 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
There is no consensus about the effects of glutamine supplementation for acute pancreatitis. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified 15 systematic reviews including 31 randomized controlled trials addressing the question of this article. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded glutamine supplementation might decrease infectious complications in acute pancreatitis, but it is not clear if it affects mortality or length of hospital stay because the certainty of the evidence is very low.
Glutamine is an amino acid required for nucleotide synthesis, which makes it an important energetic substrate for cells with fast turnover, such as intestinal epithelium.
Given plasmatic glutamine is reduced in critical care patients and in those undergoing major surgery, it is considered an essential amino acid under stress.
Acute pancreatitis constitutes a potentially severe condition, in which these mechanisms are particularly relevant. So, a potentially beneficial effect of glutamine supplementation has been proposed. However, it is not clear if it leads to clinically relevant effects.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found 15 systematic reviews [1],[2],[3],[4],[5],[6], [7],[8],[9],[10],[11],[12],[13],[14],[15] including 31 randomized controlled trials reported in 32 references [16],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26], [27],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37], [38],[39],[40],[41],[42],[43],[44],[45],[46],[47] (one study is reported in two references [30],[31]). |
|
What types of patients were included |
The different trials included patients with severe acute pancreatitis classified according to the following criteria: Glasgow in two trials [17],[21], APACHE II in eight trials [19],[20],[25],[28],[29],[30],[38],[42],[46], RANSON in six trials [19],[24],[32],[38],[46],[47], severity index according to imagenologic criteria in four [19],[28],[38], [46], ATLANTA criteria in two [26] y [27], in one trial it was not reported what criteria was used [36].Four trials used a combination of the criteria above [19],[28],[38], [46]. It was not possible to extract the information about the severity criteria used in 13 trials from any systematic review identified. |
|
What types of interventions were included |
Eight trials evaluated glutamine supplementation associated to parenteral nutrition [17],[18],[19],[20],[25], [28],[32],[37], and 10 to enteral nutrition [21],[22],[23], [24],[26],[27],[29],[30],[34],[38]. Sixteen trials used glutamine alone [17],[18],[19],[20], [21],[25],[28],[32],[36],[37],[38],[39],[42],[45],[46],[47] and eight glutamine associated to other elements [22], [23],[24],[26],[27],[29],[30],[34]: six with arginine [22], [23],[24],[26],[29],[30], one with con tributyrin and antioxidants [29], two with fiber [22],[23], one with omega-3 [30],[31] and one with Bifidobacterium, Lactobacillus and Enterococcus [34]. It was not possible to extract the information about the glutamine supplementation used in eight trials from any systematic review identified. All of the studies compared against placebo or standard treatment. |
|
What types of outcomes |
The main outcomes meta-analysed in the different reviews were: - Mortality (pooled in 13 systematic reviews). Other outcomes analysed in the different review were: plasma albumin level, plasma C-reactive protein level, surgical intervention rate, time until amylase returned to normal, hospitalization expenses, organ failure, length of intensive care unit stay, days on mechanical ventilation, feeding intolerance, systemic inflammatory response syndrome, change in white blood cells count, ventilator-associated pneumonia, abdominal pain, serious adverse events, side effects (ALT, AST, creatinine), serum amylase in patients undergoing ERCP (after 8 and 24 hours), pancreatitis in patients undergoing ERCP. The following subgroups were analysed in the different reviews: - Effect of high/low doses (more or less than 4.2 g/kg) on mortality in critical and surgical patients - Parenteral versus enteral glutamine. |
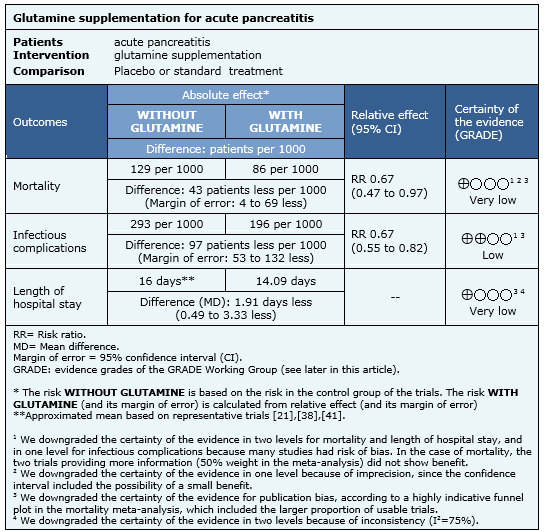
Information on the effects of glutamine for acute pancreatitis is based on 22 randomized controlled trials involving 1107 participants (nine trials did not provide data for meta-analysis). All of the trials reported mortality [16],[17],[18],[19],[20],[21],[22],[24],[25],[26],[27],[28],[29],[30],[32],[34],[35],[36],[38],[39],[41],[43], 20 trials (1063 participants) reported the outcome infectious complications [16],[17],[18],[19],[21],[22],[24],[25],[26],[27],[28],[29],[30],[32],[35],[36],[39],[41],[43],[45] and 18 trials (1018 participants) reported the outcome length of hospital stay[16],[18],[19],[21],[26],[27],[28],[29],[30],[32],[34],[35],[36],[38],[39],[41],[42],[43],[44].
The summary of findings is the following:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
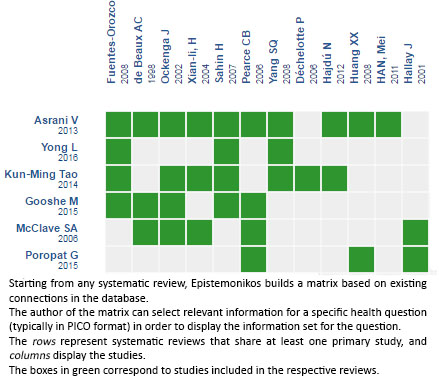
Follow the link to access the interactive version: Glutamine supplementation for acute pancreatitis
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

There is no consensus about the effects of glutamine supplementation for acute pancreatitis. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified 15 systematic reviews including 31 randomized controlled trials addressing the question of this article. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded glutamine supplementation might decrease infectious complications in acute pancreatitis, but it is not clear if it affects mortality or length of hospital stay because the certainty of the evidence is very low.
 Autores:
Victoria Castro-Gutiérrez[1,2], Gabriel Rada[2,3,4,5,6]
Autores:
Victoria Castro-Gutiérrez[1,2], Gabriel Rada[2,3,4,5,6]

Citación: Castro-Gutiérrez V, Rada G. Is there a role for glutamine supplementation in the management of acute pancreatitis?. Medwave 2016;16(Suppl3):6512 doi: 10.5867/medwave.2016.6512
Fecha de publicación: 17/8/2016

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Asrani V, Chang WK, Dong Z, Hardy G, Windsor JA, Petrov MS. Glutamine supplementation in acute pancreatitis: a meta-analysis of randomized controlled
trials. Pancreatology. 2013 Sep-Oct;13(5):468-74. | CrossRef | PubMed |
Asrani V, Chang WK, Dong Z, Hardy G, Windsor JA, Petrov MS. Glutamine supplementation in acute pancreatitis: a meta-analysis of randomized controlled
trials. Pancreatology. 2013 Sep-Oct;13(5):468-74. | CrossRef | PubMed | Avenell A. Hot topics in parenteral nutrition. Current evidence and ongoing trials on the use of glutamine in critically-ill patients and patients undergoing surgery. Proc Nutr Soc. 2009 Aug;68(3):261-8. | CrossRef | PubMed |
Avenell A. Hot topics in parenteral nutrition. Current evidence and ongoing trials on the use of glutamine in critically-ill patients and patients undergoing surgery. Proc Nutr Soc. 2009 Aug;68(3):261-8. | CrossRef | PubMed | Gooshe M, Abdolghaffari AH, Nikfar S, Mahdaviani P, Abdollahi M. Antioxidanttherapy in acute, chronic and post-endoscopic retrograde cholangiopancreatography pancreatitis: An updated systematic review and meta-analysis. World J Gastroenterol. 2015 Aug 14;21(30):9189-208. | CrossRef | PubMed |
Gooshe M, Abdolghaffari AH, Nikfar S, Mahdaviani P, Abdollahi M. Antioxidanttherapy in acute, chronic and post-endoscopic retrograde cholangiopancreatography pancreatitis: An updated systematic review and meta-analysis. World J Gastroenterol. 2015 Aug 14;21(30):9189-208. | CrossRef | PubMed | Jafari T, Feizi A, Askari G, Fallah AA. Parenteral immunonutrition in patients with acute pancreatitis: a systematic review and meta-analysis. Clin Nutr. 2015 Feb;34(1):35-43. | CrossRef | PubMed |
Jafari T, Feizi A, Askari G, Fallah AA. Parenteral immunonutrition in patients with acute pancreatitis: a systematic review and meta-analysis. Clin Nutr. 2015 Feb;34(1):35-43. | CrossRef | PubMed | Tao KM, Li XQ, Yang LQ, Yu WF, Lu ZJ, Sun YM, Wu FX. Glutamine supplementation for critically ill adults. Cochrane Database Syst Rev. 2014 Sep 9;(9):CD010050. | CrossRef | PubMed |
Tao KM, Li XQ, Yang LQ, Yu WF, Lu ZJ, Sun YM, Wu FX. Glutamine supplementation for critically ill adults. Cochrane Database Syst Rev. 2014 Sep 9;(9):CD010050. | CrossRef | PubMed | McClave SA, Chang WK, Dhaliwal R, Heyland DK. Nutrition support in acute pancreatitis: a systematic review of the literature. JPEN J Parenter Enteral
Nutr. 2006 Mar-Apr;30(2):143-56. | PubMed |
McClave SA, Chang WK, Dhaliwal R, Heyland DK. Nutrition support in acute pancreatitis: a systematic review of the literature. JPEN J Parenter Enteral
Nutr. 2006 Mar-Apr;30(2):143-56. | PubMed | Mohseni Salehi Monfared SS, Vahidi H, Abdolghaffari AH, Nikfar S, Abdollahi M. Antioxidant therapy in the management of acute, chronic and post-ERCP pancreatitis: a systematic review. World J Gastroenterol. 2009 Sep 28;15(36):4481-90. | PubMed |
Mohseni Salehi Monfared SS, Vahidi H, Abdolghaffari AH, Nikfar S, Abdollahi M. Antioxidant therapy in the management of acute, chronic and post-ERCP pancreatitis: a systematic review. World J Gastroenterol. 2009 Sep 28;15(36):4481-90. | PubMed | Petrov MS, Atduev VA, Zagainov VE. Advanced enteral therapy in acute pancreatitis: is there a room for immunonutrition? A meta-analysis. Int J Surg.
2008 Apr;6(2):119-24. | CrossRef | PubMed |
Petrov MS, Atduev VA, Zagainov VE. Advanced enteral therapy in acute pancreatitis: is there a room for immunonutrition? A meta-analysis. Int J Surg.
2008 Apr;6(2):119-24. | CrossRef | PubMed | Petrov MS, Loveday BP, Pylypchuk RD, McIlroy K, Phillips AR, Windsor JA. Systematic review and meta-analysis of enteral nutrition formulations in acute
pancreatitis. Br J Surg. 2009 Nov;96(11):1243-52. | CrossRef | PubMed |
Petrov MS, Loveday BP, Pylypchuk RD, McIlroy K, Phillips AR, Windsor JA. Systematic review and meta-analysis of enteral nutrition formulations in acute
pancreatitis. Br J Surg. 2009 Nov;96(11):1243-52. | CrossRef | PubMed | Poropat G, Giljaca V, Hauser G, timac D. Enteral nutrition formulations for acute pancreatitis. Cochrane Database Syst Rev. 2015 Mar 23;(3):CD010605. | CrossRef | PubMed |
Poropat G, Giljaca V, Hauser G, timac D. Enteral nutrition formulations for acute pancreatitis. Cochrane Database Syst Rev. 2015 Mar 23;(3):CD010605. | CrossRef | PubMed | Shen Y, Deng X, Jin W, Zhang C, Zhang X, Wang Y. Effect of pharmaconutrition-supplemented parenteral nutrition for severe acute pancreatitis: a meta-analysis of randomized controlled trials. JOP. 2014 Jul 28;15(4):371-7. | CrossRef | PubMed |
Shen Y, Deng X, Jin W, Zhang C, Zhang X, Wang Y. Effect of pharmaconutrition-supplemented parenteral nutrition for severe acute pancreatitis: a meta-analysis of randomized controlled trials. JOP. 2014 Jul 28;15(4):371-7. | CrossRef | PubMed | Wang YP, Jiao K, Li DB, Dong CL, Wu XA, Liu XJ. Alanyl-glutamine dipeptide for severe acute pancreatitis: a systematic review. Chinese J Evidence-Based Medicine. 2013;13(9):1123-1128. | Link |
Wang YP, Jiao K, Li DB, Dong CL, Wu XA, Liu XJ. Alanyl-glutamine dipeptide for severe acute pancreatitis: a systematic review. Chinese J Evidence-Based Medicine. 2013;13(9):1123-1128. | Link | Wischmeyer PE, Dhaliwal R, McCall M, Ziegler TR, Heyland DK. Parenteral glutamine supplementation in critical illness: a systematic review. Crit Care.
2014 Apr 18;18(2):R76. | PubMed |
Wischmeyer PE, Dhaliwal R, McCall M, Ziegler TR, Heyland DK. Parenteral glutamine supplementation in critical illness: a systematic review. Crit Care.
2014 Apr 18;18(2):R76. | PubMed | Yong L, Lu QP, Liu SH, Fan H. Efficacy of Glutamine-Enriched Nutrition Support for Patients With Severe Acute Pancreatitis: A Meta-Analysis. JPEN J Parenter Enteral Nutr. 2016 Jan;40(1):83-94. | CrossRef | PubMed |
Yong L, Lu QP, Liu SH, Fan H. Efficacy of Glutamine-Enriched Nutrition Support for Patients With Severe Acute Pancreatitis: A Meta-Analysis. JPEN J Parenter Enteral Nutr. 2016 Jan;40(1):83-94. | CrossRef | PubMed | Zhong X, Liang CP, Gong S. Intravenous glutamine for severe acute pancreatitis: A meta-analysis. World J Crit Care Med. 2013 Feb 4;2(1):4-8. | CrossRef | PubMed |
Zhong X, Liang CP, Gong S. Intravenous glutamine for severe acute pancreatitis: A meta-analysis. World J Crit Care Med. 2013 Feb 4;2(1):4-8. | CrossRef | PubMed | Dan W , Yong L, Effects of early glutamine supplemented enteral nutrition on clinical outcomes of patients with severe acute pancreatitis. J Jiu Jiang Univ (Nat Sci) 2010. | Link |
Dan W , Yong L, Effects of early glutamine supplemented enteral nutrition on clinical outcomes of patients with severe acute pancreatitis. J Jiu Jiang Univ (Nat Sci) 2010. | Link | de Beaux AC, O'Riordain MG, Ross JA, Jodozi L, Carter DC, Fearon KC. Glutamine-supplemented total parenteral nutrition reduces blood mononuclear cell interleukin-8 release in severe acute pancreatitis. Nutrition. 1998 Mar;14(3):261-5. | PubMed |
de Beaux AC, O'Riordain MG, Ross JA, Jodozi L, Carter DC, Fearon KC. Glutamine-supplemented total parenteral nutrition reduces blood mononuclear cell interleukin-8 release in severe acute pancreatitis. Nutrition. 1998 Mar;14(3):261-5. | PubMed | Déchelotte P, Hasselmann M, Cynober L, Allaouchiche B, Coëffier M, Hecketsweiler B, et al. L-alanyl-L-glutamine dipeptide-supplemented total parenteral nutrition reduces infectious complications and glucose intolerance in critically ill patients: the French controlled, randomized, double-blind, multicenter study. Crit Care Med. 2006 Mar;34(3):598-604. | PubMed |
Déchelotte P, Hasselmann M, Cynober L, Allaouchiche B, Coëffier M, Hecketsweiler B, et al. L-alanyl-L-glutamine dipeptide-supplemented total parenteral nutrition reduces infectious complications and glucose intolerance in critically ill patients: the French controlled, randomized, double-blind, multicenter study. Crit Care Med. 2006 Mar;34(3):598-604. | PubMed | Fuentes-Orozco C, Cervantes-Guevara G, Muciño-Hernández I, López-Ortega A, Ambriz-González G, Gutiérrez-de-la-Rosa JL, et al. L-alanyl-L-glutamine-supplemented parenteral nutrition decreases infectious morbidity rate in patients with severe acute pancreatitis. JPEN J Parenter Enteral Nutr. 2008 Jul-Aug;32(4):403-11. | CrossRef | PubMed |
Fuentes-Orozco C, Cervantes-Guevara G, Muciño-Hernández I, López-Ortega A, Ambriz-González G, Gutiérrez-de-la-Rosa JL, et al. L-alanyl-L-glutamine-supplemented parenteral nutrition decreases infectious morbidity rate in patients with severe acute pancreatitis. JPEN J Parenter Enteral Nutr. 2008 Jul-Aug;32(4):403-11. | CrossRef | PubMed | Guo Y, Xia M. Effect of Glutamine on Nutrition State in Severe Acute Pancreatitis. Clinical Journal of Medical Officer; 2006. | Link |
Guo Y, Xia M. Effect of Glutamine on Nutrition State in Severe Acute Pancreatitis. Clinical Journal of Medical Officer; 2006. | Link | Hajdú N, Belágyi T, Issekutz A, Bartek P, Gartner B, Oláh A. [Intravenous glutamine and early nasojejunal nutrition in severe acute pancreatitis -- a prospective randomized clinical study]. Magy Seb. 2012 Apr;65(2):44-51. | CrossRef | PubMed |
Hajdú N, Belágyi T, Issekutz A, Bartek P, Gartner B, Oláh A. [Intravenous glutamine and early nasojejunal nutrition in severe acute pancreatitis -- a prospective randomized clinical study]. Magy Seb. 2012 Apr;65(2):44-51. | CrossRef | PubMed | Hallay J, Kovács G, Szatmári K, Bakó A, Szentkereszty Z, Lakos G, et al. Early jejunal nutrition and changes in the immunological parameters of patients with acute pancreatitis. Hepatogastroenterology. 2001 Sep-Oct;48(41):1488-92. | PubMed |
Hallay J, Kovács G, Szatmári K, Bakó A, Szentkereszty Z, Lakos G, et al. Early jejunal nutrition and changes in the immunological parameters of patients with acute pancreatitis. Hepatogastroenterology. 2001 Sep-Oct;48(41):1488-92. | PubMed | Hallay J, Kovács G, Kiss Sz S, Farkas M, Lakos G, Sipka S, et al. Changes in the nutritional state and immune-serological parameters of esophagectomized patients fed jejunaly with glutamine-poor and glutamine-rich nutriments. Hepatogastroenterology. 2002 Nov-Dec;49(48):1555-9. | PubMed |
Hallay J, Kovács G, Kiss Sz S, Farkas M, Lakos G, Sipka S, et al. Changes in the nutritional state and immune-serological parameters of esophagectomized patients fed jejunaly with glutamine-poor and glutamine-rich nutriments. Hepatogastroenterology. 2002 Nov-Dec;49(48):1555-9. | PubMed | Hallay J, Kovacs G, Szatmari, K, Bako A, Szentkereszty Z, Lakos, G [Changes in the nutritional status and immunological parameters of patients with acute necrotizing pancreatitis after the use of nasojejunal tube feeding] Táplálkozás allergia diéta 2000. | Link |
Hallay J, Kovacs G, Szatmari, K, Bako A, Szentkereszty Z, Lakos, G [Changes in the nutritional status and immunological parameters of patients with acute necrotizing pancreatitis after the use of nasojejunal tube feeding] Táplálkozás allergia diéta 2000. | Link | Han M, Liu T, Liu, Gang, Wang Peng-zhi. Clinical observation of immune nutritional agent on the treatment effect in patients with severe pancreatitis. Journal of Tianjin Medical University.2011(2). | Link |
Han M, Liu T, Liu, Gang, Wang Peng-zhi. Clinical observation of immune nutritional agent on the treatment effect in patients with severe pancreatitis. Journal of Tianjin Medical University.2011(2). | Link | Huang XX, Wang XP, Ma JJ, Jing DD, Wang PW, Wu K. [Effects of enteral nutrition supplemented with glutamine and arginine on gut barrier in patients with severe acute pancreatitis: a prospective randomized controlled trial]. Zhonghua Yi Xue Za Zhi. 2008 Sep 9;88(34):2407-9. | PubMed |
Huang XX, Wang XP, Ma JJ, Jing DD, Wang PW, Wu K. [Effects of enteral nutrition supplemented with glutamine and arginine on gut barrier in patients with severe acute pancreatitis: a prospective randomized controlled trial]. Zhonghua Yi Xue Za Zhi. 2008 Sep 9;88(34):2407-9. | PubMed | Huang Xiao-xi, Wang, Xing-peng, Wu Kai, XU Chun-fang, Chen Wei-chang, et al. Effect of early continuous enteral nutrition combined with interstinal mucosal protective agents on gut barrier in patients with severe acute pancreatitis: A multicenter prospective randomized controlled trial. Chinese Journal of Digestion. 2008. | Link |
Huang Xiao-xi, Wang, Xing-peng, Wu Kai, XU Chun-fang, Chen Wei-chang, et al. Effect of early continuous enteral nutrition combined with interstinal mucosal protective agents on gut barrier in patients with severe acute pancreatitis: A multicenter prospective randomized controlled trial. Chinese Journal of Digestion. 2008. | Link | Ockenga J, Borchert K, Rifai K, Manns MP, Bischoff SC. Effect of glutamine-enriched total parenteral nutrition in patients with acute pancreatitis. Clin Nutr. 2002 Oct;21(5):409-16. | PubMed |
Ockenga J, Borchert K, Rifai K, Manns MP, Bischoff SC. Effect of glutamine-enriched total parenteral nutrition in patients with acute pancreatitis. Clin Nutr. 2002 Oct;21(5):409-16. | PubMed | Pearce CB, Sadek SA, Walters AM, Goggin PM, Somers SS, Toh SK, et al. A double-blind, randomised, controlled trial to study the effects of an enteral feed supplemented with glutamine, arginine, and omega-3 fatty acid in predicted acute severe pancreatitis. JOP. 2006 Jul 10;7(4):361-71. | PubMed |
Pearce CB, Sadek SA, Walters AM, Goggin PM, Somers SS, Toh SK, et al. A double-blind, randomised, controlled trial to study the effects of an enteral feed supplemented with glutamine, arginine, and omega-3 fatty acid in predicted acute severe pancreatitis. JOP. 2006 Jul 10;7(4):361-71. | PubMed | Poropat G, Giljaca V, Hauser G, timac D. Enteral nutrition formulations for acute pancreatitis. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No.: CD010605. | CrossRef |
Poropat G, Giljaca V, Hauser G, timac D. Enteral nutrition formulations for acute pancreatitis. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No.: CD010605. | CrossRef | Ong JP, Fock KM. Nutritional support in acute pancreatitis. J Dig Dis. 2012 Sep;13(9):445-52.
| CrossRef | PubMed |
Ong JP, Fock KM. Nutritional support in acute pancreatitis. J Dig Dis. 2012 Sep;13(9):445-52.
| CrossRef | PubMed | Sahin H, Mercanligil SM, Inanç N, Ok E. Effects of glutamine-enriched total parenteral nutrition on acute pancreatitis. Eur J Clin Nutr. 2007 Dec;61(12):1429-34. Epub 2007 Feb 21. | PubMed |
Sahin H, Mercanligil SM, Inanç N, Ok E. Effects of glutamine-enriched total parenteral nutrition on acute pancreatitis. Eur J Clin Nutr. 2007 Dec;61(12):1429-34. Epub 2007 Feb 21. | PubMed | Tong Zhi-hui, LiI Wei-qin, YU Wen-kui, Wang Xin-ying, Ye Xiang-hong, Li Ning,et al. Effects of early enteral nutrition and glutamine-supplemented EEN on the inflammatory response and immune function in patients with severe acute pancreatitis. Parenteral & Enteral Nutrition. 2009(05). | CrossRef |
Tong Zhi-hui, LiI Wei-qin, YU Wen-kui, Wang Xin-ying, Ye Xiang-hong, Li Ning,et al. Effects of early enteral nutrition and glutamine-supplemented EEN on the inflammatory response and immune function in patients with severe acute pancreatitis. Parenteral & Enteral Nutrition. 2009(05). | CrossRef | Wang YZ, Ding YB, Wu J, Deng B, Xiao WM. Treatment of 64 cases severe acute pancreatitis with early enteral nutrition and intestinal barrier protective agents. World Chinese Journal of Digestology. 2007
| Link |
Wang YZ, Ding YB, Wu J, Deng B, Xiao WM. Treatment of 64 cases severe acute pancreatitis with early enteral nutrition and intestinal barrier protective agents. World Chinese Journal of Digestology. 2007
| Link | Wang, Z, Huang SW, Liu P. Significance of Application of Total Parenteral Nutrition Associated with Alanyl-glutamine on Patients with Acute Severe Pancreatitis. Practical Preventive Medicine. 2009. | CrossRef |
Wang, Z, Huang SW, Liu P. Significance of Application of Total Parenteral Nutrition Associated with Alanyl-glutamine on Patients with Acute Severe Pancreatitis. Practical Preventive Medicine. 2009. | CrossRef | Xian-li H, Qing-jiu M, Jian-guo L, Yan-kui, C, Xi-lin D. Effect of total parenteral nutrition (TPN) with and without glutamine dipeptide supplementation on outcome in severe acute pancreatitis (SAP). Clinical Nutrition Supplements. 2004. | CrossRef |
Xian-li H, Qing-jiu M, Jian-guo L, Yan-kui, C, Xi-lin D. Effect of total parenteral nutrition (TPN) with and without glutamine dipeptide supplementation on outcome in severe acute pancreatitis (SAP). Clinical Nutrition Supplements. 2004. | CrossRef | Xue P, Deng LH, Xia Q, Zhang ZD, Hu WM, Yang XN, Song B, Huang ZW. Impact of alanyl-glutamine dipeptide on severe acute pancreatitis in early stage. World J Gastroenterol. 2008 Jan 21;14(3):474-8. | PubMed |
Xue P, Deng LH, Xia Q, Zhang ZD, Hu WM, Yang XN, Song B, Huang ZW. Impact of alanyl-glutamine dipeptide on severe acute pancreatitis in early stage. World J Gastroenterol. 2008 Jan 21;14(3):474-8. | PubMed | Yang SQ, Xu JG. [Effect of glutamine on serum interleukin-8 and tumor necrosis factor-alpha levels in patients with severe pancreatitis]. Nan Fang Yi Ke Da Xue Xue Bao. 2008 Jan;28(1):129-31. | PubMed |
Yang SQ, Xu JG. [Effect of glutamine on serum interleukin-8 and tumor necrosis factor-alpha levels in patients with severe pancreatitis]. Nan Fang Yi Ke Da Xue Xue Bao. 2008 Jan;28(1):129-31. | PubMed | Zhao G, Zhang JG, Wu HS, Tao J, Qin Q, Deng SC, et al. Effects of different resuscitation fluid on severe acute pancreatitis. World J Gastroenterol. 2013 Apr 7;19(13):2044-52. | CrossRef | PubMed |
Zhao G, Zhang JG, Wu HS, Tao J, Qin Q, Deng SC, et al. Effects of different resuscitation fluid on severe acute pancreatitis. World J Gastroenterol. 2013 Apr 7;19(13):2044-52. | CrossRef | PubMed | Zhao G, Wang CY, Wang F, Xiong JX. Clinical study on nutrition support in patients with severe acute pancreatitis. World J Gastroenterol. 2003 Sep;9(9):2105-8. | PubMed |
Zhao G, Wang CY, Wang F, Xiong JX. Clinical study on nutrition support in patients with severe acute pancreatitis. World J Gastroenterol. 2003 Sep;9(9):2105-8. | PubMed | Zhou RX. Effect of Glutamine-Fortified Early Intensive Enteral Nutrition in Patients with Severe Acute Pancreatitis. Herald of Medicine.2013(7)
| Link |
Zhou RX. Effect of Glutamine-Fortified Early Intensive Enteral Nutrition in Patients with Severe Acute Pancreatitis. Herald of Medicine.2013(7)
| Link | Huan Bin, Chen Shaopeng, Yang Li, Ding Zhuoqi. Severe acute pancreatitis application alanyl - glutamine was observed after treatment. Medical Information. 2011. | Link |
Huan Bin, Chen Shaopeng, Yang Li, Ding Zhuoqi. Severe acute pancreatitis application alanyl - glutamine was observed after treatment. Medical Information. 2011. | Link | He X-L, Ma Q-J, Lu J-G, et al. Effect of the application of total parenteral nutririon (TPN) and glutamine-supplemented TPN on patients with serious acute pancreatitis. Journal of the Fourth Military Medical University. 2002;23(21):1978-1981. | CrossRef |
He X-L, Ma Q-J, Lu J-G, et al. Effect of the application of total parenteral nutririon (TPN) and glutamine-supplemented TPN on patients with serious acute pancreatitis. Journal of the Fourth Military Medical University. 2002;23(21):1978-1981. | CrossRef | Lv X-F, Fang L-F, Ma R-L, et al. Influence of early glutamine supplemented enteral nutrition on the nutritional status of patients with severe acute pancreatitis. Chinese Pract Med. 2013;8(15):104-105 | Link |
Lv X-F, Fang L-F, Ma R-L, et al. Influence of early glutamine supplemented enteral nutrition on the nutritional status of patients with severe acute pancreatitis. Chinese Pract Med. 2013;8(15):104-105 | Link | Wáng Zhàn, Huángshèn Gwàng, Liú Péi, Liú Shǒu Jì, Wáng Qīng. Significance of Application of Total Parenteral Nutrition Associated with Alanyl-glutamine on Patients with Acute Severe Pan creatitis. Practical Preventive Medicine. 2009. | CrossRef |
Wáng Zhàn, Huángshèn Gwàng, Liú Péi, Liú Shǒu Jì, Wáng Qīng. Significance of Application of Total Parenteral Nutrition Associated with Alanyl-glutamine on Patients with Acute Severe Pan creatitis. Practical Preventive Medicine. 2009. | CrossRef | Zhao Huimin, Huang Qian. Alanyl - glutamine prevention of Severe Acute intestinal failure in clinical research. Chinese Journal of Clinical Rational Drug Use. 2010. | CrossRef |
Zhao Huimin, Huang Qian. Alanyl - glutamine prevention of Severe Acute intestinal failure in clinical research. Chinese Journal of Clinical Rational Drug Use. 2010. | CrossRef | Huang X, Huang H. Application of alany-glutamine dipeptide in patients with serious acute pancreatitis. Mod Diagn Treat. 2010;21(6): 342-343. | CrossRef |
Huang X, Huang H. Application of alany-glutamine dipeptide in patients with serious acute pancreatitis. Mod Diagn Treat. 2010;21(6): 342-343. | CrossRef | Tenner S, Baillie J, DeWitt J, Vege SS; American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416. | CrossRef | PubMed |
Tenner S, Baillie J, DeWitt J, Vege SS; American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416. | CrossRef | PubMed | American Gastroenterological Association (AGA) Institute on "Management of Acute Pancreatits" Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute medical position statement on acute pancreatitis. Gastroenterology. 2007 May;132(5):2019-21. | CrossRef | PubMed |
American Gastroenterological Association (AGA) Institute on "Management of Acute Pancreatits" Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute medical position statement on acute pancreatitis. Gastroenterology. 2007 May;132(5):2019-21. | CrossRef | PubMed | Forsmark CE, Baillie J; AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute
pancreatitis. Gastroenterology. 2007 May;132(5):2022-44. | PubMed |
Forsmark CE, Baillie J; AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute
pancreatitis. Gastroenterology. 2007 May;132(5):2022-44. | PubMed | Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul;13(4 Suppl 2):e1-e15. | CrossRef | PubMed |
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul;13(4 Suppl 2):e1-e15. | CrossRef | PubMed | Saraya A. A clinical trial to study the effects of glutamine (an amino acid)supplementation in patients with acute pancreatitis. Clinical Trials Registry - India. CTRI/2009/091/000945 [on line]. | Link |
Saraya A. A clinical trial to study the effects of glutamine (an amino acid)supplementation in patients with acute pancreatitis. Clinical Trials Registry - India. CTRI/2009/091/000945 [on line]. | Link | Asian Institute of Gastroenterology, India. Efficacy of Enteral Glutamine Supplementation in Patients With Predicted Severe Acute Pancreatitis- A Double-Blinded Randomized Controlled Trial. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). 2016. [on line]. | Link |
Asian Institute of Gastroenterology, India. Efficacy of Enteral Glutamine Supplementation in Patients With Predicted Severe Acute Pancreatitis- A Double-Blinded Randomized Controlled Trial. In: ClinicalTrials.gov. Bethesda (MD): National Library of Medicine (US). 2016. [on line]. | Link |