 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
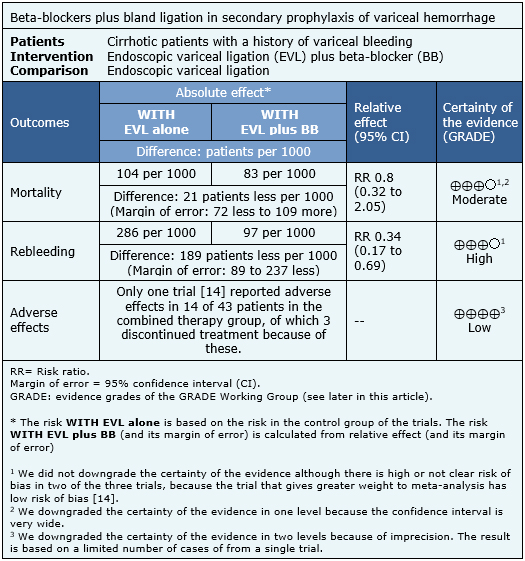
Cirrhotic patients who have had an episode of bleeding from gastroesophageal varices are at high risk of rebleeding, despite treatment with endoscopic variceal ligation. Adding beta-blockers could reduce this risk, but it is associated with adverse effects. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified seven systematic reviews including 21 randomized controlled trials addressing the question of this article. We extracted data, combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded the addition of beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal bleeding reduces the risk of rebleeding, but probably does not lead to any difference in terms of mortality. Even though it is associated to frequent adverse effects, these would be mild and generally do not lead to discontinuation of treatment.
Variceal bleeding in cirrhosis has a mortality risk between 20-50% per episode, as a consequence of hypovolemic shock or decompensation of underlying chronic liver damage [1]. Variceal rebleeding occurs in 60 to 70% of patients within the first two years after the first episode [2],[3],[4]. The standard strategy as secondary prophylaxis is eradication of varices with multiple sessions of endoscopic ligation. On the other hand, beta-blockers have proved to be better than placebo and randomized trials have shown there might be no difference in effectiveness when compared with endoscopic therapy [5],[6],[7],[8],[9],[10].
Endoscopic band ligation eradicates varices with high bleeding risk and beta-blockers reduce portal pressure, the main risk factor for variceal bleeding. However, it is not clear whether the combination of both therapies translates into a relevant clinical benefit when compared to endoscopic ligation alone.
We used Epistemonikos database, which is maintained by screening multiple databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found seven [1],[2],[3],[4],[5],[11],[12] systematic reviews including three randomized controlled trials reported in four references addressing the question of interest [13], [14],[15],[16]. |
|
What types of patients were included |
All reviewed trials included patients who had already had a previous episode of variceal bleeding. |
|
What types of interventions were included |
The interval between ligation sessions was less than three weeks in two trials [14],[15]. One trial [16] did not report this data. |
|
What types of outcomes |
The main outcomes were overall mortality and rebleeding in all of the systematic reviews identified. Four reviews [1], [2],[3],[12] included adverse effects in their analysis, but none of them reported the data of adverse effects of the trials included in this summary. |
The information on the effects of adding beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal bleeding is based on three randomized trials involving 161 patients [14],[15],[16]. All of the trials reported mortality and rebleeding and only one reported adverse effects [14]. The summary of findings is as follows:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
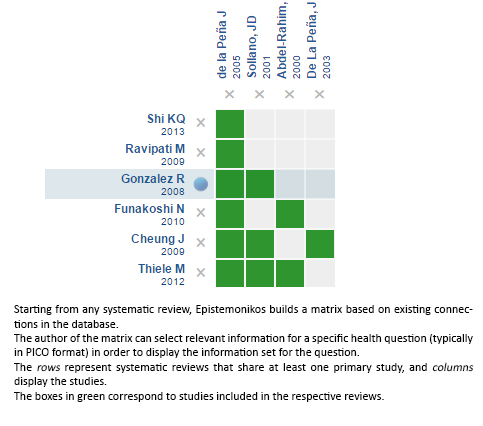
Follow the link to access the interactive version: Banding ligation versus beta-blockers for primary prevention of variceal bleeding
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Cirrhotic patients who have had an episode of bleeding from gastroesophageal varices are at high risk of rebleeding, despite treatment with endoscopic variceal ligation. Adding beta-blockers could reduce this risk, but it is associated with adverse effects. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified seven systematic reviews including 21 randomized controlled trials addressing the question of this article. We extracted data, combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded the addition of beta-blockers to endoscopic variceal ligation as secondary prophylaxis of variceal bleeding reduces the risk of rebleeding, but probably does not lead to any difference in terms of mortality. Even though it is associated to frequent adverse effects, these would be mild and generally do not lead to discontinuation of treatment.
 Autores:
Petre Cotoras[1,2], Jorge Faúndez[1,2], Roberto Candia[2,3,4]
Autores:
Petre Cotoras[1,2], Jorge Faúndez[1,2], Roberto Candia[2,3,4]

Citación: Cotoras P, Faúndez J, Candia R. Should we add beta-blockers to band ligation for secondary prophylaxis of variceal bleeding?. Medwave 2017; 17(Suppl1):e6847 doi: 10.5867/medwave.2017.6847
Fecha de publicación: 23/2/2017

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Puente A, Hernández-Gea V, Graupera I, Roque M, Colomo A, Poca M, et al. Drugs plus ligation to prevent rebleeding in cirrhosis: an updated systematic review. Liver Int. 2014 Jul;34(6):823-33 | CrossRef | PubMed |
Puente A, Hernández-Gea V, Graupera I, Roque M, Colomo A, Poca M, et al. Drugs plus ligation to prevent rebleeding in cirrhosis: an updated systematic review. Liver Int. 2014 Jul;34(6):823-33 | CrossRef | PubMed | Thiele M, Krag A, Rohde U, Gluud LL. Meta-analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012 May;35(10):1155-65 | CrossRef | PubMed |
Thiele M, Krag A, Rohde U, Gluud LL. Meta-analysis: banding ligation and medical interventions for the prevention of rebleeding from oesophageal varices. Aliment Pharmacol Ther. 2012 May;35(10):1155-65 | CrossRef | PubMed | Cheung J, Zeman M, van Zanten SV, Tandon P. Systematic review: secondary prevention with band ligation, pharmacotherapy or combination therapy after bleeding from oesophageal varices. Aliment Pharmacol Ther. 2009 Sep 15;30(6):577-88 | CrossRef | PubMed |
Cheung J, Zeman M, van Zanten SV, Tandon P. Systematic review: secondary prevention with band ligation, pharmacotherapy or combination therapy after bleeding from oesophageal varices. Aliment Pharmacol Ther. 2009 Sep 15;30(6):577-88 | CrossRef | PubMed | Ravipati M, Katragadda S, Swaminathan PD, Molnar J, Zarling E. Pharmacotherapy plus endoscopic intervention is more effective than pharmacotherapy or endoscopy alone in the secondary prevention of esophageal variceal bleeding: a meta-analysis of randomized, controlled trials. Gastrointest Endosc. 2009 Oct;70(4):658-664.e5 | CrossRef | PubMed |
Ravipati M, Katragadda S, Swaminathan PD, Molnar J, Zarling E. Pharmacotherapy plus endoscopic intervention is more effective than pharmacotherapy or endoscopy alone in the secondary prevention of esophageal variceal bleeding: a meta-analysis of randomized, controlled trials. Gastrointest Endosc. 2009 Oct;70(4):658-664.e5 | CrossRef | PubMed | Shi KQ, Liu WY, Pan ZZ, Ling XF, Chen SL, Chen YP, et al. Secondary prophylaxis of variceal bleeding for cirrhotic patients: a multiple-treatments meta-analysis. Eur J Clin Invest. 2013 Aug;43(8):844-54. | CrossRef | PubMed |
Shi KQ, Liu WY, Pan ZZ, Ling XF, Chen SL, Chen YP, et al. Secondary prophylaxis of variceal bleeding for cirrhotic patients: a multiple-treatments meta-analysis. Eur J Clin Invest. 2013 Aug;43(8):844-54. | CrossRef | PubMed | Colombo M, de Franchis R, Tommasini M, Sangiovanni A, Dioguardi N. Beta-blockade prevents recurrent gastrointestinal bleeding in well-compensated patients with alcoholic cirrhosis: a multicenter randomized controlled trial. Hepatology. 1989 Mar;9(3):433-8 | PubMed |
Colombo M, de Franchis R, Tommasini M, Sangiovanni A, Dioguardi N. Beta-blockade prevents recurrent gastrointestinal bleeding in well-compensated patients with alcoholic cirrhosis: a multicenter randomized controlled trial. Hepatology. 1989 Mar;9(3):433-8 | PubMed | Garden OJ, Mills PR, Birnie GG, Murray GD, Carter DC. Propranolol in the prevention of recurrent variceal hemorrhage in cirrhotic patients. A controlled trial. Gastroenterology. 1990 Jan;98(1):185-90 | PubMed |
Garden OJ, Mills PR, Birnie GG, Murray GD, Carter DC. Propranolol in the prevention of recurrent variceal hemorrhage in cirrhotic patients. A controlled trial. Gastroenterology. 1990 Jan;98(1):185-90 | PubMed | Ahmad I, Khan AA, Alam A, Butt AK, Shafqat F, Sarwar S. Propranolol, isosorbide mononitrate and endoscopic band ligation - alone or in varying combinations for the prevention of esophageal variceal rebleeding. J Coll Physicians Surg Pak. 2009 May;19(5):283-6 | CrossRef | PubMed |
Ahmad I, Khan AA, Alam A, Butt AK, Shafqat F, Sarwar S. Propranolol, isosorbide mononitrate and endoscopic band ligation - alone or in varying combinations for the prevention of esophageal variceal rebleeding. J Coll Physicians Surg Pak. 2009 May;19(5):283-6 | CrossRef | PubMed | Lo GH, Chen WC, Chen MH, Hsu PI, Lin CK, Tsai WL, et al. Banding ligation versus nadolol and isosorbide mononitrate for the prevention of esophageal variceal rebleeding. Gastroenterology. 2002 Sep;123(3):728-34 | PubMed |
Lo GH, Chen WC, Chen MH, Hsu PI, Lin CK, Tsai WL, et al. Banding ligation versus nadolol and isosorbide mononitrate for the prevention of esophageal variceal rebleeding. Gastroenterology. 2002 Sep;123(3):728-34 | PubMed | Sarin SK, Wadhawan M, Gupta R, Shahi H. Evaluation of endoscopic variceal ligation (EVL) versus propanolol plus isosorbide mononitrate/nadolol (ISMN) in the prevention of variceal rebleeding: comparison of cirrhotic and noncirrhotic patients. Dig Dis Sci. 2005 Aug;50(8):1538-47 | PubMed |
Sarin SK, Wadhawan M, Gupta R, Shahi H. Evaluation of endoscopic variceal ligation (EVL) versus propanolol plus isosorbide mononitrate/nadolol (ISMN) in the prevention of variceal rebleeding: comparison of cirrhotic and noncirrhotic patients. Dig Dis Sci. 2005 Aug;50(8):1538-47 | PubMed | Funakoshi N, Ségalas-Largey F, Duny Y, Oberti F, Valats JC, Bismuth M, et al. Benefit of combination β-blocker and endoscopic treatment to prevent variceal rebleeding: a meta-analysis. World J Gastroenterol. 2010 Dec 21;16(47):5982-92 | PubMed |
Funakoshi N, Ségalas-Largey F, Duny Y, Oberti F, Valats JC, Bismuth M, et al. Benefit of combination β-blocker and endoscopic treatment to prevent variceal rebleeding: a meta-analysis. World J Gastroenterol. 2010 Dec 21;16(47):5982-92 | PubMed | Gonzalez R, Zamora J, Gomez-Camarero J, Molinero LM, Bañares R, Albillos A. Meta-analysis: Combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Ann Intern Med. 2008 Jul 15;149(2):109-22 | PubMed |
Gonzalez R, Zamora J, Gomez-Camarero J, Molinero LM, Bañares R, Albillos A. Meta-analysis: Combination endoscopic and drug therapy to prevent variceal rebleeding in cirrhosis. Ann Intern Med. 2008 Jul 15;149(2):109-22 | PubMed | De La Peña J, Rivero M, Suárez C, Brullet E, Campo R, Vergara M, et al. Variceal ligation plus nadolol compared with variceal ligation after bleeding. Multicenter randomized trial. Preliminary analysis. Gastroenterology. 2003;124(4, Supplement 1):A733 | CrossRef |
De La Peña J, Rivero M, Suárez C, Brullet E, Campo R, Vergara M, et al. Variceal ligation plus nadolol compared with variceal ligation after bleeding. Multicenter randomized trial. Preliminary analysis. Gastroenterology. 2003;124(4, Supplement 1):A733 | CrossRef | de la Peña J, Brullet E, Sanchez-Hernández E, Rivero M, Vergara M, Martin-Lorente JL, et al. Variceal ligation plus nadolol compared with ligation for prophylaxis of variceal rebleeding: a multicenter trial. Hepatology. 2005 Mar;41(3):572-8 | PubMed |
de la Peña J, Brullet E, Sanchez-Hernández E, Rivero M, Vergara M, Martin-Lorente JL, et al. Variceal ligation plus nadolol compared with ligation for prophylaxis of variceal rebleeding: a multicenter trial. Hepatology. 2005 Mar;41(3):572-8 | PubMed | Sollano JD, Melchor MC, Ismael AE, Babaran RP, Lira EL. Propranolol prevents rebleeding after variceal ligation. Gastrointestinal Endoscopy. 2001;53(5):AB143 | CrossRef |
Sollano JD, Melchor MC, Ismael AE, Babaran RP, Lira EL. Propranolol prevents rebleeding after variceal ligation. Gastrointestinal Endoscopy. 2001;53(5):AB143 | CrossRef | Abdel-Rahim AY, Abdel-Ghany MS, El-Kholy B. Band ligation alone versus band ligation and propranolol in the management of bleeding esophageal varices. The American Journal of Gastroenterology. 2000;95(9):2442-2442 | CrossRef |
Abdel-Rahim AY, Abdel-Ghany MS, El-Kholy B. Band ligation alone versus band ligation and propranolol in the management of bleeding esophageal varices. The American Journal of Gastroenterology. 2000;95(9):2442-2442 | CrossRef | Lo GH, Chen WC, Chan HH, Tsai WL, Hsu PI, Lin CK, et al. A randomized, controlled trial of banding ligation plus drug therapy versus drug therapy alone in the prevention of esophageal variceal rebleeding. J Gastroenterol Hepatol. 2009 Jun;24(6):982-7 | CrossRef | PubMed |
Lo GH, Chen WC, Chan HH, Tsai WL, Hsu PI, Lin CK, et al. A randomized, controlled trial of banding ligation plus drug therapy versus drug therapy alone in the prevention of esophageal variceal rebleeding. J Gastroenterol Hepatol. 2009 Jun;24(6):982-7 | CrossRef | PubMed | Jha SK, Kumar A, Sharma BC, Sarin SK. Endoscopic variceal ligation (EVL) plus propranolol (P) and isosorbide mononitrate (ISMN) versus EVL alone in secondary prophylaxis of variceal bleeding: a prospective RCT [Abstract]. Hepatology 2007; 46(Suppl S): 250A–1A. | Link |
Jha SK, Kumar A, Sharma BC, Sarin SK. Endoscopic variceal ligation (EVL) plus propranolol (P) and isosorbide mononitrate (ISMN) versus EVL alone in secondary prophylaxis of variceal bleeding: a prospective RCT [Abstract]. Hepatology 2007; 46(Suppl S): 250A–1A. | Link | de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015 Sep;63(3):743-52 | CrossRef | PubMed |
de Franchis R; Baveno VI Faculty. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J Hepatol. 2015 Sep;63(3):743-52 | CrossRef | PubMed | Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al; Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015 Nov;64(11):1680-704. | CrossRef | PubMed |
Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H, et al; Clinical Services and Standards Committee of the British Society of Gastroenterology. U.K. guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut. 2015 Nov;64(11):1680-704. | CrossRef | PubMed | Banding Ligation Plus Propranolol Versus Banding Ligation to Prevent Rebleeding of Esophageal Varices 2013 [on line] | Link |
Banding Ligation Plus Propranolol Versus Banding Ligation to Prevent Rebleeding of Esophageal Varices 2013 [on line] | Link |