 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
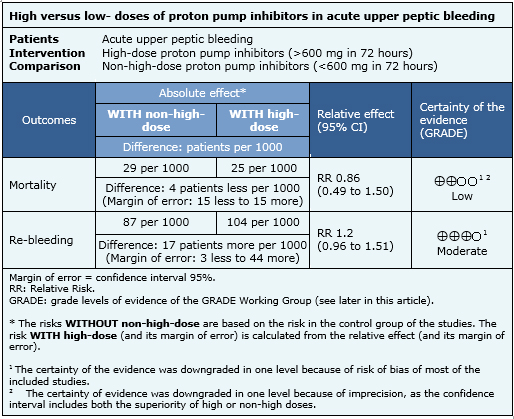
Although there is broad consensus about the benefits of proton pump inhibitors in acute upper peptic bleeding, there is still controversy over their optimal dosing. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified six systematic reviews including 27 randomized trials addressing this question. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded high-dose proton pump inhibitors probably result in little or no difference in re-bleeding rate or mortality. The risk/benefit and cost/benefit balance probably favor use of low-doses.
Acute upper peptic bleeding is a serious clinical problem often requiring management in critical care units, and is associated with important morbidity and mortality.Proton pump inhibitors effectively block gastric acid secretion, favoring the healing of ulcer and halting of bleeding. The benefits of these drugs in acute upper peptic bleeding are widely recognized, but there is still controversy over their optimal dosing in this setting.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
|
What is the evidence. |
We found six systematic reviews [1],[2],[3],[4],[5],[6] that included 27 randomized controlled trials [7],[8],[9], [10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20], [21],[22],[23],[24],[25],[26],[27],[28],[29],[31],[32],[33]. |
|
What types of patients were included |
All of the studies included adult patients hospitalized for acute upper peptic bleeding. In 19 studies all patients achieved endoscopic hemostasis prior to receiving proton pump inhibitors [7],[8],[11],[13],[14], [15],[17],[18],[19],[20],[21],[22],[23],[24],[25],[26],[27], [28],[31],[32]. In six studies prior endoscopic hemostasis was achieved in some but not all patients [10],[12],[16],[25],[30],[33]. In two studies the information about endoscopic hemostasis was not available [9],[29]. In 14 studies ulcer characteristics were used as inclusion criteria. Thirteen studies exclusively included patients with bleeding secondary to Forrest IA to IIB ulcers [7],[8],[14],[15],[16],[17],[18],[19],[26],[27],[28],[31],[32], and only one study included Forrest IA to III ulcers [9]. |
|
What types of interventions were included |
All studies compared ‘high-dose’ proton pump inhibitors (accumulated dose of 600 mg or more in the first 72 hours) against ‘non-high’ dose (accumulated dose of less than 600 mg in first 72 hours). In all studies 'high-dose' consisted in 80 mg bolus followed by a continuous infusion of 8 mg/hour for at least 72 hours. In 18 studies ’non-high’ dose was administered by intermittent intravenous bolus [7],[8],[10],[11],[12],[13],[14],[15],[16],[17],[18],[19],[20], [22],[24],[26],[28],[30],[31]. In eight studies it was administered orally [9],[15],[21],[23],[25],[27],[29],[32], while only one study used a low dose continuous infusion [33]. |
|
What types of outcomes |
The systematic reviews identified pooled the following outcomes:
|
The information about the effects of different doses of proton pump inhibitors in acute upper peptic bleeding is based on 21 of 27 randomized studies identified, including 2565 patients. Thirteen studies evaluated mortality [7],[9],[10],[13],[16],[19],[21],[25],[26],[29],[30],[31],[33] and 21 studies evaluated re-bleeding [7],[8],[9],[10],[13],[14],[15],[16],[17],[18],[19],[21],[25],[26],[27],[28],[29],[30],[31],[32],[33]. In the remaining six studies the data could not be extracted for meta-analysis [11],[12],[20],[22],[23],[24]. The summary of the results is the following:

|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
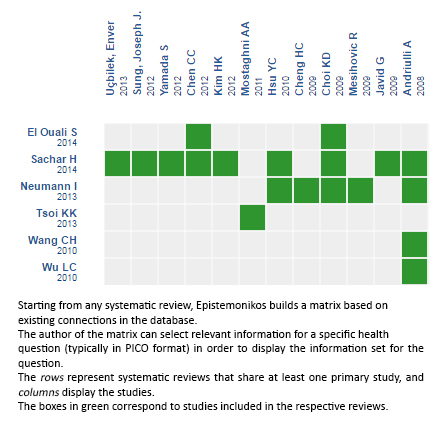
Follow the link to access the interactive version: High-dose versus non-high-dose proton pump inhibitors for bleeding peptic ulcer
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Although there is broad consensus about the benefits of proton pump inhibitors in acute upper peptic bleeding, there is still controversy over their optimal dosing. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified six systematic reviews including 27 randomized trials addressing this question. We combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded high-dose proton pump inhibitors probably result in little or no difference in re-bleeding rate or mortality. The risk/benefit and cost/benefit balance probably favor use of low-doses.
 Autores:
Alejandro Villalón[1,2], Roberto Olmos[1,2], Gabriel Rada[1,2,3,4,5]
Autores:
Alejandro Villalón[1,2], Roberto Olmos[1,2], Gabriel Rada[1,2,3,4,5]

Citación: Villalón A, Olmos R, Rada G. Are higher doses of proton pump inhibitors better in acute peptic bleeding? . Medwave 2016;16(Suppl 2):e6476 doi: 10.5867/medwave.2016.6476
Fecha de publicación: 24/6/2016

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Neumann I, Letelier LM, Rada G, Claro JC, Martin J, Howden CW, et alI. Comparison of different regimens of proton pump inhibitors for acute peptic ulcer bleeding. Cochrane Database Syst Rev. 2013 Jun 12;(6):CD007999. | CrossRef | PubMed |
Neumann I, Letelier LM, Rada G, Claro JC, Martin J, Howden CW, et alI. Comparison of different regimens of proton pump inhibitors for acute peptic ulcer bleeding. Cochrane Database Syst Rev. 2013 Jun 12;(6):CD007999. | CrossRef | PubMed | Wang CH, Ma MH, Chou HC, Yen ZS, Yang CW, Fang CC, et al. High-dose vs non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010 May 10;170(9):751-8. | CrossRef | PubMed |
Wang CH, Ma MH, Chou HC, Yen ZS, Yang CW, Fang CC, et al. High-dose vs non-high-dose proton pump inhibitors after endoscopic treatment in patients with bleeding peptic ulcer: a systematic review and meta-analysis of randomized controlled trials. Arch Intern Med. 2010 May 10;170(9):751-8. | CrossRef | PubMed | Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013 Oct;38(7):721-8. | CrossRef | PubMed |
Tsoi KK, Hirai HW, Sung JJ. Meta-analysis: comparison of oral vs. intravenous proton pump inhibitors in patients with peptic ulcer bleeding. Aliment Pharmacol Ther. 2013 Oct;38(7):721-8. | CrossRef | PubMed | El Ouali S, Barkun A, Martel M, Maggio D. Timing of rebleeding in high-risk peptic ulcer bleeding after successful hemostasis: a systematic review. Can J Gastroenterol Hepatol. 2014 Nov;28(10):543-8 | PubMed |
El Ouali S, Barkun A, Martel M, Maggio D. Timing of rebleeding in high-risk peptic ulcer bleeding after successful hemostasis: a systematic review. Can J Gastroenterol Hepatol. 2014 Nov;28(10):543-8 | PubMed | Wu LC, Cao YF, Huang JH, Liao C, Gao F. High-dose vs low-dose proton pump inhibitors for upper gastrointestinal bleeding: a meta-analysis. World J Gastroenterol. 2010 May 28;16(20):2558-65. | PubMed |
Wu LC, Cao YF, Huang JH, Liao C, Gao F. High-dose vs low-dose proton pump inhibitors for upper gastrointestinal bleeding: a meta-analysis. World J Gastroenterol. 2010 May 28;16(20):2558-65. | PubMed | Sachar H, Vaidya K, Laine L. Intermittent vs continuous proton pump inhibitor therapy for high-risk bleeding ulcers: a systematic review and meta-analysis. JAMA Intern Med. 2014 Nov;174(11):1755-62. | CrossRef | PubMed |
Sachar H, Vaidya K, Laine L. Intermittent vs continuous proton pump inhibitor therapy for high-risk bleeding ulcers: a systematic review and meta-analysis. JAMA Intern Med. 2014 Nov;174(11):1755-62. | CrossRef | PubMed | Andriulli A, Loperfido S, Focareta R, Leo P, Fornari F, Garripoli A, et al. High- versus low-dose proton pump inhibitors after endoscopic hemostasis in patients with peptic ulcer bleeding: a multicentre, randomized study. Am J Gastroenterol. 2008 Dec;103(12):3011-8. | CrossRef | PubMed |
Andriulli A, Loperfido S, Focareta R, Leo P, Fornari F, Garripoli A, et al. High- versus low-dose proton pump inhibitors after endoscopic hemostasis in patients with peptic ulcer bleeding: a multicentre, randomized study. Am J Gastroenterol. 2008 Dec;103(12):3011-8. | CrossRef | PubMed | Yamada S, Wongwanakul P. Randomized controlled trial of high dose bolus versus continuous intravenous infusion pantoprazole as an adjunct therapy to therapeutic endoscopy in massive bleeding peptic ulcer. J Med Assoc Thai. 2012 Mar;95(3):349-57. | PubMed |
Yamada S, Wongwanakul P. Randomized controlled trial of high dose bolus versus continuous intravenous infusion pantoprazole as an adjunct therapy to therapeutic endoscopy in massive bleeding peptic ulcer. J Med Assoc Thai. 2012 Mar;95(3):349-57. | PubMed | Mostaghni AA, Hashemi SA, Heydari ST. Comparison of oral and intravenous proton pump inhibitor on patients with high risk bleeding peptic ulcers: a prospective, randomized, controlled clinical trial. Iran Red Crescent Med J. 2011 Jul;13(7):458-63. | PubMed |
Mostaghni AA, Hashemi SA, Heydari ST. Comparison of oral and intravenous proton pump inhibitor on patients with high risk bleeding peptic ulcers: a prospective, randomized, controlled clinical trial. Iran Red Crescent Med J. 2011 Jul;13(7):458-63. | PubMed | Garrido A, Giráldez A, Trigo C, Leo E, Guil A, Márquez JL. [Intravenous proton-pump inhibitor for acute peptic ulcer bleeding--is profound acid suppression beneficial to reduce the risk of rebleeding?]. Rev Esp Enferm Dig. 2008 Aug;100(8):466-9. | PubMed |
Garrido A, Giráldez A, Trigo C, Leo E, Guil A, Márquez JL. [Intravenous proton-pump inhibitor for acute peptic ulcer bleeding--is profound acid suppression beneficial to reduce the risk of rebleeding?]. Rev Esp Enferm Dig. 2008 Aug;100(8):466-9. | PubMed | Lin HJ, Lo WC, Cheng YC, Perng CL. Role of intravenous omeprazole in patients with high-risk peptic ulcer bleeding after successful endoscopic epinephrine injection: a prospective randomized comparative trial. Am J Gastroenterol. 2006 Mar;101(3):500-5. | PubMed |
Lin HJ, Lo WC, Cheng YC, Perng CL. Role of intravenous omeprazole in patients with high-risk peptic ulcer bleeding after successful endoscopic epinephrine injection: a prospective randomized comparative trial. Am J Gastroenterol. 2006 Mar;101(3):500-5. | PubMed | Dokas SM, Lazaraki GI, Kontoninas Z, Kouklakis GS, Adamidou A, Tsiaousi E, et al. Bolus intravenous omeprazole B.I.D. vs. continuous intravenous omeprazole infusion combined with endoscopic hemostasis in the treatment of peptic ulcer bleeding. Preliminary results. Gut. 2004 2004;53(Suppl VI):A290 (Abstract WED-G-6). | Link |
Dokas SM, Lazaraki GI, Kontoninas Z, Kouklakis GS, Adamidou A, Tsiaousi E, et al. Bolus intravenous omeprazole B.I.D. vs. continuous intravenous omeprazole infusion combined with endoscopic hemostasis in the treatment of peptic ulcer bleeding. Preliminary results. Gut. 2004 2004;53(Suppl VI):A290 (Abstract WED-G-6). | Link | Schonekas H, Ahrens H, Pannewick U, Ell C, Koop H, Petritsch W, et al. Comparison of two doses of intravenous pantoprazole in peptic ulcer bleeding. Gastroenterology. 1999;116(4 Part 2):A305 (G1336). | Link |
Schonekas H, Ahrens H, Pannewick U, Ell C, Koop H, Petritsch W, et al. Comparison of two doses of intravenous pantoprazole in peptic ulcer bleeding. Gastroenterology. 1999;116(4 Part 2):A305 (G1336). | Link | Choi KD, Kim N, Jang IJ, Park YS, Cho JY, Kim JR, et al. Optimal dose of intravenous pantoprazole in patients with peptic ulcer bleeding requiring endoscopic hemostasis in Korea. J Gastroenterol Hepatol. 2009 Oct;24(10):1617-24. | CrossRef | PubMed |
Choi KD, Kim N, Jang IJ, Park YS, Cho JY, Kim JR, et al. Optimal dose of intravenous pantoprazole in patients with peptic ulcer bleeding requiring endoscopic hemostasis in Korea. J Gastroenterol Hepatol. 2009 Oct;24(10):1617-24. | CrossRef | PubMed | Sung JJ, Suen B-y, Ching J, Chan FKL, Wu JC, Chiu PW, et al. 1079 Effects of Intravenous and Oral Esomeprazole in Prevention of Recurrent Bleeding From Peptic Ulcers After Endoscopic Therapy. Gastroenterology. 2012 2012;142(5):S-192-S-3. | CrossRef |
Sung JJ, Suen B-y, Ching J, Chan FKL, Wu JC, Chiu PW, et al. 1079 Effects of Intravenous and Oral Esomeprazole in Prevention of Recurrent Bleeding From Peptic Ulcers After Endoscopic Therapy. Gastroenterology. 2012 2012;142(5):S-192-S-3. | CrossRef | Cheng HC, Kao AW, Chuang CH, Sheu BS. The efficacy of high- and low-dose intravenous omeprazole in preventing rebleeding for patients with bleeding peptic ulcers and comorbid illnesses. Dig Dis Sci. 2005 Jul;50(7):1194-201. | PubMed |
Cheng HC, Kao AW, Chuang CH, Sheu BS. The efficacy of high- and low-dose intravenous omeprazole in preventing rebleeding for patients with bleeding peptic ulcers and comorbid illnesses. Dig Dis Sci. 2005 Jul;50(7):1194-201. | PubMed | Javid G, Zargar SA, U-Saif R, Khan BA, Yatoo GN, Shah AH, et al. Comparison of p.o. or i.v. proton pump inhibitors on 72-h intragastric pH in bleeding peptic ulcer. J Gastroenterol Hepatol. 2009 Jul;24(7):1236-43. | CrossRef | PubMed |
Javid G, Zargar SA, U-Saif R, Khan BA, Yatoo GN, Shah AH, et al. Comparison of p.o. or i.v. proton pump inhibitors on 72-h intragastric pH in bleeding peptic ulcer. J Gastroenterol Hepatol. 2009 Jul;24(7):1236-43. | CrossRef | PubMed | Uçbilek E, Sezgin O, Altintas E. Low Dose Bolus Pantoprazole Following Succesful Endoscopic Treatment for Acute Peptic Ulcer Bleeding Is Effective: A Randomised, Prospective, Double-Blind, Double Dummy Pilot Study. Gastroenterology. 2013 2013;144(5, Supplement 1):S-506. | CrossRef |
Uçbilek E, Sezgin O, Altintas E. Low Dose Bolus Pantoprazole Following Succesful Endoscopic Treatment for Acute Peptic Ulcer Bleeding Is Effective: A Randomised, Prospective, Double-Blind, Double Dummy Pilot Study. Gastroenterology. 2013 2013;144(5, Supplement 1):S-506. | CrossRef | Yüksel I, Ataseven H, Köklü S, Ertuğrul I, Başar O, Odemiş B, et al. Intermittent versus continuous pantoprazole infusion in peptic ulcer bleeding: a prospective randomized study. Digestion. 2008;78(1):39-43. | CrossRef | PubMed |
Yüksel I, Ataseven H, Köklü S, Ertuğrul I, Başar O, Odemiş B, et al. Intermittent versus continuous pantoprazole infusion in peptic ulcer bleeding: a prospective randomized study. Digestion. 2008;78(1):39-43. | CrossRef | PubMed | Mesihovic R, Vanis N, Mehmedovic A, Gornjakovic S, Gribajcevic M. Proton pump inhibitors after endoscopic hemostasis in patients with peptic ulcer bleeding. Med Arh. 2009;63(6):323-7. | PubMed |
Mesihovic R, Vanis N, Mehmedovic A, Gornjakovic S, Gribajcevic M. Proton pump inhibitors after endoscopic hemostasis in patients with peptic ulcer bleeding. Med Arh. 2009;63(6):323-7. | PubMed | Jang JY, Dong SH, Jung JH, Chae MJ, Kim NH, Lee SK, et al. High-dose oral proton pump inhibitor is as effective as intravenous administration in the aspect of increasing intragastric pH and reducing rebleeding after endoscopic treatment of bleeding peptic ulcers. Digestive Disease Week; 20062006. p. TI067. | Link |
Jang JY, Dong SH, Jung JH, Chae MJ, Kim NH, Lee SK, et al. High-dose oral proton pump inhibitor is as effective as intravenous administration in the aspect of increasing intragastric pH and reducing rebleeding after endoscopic treatment of bleeding peptic ulcers. Digestive Disease Week; 20062006. p. TI067. | Link | Chilovi F, Piazzi L, Zancanella L, De Guelmi A, Grasso T, Di Fede F, et al. Intravenous omeprazole and pantoprazole after endoscopic treatment of bleeding peptic ulcers. Gastrointestinal Endoscopy. 2003 2003;57(5):AB150. | Link |
Chilovi F, Piazzi L, Zancanella L, De Guelmi A, Grasso T, Di Fede F, et al. Intravenous omeprazole and pantoprazole after endoscopic treatment of bleeding peptic ulcers. Gastrointestinal Endoscopy. 2003 2003;57(5):AB150. | Link | Focareta R, Ciarleglio A, Piai G, Levoli F, Forte G. Proton-pump inhibitor (PPI) and acute peptic ulcer bleeding: effectiveness of oral esomeprazole vs intravenous omeprazole in reducing the risk of recurrent bleeding. X Congresso Nazionale delle Malattie Digestive. 2004. | Link |
Focareta R, Ciarleglio A, Piai G, Levoli F, Forte G. Proton-pump inhibitor (PPI) and acute peptic ulcer bleeding: effectiveness of oral esomeprazole vs intravenous omeprazole in reducing the risk of recurrent bleeding. X Congresso Nazionale delle Malattie Digestive. 2004. | Link | Oh JH, Choi MG, Dong MS, Park JM, Paik CN, Cho YK, et al. Low-dose intravenous pantoprazole for optimal inhibition of gastric acid in Korean patients. J Gastroenterol Hepatol. 2007 Sep;22(9):1429-34.
| PubMed |
Oh JH, Choi MG, Dong MS, Park JM, Paik CN, Cho YK, et al. Low-dose intravenous pantoprazole for optimal inhibition of gastric acid in Korean patients. J Gastroenterol Hepatol. 2007 Sep;22(9):1429-34.
| PubMed | Bajaj JS, Dua KS, Hanson K, Presberg K. Prospective, randomized trial comparing effect of oral versus intravenous pantoprazole on rebleeding after nonvariceal upper gastrointestinal bleeding: a pilot study. Dig Dis Sci. 2007 Sep;52(9):2190-4. | PubMed |
Bajaj JS, Dua KS, Hanson K, Presberg K. Prospective, randomized trial comparing effect of oral versus intravenous pantoprazole on rebleeding after nonvariceal upper gastrointestinal bleeding: a pilot study. Dig Dis Sci. 2007 Sep;52(9):2190-4. | PubMed | Hsu YC, Perng CL, Yang TH, Wang CS, Hsu WL, Wu HT, et al. A randomized controlled trial comparing two different dosages of infusional pantoprazole in peptic ulcer bleeding. Br J Clin Pharmacol. 2010 Mar;69(3):245-51.
| CrossRef | PubMed |
Hsu YC, Perng CL, Yang TH, Wang CS, Hsu WL, Wu HT, et al. A randomized controlled trial comparing two different dosages of infusional pantoprazole in peptic ulcer bleeding. Br J Clin Pharmacol. 2010 Mar;69(3):245-51.
| CrossRef | PubMed | Kim HK, Kim JS, Kim TH, Kim CW, Cho YS, Kim SS, et al. Effect of high-dose oral rabeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. Gastroenterol Res Pract. 2012;2012:317125. | CrossRef | PubMed |
Kim HK, Kim JS, Kim TH, Kim CW, Cho YS, Kim SS, et al. Effect of high-dose oral rabeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. Gastroenterol Res Pract. 2012;2012:317125. | CrossRef | PubMed | Chen CC, Lee JY, Fang YJ, Hsu SJ, Han ML, Tseng PH, et al. Randomised clinical trial: high-dose vs. standard-dose proton pump inhibitors for the prevention of recurrent haemorrhage after combined endoscopic haemostasis of bleeding peptic ulcers. Aliment Pharmacol Ther. 2012 Apr;35(8):894-903. | CrossRef | PubMed |
Chen CC, Lee JY, Fang YJ, Hsu SJ, Han ML, Tseng PH, et al. Randomised clinical trial: high-dose vs. standard-dose proton pump inhibitors for the prevention of recurrent haemorrhage after combined endoscopic haemostasis of bleeding peptic ulcers. Aliment Pharmacol Ther. 2012 Apr;35(8):894-903. | CrossRef | PubMed | Yilmaz S, Bayan K, Tüzün Y, Dursun M, Canoruç F. A head to head comparison of oral vs intravenous omeprazole for patients with bleeding peptic ulcers with a clean base, flat spots and adherent clots. World J Gastroenterol. 2006 Dec 28;12(48):7837-43. | PubMed |
Yilmaz S, Bayan K, Tüzün Y, Dursun M, Canoruç F. A head to head comparison of oral vs intravenous omeprazole for patients with bleeding peptic ulcers with a clean base, flat spots and adherent clots. World J Gastroenterol. 2006 Dec 28;12(48):7837-43. | PubMed | Udd M, Miettinen P, Palmu A, Heikkinen M, Janatuinen E, Pasanen P, Tarvainen R, Kairaluoma MV, Lohman M, Mustonen H, Julkunen R. Regular-dose versus high-dose omeprazole in peptic ulcer bleeding: a prospective randomized double-blind study. Scand J Gastroenterol. 2001 Dec;36(12):1332-8. | PubMed |
Udd M, Miettinen P, Palmu A, Heikkinen M, Janatuinen E, Pasanen P, Tarvainen R, Kairaluoma MV, Lohman M, Mustonen H, Julkunen R. Regular-dose versus high-dose omeprazole in peptic ulcer bleeding: a prospective randomized double-blind study. Scand J Gastroenterol. 2001 Dec;36(12):1332-8. | PubMed | Hung WK, Li VK, Chung CK, Ying MW, Loo CK, Liu CK, Lam BY, Chan MC. Randomized trial comparing pantoprazole infusion, bolus and no treatment on gastric pH and recurrent bleeding in peptic ulcers. ANZ J Surg. 2007 Aug;77(8):677-81. | PubMed |
Hung WK, Li VK, Chung CK, Ying MW, Loo CK, Liu CK, Lam BY, Chan MC. Randomized trial comparing pantoprazole infusion, bolus and no treatment on gastric pH and recurrent bleeding in peptic ulcers. ANZ J Surg. 2007 Aug;77(8):677-81. | PubMed | Jang JY, Joo KR, Hwangbo Y, Jeong LI, Choi SY, Jung JH, et al. A Comparison of the Effect of High-dose Oral and Intravenous Proton Pump Inhibitor on the Prevention of Rebleeding after Endoscopic Treatment of Bleeding Peptic Ulcers. Kr J of Gastrointest Endoscop. 2006;33(1):6-11. | Link |
Jang JY, Joo KR, Hwangbo Y, Jeong LI, Choi SY, Jung JH, et al. A Comparison of the Effect of High-dose Oral and Intravenous Proton Pump Inhibitor on the Prevention of Rebleeding after Endoscopic Treatment of Bleeding Peptic Ulcers. Kr J of Gastrointest Endoscop. 2006;33(1):6-11. | Link | Cheng HC, Chang WL, Yeh YC, Chen WY, Tsai YC, Sheu BS. Seven-day intravenous low-dose omeprazole infusion reduces peptic ulcer rebleeding for patients with comorbidities. Gastrointest Endosc. 2009 Sep;70(3):433-9. | CrossRef | PubMed |
Cheng HC, Chang WL, Yeh YC, Chen WY, Tsai YC, Sheu BS. Seven-day intravenous low-dose omeprazole infusion reduces peptic ulcer rebleeding for patients with comorbidities. Gastrointest Endosc. 2009 Sep;70(3):433-9. | CrossRef | PubMed | National Institute for Health and Clinical Excellence (NICE) (2012) Acute upper gastrointestinal bleeding in over 16s: management NICE guidelines [CG141]. [Online]. | Link |
National Institute for Health and Clinical Excellence (NICE) (2012) Acute upper gastrointestinal bleeding in over 16s: management NICE guidelines [CG141]. [Online]. | Link | Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012 Mar;107(3):345-60; quiz 361. | CrossRef | PubMed |
Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012 Mar;107(3):345-60; quiz 361. | CrossRef | PubMed | American Society for Gastrointestinal Endoscopy (ASGE) Standards of Practice Committee, Anderson MA, Appalaneni V, Ben-Menachem T, Decker GA, Early DS, et al. The role of endoscopy in the evaluation and treatment of patients with biliary neoplasia. Gastrointest Endosc. 2013 Feb;77(2):167-74. | CrossRef | PubMed |
American Society for Gastrointestinal Endoscopy (ASGE) Standards of Practice Committee, Anderson MA, Appalaneni V, Ben-Menachem T, Decker GA, Early DS, et al. The role of endoscopy in the evaluation and treatment of patients with biliary neoplasia. Gastrointest Endosc. 2013 Feb;77(2):167-74. | CrossRef | PubMed |