 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
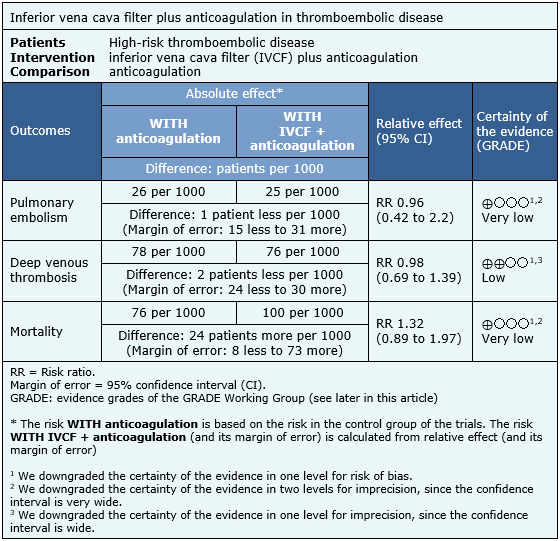
Some patients who have presented a thromboembolic event persist with a high risk of recurrence despite anticoagulant treatment. It has been suggested that adding an inferior vena cava filter may reduce this risk, but the clinical effects of this measure are not clear. To answer this question we searched in Epistemonikos database, which is maintained by screening multiple information sources. We identified three systematic reviews including four randomized trials answering this question. We extracted data, conducted a meta-analysis and generated a summary of findings table using the GRADE approach. We concluded there might be little or no difference on the occurrence of deep venous thrombosis by adding an inferior vena cava filter in anticoagulated patients, and it is not clear whether there are differences in the occurrence of pulmonary embolism or mortality because the certainty of evidence is very low.
Patients with thromboembolic disease have a variable risk of developing recurrent thrombi that might be detached and travel intravascularly in favor of circulation. After a first episode, this risk persists in spite of anticoagulant treatment, so it has been proposed that the placement of an inferior vena cava filter in patients with high risk of developing pulmonary embolism might be beneficial.
Inferior vena cava filters are intraluminal devices that mechanically trap fragmented thrombi from deep veins of the leg, thus preventing their passage into the lung. They are designed to be introduced percutaneously, through jugular, subclavian or femoral veins depending on the filter model. Although its use for prevention of pulmonary embolism appears to be beneficial in theory, its clinical efficacy and adverse events profile are not clear.
We used Epistemonikos database, which is maintained by screening multiple information sources, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found three systematic reviews [1],[2],[3] including four primary studies answering the question of interest, reported in six references [4],[5],[6],[7],[8],[9]. All of the studies correspond to randomized controlled trials. |
|
What types of patients were included* |
All of the trials included patients at high risk for pulmonary embolism [4],[7],[8],[9]. One trial (PREPIC) included patients with documented proximal deep vein thrombosis or pulmonary embolism [4], another trial included patients with documented deep vein thrombosis and cancer [7], another trial (FILTER-PEVI) included patients with symptomatic proximal deep venous thrombosis [8], and the remaining trial included inpatients with symptomatic acute pulmonary embolism with pre-existing deep venous thrombosis presenting a high risk of recurrence [9]. |
|
What types of interventions were included* |
All of the trials evaluated the addition of an inferior vena cava filter to anticoagulant treatment for the prevention of pulmonary embolism. Two trials used a permanent filter; one used Vena Tech LGM, B. Braun; Titanium Greenfield, Boston Scientific; Cardial, Bard; Bird's Nest, Cook Group [4], and the other trial used Vena Tech Vena TMLP, B. Braun [7]. One trial used a removable vena cava filter (ALN filter, ALN Implants Chirurgicaux) [9]. One trial used several filters (Celect, Tulip [Cook Medical, Bloomington, IN], Optease [Cordis,Miami, FL]; Eclipse [Bard, Tempe, AZ]) ** [8]. All trials compared against anticoagulant treatment; one trial used low molecular weight heparin (enoxaparin), unfractionated heparin or vitamin K antagonists [4]; one trial used fondaparinux [7]; another trial used tinzaparin, enoxaparin, fondaparinux, unfractionated heparin or vitamin K antagonists; the remaining trial used enoxaparin or unfractionated heparin in those with renal insufficiency, followed by warfarin ** [8]. |
|
What types of outcomes |
The different systematic reviews grouped the outcomes as follows:
|
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
** Information extracted from the full text of the primary study.
The information on the effects of the addition of an inferior vena cava filter to anticoagulation in patients with thromboembolic disease is based on four randomized trials involving 1004 participants in total [4],[7],[8],[9]. All of the trials reported the outcomes pulmonary embolism, deep venous thrombosis and mortality. The summary of findings is as follows:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
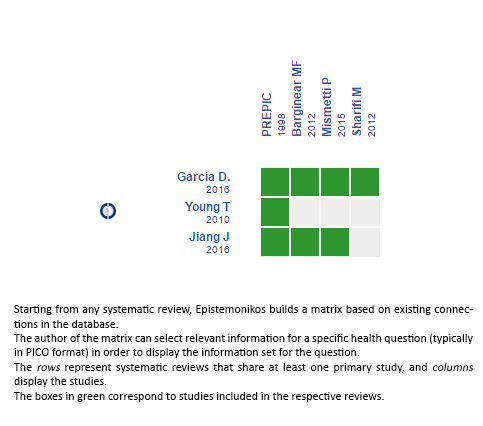
Follow the link to access the interactive version: Vena cava filters plus anticoagulation versus anticoagulation for patients with thromboembolic disease.
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Some patients who have presented a thromboembolic event persist with a high risk of recurrence despite anticoagulant treatment. It has been suggested that adding an inferior vena cava filter may reduce this risk, but the clinical effects of this measure are not clear. To answer this question we searched in Epistemonikos database, which is maintained by screening multiple information sources. We identified three systematic reviews including four randomized trials answering this question. We extracted data, conducted a meta-analysis and generated a summary of findings table using the GRADE approach. We concluded there might be little or no difference on the occurrence of deep venous thrombosis by adding an inferior vena cava filter in anticoagulated patients, and it is not clear whether there are differences in the occurrence of pulmonary embolism or mortality because the certainty of evidence is very low.
 Autores:
Alexandra Yunes[1,2], Andrés Aizman[2,3]
Autores:
Alexandra Yunes[1,2], Andrés Aizman[2,3]

Citación: Yunes A, Aizman A. Is it worth adding an inferior vena cava filter to anticoagulation in thromboembolic disease?. Medwave2017;17(Suppl2):e6935 doi: 10.5867/medwave.2017.6935
Fecha de envío: 23/3/2017
Fecha de aceptación: 30/3/2017
Fecha de publicación: 28/4/2017

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Garcia D, Ansari M, Cardoso R, Mendoza-Trauco C, Diaz-Sandoval L, Saab F, et al. Clinical outcomes of retrievable inferior vena cava filter plus anticoagulation versus anticoagulation alone on high-risk patients: A meta-analysis. Journal of the American College of Cardiology. 2016;:2267. | CrossRef |
Garcia D, Ansari M, Cardoso R, Mendoza-Trauco C, Diaz-Sandoval L, Saab F, et al. Clinical outcomes of retrievable inferior vena cava filter plus anticoagulation versus anticoagulation alone on high-risk patients: A meta-analysis. Journal of the American College of Cardiology. 2016;:2267. | CrossRef | Young T, Tang H, Hughes R. Vena caval filters for the prevention of pulmonary embolism. Cochrane Database Syst Rev. 2010 Feb 17;(2):CD006212 | CrossRef | PubMed |
Young T, Tang H, Hughes R. Vena caval filters for the prevention of pulmonary embolism. Cochrane Database Syst Rev. 2010 Feb 17;(2):CD006212 | CrossRef | PubMed | Jiang J, Jiao Y, Zhang X. The short-term efficacy of vena cava filters for the prevention of pulmonary embolism in patients with venous thromboembolism receiving anticoagulation: Meta-analysis of randomized controlled trials. Phlebology. 2016 Dec 2. pii: 0268355516669004 | PubMed |
Jiang J, Jiao Y, Zhang X. The short-term efficacy of vena cava filters for the prevention of pulmonary embolism in patients with venous thromboembolism receiving anticoagulation: Meta-analysis of randomized controlled trials. Phlebology. 2016 Dec 2. pii: 0268355516669004 | PubMed | Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998 Feb 12;338(7):409-15 | PubMed |
Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d'Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med. 1998 Feb 12;338(7):409-15 | PubMed | Decousus H. Eight-year follow-up of a randomized trial investigating vena caval filters in the prevention of PE in patients presenting a proximal DVT: The PREPIC trial. Journal of Thrombosis & Haemostasis. 2003;1(Suppl 1):OC440. | Link |
Decousus H. Eight-year follow-up of a randomized trial investigating vena caval filters in the prevention of PE in patients presenting a proximal DVT: The PREPIC trial. Journal of Thrombosis & Haemostasis. 2003;1(Suppl 1):OC440. | Link | PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005 Jul 19;112(3):416-22 | PubMed |
PREPIC Study Group. Eight-year follow-up of patients with permanent vena cava filters in the prevention of pulmonary embolism: the PREPIC (Prevention du Risque d'Embolie Pulmonaire par Interruption Cave) randomized study. Circulation. 2005 Jul 19;112(3):416-22 | PubMed | Barginear MF, Gralla RJ, Bradley TP, Ali SS, Shapira I, Greben C, et al. Investigating the benefit of adding a vena cava filter to anticoagulation with fondaparinux sodium in patients with cancer and venous thromboembolism in a prospective randomized clinical trial. Support Care Cancer. 2012 Nov;20(11):2865-72 | CrossRef | PubMed |
Barginear MF, Gralla RJ, Bradley TP, Ali SS, Shapira I, Greben C, et al. Investigating the benefit of adding a vena cava filter to anticoagulation with fondaparinux sodium in patients with cancer and venous thromboembolism in a prospective randomized clinical trial. Support Care Cancer. 2012 Nov;20(11):2865-72 | CrossRef | PubMed | Sharifi M, Bay C, Skrocki L, Lawson D, Mazdeh S. Role of IVC filters in endovenous therapy for deep venous thrombosis: the FILTER-PEVI (filter implantation to lower thromboembolic risk in percutaneous endovenous intervention) trial. Cardiovasc Intervent Radiol. 2012 Dec;35(6):1408-13 | CrossRef | PubMed |
Sharifi M, Bay C, Skrocki L, Lawson D, Mazdeh S. Role of IVC filters in endovenous therapy for deep venous thrombosis: the FILTER-PEVI (filter implantation to lower thromboembolic risk in percutaneous endovenous intervention) trial. Cardiovasc Intervent Radiol. 2012 Dec;35(6):1408-13 | CrossRef | PubMed | Mismetti P, Laporte S, Pellerin O, Ennezat PV, Couturaud F, Elias A, et al; PREPIC2 Study Group. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA. 2015 Apr 28;313(16):1627-35 | CrossRef | PubMed |
Mismetti P, Laporte S, Pellerin O, Ennezat PV, Couturaud F, Elias A, et al; PREPIC2 Study Group. Effect of a retrievable inferior vena cava filter plus anticoagulation vs anticoagulation alone on risk of recurrent pulmonary embolism: a randomized clinical trial. JAMA. 2015 Apr 28;313(16):1627-35 | CrossRef | PubMed |