 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: benzodiazepines, substance-related disorders, harm reduction
Benzodiazepines are widely used in primary health care, and their prolonged use is an important problem given the medical consequences particularly in older adults, such as dependence, cognitive impairment, and risk of falls, among others. Primary care doctors generally have few tools to help with managing withdrawal from benzodiazepines. We conducted a review of the best available evidence on practical strategies to avoid dependence at the time of the initial prescription, and to help the patient with prolonged and probably dependent use. We found ten relevant systematic reviews showing evidence in favor of the use of multifaceted prescription strategies, gradual dose reduction, standardized letters, standardized counseling, pharmacotherapy and cognitive behavioral psychotherapy. For benzodiazepine withdrawal, a simple strategy that can be effective and long-lasting is to inform patients of the need to reduce consumption, giving them in writing the withdrawal guideline, indicating the possible effects of withdrawal and its solution. Given the available evidence, an integrated and step-by-step model is proposed for the management of the benzodiazepine user, from prescription to withdrawal.
Benzodiazepines are widely used anxiolytic, sedative and hypnotic drugs [1],[2],[3]. The frequency of mental health pathologies at primary health care level and the chronic evolution of these make their use something usual and often prolonged [4]. There are different systematic reviews that have evaluated the role of benzodiazepines, standing out as coadjuvants in the initial phase of mood disorders [5] and for the management of seizures in anxiety disorders [6]. In both, there is no evidence that its use for more than four weeks is associated with benefits, but rather with known risks [7],[8],[9],[10],[11],[12],[13].
Some studies show that its withdrawal results in better health in older adults [14], however, it is not always easy. The pattern of gradual dose reduction is widely known as strategy, with varying success rates, which increase if it is associated with other strategies such as letters [15], interviews with standardized content [16], or cognitive behavioral therapy [17].
The present review aims to present an integrated, practical and updated strategy based on the best available evidence, to address withdrawal in the consumption of benzodiazepines in the patient with dependence, in primary health care.
We carried out a narrative (non-systematic) review of the literature, with the search for articles addressing the issue of withdrawal strategies for benzodiazepine consumption. We consulted MEDLINE/PubMed, Cochrane, Epistemonikos and Google Scholar databases. The term "benzodiazepine" was used alone or in conjunction with other terms such as "dependence", "withdrawal", and others. The inclusion criteria were: review articles, systematic or not; limited to english, outpatient management, with participants older than 15 years, and not prior to 2006. The results were analyzed and grouped by type of intervention in five large groups: interventions during prescription, gradual dose reduction, psychosocial interventions, pharmacotherapy and psychotherapy. With this information, we created a management proposal for the patient with benzodiazepine dependence.
We found ten relevant systematic reviews that addressed strategies of withdrawal and prescribing control of benzodiazepines [18],[19],[20],[21],[22],[23],[24],[25],[26],[27]. Two systematic reviews evaluated strategies used during the prescription to decrease the chronic use of benzodiazepines [22],[23]; three systematic reviews evaluated the use of gradual dose reduction [19],[20],[24]; five evaluated different psychosocial interventions (education, certified letters, e-counseling, supervised gradual dose reduction, standardized medical counseling, motivational interview, minimal intervention and relaxation techniques) [19],[20],[21],[25],[27]. Seven systematic reviews evaluated the use of pharmacological replacement [18],[19],[20],[23],[24],[26],[27]. Finally, four systematic reviews evaluated psychotherapy [19],[23],[24],[25].
Details of the results reported in each systematic review (type of intervention, number of primary studies, number of patients involved, point estimator, confidence interval) grouped by type of intervention, are presented in Table 1.
Table 1. Results reported by systematic reviews
1. Strategies used during the prescription of benzodiazepines
Fisher et al. evaluated benzodiazepine prescription monitoring programs in the State of New York, concluding that their use decreases the general use of the drugs [22]. On the other hand, Gould et al. evaluated interventions carried out at the time of benzodiazepines prescription such as education, counseling, review of pharmacological aspects and feedback on the prescription to the prescribing physician. They concluded that the use of several of these interventions simultaneously would be beneficial for the decrease in the number of chronic users of benzodiazepines, however, they found no evidence in favor of the use of a single strategy [22].
2. Gradual dose reduction for benzodiazepines withdrawal
Voshaar et al. and Paar et al. evaluated the use of a gradual dose reduction scheme supervised by a doctor or psychologist versus no intervention, concluding a benefit in favor of gradual dose reduction (both reported the same primary study) [20]. Paquin et al. (2014) concluded a benefit of the use of gradual dose reductiont in older adult population [24].
3. Psychosocial intervention for benzodiazepines withdrawal
Voshaar et al. compared the use of minimal intervention (use of letters or group meetings for the recommendation of cessation of benzodiazepines) with non-intervention, concluding a benefit in favor of these interventions [19]. Parr et al. compared psychological interventions (relaxation training, education on abstinence from benzodiazepines and non-medical strategies for the management of insomnia) with non-intervention, concluding a benefit in favor of these strategies [20]. Mugunthan et al. compared the use of minimal interventions (use of letters to the patient, counseling, monthly written notes in which abstinence was urged and / or self-help booklets) with allowing to continue the use of benzodiazepines, concluding a benefit for the interventions [21].
Darker et al. [25], in a Cochrane review, includes different comparisons of minimal interventions where it is worth noting that the standardized counseling by a family doctor associated with a gradual dose reduction would be superior to the usual counseling. However, this benefit would be lost at three years of follow-up. No benefit from the use of non-standardized motivational letters (standardized were better than non-standardized letters); or from the use of motivational interviewing, relaxation techniques and e-counseling [20] was also prominent in this review. Finally, Reeve et al. found favorable results with the use of such strategies as educational empowerment brochures, information on the gradual dose reduction, information on long-term adverse effects and instruction for cessation,in the population of adults over 6 and 12 months of follow-up [20].
4. Pharmacological intervention for benzodiazepines withdrawal
Denis et al. analyzed the use of different drugs for benzodiazepines withdrawal, finding good results with the use of carbamazepine associated with gradual dose reduction and concluded there was no benefit with the use of propanolol, hydroxyzine, progesterone, and antidepressants tricycles [18]. Voshaar et al. concluded that the use of imipramine associated with gradual dose reduction would be beneficial for the cessation of use of benzodiazepines compared to the gradual dose reduction. However, no benefit was reported with the use of propanolol, buspirone, carbamazepine and trazodone [19]. Parr et al. concluded that gradual dose reduction associated with paroxetine, melatonin, trazadone and valproic acid [20] were beneficial. Gould et al. (2014) concluded an absence of benefit from adding pharmacological substitution to gradual dose reduction compared with placebo [23]. Paquin et al. concluded that adding pharmacological substitution in the elderly population [24] would be beneficial. Wright et al. pointed out that adding melatonin to supervised gradual dose reduction would not imply any benefit [26]. Finally, Reeve et al. reported good results for the use of melatonin, lormetazepam and trazodone in the elderly population [27].
5. Psychotherapy
Voshaar et al. concluded that the use of cognitive behavioral therapy would be positive [19]. Gould et al. concluded that psychotherapy associated with supervised abstinence, meant a benefit that decreased (remaining statistically significant) at 3 and 12 months [23]. Paquin et al. concluded that psychotherapy had good results in the elderly population [24]. Finally, a benefit of adding cognitive behavioral psychotherapy to the gradual dose reduction was found in the Cochrane review by Darker et al. This benefit lost its statistical significance at a follow-up of more than 6 months [25].
Lifetime prevalence for the consumption of these drugs lies between 0.2 and 8% worldwide [28]. In a recent literature review on the population of elderly Latinos treated in primary health care, the frequency of consumption at least once in their life fluctuated between 25% and 61% [29]. A study conducted in primary health care population in Chile, reported an annual prevalence of 26%, with a consumption over one year in 11% of the respondents [30].
The Diagnostic and Statistical Manual of Mental Disorders-Text Revised-IV (DSM-IV-TR) defines dependence as a maladaptive pattern of substance use that leads to clinically significant impairment or discomfort [31]. However, the American Psychiatric Association (APA) in the Diagnostic and Statistical Manual of Mental Disorders-V (DSM-V) recently unified the concepts of substance abuse and dependence, creating the concept of substance use disorder [32]. According to the literature, benzodiazepines consumption for more than four to six weeks is an important risk factor for dependence [33]. Because of this, different treatments have emerged that favor the cessation of the chronic consumption of these drugs [34],[35],[36],[37].
As a summary of the evidence presented, we found reports in the literature that showed benefits for the use of combined techniques at the time of prescription, the use of gradual dose reduction schemes, the use of letters of motivation, the use of standardized counseling and the use of psychotherapy. There is evidence of low level of certainty (isolated and contradictory randomized trials) that showed a significant benefit for the use of drugs such as carbamazepine, imipramine, paroxetine, melatonin, trazodone, valproic acid and lormetazepam. From the analysis of the evidence, it was also possible to conclude that, all together, primary studies would have a moderate risk of bias. Furthermore, within the limitations of the summarized evidence, it was found that the control treatment was not always detailed but repored as usual therapy (treat as usual), making difficult the comparison between systematic reviews.
On the other hand, many of the disagreements among the systematic reviews could be due to the fact that, when comparing the primary reports, each one would use different studies to perform the respective meta-analyses. In sum, using the available evidence, the following strategy was designed for the prescription, monitoring and cessation of chronic consumption and benzodiazepine abuse (Figure 1).
Step 0 - Prescription (apply in initial prescription of benzodiazepines):
The objective of this first stage is to reduce the possibility of incidence of chronic users or patients with benzodiazepine consumption disorder. It includes the following strategies:
a) Prescription of benzodiazepines must be restricted to a maximum of four weeks, for psychiatric disorders.
b) It is suggested to educate the patient at the time of the prescription about the adverse effects and the risk of consumption disorder from its chronic use.
c) Deliver, in print, along with benzodiazepines, a brief summary of the adverse effects of prolonged use of these drugs.
d) At the time of prescribing benzodiazepines the doctor will have a reminder, either at desk or computer, which will say: "benzodiazepines are not, according to current evidence, indicated for leep disorders" and "according to current evidence, benzodiazepines do not report benefit after four weeks of use in mood and anxiety disorders”
e) At the time of prescribing benzodiazepines, the doctor will have a reminder either on the desk or on the computer that will read: "The benzodiazepines are not, according to the current evidence, indicated for sleep disorders", "the benzodiazepines do not report benefit, according to the current evidence, after four weeks of use in mood and anxiety disorders.”
e) As part of the prescription of benzodiazepines, during week three and four, it is suggested to have gradual reduction schemes.
Step 1. Non face-to-face consumption cessation (to apply in patients with a consumption greater than 4 weeks):
The objective of this stage is to get people to make the decision motivated by their desire for self-care guided by brief information about the benefits of stopping consumption and a written guide on how to do it. In this way, we will try to reduce the chronic use of benzodiazepines without involving hours of doctor's attention that can be used in the management of the underlying pathology. This stage consists in the delivery of a letter with the agreed dose of benzodiazepines on behalf of the medical team of the health center, suggesting cessation of use, in a "standardized letter" (Table 2). Along with this letter, a gradual dose reduction pattern suggesting a 25% decrease of the initial dose each week is also delivered (optimal scenario).
Step 2 - Face-to-face withdrawal consumption through minimum intervention and supervised gradual dose reduction (from the eighth week):
The objective of this step is to achieve cessation with minimal non-standardized face-to-face intervention and the controlled prescription of drugs. In this stage, the patient has already received education at the time of the initial prescription, has received at least one letter at the time of withdrawal of the drug, and this last intervention is intended to end the consumption gradually.
Step 3 - Face-to-face withdrawal consumption through standardized counseling and supervised gradual dose reduction (since the twelfth week):
The objective of this stage is achieving cessation of benzodiazepine consumption using the maximum resources available in the health center. In this stage, detailed standardized counseling (Table 3) is applied to encourage the motivation for cessation of benzodiazepine use. As part of this stage, patients receive a gradual dose reduction scheme (Similar to step 1). Substitution drugs may also considered in this stage (Table 4).
Table 3. Standardized Counseling.
Table 4. Substitution drugs in the cessation of benzodiazepines.
Step 4 - Specialist referral for patients refractory to the previous steps (from the twelfth week or according to the doctor's criteria):
The objective of this stage is that, having a patient motivated to cease, and exceeding the resources available in the health center, the patient will be referred to the mental health center for specialized management. This is because psychotherapy is the treatment with the highest evidence level for benzodiazepines withdrawal. However, because it is an expensive and scarce resource, it is left for patients who are refractory to less complexity management, and as the cusp of management proposed in this protocol.
To stop prescribing treatments to patients when they no longer need them is an essential part of a good medical exercise. There is a lot of scientific evidence about how to start a treatment, but there is very little about the best way to stop prescribing. This would not be important if the withdrawal of drugs, when they are unnecessary, was a routine activity.
The inertia of the prescription establishes a perfect framework to understand why some prescriptions become chronic, despite being recommended only in short treatments. Some classic examples of this reality are the prescription of benzodiazepines, nonsteroidal anti-inflammatory drugs (including COX-2), proton pump inhibitors (PPI) and analgesics [36].
The chronic use of benzodiazepines presents different adverse effects, among which dementia, the risk of falling and fractures, traffic accidents and upheaval by consumption of these substances stand out. Hence, several meta-analyses have compared the effectiveness of different withdrawal strategies for benzodiazepines.
It is observed that any type of intervention, even the simplest to implement (letter, talk or interview), improve the results obtained compared to routine performance. In general, the best results are obtained with an intervention to which a psychotherapy technique is added, OR = 5.06 (95% CI: 2.68 to 9.57) [23]. The minimal interventions were also effective, although to a lesser extent, OR = 1.37 (95% CI: 1.1 to 1.72).
In one study, 258 primary care patients with prolonged treatment (more than three months), who had ceased consumption after receiving a single "letter of interruption" by their family doctor (measured at three months after delivery), were allowed medical consultations on the subject and followed for 10 years. At 21 months, 59.8% remained abstinent and 58.8% after 10 years. This study also showed that probabilities of success in abstinence are not related to less time of previous consumption, use of basic antidepressants or type of benzodiazepines [37].
On the other hand, the use of drugs did not show significant differences compared with routine interventions, OR = 1.31 (95% CI: 0.68 to 2.53), which is why they were not included in the proposed strategy [23].
It is important to bear in mind that the currently available evidence does not allow us to have a high certainty that this will not change in the future, this is especially true for the use of pharmacological replacement. Thus, we propose an effective discontinuation strategy, at a minimum cost, and with a low need for professional time, both of which are relevant issues in the primary care setting.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Acknowledgements
The authors would like to thank Dr. Pamela Rojas for her advice in carrying out this work.
Declaration of conflicts of interest
The authors have completed the ICMJE Conflict of Interest declaration form, and declare that they have not received funding for the report; have no financial relationships with organizations that might have an interest in the published article in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the author responsible or the editorial management of the Journal.
Financing
The authors state that there were no external sources of funding.

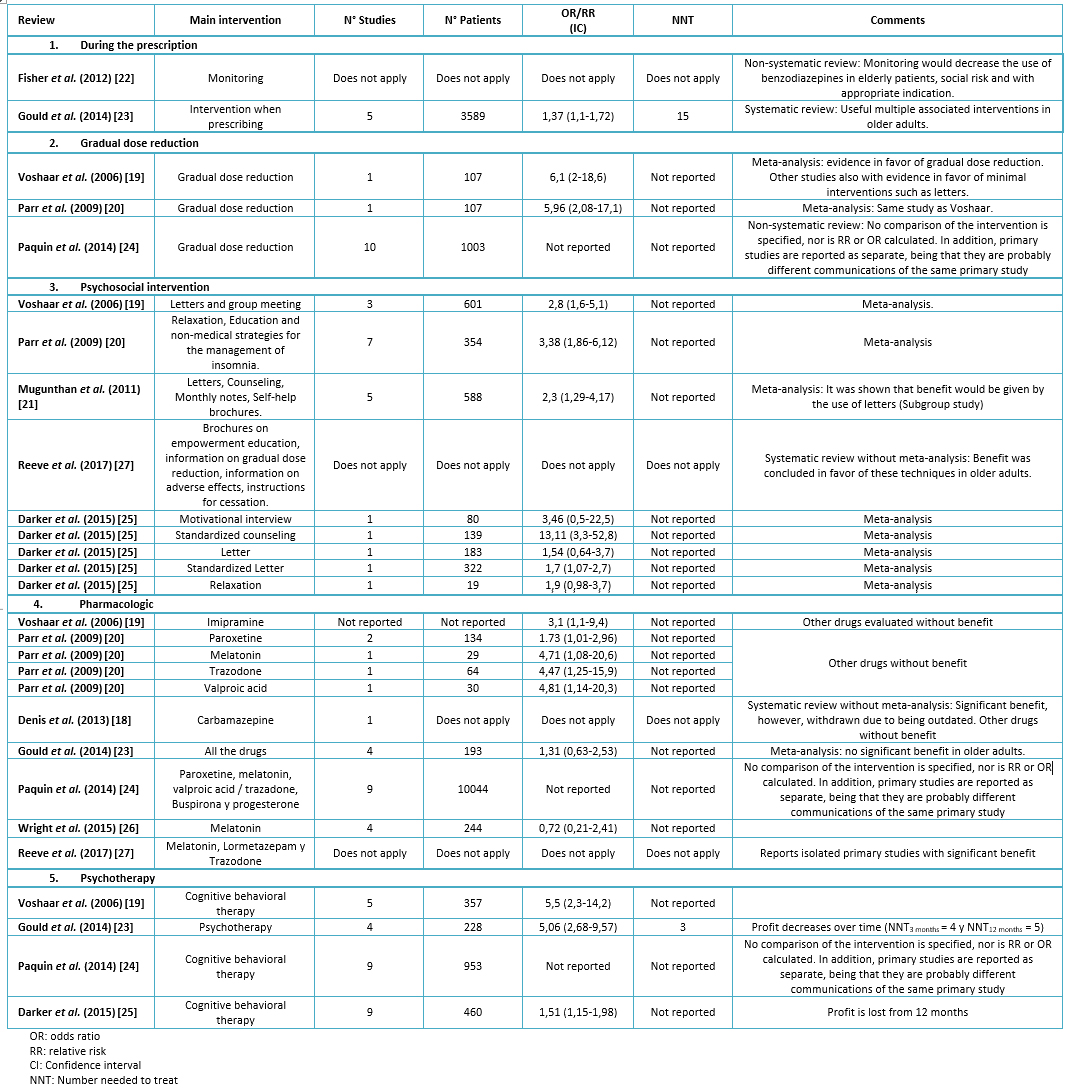 Table 1. Results reported by systematic reviews
Table 1. Results reported by systematic reviews

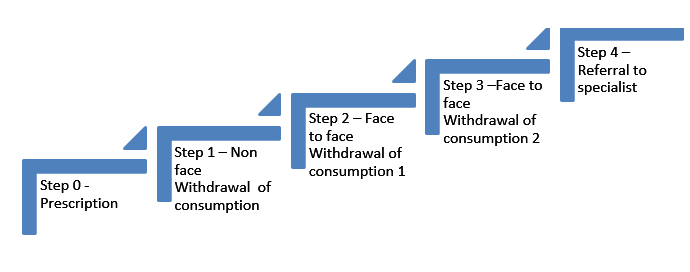 Figure 1. Strategy for the prescription, monitoring and cessation of chronic consumption and abuse of benzodiazepines.
Figure 1. Strategy for the prescription, monitoring and cessation of chronic consumption and abuse of benzodiazepines.

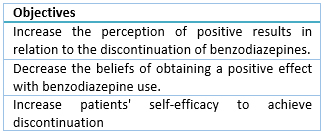 Table 2. Standarized Letter.
Table 2. Standarized Letter.

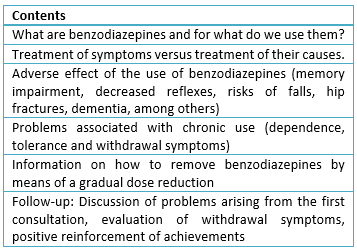 Table 3. Standardized Counseling.
Table 3. Standardized Counseling.

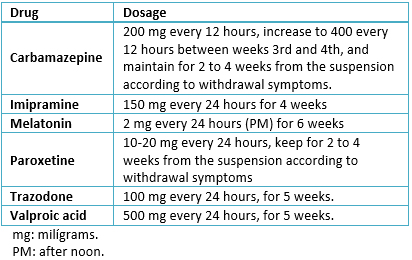 Table 4. Substitution drugs in the cessation of benzodiazepines.
Table 4. Substitution drugs in the cessation of benzodiazepines.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Benzodiazepines are widely used in primary health care, and their prolonged use is an important problem given the medical consequences particularly in older adults, such as dependence, cognitive impairment, and risk of falls, among others. Primary care doctors generally have few tools to help with managing withdrawal from benzodiazepines. We conducted a review of the best available evidence on practical strategies to avoid dependence at the time of the initial prescription, and to help the patient with prolonged and probably dependent use. We found ten relevant systematic reviews showing evidence in favor of the use of multifaceted prescription strategies, gradual dose reduction, standardized letters, standardized counseling, pharmacotherapy and cognitive behavioral psychotherapy. For benzodiazepine withdrawal, a simple strategy that can be effective and long-lasting is to inform patients of the need to reduce consumption, giving them in writing the withdrawal guideline, indicating the possible effects of withdrawal and its solution. Given the available evidence, an integrated and step-by-step model is proposed for the management of the benzodiazepine user, from prescription to withdrawal.
 Autores:
Josefina Aguiluz[1], Matías Álvarez[1], Eduardo Pimentel[1], Carolina Abarca[2,3], Philippa Moore[3]
Autores:
Josefina Aguiluz[1], Matías Álvarez[1], Eduardo Pimentel[1], Carolina Abarca[2,3], Philippa Moore[3]

Citación: Aguiluz J, Álvarez M, Pimentel E, Abarca C, Moore P. How to face a patient with benzodiazepine dependence in primary health care? Strategies for withdrawal. Medwave 2018 Ene-Feb;17(1):e7159 doi: 10.5867/medwave.2018.01.7159
Fecha de envío: 12/11/2017
Fecha de aceptación: 8/1/2018
Fecha de publicación: 30/1/2018
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Smith TA. Type A gamma-aminobutyric acid (GABAA) receptor subunits and benzodiazepine binding: significance to clinical syndromes and their treatment. Br J Biomed Sci. 2001;58(2):111-21. | PubMed |
Smith TA. Type A gamma-aminobutyric acid (GABAA) receptor subunits and benzodiazepine binding: significance to clinical syndromes and their treatment. Br J Biomed Sci. 2001;58(2):111-21. | PubMed | Baldwin DS, Aitchison K, Bateson A, Curran HV, Davies S, Leonard B, et al. Benzodiazepines: risks and benefits. A reconsideration. J Psychopharmacol. 2013 Nov;27(11):967-71.
| CrossRef | PubMed |
Baldwin DS, Aitchison K, Bateson A, Curran HV, Davies S, Leonard B, et al. Benzodiazepines: risks and benefits. A reconsideration. J Psychopharmacol. 2013 Nov;27(11):967-71.
| CrossRef | PubMed | Davies J, Rae TC, Montagu L. Long-term benzodiazepine and Z-drugs use in the UK: a survey of general practice. Br J Gen Pract. 2017 Sep;67(662):e609-e613. | CrossRef | PubMed |
Davies J, Rae TC, Montagu L. Long-term benzodiazepine and Z-drugs use in the UK: a survey of general practice. Br J Gen Pract. 2017 Sep;67(662):e609-e613. | CrossRef | PubMed | Furukawa TA, Streiner DL, Young LT. Antidepressant plus benzodiazepine for major depression. Cochrane Database Syst Rev. 2001;(2):CD001026. | PubMed |
Furukawa TA, Streiner DL, Young LT. Antidepressant plus benzodiazepine for major depression. Cochrane Database Syst Rev. 2001;(2):CD001026. | PubMed | Bighelli I, Trespidi C, Castellazzi M, Cipriani A, Furukawa TA, Girlanda F, et al. Antidepressants and benzodiazepines for panic disorder in adults. Cochrane Database Syst Rev. 2016 Sep 12;9:CD011567. | PubMed |
Bighelli I, Trespidi C, Castellazzi M, Cipriani A, Furukawa TA, Girlanda F, et al. Antidepressants and benzodiazepines for panic disorder in adults. Cochrane Database Syst Rev. 2016 Sep 12;9:CD011567. | PubMed | Xing D, Ma XL, Ma JX, Wang J, Yang Y, Chen Y. Association between use of benzodiazepines and risk of fractures: a meta-analysis. Osteoporos Int. 2014 Jan;25(1):105-20. | CrossRef | PubMed |
Xing D, Ma XL, Ma JX, Wang J, Yang Y, Chen Y. Association between use of benzodiazepines and risk of fractures: a meta-analysis. Osteoporos Int. 2014 Jan;25(1):105-20. | CrossRef | PubMed | Donnelly K, Bracchi R, Hewitt J, Routledge PA, Carter B. Benzodiazepines, Z-drugs and the risk of hip fracture: A systematic review and meta-analysis. PLoS One. 2017 Apr 27;12(4):e0174730. | CrossRef | PubMed |
Donnelly K, Bracchi R, Hewitt J, Routledge PA, Carter B. Benzodiazepines, Z-drugs and the risk of hip fracture: A systematic review and meta-analysis. PLoS One. 2017 Apr 27;12(4):e0174730. | CrossRef | PubMed | Rapoport MJ, Lanctôt KL, Streiner DL, Bédard M, Vingilis E, Murray B, et al. Benzodiazepine use and driving: a meta-analysis. J Clin Psychiatry. 2009 Apr 21;70(5):663-73. | CrossRef | PubMed |
Rapoport MJ, Lanctôt KL, Streiner DL, Bédard M, Vingilis E, Murray B, et al. Benzodiazepine use and driving: a meta-analysis. J Clin Psychiatry. 2009 Apr 21;70(5):663-73. | CrossRef | PubMed | Thomas RE. Benzodiazepine use and motor vehicle accidents. Systematic review of reported association. Can Fam Physician. 1998 Apr;44:799-808. | PubMed |
Thomas RE. Benzodiazepine use and motor vehicle accidents. Systematic review of reported association. Can Fam Physician. 1998 Apr;44:799-808. | PubMed | Zhong G, Wang Y, Zhang Y, Zhao Y. Association between Benzodiazepine Use and Dementia: A Meta-Analysis. PLoS One. 2015 May 27;1(5):e0127836. | CrossRef | PubMed |
Zhong G, Wang Y, Zhang Y, Zhao Y. Association between Benzodiazepine Use and Dementia: A Meta-Analysis. PLoS One. 2015 May 27;1(5):e0127836. | CrossRef | PubMed | Zandstra SM, Furer JW, van de Lisdonk EH, van't HM, Bor JH, van Weel C, et al. Different study criteria affect the prevalence of benzodiazepine use. Soc Psychiatry Psychiatr Epidemiol. 2002 Mar;37(3):139-44. | PubMed |
Zandstra SM, Furer JW, van de Lisdonk EH, van't HM, Bor JH, van Weel C, et al. Different study criteria affect the prevalence of benzodiazepine use. Soc Psychiatry Psychiatr Epidemiol. 2002 Mar;37(3):139-44. | PubMed | Danza Á, Cristiani F, Tamosiunas G. Riesgos asociados al uso de Benzodiazepinas: Benzodiazepine-related risks. Arch Med In. 2009 Dic;31(4):103-7. | Link |
Danza Á, Cristiani F, Tamosiunas G. Riesgos asociados al uso de Benzodiazepinas: Benzodiazepine-related risks. Arch Med In. 2009 Dic;31(4):103-7. | Link | Curran HV, Collins R, Fletcher S, Kee SC, Woods B, Iliffe S. Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life. Psychol Med. 2003 Oct;33(7):1223-37. | PubMed |
Curran HV, Collins R, Fletcher S, Kee SC, Woods B, Iliffe S. Older adults and withdrawal from benzodiazepine hypnotics in general practice: effects on cognitive function, sleep, mood and quality of life. Psychol Med. 2003 Oct;33(7):1223-37. | PubMed | Gorgels WJ1, Oude Voshaar RC, Mol AJ, van de Lisdonk EH, van Balkom AJ, van den Hoogen HJ, et al. Discontinuationof long-term benzodiazepine use by sending a letter to users infamily practise: a prospective controlled intervention studyDrug Alcohol Depend. 2005 Apr 4;78(1):49-56. | CrossRef | PubMed |
Gorgels WJ1, Oude Voshaar RC, Mol AJ, van de Lisdonk EH, van Balkom AJ, van den Hoogen HJ, et al. Discontinuationof long-term benzodiazepine use by sending a letter to users infamily practise: a prospective controlled intervention studyDrug Alcohol Depend. 2005 Apr 4;78(1):49-56. | CrossRef | PubMed | Vicens C, Fiol F, Llobera J, Campoamor F, Mateu C, Alegret S, Socías I. Withdrawal from long-term benzodiazepine use: randomised trial in family practice. Br J Gen Pract. 2006 Dec;56(533):958-63. | PubMed |
Vicens C, Fiol F, Llobera J, Campoamor F, Mateu C, Alegret S, Socías I. Withdrawal from long-term benzodiazepine use: randomised trial in family practice. Br J Gen Pract. 2006 Dec;56(533):958-63. | PubMed | Voshaar RC, Gorgels WJ, Mol AJ, van Balkom AJ, van de Lisdonk EH, Breteler MH, et al. Tapering off long-term benzodiazepine use with or without group cognitive-behavioral therapy: three-condition, randomized controlled trial. Br J Psychiatry. 2003 Jun;182:498-504. | PubMed |
Voshaar RC, Gorgels WJ, Mol AJ, van Balkom AJ, van de Lisdonk EH, Breteler MH, et al. Tapering off long-term benzodiazepine use with or without group cognitive-behavioral therapy: three-condition, randomized controlled trial. Br J Psychiatry. 2003 Jun;182:498-504. | PubMed | Denis C, Fatséas M, Lavie E, Auriacombe M. Pharmacological interventions for benzodiazepine mono-dependence management in outpatient settings. Cochrane Database Syst Rev. 2006 Jul 19;(3):CD005194. | PubMed |
Denis C, Fatséas M, Lavie E, Auriacombe M. Pharmacological interventions for benzodiazepine mono-dependence management in outpatient settings. Cochrane Database Syst Rev. 2006 Jul 19;(3):CD005194. | PubMed | Voshaar RC, Couvée JE, van Balkom AJ, Mulder PG, Zitman FG. Strategies for discontinuing long-term benzodiazepine use: meta-analysis. Br J Psychiatry. 2006 Sep;189:213-20. | PubMed |
Voshaar RC, Couvée JE, van Balkom AJ, Mulder PG, Zitman FG. Strategies for discontinuing long-term benzodiazepine use: meta-analysis. Br J Psychiatry. 2006 Sep;189:213-20. | PubMed | Parr JM, Kavanagh DJ, Cahill L, Mitchell G, McD Young R. Effectiveness of current treatment approaches for benzodiazepine discontinuation: a meta-analysis. Addiction. 2009 Jan;104(1):13-24. | CrossRef | PubMed |
Parr JM, Kavanagh DJ, Cahill L, Mitchell G, McD Young R. Effectiveness of current treatment approaches for benzodiazepine discontinuation: a meta-analysis. Addiction. 2009 Jan;104(1):13-24. | CrossRef | PubMed | Mugunthan K, McGuire T, Glasziou P. Minimal interventions to decrease long-term use of benzodiazepines in primary care: a systematic review and meta-analysis. Br J Gen Pract. 2011 Sep;61(590):e573-8. | CrossRef | PubMed |
Mugunthan K, McGuire T, Glasziou P. Minimal interventions to decrease long-term use of benzodiazepines in primary care: a systematic review and meta-analysis. Br J Gen Pract. 2011 Sep;61(590):e573-8. | CrossRef | PubMed | Fisher J, Sanyal C, Frail D, Sketris I. The intended and unintended consequences of benzodiazepine monitoring programmes: a review of the literature. J Clin Pharm Ther. 2012 Feb;37(1):7-21. | CrossRef | PubMed |
Fisher J, Sanyal C, Frail D, Sketris I. The intended and unintended consequences of benzodiazepine monitoring programmes: a review of the literature. J Clin Pharm Ther. 2012 Feb;37(1):7-21. | CrossRef | PubMed | Gould RL, Coulson MC, Patel N, Highton-Williamson E, Howard RJ. Interventions for reducing benzodiazepine use in older people: meta-analysis of randomised controlled trials. Br J Psychiatry. 2014 Feb;204(2):98-107. | CrossRef | PubMed |
Gould RL, Coulson MC, Patel N, Highton-Williamson E, Howard RJ. Interventions for reducing benzodiazepine use in older people: meta-analysis of randomised controlled trials. Br J Psychiatry. 2014 Feb;204(2):98-107. | CrossRef | PubMed | Paquin AM, Zimmerman K, Rudolph JL. Risk versus risk: a review of benzodiazepine reduction in older adults. Expert Opin Drug Saf. 2014 Jul;13(7):919-34. | CrossRef | PubMed |
Paquin AM, Zimmerman K, Rudolph JL. Risk versus risk: a review of benzodiazepine reduction in older adults. Expert Opin Drug Saf. 2014 Jul;13(7):919-34. | CrossRef | PubMed | Darker CD, Sweeney BP, Barry JM, Farrell MF, Donnelly-Swift E. Psychosocial interventions for benzodiazepine harmful use, abuse or dependence. Cochrane Database Syst Rev. 2015;(5):CD009652. | PubMed |
Darker CD, Sweeney BP, Barry JM, Farrell MF, Donnelly-Swift E. Psychosocial interventions for benzodiazepine harmful use, abuse or dependence. Cochrane Database Syst Rev. 2015;(5):CD009652. | PubMed | Wright A, Diebold J, Otal J, Stoneman C, Wong J, Wallace C, et al. The Effect of Melatonin on Benzodiazepine Discontinuation and Sleep Quality in Adults Attempting to Discontinue Benzodiazepines: A Systematic Review and Meta-Analysis.Drugs Aging. 2015 Dec;32(12):1009-18. | CrossRef | PubMed |
Wright A, Diebold J, Otal J, Stoneman C, Wong J, Wallace C, et al. The Effect of Melatonin on Benzodiazepine Discontinuation and Sleep Quality in Adults Attempting to Discontinue Benzodiazepines: A Systematic Review and Meta-Analysis.Drugs Aging. 2015 Dec;32(12):1009-18. | CrossRef | PubMed | Reeve E, Ong M, Wu A, Jansen J, Petrovic M, Gnjidic D. A systematic review of interventions to deprescribe benzodiazepines and other hypnotics among older people. EurJ Clin Pharmacol. 2017 Aug;73(8):927-935. | CrossRef | PubMed |
Reeve E, Ong M, Wu A, Jansen J, Petrovic M, Gnjidic D. A systematic review of interventions to deprescribe benzodiazepines and other hypnotics among older people. EurJ Clin Pharmacol. 2017 Aug;73(8):927-935. | CrossRef | PubMed | Stillwell G, Fountain J. Benzodiazepine use-a report of a survey of benzodiazepine consumption in the member countries of the Pompidou group. Geneva: World Health Organization. 2002. | Link |
Stillwell G, Fountain J. Benzodiazepine use-a report of a survey of benzodiazepine consumption in the member countries of the Pompidou group. Geneva: World Health Organization. 2002. | Link | Gómez S, León T, Macuer M, Alves M, Ruiz S. [Benzodiazepine use in elderly population in Latin America]. Rev Med Chil. 2017 Mar;145(3):351-359. | CrossRef | PubMed |
Gómez S, León T, Macuer M, Alves M, Ruiz S. [Benzodiazepine use in elderly population in Latin America]. Rev Med Chil. 2017 Mar;145(3):351-359. | CrossRef | PubMed | Galleguillos T, Risco L, Garay JL, González M, Vogel, M. Tendencia del uso de benzodiazepinas en una muestra de consultantes en atención primaria. Rev Med Chil. 2003;131(5),535-40.
| Link |
Galleguillos T, Risco L, Garay JL, González M, Vogel, M. Tendencia del uso de benzodiazepinas en una muestra de consultantes en atención primaria. Rev Med Chil. 2003;131(5),535-40.
| Link | American Psychiatric Association. DSM IV TR: manual diagnóstico y estadístico de los trastornos mentales: texto revisado. Masson.2003. | Link |
American Psychiatric Association. DSM IV TR: manual diagnóstico y estadístico de los trastornos mentales: texto revisado. Masson.2003. | Link | Manual diagnóstico y estadístico de los trastornos mentales: DSM-5. Editorial Médica Panamericana. 2014. | Link |
Manual diagnóstico y estadístico de los trastornos mentales: DSM-5. Editorial Médica Panamericana. 2014. | Link | Lader M, Tylee A, Donoghue J. Withdrawing benzodiazepines in primary care. CNS Drugs. 2009;23(1):19-34. | CrossRef | PubMed |
Lader M, Tylee A, Donoghue J. Withdrawing benzodiazepines in primary care. CNS Drugs. 2009;23(1):19-34. | CrossRef | PubMed | Soyka M. Treatment of Benzodiazepine Dependence. N Engl J Med. 2017 Mar 23;376(12):1147-1157. | CrossRef | PubMed |
Soyka M. Treatment of Benzodiazepine Dependence. N Engl J Med. 2017 Mar 23;376(12):1147-1157. | CrossRef | PubMed | Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. | CrossRef | PubMed |
Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Review of deprescribing processes and development of an evidence-based, patient-centred deprescribing process. Br J Clin Pharmacol. 2014 Oct;78(4):738-47. | CrossRef | PubMed |