the fundamental phase of the intervention is the Reactions phase and not the verbalization of the facts themselves (Facts phase).
'Critical Incident Stress Debriefing' increases awareness of the most frequent post-traumatic manifestations. It aims to normalize them, attenuating the alarm signals, resulting in less environmental support [18]. On the other hand, the psychoeducational approach may medicalize common post-traumatic reactions and even produce secondary traumatization [49]. Nevertheless, low perception of social support and a high perception of psychosocial stress are risk factors for post-traumatic stress disorder.
The most appropriate temporal window for applying interventions involving verbalization of the traumatic event is poorly elucidated. Bisson et al. [20] found that single-session debriefing would worsen the clinical picture. The authors state that a possible explanatory mechanism is an intense exposure to traumatic imagery near the event, which would deepen the traumatization by altering the emotional processing of the experience. At the same time, the authors point out that psychological debriefing has a limited time, especially if it is a single session, so it would represent a new traumatic experience without achieving habituation if the person does not undergo additional interventions.
Although clinical trials and systematic reviews analyzing the effect of psychological debriefing are scarce, the current evidence is consistent in not endorsing it as a form of treatment or prevention of post-traumatic symptomatology. Furthermore, some studies have even reported that it could worsen it. The main clinical guidelines for managing post-traumatic stress recommend not to practice psychological debriefing. These conclusions are relevant, particularly in the current pandemic context [50], which has facilitated potentially traumatic experiences among people – for example, facing the death of a significant person or favoring intrafamily violence associated with confinement.
This article synthesizes and critically discusses the secondary evidence and the recommendations of clinical guidelines on psychological debriefing, thus concluding the intervention benefit based on accumulated evidence. In light of these findings, psychological debriefing and associated interventions should be avoided in the management of acute trauma. We suggest exploring new forms of prevention and treatment of post-traumatic symptomatology based on scientific evidence.
Contributor roles
All authors contributed to the planning and writing of the original manuscript, participating in the writing of the Introduction, evidence synthesis, and discussion. MA, FL, and JM developed the description of the intervention. MA prepared Boxes 1 and 2. AM, UR, ES, and VV prepared tables 1 and 2.
Competing interests
The authors completed the ICMJE conflict of interest statement and declared that they received no funding for the conduct of this article; they have no financial relationships with organizations that may have an interest in the published article in the last three years; and they have no other relationships or activities that may influence the publication of the article. The forms can be requested by contacting the responsible author or the Editorial Committee of the Journal.
Funding
The authors declare that there were no external sources of funding.
Ethics
This study did not require evaluation by an ethical-scientific committee because it worked on secondary sources.
Provenance and peer review
Not commissioned. Externally peer-reviewed by three reviewers, double-blind
Language of submission
Spanish.

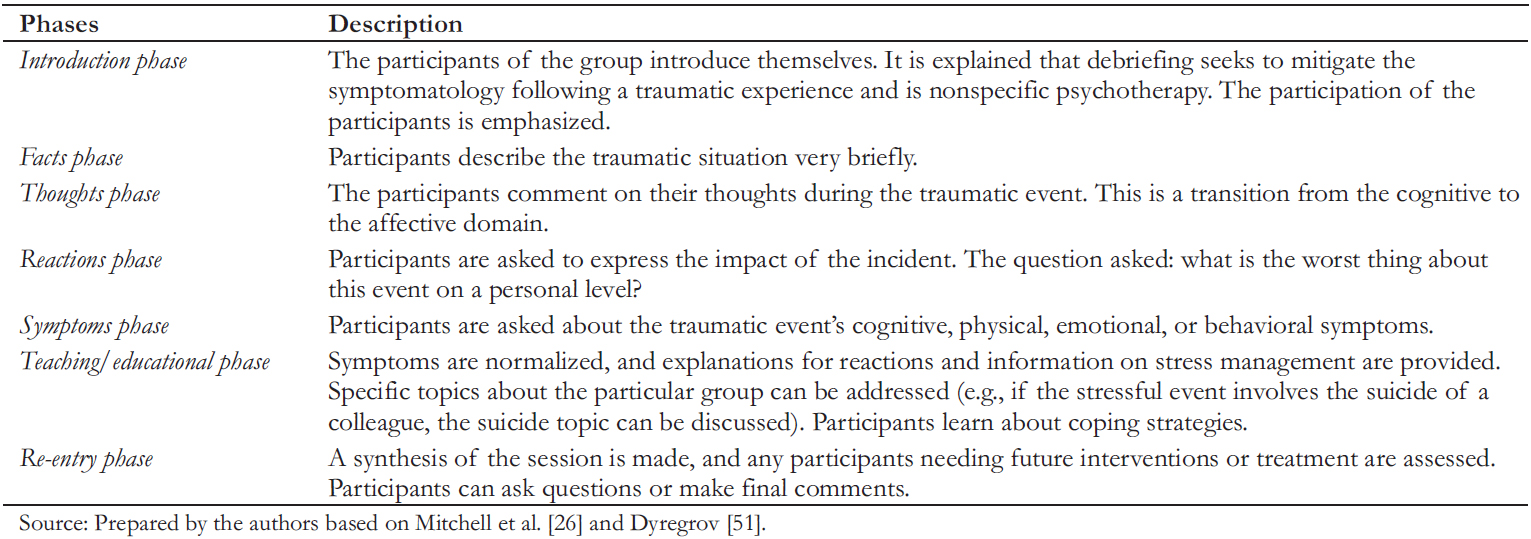 Table 1. Phases of psychological debriefing.
Table 1. Phases of psychological debriefing.

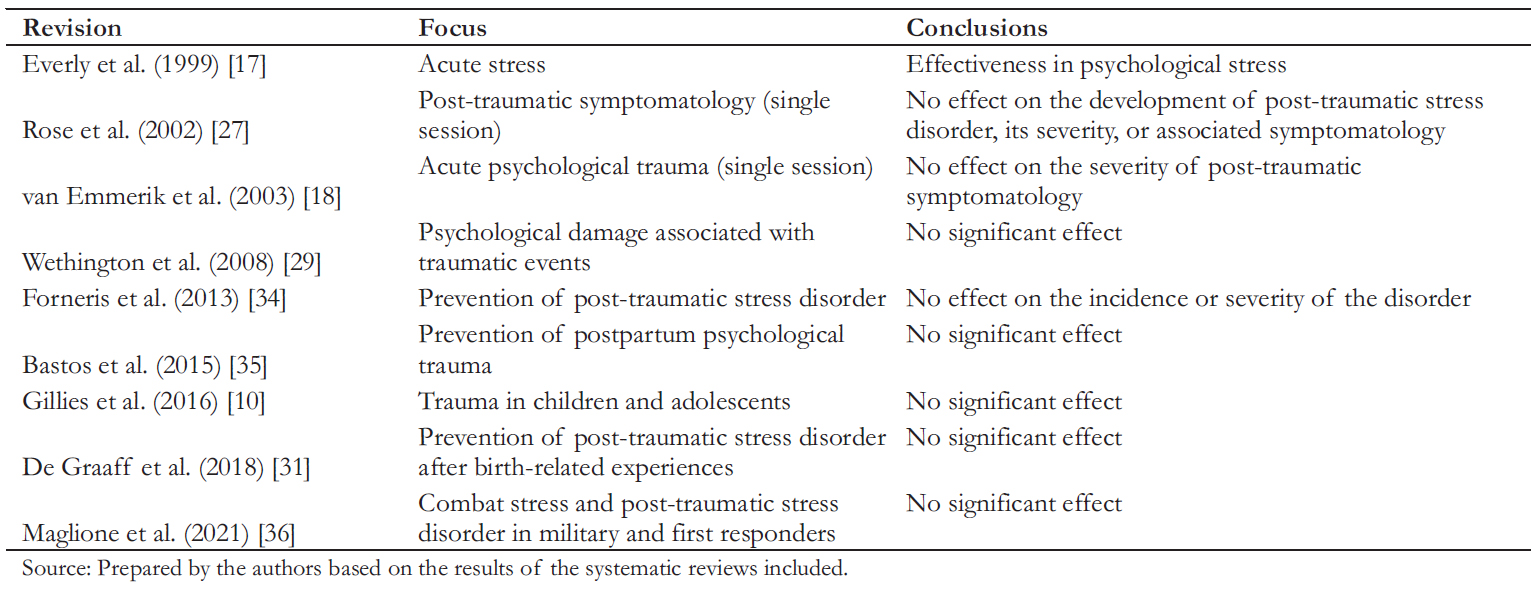 Table 2. Synthesis of the main findings of the systematic reviews.
Table 2. Synthesis of the main findings of the systematic reviews.

Stressful life situations can generate chronic symptomatology, so it is of great concern to analyze preventive strategies. Psychological debriefing is an intervention for acute trauma, which verbalizes perceptions, thoughts, and emotions experienced during a recent traumatic event. The evidence surrounding its efficacy is controversial. This article discusses the efficacy of psychological debriefing based on systematic reviews and clinical practice guidelines. In all, nine systematic reviews were included. Only one of them found that psychological debriefing effectively decreased psychological stress, while the remaining eight found no significant effects for outcomes such stress, depressive and anxious symptoms, or development and severity of post-traumatic stress disorder. Moreover, two clinical trials found that the intervention had a significantly deleterious effect. Another study found a worsening in the symptomatology associated with the event. Of the eight clinical practice guidelines incorporated, none recommended psychological debriefing as an intervention for acute trauma. Some phenomena could explain the lack of success of the intervention in the scientific evidence. The bioethical conditions related to the traumatic scenario hinder its research, and its lack of standardization makes its evaluation in clinical trials problematic. Other variables such as ethnicity, personality, culture, gender, and history of traumatic experiences have been little considered in research. Nevertheless, the intervention may hinder the adequate processing of traumatic memory and emotions. Current evidence is consistent in not recommending psychological debriefing as an intervention for acute trauma, so its management should avoid it. It is suggested to promote research on preventive interventions to develop chronic traumatic symptomatology.
 Autores:
Marcelo Arancibia[1,2], Fanny Leyton[1,3], Javier Morán[1,4], Andrea Muga[1,5], Ulises Ríos[1,6], Elisa Sepúlveda[1,3], Valentina Vallejo-Correa[1,7]
Autores:
Marcelo Arancibia[1,2], Fanny Leyton[1,3], Javier Morán[1,4], Andrea Muga[1,5], Ulises Ríos[1,6], Elisa Sepúlveda[1,3], Valentina Vallejo-Correa[1,7]

Citación: Arancibia M, Leyton F, Morán J, Muga A, Ríos U, Sepúlveda E, et al. Phycological debriefing in acute traumatic events: Evidence synthesis. Medwave 2022;22(1):e002538 doi: 10.5867/medwave.2022.01.002538
Fecha de envío: 27/10/2021
Fecha de aceptación: 20/12/2021
Fecha de publicación: 18/1/2022
Origen: No solicitado
Tipo de revisión: Con revisión por pares externa, por tres árbitros a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61 Suppl 5: 4–12. | Link |
Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61 Suppl 5: 4–12. | Link | Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PLoS One. 2013;8. | CrossRef |
Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, et al. A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: intentional and non-intentional traumatic events. PLoS One. 2013;8. | CrossRef | Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. The capacity of acute stress disorder to predict posttraumatic psychiatric disorders. J Psychiatr Res. 2012;46: 168–73. | CrossRef |
Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. The capacity of acute stress disorder to predict posttraumatic psychiatric disorders. J Psychiatr Res. 2012;46: 168–73. | CrossRef | Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC, Forbes D. A comparison of the capacity of DSM-IV and DSM-5 acute stress disorder definitions to predict posttraumatic stress disorder and related disorders. J Clin Psychiatry. 2015;76: 391–7. | CrossRef |
Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC, Forbes D. A comparison of the capacity of DSM-IV and DSM-5 acute stress disorder definitions to predict posttraumatic stress disorder and related disorders. J Clin Psychiatry. 2015;76: 391–7. | CrossRef | Green BL, Lindy JD, Grace MC, Leonard AC. Chronic posttraumatic stress disorder and diagnostic comorbidity in a disaster sample. J Nerv Ment Dis. 1992;180: 760–6. | CrossRef |
Green BL, Lindy JD, Grace MC, Leonard AC. Chronic posttraumatic stress disorder and diagnostic comorbidity in a disaster sample. J Nerv Ment Dis. 1992;180: 760–6. | CrossRef | Figueroa RA, Cortés PF, Accatino L, Sorensen R. Trauma psicológico en la atención primaria: orientaciones de manejo. Rev méd Chile. 2016;144: 643–655. | CrossRef |
Figueroa RA, Cortés PF, Accatino L, Sorensen R. Trauma psicológico en la atención primaria: orientaciones de manejo. Rev méd Chile. 2016;144: 643–655. | CrossRef | ISTSS Guidelines Committee. ISTSS Guidelines Position Paper on Complex PTSD in Adults [Internet. Oakbrook Terrace; 2018. | Link |
ISTSS Guidelines Committee. ISTSS Guidelines Position Paper on Complex PTSD in Adults [Internet. Oakbrook Terrace; 2018. | Link | Zlotnick C, Johnson J, Kohn R, Vicente B, Rioseco P, Saldivia S. Epidemiology of trauma, post-traumatic stress disorder (PTSD) and co-morbid disorders in Chile. Psychol Med. 2006;36: 1523–33. | CrossRef |
Zlotnick C, Johnson J, Kohn R, Vicente B, Rioseco P, Saldivia S. Epidemiology of trauma, post-traumatic stress disorder (PTSD) and co-morbid disorders in Chile. Psychol Med. 2006;36: 1523–33. | CrossRef | Norris FH, Murphy AD, Baker CK, Perilla JL, Rodriguez FG, Rodriguez J de JG. Epidemiology of trauma and posttraumatic stress disorder in Mexico. J Abnorm Psychol. 2003;112: 646–56. | CrossRef |
Norris FH, Murphy AD, Baker CK, Perilla JL, Rodriguez FG, Rodriguez J de JG. Epidemiology of trauma and posttraumatic stress disorder in Mexico. J Abnorm Psychol. 2003;112: 646–56. | CrossRef | Gillies D, Maiocchi L, Bhandari AP, Taylor F, Gray C, O’Brien L. Psychological therapies for children and adolescents exposed to trauma. Cochrane Database Syst Rev. 2016;10: CD012371. | CrossRef |
Gillies D, Maiocchi L, Bhandari AP, Taylor F, Gray C, O’Brien L. Psychological therapies for children and adolescents exposed to trauma. Cochrane Database Syst Rev. 2016;10: CD012371. | CrossRef | National Institute for Health and Care Excellence. Post- traumatic stress disorder. Evidence reviews for psychological, psychosocial and other non-pharmacological interventions for the prevention of PTSD in adults. London; 2018. | Link |
National Institute for Health and Care Excellence. Post- traumatic stress disorder. Evidence reviews for psychological, psychosocial and other non-pharmacological interventions for the prevention of PTSD in adults. London; 2018. | Link | World Health Organization. Guidelines for the Management of Conditions Specifically Related to Stress. Geneva; 2013. | Link |
World Health Organization. Guidelines for the Management of Conditions Specifically Related to Stress. Geneva; 2013. | Link | Organización Mundial de la Salud. Primera ayuda psicológica: Guía para trabajadores de campo. Ginebra; 2012. | Link |
Organización Mundial de la Salud. Primera ayuda psicológica: Guía para trabajadores de campo. Ginebra; 2012. | Link | Mitchell JT. When disaster strikes...the critical incident stress debriefing process. JEMS. 1983;8: 36–9. | Link |
Mitchell JT. When disaster strikes...the critical incident stress debriefing process. JEMS. 1983;8: 36–9. | Link | Bessoles P. Psicoterapia post-traumática: contribución a una teorización psicodinámica de defusing y debriefing psicológico. Subj y Procesos Cogn. 2006;9: 53–68. | Link |
Bessoles P. Psicoterapia post-traumática: contribución a una teorización psicodinámica de defusing y debriefing psicológico. Subj y Procesos Cogn. 2006;9: 53–68. | Link | Everly GS, Boyle SH, Lating JM. The effectiveness of psychological debriefing with vicarious trauma: a meta-analysis. Stress Med. 1999;15: 229–233. | CrossRef |
Everly GS, Boyle SH, Lating JM. The effectiveness of psychological debriefing with vicarious trauma: a meta-analysis. Stress Med. 1999;15: 229–233. | CrossRef | van Emmerik AAP, Kamphuis JH, Hulsbosch AM, Emmelkamp PMG. Single session debriefing after psychological trauma: a meta-analysis. Lancet. 2002;360: 766–71. | CrossRef |
van Emmerik AAP, Kamphuis JH, Hulsbosch AM, Emmelkamp PMG. Single session debriefing after psychological trauma: a meta-analysis. Lancet. 2002;360: 766–71. | CrossRef | Hawker DM, Durkin J, Hawker DSJ. To debrief or not to debrief our heroes: that is the question. Clin Psychol Psychother. 2011;18: 453–63. | CrossRef |
Hawker DM, Durkin J, Hawker DSJ. To debrief or not to debrief our heroes: that is the question. Clin Psychol Psychother. 2011;18: 453–63. | CrossRef | Bisson JI, Jenkins PL, Alexander J, Bannister C. Randomised controlled trial of psychological debriefing for victims of acute burn trauma. Br J Psychiatry. 1997;171: 78–81. | CrossRef |
Bisson JI, Jenkins PL, Alexander J, Bannister C. Randomised controlled trial of psychological debriefing for victims of acute burn trauma. Br J Psychiatry. 1997;171: 78–81. | CrossRef | Hobbs M, Mayou R, Harrison B, Worlock P. A randomised controlled trial of psychological debriefing for victims of road traffic accidents. BMJ. 1996;313: 1438–9. | CrossRef |
Hobbs M, Mayou R, Harrison B, Worlock P. A randomised controlled trial of psychological debriefing for victims of road traffic accidents. BMJ. 1996;313: 1438–9. | CrossRef | Santacruz J. Una revisión acerca del debriefing como intervención en crisis y para la prevención del TEPT (trastorno de estrés postraumático). Rev Colomb Psiquiatr. 2008;37: 198–205. | Link |
Santacruz J. Una revisión acerca del debriefing como intervención en crisis y para la prevención del TEPT (trastorno de estrés postraumático). Rev Colomb Psiquiatr. 2008;37: 198–205. | Link | Bisson JI, Brayne M, Ochberg FM, Everly GS. Early psychosocial intervention following traumatic events. Am J Psychiatry. 2007;164: 1016–9. | CrossRef |
Bisson JI, Brayne M, Ochberg FM, Everly GS. Early psychosocial intervention following traumatic events. Am J Psychiatry. 2007;164: 1016–9. | CrossRef | McNally RJ, Bryant RA, Ehlers A. Does Early Psychological Intervention Promote Recovery From Posttraumatic Stress? Psychol Sci Public Interest. 2003;4: 45–79. | CrossRef |
McNally RJ, Bryant RA, Ehlers A. Does Early Psychological Intervention Promote Recovery From Posttraumatic Stress? Psychol Sci Public Interest. 2003;4: 45–79. | CrossRef | Mitchell J, Everly Jr G. The scientific evidence for critical incident stress management. JEMS. 1997;22: 86–93. | Link |
Mitchell J, Everly Jr G. The scientific evidence for critical incident stress management. JEMS. 1997;22: 86–93. | Link | Mitchell J, Everly Jr G. Critical incident stress debriefing: An operations manual for CISD, defusing and other group crisis intervention services. Ellicott City: Chevron Publishing Cooperation; 2001. | Link |
Mitchell J, Everly Jr G. Critical incident stress debriefing: An operations manual for CISD, defusing and other group crisis intervention services. Ellicott City: Chevron Publishing Cooperation; 2001. | Link | Rose SC, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2002; CD000560. | CrossRef |
Rose SC, Bisson J, Churchill R, Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst Rev. 2002; CD000560. | CrossRef | Gillies D, Taylor F, Gray C, O’Brien L, D’Abrew N. Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents. Cochrane Database Syst Rev. 2012;12: CD006726. | CrossRef |
Gillies D, Taylor F, Gray C, O’Brien L, D’Abrew N. Psychological therapies for the treatment of post-traumatic stress disorder in children and adolescents. Cochrane Database Syst Rev. 2012;12: CD006726. | CrossRef | Wethington HR, Hahn RA, Fuqua-Whitley DS, Sipe TA, Crosby AE, Johnson RL, et al. The effectiveness of interventions to reduce psychological harm from traumatic events among children and adolescents: a systematic review. Am J Prev Med. 2008;35: 287–313. | CrossRef |
Wethington HR, Hahn RA, Fuqua-Whitley DS, Sipe TA, Crosby AE, Johnson RL, et al. The effectiveness of interventions to reduce psychological harm from traumatic events among children and adolescents: a systematic review. Am J Prev Med. 2008;35: 287–313. | CrossRef | Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G. A randomised controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. J Child Psychol Psychiatry. 2006;47: 127–34. | CrossRef |
Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G. A randomised controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. J Child Psychol Psychiatry. 2006;47: 127–34. | CrossRef | de Graaff LF, Honig A, van Pampus MG, Stramrood CAI. Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: a systematic review. Acta Obstet Gynecol Scand. 2018;97: 648–656. | CrossRef |
de Graaff LF, Honig A, van Pampus MG, Stramrood CAI. Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: a systematic review. Acta Obstet Gynecol Scand. 2018;97: 648–656. | CrossRef | Priest SR, Henderson J, Evans SF, Hagan R. Stress debriefing after childbirth: a randomised controlled trial. Medical Journal of Australia. 2003;178: 542–545. | CrossRef | Link |
Priest SR, Henderson J, Evans SF, Hagan R. Stress debriefing after childbirth: a randomised controlled trial. Medical Journal of Australia. 2003;178: 542–545. | CrossRef | Link | Gamble J, Creedy D, Moyle W, Webster J, McAllister M,DicksonP.Effectivenessof acounselingintervention after a traumatic childbirth: a randomized controlled trial. Birth. 2005;32: 11–9. | CrossRef |
Gamble J, Creedy D, Moyle W, Webster J, McAllister M,DicksonP.Effectivenessof acounselingintervention after a traumatic childbirth: a randomized controlled trial. Birth. 2005;32: 11–9. | CrossRef | Forneris CA, Gartlehner G, Brownley KA, Gaynes BN, Sonis J, Coker-Schwimmer E, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med. 2013;44: 635–50. | CrossRef |
Forneris CA, Gartlehner G, Brownley KA, Gaynes BN, Sonis J, Coker-Schwimmer E, et al. Interventions to prevent post-traumatic stress disorder: a systematic review. Am J Prev Med. 2013;44: 635–50. | CrossRef | Bastos MH, Furuta M, Small R, McKenzie-McHarg K, Bick D. Debriefing interventions for the prevention of psychological trauma in women following childbirth. Cochrane Database Syst Rev. 2015;2015: CD007194. | CrossRef |
Bastos MH, Furuta M, Small R, McKenzie-McHarg K, Bick D. Debriefing interventions for the prevention of psychological trauma in women following childbirth. Cochrane Database Syst Rev. 2015;2015: CD007194. | CrossRef | Maglione MA, Chen C, Bialas A, Motala A, Chang J, Akinniranye O, et al. Combat and Operational Stress Control Interventions and PTSD: A Systematic Review and Meta-Analysis. Mil Med. 2021. | CrossRef |
Maglione MA, Chen C, Bialas A, Motala A, Chang J, Akinniranye O, et al. Combat and Operational Stress Control Interventions and PTSD: A Systematic Review and Meta-Analysis. Mil Med. 2021. | CrossRef | Ministerio de Salud, Gobierno de Chile. Orientaciones para el manejo del Trastorno de Estrés Agudo. Santiago; 2019. | Link |
Ministerio de Salud, Gobierno de Chile. Orientaciones para el manejo del Trastorno de Estrés Agudo. Santiago; 2019. | Link | Association AP. Clinical Practice Guideline for the Treatment of PTSD. Washington DC; 2017. | Link |
Association AP. Clinical Practice Guideline for the Treatment of PTSD. Washington DC; 2017. | Link | Australia P, Centre for Posttraumatic Mental Health. Australian Guidelines for the Treatment of Acute Stress Disorder & Posttraumatic Stress Disorder. Melbourne; 2013. | Link |
Australia P, Centre for Posttraumatic Mental Health. Australian Guidelines for the Treatment of Acute Stress Disorder & Posttraumatic Stress Disorder. Melbourne; 2013. | Link | Department of Veterans’ Affairs - Department of Defense. VA/VOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. Washington DC; 2017. | Link |
Department of Veterans’ Affairs - Department of Defense. VA/VOD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. Washington DC; 2017. | Link | Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry. 2004;161: 3–31.
| Link |
Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry. 2004;161: 3–31.
| Link | Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive- compulsive disorders. BMC Psychiatry. 2014;14 Suppl 1. | CrossRef |
Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive- compulsive disorders. BMC Psychiatry. 2014;14 Suppl 1. | CrossRef | Arendt M, Elklit A. Effectiveness of psychological debriefing. Acta Psychiatr Scand. 2001;104: 423–37. | CrossRef |
Arendt M, Elklit A. Effectiveness of psychological debriefing. Acta Psychiatr Scand. 2001;104: 423–37. | CrossRef | British Psychological Society. British Psychological Society. Psychological debriefing: Professional practice board working party. BPS; 2002.
| Link |
British Psychological Society. British Psychological Society. Psychological debriefing: Professional practice board working party. BPS; 2002.
| Link | Seely MR. Psychological Debriefing May Not Be Clinically Effective: Implications for a Humanistic Approach to Trauma Intervention. The Journal of Humanistic Counseling, Education and Development. 2007;46: 172–182. | CrossRef |
Seely MR. Psychological Debriefing May Not Be Clinically Effective: Implications for a Humanistic Approach to Trauma Intervention. The Journal of Humanistic Counseling, Education and Development. 2007;46: 172–182. | CrossRef | MacDonald CM. Evaluation of stress debriefing interventions with military populations. Mil Med. 2003;168: 961–8.
| CrossRef |
MacDonald CM. Evaluation of stress debriefing interventions with military populations. Mil Med. 2003;168: 961–8.
| CrossRef | Bolwig TG. Debriefing after psychological trauma. Acta Psychiatr Scand. 1998;98: 169–70. | CrossRef |
Bolwig TG. Debriefing after psychological trauma. Acta Psychiatr Scand. 1998;98: 169–70. | CrossRef | Dyregrov A. Caring for helpers in disaster situations: psychological debriefing. Disaster Manag. 1989;2: 25–30. | Link |
Dyregrov A. Caring for helpers in disaster situations: psychological debriefing. Disaster Manag. 1989;2: 25–30. | Link | Salmon T. The care and treatment of mental diseases and war neuroses (“shell shock”) in the British Army. Bethesda: University Archives, Uniformed Services University of the Health Sciences; 1917.
| Link |
Salmon T. The care and treatment of mental diseases and war neuroses (“shell shock”) in the British Army. Bethesda: University Archives, Uniformed Services University of the Health Sciences; 1917.
| Link | Wessely S, Deahl M. Psychological debriefing is a waste of time. Br J Psychiatry. 2003;183: 12–4. | CrossRef |
Wessely S, Deahl M. Psychological debriefing is a waste of time. Br J Psychiatry. 2003;183: 12–4. | CrossRef |