 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
INTRODUCTION
Antipsychotics have been proposed as a pharmacological alternative to prevent postoperative delirium. Nonetheless, their actual clinical benefits and harms are a matter of debate.
METHODS
To answer this question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the chosen systematic reviews, reanalyzed the data from the primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
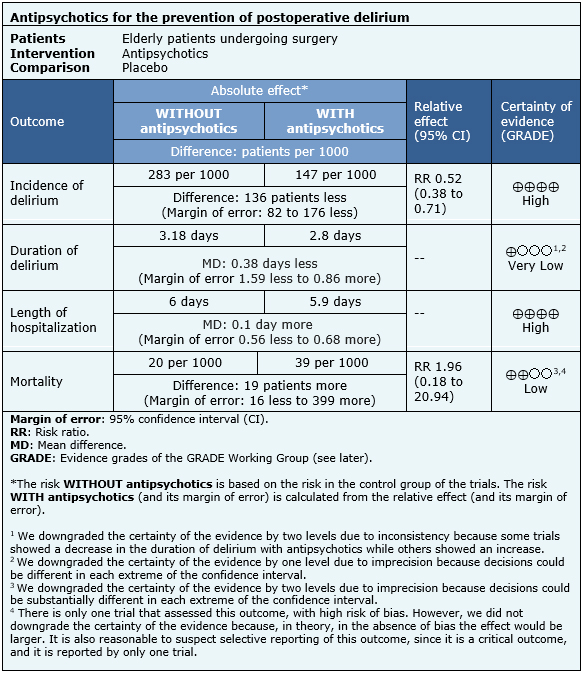
We identified 16 systematic reviews that included eight primary studies, all were randomized trials. We concluded the use of prophylactic antipsychotics reduces the incidence of postoperative delirium, but has no effect on the duration of hospital stay and might increase mortality.
Postoperative delirium is associated to an increase in morbidity, mortality, prolongation of hospital stay and increased costs, especially in elderly patients.
Several non-pharmacological interventions have been proposed in order to reduce the incidence of this complication, but the role of pharmacological alternatives is still controversial. It is known antipsychotics are effective in the prevention of delirium. However, their efficacy and safety in the postoperative context are not yet clearly established.
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found 16 systematic reviews [1],[2],[3],[4],[5],[6], |
|
What types of patients were included* |
Four trials included patients undergoing orthopedic surgery [17],[18],[20],[21], two included patients undergoing cardiovascular surgery [19],[22], two included patients undergoing gastrointestinal surgery [18],[23], and one trial mentioned the participants were not submitted to cardiovascular surgery [24]. Average age was reported in six trials [17],[20],[21],[22],[23],[24], ranging between 61 and 87 years, with an average of 74.6 years. All the trials reported the gender of included participants. The average proportion of men was 50.4%, with a range from 20.2% to 68.3%. |
|
What types of interventions were included* |
Typical (haloperidol) and atypical (risperidone, olanzapine) antipsychotics were used in the trials. Five trials used haloperidol, between 0.5 and 5 mg intravenously [17],[18],[20],[23],[24]. Two trials used risperidone 0.5 mg [20] and 1 mg [23]. One trial used olanzapine 5 mg [22]. In most of the trials the intervention was postoperative [17],[18],[19], and in two trials [20],[21] it was administered before and after surgery. All trials compared against placebo. It is important to note the trials did not make any distinction according to psychomotor activity of delirium, except for one trial [19] that applied the intervention to ‘subsyndromal delirium’. |
|
What types of outcomes |
The main outcomes evaluated by the systematic reviews were: incidence of postoperative delirium, duration of delirium, days of hospitalization, length of stay in intensive care unit, severity of delirium, safety of haloperidol, and mortality. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
The main outcomes evaluated by the systematic reviews were: incidence of postoperative delirium, duration of delirium, days of hospitalization, lenght of stay in intensive care unit, severity of delirium, safety of haloperidol, and mortality.
The information about the effects of antipsychotics for the prevention of postoperative delirium is based on eight randomized trials [17],[18],[19],[20],[21],[22],[23],[24] that included 1932 patients overall. Seven trials reported the incidence of delirium [17],[18],[19],[20],[21],[22],[23],[24]; four trials reported the duration of delirium [19],[20],[21],[24]; four trials reported the length of hospital stay [19],[20],[22],[24]; and only one trial reported mortality [19]. The summary of findings is the following:
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
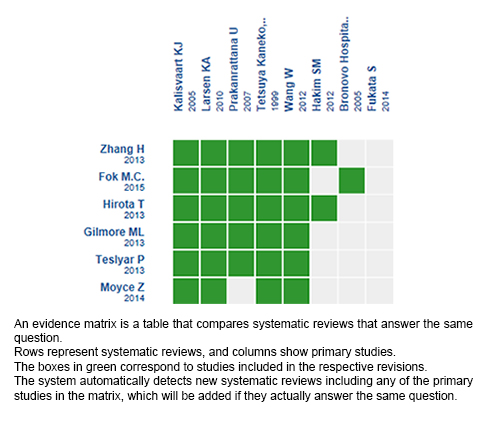
Follow the link to access the interactive version: Antipsychotics for the prevention of postoperative delirium
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Antipsychotics have been proposed as a pharmacological alternative to prevent postoperative delirium. Nonetheless, their actual clinical benefits and harms are a matter of debate.
METHODS
To answer this question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the chosen systematic reviews, reanalyzed the data from the primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified 16 systematic reviews that included eight primary studies, all were randomized trials. We concluded the use of prophylactic antipsychotics reduces the incidence of postoperative delirium, but has no effect on the duration of hospital stay and might increase mortality.
 Autores:
Viviana Castro[1,2], Rami Guinguis[1,2], Marcela Carrasco[2,3]
Autores:
Viviana Castro[1,2], Rami Guinguis[1,2], Marcela Carrasco[2,3]

Citación: Castro V, Guinguis R, Carrasco M. Are antipsychotics effective for the prevention of postoperative delirium?. Medwave 2018 Mar-Abr;18(2):e7195 doi: 10.5867/medwave.2018.02.7195
Fecha de envío: 25/8/2017
Fecha de aceptación: 20/12/2017
Fecha de publicación: 20/4/2018
Origen: Este artículo es producto del Epistemonikos Evidence Synthesis Project de la Fundación Epistemonikos, en colaboración con Medwave para su publicación.
Tipo de revisión: Con revisión por pares sin ciego por parte del equipo metodológico del Epistemonikos Evidence Synthesis Project.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Bin Abd Razak HR, Yung WY. Postoperative Delirium in Patients Undergoing Total Joint Arthroplasty: A Systematic Review. J Arthroplasty. 2015 Aug;30(8):1414-7. | CrossRef | PubMed |
Bin Abd Razak HR, Yung WY. Postoperative Delirium in Patients Undergoing Total Joint Arthroplasty: A Systematic Review. J Arthroplasty. 2015 Aug;30(8):1414-7. | CrossRef | PubMed | Bourne RS, Tahir TA, Borthwick M, Sampson EL. Drug treatment of delirium: past, present and future. J Psychosom Res. 2008 Sep;65(3):273-82. | CrossRef | PubMed |
Bourne RS, Tahir TA, Borthwick M, Sampson EL. Drug treatment of delirium: past, present and future. J Psychosom Res. 2008 Sep;65(3):273-82. | CrossRef | PubMed | Fok MC, Sepehry AA, Frisch L, Sztramko R, Borger van der Burg BL, Vochteloo AJ, Chan P. Do antipsychotics prevent postoperative delirium? A systematic review and meta-analysis. Int J Geriatr Psychiatry. 2015 Apr;30(4):333-44. | CrossRef | PubMed |
Fok MC, Sepehry AA, Frisch L, Sztramko R, Borger van der Burg BL, Vochteloo AJ, Chan P. Do antipsychotics prevent postoperative delirium? A systematic review and meta-analysis. Int J Geriatr Psychiatry. 2015 Apr;30(4):333-44. | CrossRef | PubMed | Gilmore ML, Wolfe DJ. Antipsychotic prophylaxis in surgical patients modestly decreases delirium incidence--but not duration--in high-incidence samples: a meta-analysis. Gen Hosp Psychiatry. 2013 Jul-Aug;35(4):370-5. | CrossRef | PubMed |
Gilmore ML, Wolfe DJ. Antipsychotic prophylaxis in surgical patients modestly decreases delirium incidence--but not duration--in high-incidence samples: a meta-analysis. Gen Hosp Psychiatry. 2013 Jul-Aug;35(4):370-5. | CrossRef | PubMed | Hempenius L, van Leeuwen BL, van Asselt DZ, Hoekstra HJ, Wiggers T, Slaets JP, de Bock GH. Structured analyses of interventions to prevent delirium. Int J Geriatr Psychiatry. 2011 May;26(5):441-50. | CrossRef | PubMed |
Hempenius L, van Leeuwen BL, van Asselt DZ, Hoekstra HJ, Wiggers T, Slaets JP, de Bock GH. Structured analyses of interventions to prevent delirium. Int J Geriatr Psychiatry. 2011 May;26(5):441-50. | CrossRef | PubMed | Hirota T, Kishi T. Prophylactic antipsychotic use for postoperative delirium: a systematic review and meta-analysis. J Clin Psychiatry. 2013 Dec;74(12):e1136-44. | CrossRef | PubMed |
Hirota T, Kishi T. Prophylactic antipsychotic use for postoperative delirium: a systematic review and meta-analysis. J Clin Psychiatry. 2013 Dec;74(12):e1136-44. | CrossRef | PubMed | Khan BA, Gutteridge D, Campbell NL. Update on Pharmacotherapy for Prevention and Treatment of Post-operative Delirium: A Systematic Evidence Review. Curr Anesthesiol Rep. 2015 Mar;5(1):57-64. | PubMed | PMC |
Khan BA, Gutteridge D, Campbell NL. Update on Pharmacotherapy for Prevention and Treatment of Post-operative Delirium: A Systematic Evidence Review. Curr Anesthesiol Rep. 2015 Mar;5(1):57-64. | PubMed | PMC | Lonergan E, Britton AM, Luxenberg J, Wyller T. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007 Apr 18;(2):CD005594. Review. | PubMed |
Lonergan E, Britton AM, Luxenberg J, Wyller T. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007 Apr 18;(2):CD005594. Review. | PubMed | Moyce Z, Rodseth RN, Biccard BM. The efficacy of peri-operative interventions to decrease postoperative delirium in non-cardiac surgery: a systematic review and meta-analysis. Anaesthesia. 2014 Mar;69(3):259-69. Erratum in: Anaesthesia. 2015 Aug;70(8):1011. | CrossRef | PubMed |
Moyce Z, Rodseth RN, Biccard BM. The efficacy of peri-operative interventions to decrease postoperative delirium in non-cardiac surgery: a systematic review and meta-analysis. Anaesthesia. 2014 Mar;69(3):259-69. Erratum in: Anaesthesia. 2015 Aug;70(8):1011. | CrossRef | PubMed | Mu JL, Lee A, Joynt GM. Pharmacologic agents for the prevention and treatment of delirium in patients undergoing cardiac surgery: systematic review and metaanalysis. Crit Care Med. 2015 Jan;43(1):194-204. | CrossRef | PubMed |
Mu JL, Lee A, Joynt GM. Pharmacologic agents for the prevention and treatment of delirium in patients undergoing cardiac surgery: systematic review and metaanalysis. Crit Care Med. 2015 Jan;43(1):194-204. | CrossRef | PubMed | Orena EF, King AB, Hughes CG. The role of anesthesia in the prevention of postoperative delirium: a systematic review. Minerva Anestesiol. 2016 Jun;82(6):669-83. | PubMed |
Orena EF, King AB, Hughes CG. The role of anesthesia in the prevention of postoperative delirium: a systematic review. Minerva Anestesiol. 2016 Jun;82(6):669-83. | PubMed | Schrader SL, Wellik KE, Demaerschalk BM, Caselli RJ, Woodruff BK, Wingerchuk DM. Adjunctive haloperidol prophylaxis reduces postoperative delirium severity and duration in at-risk elderly patients. Neurologist. 2008 Mar;14(2):134-7. | CrossRef | PubMed |
Schrader SL, Wellik KE, Demaerschalk BM, Caselli RJ, Woodruff BK, Wingerchuk DM. Adjunctive haloperidol prophylaxis reduces postoperative delirium severity and duration in at-risk elderly patients. Neurologist. 2008 Mar;14(2):134-7. | CrossRef | PubMed | Schrijver EJ, de Graaf K, de Vries OJ, Maier AB, Nanayakkara PW. Efficacy and safety of haloperidol for in-hospital delirium prevention and treatment: A systematic review of current evidence. Eur J Intern Med. 2016 Jan;27:14-23. | CrossRef | PubMed |
Schrijver EJ, de Graaf K, de Vries OJ, Maier AB, Nanayakkara PW. Efficacy and safety of haloperidol for in-hospital delirium prevention and treatment: A systematic review of current evidence. Eur J Intern Med. 2016 Jan;27:14-23. | CrossRef | PubMed | Teslyar P, Stock VM, Wilk CM, Camsari U, Ehrenreich MJ, Himelhoch S. Prophylaxis with antipsychotic medication reduces the risk of post-operative delirium in elderly patients: a meta-analysis. Psychosomatics. 2013 Mar-Apr;54(2):124-31. | CrossRef | PubMed |
Teslyar P, Stock VM, Wilk CM, Camsari U, Ehrenreich MJ, Himelhoch S. Prophylaxis with antipsychotic medication reduces the risk of post-operative delirium in elderly patients: a meta-analysis. Psychosomatics. 2013 Mar-Apr;54(2):124-31. | CrossRef | PubMed | Tse L, Schwarz SK, Bowering JB, Moore RL, Burns KD, Richford CM, Osborn JA, Barr AM. Pharmacological risk factors for delirium after cardiac surgery: a review. Curr Neuropharmacol. 2012 Sep;10(3):181-96. | CrossRef | PubMed | PMC |
Tse L, Schwarz SK, Bowering JB, Moore RL, Burns KD, Richford CM, Osborn JA, Barr AM. Pharmacological risk factors for delirium after cardiac surgery: a review. Curr Neuropharmacol. 2012 Sep;10(3):181-96. | CrossRef | PubMed | PMC | Zhang H, Lu Y, Liu M, Zou Z, Wang L, Xu FY, Shi XY. Strategies for prevention of postoperative delirium: a systematic review and meta-analysis of randomized trials. Crit Care. 2013 Mar 18;17(2):R47. | CrossRef | PubMed | PMC |
Zhang H, Lu Y, Liu M, Zou Z, Wang L, Xu FY, Shi XY. Strategies for prevention of postoperative delirium: a systematic review and meta-analysis of randomized trials. Crit Care. 2013 Mar 18;17(2):R47. | CrossRef | PubMed | PMC | Borger van der Burg. Postoperative haloperidol versus placebo for prevention of post-operative delirium after acute hip surgery. NCT00250237. | Link |
Borger van der Burg. Postoperative haloperidol versus placebo for prevention of post-operative delirium after acute hip surgery. NCT00250237. | Link | Fukata S, Kawabata Y, Fujisiro K, Katagawa Y, Kuroiwa K, Akiyama H, Terabe Y, Ando M, Kawamura T, Hattori H. Haloperidol prophylaxis does not prevent postoperative delirium in elderly patients: a randomized, open-label prospective trial. Surg Today. 2014 Dec;44(12):2305-13. | CrossRef | PubMed |
Fukata S, Kawabata Y, Fujisiro K, Katagawa Y, Kuroiwa K, Akiyama H, Terabe Y, Ando M, Kawamura T, Hattori H. Haloperidol prophylaxis does not prevent postoperative delirium in elderly patients: a randomized, open-label prospective trial. Surg Today. 2014 Dec;44(12):2305-13. | CrossRef | PubMed | Hakim SM, Othman AI, Naoum DO. Early treatment with risperidone for subsyndromal delirium after on-pump cardiac surgery in the elderly: a randomized trial. Anesthesiology. 2012 May;116(5):987-97. | CrossRef | PubMed |
Hakim SM, Othman AI, Naoum DO. Early treatment with risperidone for subsyndromal delirium after on-pump cardiac surgery in the elderly: a randomized trial. Anesthesiology. 2012 May;116(5):987-97. | CrossRef | PubMed | Kalisvaart KJ, de Jonghe JF, Bogaards MJ, Vreeswijk R, Egberts TC, Burger BJ, Eikelenboom P, van Gool WA. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc. 2005 Oct;53(10):1658-66. | PubMed |
Kalisvaart KJ, de Jonghe JF, Bogaards MJ, Vreeswijk R, Egberts TC, Burger BJ, Eikelenboom P, van Gool WA. Haloperidol prophylaxis for elderly hip-surgery patients at risk for delirium: a randomized placebo-controlled study. J Am Geriatr Soc. 2005 Oct;53(10):1658-66. | PubMed | Larsen KA, Kelly SE, Stern TA, Bode RH Jr, Price LL, Hunter DJ, Gulczynski D, Bierbaum BE, Sweeney GA, Hoikala KA, Cotter JJ, Potter AW. Administration of olanzapine to prevent postoperative delirium in elderly joint-replacement patients: a randomized, controlled trial. Psychosomatics. 2010 Sep-Oct;51(5):409-18. | CrossRef | PubMed |
Larsen KA, Kelly SE, Stern TA, Bode RH Jr, Price LL, Hunter DJ, Gulczynski D, Bierbaum BE, Sweeney GA, Hoikala KA, Cotter JJ, Potter AW. Administration of olanzapine to prevent postoperative delirium in elderly joint-replacement patients: a randomized, controlled trial. Psychosomatics. 2010 Sep-Oct;51(5):409-18. | CrossRef | PubMed | Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. 2007 Oct;35(5):714-9. | PubMed |
Prakanrattana U, Prapaitrakool S. Efficacy of risperidone for prevention of postoperative delirium in cardiac surgery. Anaesth Intensive Care. 2007 Oct;35(5):714-9. | PubMed | Kaneko T. Prophylactic consecutive administration of haloperidol can reduce the ocurrence of postoperative delirium in gastrointestinal surgery. Yonago Acta Med 42(3): 179-184.
Kaneko T. Prophylactic consecutive administration of haloperidol can reduce the ocurrence of postoperative delirium in gastrointestinal surgery. Yonago Acta Med 42(3): 179-184.  Wang W, Li HL, Wang DX, Zhu X, Li SL, Yao GQ, Chen KS, Gu XE, Zhu SN. Haloperidol prophylaxis decreases delirium incidence in elderly patients after noncardiac surgery: a randomized controlled trial*. Crit Care Med. 2012 Mar;40(3):731-9. | CrossRef | PubMed |
Wang W, Li HL, Wang DX, Zhu X, Li SL, Yao GQ, Chen KS, Gu XE, Zhu SN. Haloperidol prophylaxis decreases delirium incidence in elderly patients after noncardiac surgery: a randomized controlled trial*. Crit Care Med. 2012 Mar;40(3):731-9. | CrossRef | PubMed | Polcwiartek C, Kragholm K, Schjerning O, Graff C, Nielsen J. Cardiovascular safety of antipsycotics: a clinical overview. Expert Opin Drug Saf. 2016 May;15(5): 679-88. | CrossRef | PubMed |
Polcwiartek C, Kragholm K, Schjerning O, Graff C, Nielsen J. Cardiovascular safety of antipsycotics: a clinical overview. Expert Opin Drug Saf. 2016 May;15(5): 679-88. | CrossRef | PubMed | American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc. 2015 Jan;63(1):142-50. | CrossRef | PubMed | Link |
American Geriatrics Society Expert Panel on Postoperative Delirium in Older Adults. American Geriatrics Society abstracted clinical practice guideline for postoperative delirium in older adults. J Am Geriatr Soc. 2015 Jan;63(1):142-50. | CrossRef | PubMed | Link | Fukata S. A study on the aggravation prophylaxis of postoperative delirium for the elderly. ID: JPRN-UMIN000007204. | Link |
Fukata S. A study on the aggravation prophylaxis of postoperative delirium for the elderly. ID: JPRN-UMIN000007204. | Link | Fukata S. A study on the prevention of postoperative delirium for the elderly. ID: JPRN-UMIN000002891. | Link |
Fukata S. A study on the prevention of postoperative delirium for the elderly. ID: JPRN-UMIN000002891. | Link | Kelly S. A Double-Blind, Randomized, Placebo-Controlled Study of Perioperative Administration of Olanzapine to Prevent Postoperative Delirium in Joint Replacement Patients. NCT00699946. | Link |
Kelly S. A Double-Blind, Randomized, Placebo-Controlled Study of Perioperative Administration of Olanzapine to Prevent Postoperative Delirium in Joint Replacement Patients. NCT00699946. | Link | Hattori H. A randomized placebo-controlled study of small dose and short duration Haloperidol prophylaxis for elderly at risk for postoperative delirium. ID: JPRN-UMIN000001039. | Link |
Hattori H. A randomized placebo-controlled study of small dose and short duration Haloperidol prophylaxis for elderly at risk for postoperative delirium. ID: JPRN-UMIN000001039. | Link |