 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
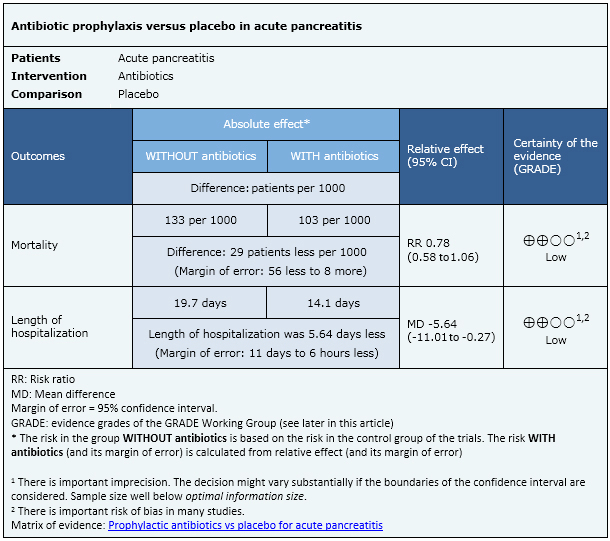
This Living FRISBEE (Living FRIendly Summary of the Body of Evidence using Epistemonikos) is an update of the summary published in August 2014, based on two systematic reviews appeared in January and February 2015. There is controversy about the effects of prophylactic antibiotics in acute pancreatitis. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified 18 systematic reviews including 19 randomised studies overall. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded that prophylactic antibiotics may reduce mortality and length of hospitalization in patients with acute pancreatitis, but the certainty of the evidence is low. The probability that future evidence change what we know is high.
The article updates the August 2014 Living FRISBEE (Living FRIendly Summary of the Body of Evidence using Epistemonikos) (doi: 10.5867/medwave.2014.07.6004) by including two new systematic reviews that appeared after publication of the original article [1],[2].
The new evidence incorporated in this summary does not lead to a modification on the certainty of the evidence, the key messages or other considerations for decision-making.
Notwithstanding, it is important to mention that our summary (consistent with the new reviews) is discordant with the results of the majority of previous systematic reviews and guidelines.
|
Key messages
|
Most cases of acute pancreatitis are mild but some patients develop a severe form of this condition characterized by organ dysfunction and/or local complications, such as pancreatic necrosis.
The initial stage is characterized by complications derived from the inflammatory systemic response, and in the second stage infectious complications might ensue with associated morbidity and mortality. Antibiotic prophylaxis has been proposed as an alternative to avoid the latter, but its use is controversial since it is also associated with adverse effects and antibiotic resistance.
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information, we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
What is the evidence.(See evidence matrix in Epistemonikos later).
|
We found 18 systematic reviews [1],[2],[3],[4],[5],[6],[7], |
| What types of patients were included. |
Most studies included patients with necrotizing pancreatitis [19],[29],[32],[35], severe pancreatitis [27],[33],[34],[38], any of these [24],[28],[31],[37], ], or severe necrotizing pancreatitis [22],[26],[30]. One study included patients with alcoholic pancreatitis plus two or more collections [21] and three old studies included patients based only on clinical and biochemical criteria [20],[23],[25]. |
|
What types of interventions were included. |
All studies except one [27] used intravenous antibiotics. Two studies used ampicillin [20],[23], one ampicillin or lincomycin [25], six imipenem [19],[28],[29],[30],[37],[38], two meropenem [22],[36], one ciprofloxacin [24] and three used a combination of ciprofloxacin and metronidazole [26],[34],[35]. Five studies allowed different antibiotic options [21],[22],[27],[31],[32]. |
|
What types of outcomes were measured. |
All studies measured mortality, but only three reported length of hospitalization. Other outcomes reported were pancreatic or peripancreatic infection, fungal infection, surgical intervention need, non-pancreatic infection, sepsis. |
This information is based on 19 studies including 1178 patients. All studies evaluated mortality but only three (153 patients) measured length of hospitalization.
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
Follow the link to access the interactive version Prophylactic antibiotics vs placebo for acute pancreatitis
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here: http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Potential conflicts of interest
The authors do not have relevant interests to declare.

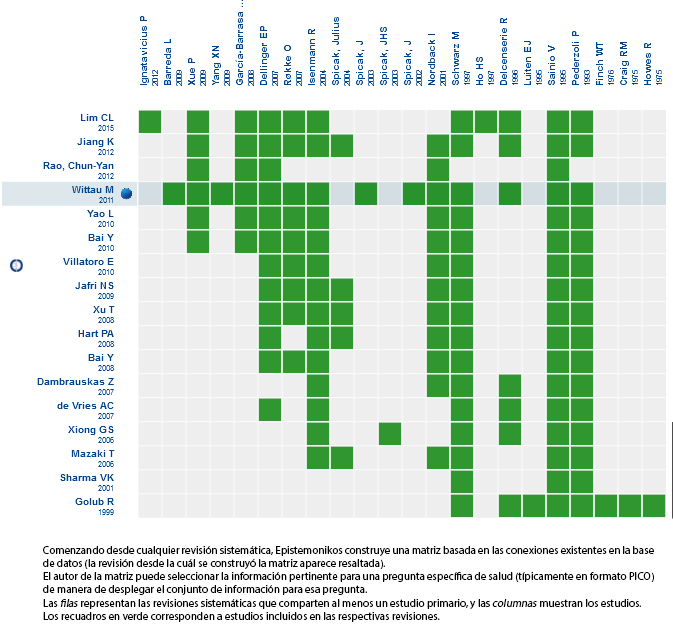 Matrix of evidence
Matrix of evidence
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

This Living FRISBEE (Living FRIendly Summary of the Body of Evidence using Epistemonikos) is an update of the summary published in August 2014, based on two systematic reviews appeared in January and February 2015. There is controversy about the effects of prophylactic antibiotics in acute pancreatitis. Searching in Epistemonikos database, which is maintained by screening 30 databases, we identified 18 systematic reviews including 19 randomised studies overall. We combined the evidence using meta-analysis and generated a summary of findings following the GRADE approach. We concluded that prophylactic antibiotics may reduce mortality and length of hospitalization in patients with acute pancreatitis, but the certainty of the evidence is low. The probability that future evidence change what we know is high.
 Autores:
Gabriel Rada[1,2,3,4,5], José Peña[1,2,5]
Autores:
Gabriel Rada[1,2,3,4,5], José Peña[1,2,5]

Citación: Rada G, Peña J. Is antibiotic prophylaxis beneficial in acute pancreatitis? - First update. Medwave 2015 Abr;15(3):e6125 doi: 10.5867/medwave.2015.03.6125
Fecha de publicación: 23/4/2015

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Lim CL, Lee W, Liew YX, Tang SS, Chlebicki MP, Kwa AL. Role of antibiotic prophylaxis in necrotizing pancreatitis: a meta-analysis. J Gastrointest Surg. 2015 Mar;19(3):480-91. | CrossRef | PubMed |
Lim CL, Lee W, Liew YX, Tang SS, Chlebicki MP, Kwa AL. Role of antibiotic prophylaxis in necrotizing pancreatitis: a meta-analysis. J Gastrointest Surg. 2015 Mar;19(3):480-91. | CrossRef | PubMed | Ukai T, Shikata S, Inoue M, Noguchi Y, Igarashi H, Isaji S, et al. Early prophylactic antibiotics administration for acute necrotizing pancreatitis: a meta-analysis of randomized controlled trials. J Hepatobiliary Pancreat Sci. 2015 Apr;22(4):316-21. | CrossRef | PubMed |
Ukai T, Shikata S, Inoue M, Noguchi Y, Igarashi H, Isaji S, et al. Early prophylactic antibiotics administration for acute necrotizing pancreatitis: a meta-analysis of randomized controlled trials. J Hepatobiliary Pancreat Sci. 2015 Apr;22(4):316-21. | CrossRef | PubMed | Sharma VK, Howden CW. Prophylactic antibiotic administration reduces sepsis and mortality in acute necrotizing pancreatitis: a meta-analysis. Pancreas. 2001 2001;22(1):28-31. | PubMed |
Sharma VK, Howden CW. Prophylactic antibiotic administration reduces sepsis and mortality in acute necrotizing pancreatitis: a meta-analysis. Pancreas. 2001 2001;22(1):28-31. | PubMed | Rao C-Y, Zhao X-Y, Hu C-L. Role of prophylactic antibiotics in the management of acute necrotizing pancreatitis: A meta-analysis. World Chinese Journal of Digestology. 2012;20(14):1246-51.
Rao C-Y, Zhao X-Y, Hu C-L. Role of prophylactic antibiotics in the management of acute necrotizing pancreatitis: A meta-analysis. World Chinese Journal of Digestology. 2012;20(14):1246-51.  Mazaki T1, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. Br J Surg. 2006 Jun;93(6):674-84. | CrossRef | PubMed |
Mazaki T1, Ishii Y, Takayama T. Meta-analysis of prophylactic antibiotic use in acute necrotizing pancreatitis. Br J Surg. 2006 Jun;93(6):674-84. | CrossRef | PubMed | Xiong GS1, Wu SM, Wang ZH. Role of prophylactic antibiotic administration in severe acute pancreatitis: a meta-analysis. Med Princ Pract. 2006;15(2):106-10. | CrossRef | PubMed |
Xiong GS1, Wu SM, Wang ZH. Role of prophylactic antibiotic administration in severe acute pancreatitis: a meta-analysis. Med Princ Pract. 2006;15(2):106-10. | CrossRef | PubMed | de Vries AC1, Besselink MG, Buskens E, Ridwan BU, Schipper M, van Erpecum KJ, et al. Randomized controlled trials of antibiotic prophylaxis in severe acute pancreatitis: relationship between methodological quality and outcome. Pancreatology. 2007;7(5-6):531-8. | CrossRef | PubMed |
de Vries AC1, Besselink MG, Buskens E, Ridwan BU, Schipper M, van Erpecum KJ, et al. Randomized controlled trials of antibiotic prophylaxis in severe acute pancreatitis: relationship between methodological quality and outcome. Pancreatology. 2007;7(5-6):531-8. | CrossRef | PubMed | Bai Y, Gao J, Zou DW, Li ZS. Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in acute necrotizing pancreatitis: evidence from a meta-analysis of randomized controlled trials. Am J Gastroenterol. 2008 Jan;103(1):104-10. | CrossRef | PubMed |
Bai Y, Gao J, Zou DW, Li ZS. Prophylactic antibiotics cannot reduce infected pancreatic necrosis and mortality in acute necrotizing pancreatitis: evidence from a meta-analysis of randomized controlled trials. Am J Gastroenterol. 2008 Jan;103(1):104-10. | CrossRef | PubMed | Villatoro E, Mulla M, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. 2010 May 12;(5):CD002941. | CrossRef | PubMed |
Villatoro E, Mulla M, Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. 2010 May 12;(5):CD002941. | CrossRef | PubMed | Hart PA, Bechtold ML, Marshall JB, Choudhary A, Puli SR, Roy PK. Prophylactic antibiotics in necrotizing pancreatitis: a meta-analysis. South Med J. 2008 Nov;101(11):1126-31.
| CrossRef | PubMed |
Hart PA, Bechtold ML, Marshall JB, Choudhary A, Puli SR, Roy PK. Prophylactic antibiotics in necrotizing pancreatitis: a meta-analysis. South Med J. 2008 Nov;101(11):1126-31.
| CrossRef | PubMed | Jafri NS, Mahid SS, Idstein SR, Hornung CA, Galandiuk S. Antibiotic prophylaxis is not protective in severe acute pancreatitis: a systematic review and meta-analysis. Am J Surg. 2009 Jun;197(6):806-13. | CrossRef | PubMed |
Jafri NS, Mahid SS, Idstein SR, Hornung CA, Galandiuk S. Antibiotic prophylaxis is not protective in severe acute pancreatitis: a systematic review and meta-analysis. Am J Surg. 2009 Jun;197(6):806-13. | CrossRef | PubMed | Xu T, Cai Q. Prophylactic antibiotic treatment in acute necrotizing pancreatitis: results from a meta-analysis. Scand J Gastroenterol. 2008;43(10):1249-58. | CrossRef | PubMed |
Xu T, Cai Q. Prophylactic antibiotic treatment in acute necrotizing pancreatitis: results from a meta-analysis. Scand J Gastroenterol. 2008;43(10):1249-58. | CrossRef | PubMed | Golub R, Siddiqi F, Pohl D. Role of antibiotics in acute pancreatitis: A meta-analysis. J Gastrointest Surg. 1998 Nov-Dec;2(6):496-503. | CrossRef | PubMed |
Golub R, Siddiqi F, Pohl D. Role of antibiotics in acute pancreatitis: A meta-analysis. J Gastrointest Surg. 1998 Nov-Dec;2(6):496-503. | CrossRef | PubMed | Bai Y, Gao J, Zou DW, Li ZS. Antibiotics prophylaxis in acute necrotizing pancreatitis: an update.Am J Gastroenterol. 2010 Mar;105(3):705-7. | CrossRef | PubMed |
Bai Y, Gao J, Zou DW, Li ZS. Antibiotics prophylaxis in acute necrotizing pancreatitis: an update.Am J Gastroenterol. 2010 Mar;105(3):705-7. | CrossRef | PubMed | Yao L, Huang X, Li Y, Shi R, Zhang G. Prophylactic antibiotics reduce pancreatic necrosis in acute necrotizing pancreatitis: a meta-analysis of randomized trials. Dig Surg. 2010;27(6):442-9. | CrossRef | PubMed |
Yao L, Huang X, Li Y, Shi R, Zhang G. Prophylactic antibiotics reduce pancreatic necrosis in acute necrotizing pancreatitis: a meta-analysis of randomized trials. Dig Surg. 2010;27(6):442-9. | CrossRef | PubMed | Dambrauskas Z, Gulbinas A, Pundzius J, Barauskas G. Meta-analysis of prophylactic parenteral antibiotic use in acute necrotizing pancreatitis. Medicina (Kaunas). 2007;43(4):291-300. | PubMed | Link |
Dambrauskas Z, Gulbinas A, Pundzius J, Barauskas G. Meta-analysis of prophylactic parenteral antibiotic use in acute necrotizing pancreatitis. Medicina (Kaunas). 2007;43(4):291-300. | PubMed | Link | Jiang K, Huang W, Yang XN, Xia Q. Present and future of prophylactic antibiotics for severe acute pancreatitis. World J Gastroenterol. 2012 Jan 21;18(3):279-84. | CrossRef | PubMed |
Jiang K, Huang W, Yang XN, Xia Q. Present and future of prophylactic antibiotics for severe acute pancreatitis. World J Gastroenterol. 2012 Jan 21;18(3):279-84. | CrossRef | PubMed | Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011 Mar;46(3):261-70. | CrossRef | PubMed |
Wittau M, Mayer B, Scheele J, Henne-Bruns D, Dellinger EP, Isenmann R. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011 Mar;46(3):261-70. | CrossRef | PubMed | Barreda L, Targarona J, Milian W, Portugal J, Sequeiros J, Pando E, Calisto JL. Is the prophylactic antibiotic therapy with Imipenem effective for patients with pancreatic necrosis?. Acta Gastroenterol Latinoam. 2009 Mar;39(1):24-9. | PubMed |
Barreda L, Targarona J, Milian W, Portugal J, Sequeiros J, Pando E, Calisto JL. Is the prophylactic antibiotic therapy with Imipenem effective for patients with pancreatic necrosis?. Acta Gastroenterol Latinoam. 2009 Mar;39(1):24-9. | PubMed | Craig RM, Dordal E, Myles L. Letter: The use of ampicillin in acute pancreatitis. Annals of internal medicine. Ann Intern Med. 1975 Dec;83(6):831-2. | PubMed |
Craig RM, Dordal E, Myles L. Letter: The use of ampicillin in acute pancreatitis. Annals of internal medicine. Ann Intern Med. 1975 Dec;83(6):831-2. | PubMed | Delcenserie R, Yzet T, Ducroix JP. Prophylactic antibiotics in treatment of severe acute alcoholic pancreatitis. Pancreas. 1996;13(2):198-201.
| PubMed |
Delcenserie R, Yzet T, Ducroix JP. Prophylactic antibiotics in treatment of severe acute alcoholic pancreatitis. Pancreas. 1996;13(2):198-201.
| PubMed | Dellinger EP, Tellado JM, Soto NE, Ashley SW, Barie PS, Dugernier T, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Annals of surgery. 2007;245(5):674-83. | PubMed |
Dellinger EP, Tellado JM, Soto NE, Ashley SW, Barie PS, Dugernier T, et al. Early antibiotic treatment for severe acute necrotizing pancreatitis: a randomized, double-blind, placebo-controlled study. Annals of surgery. 2007;245(5):674-83. | PubMed | Finch WT, Sawyers JL, Schenker S. A prospective study to determine the efficacy of antibiotics in acute pancreatitis. Annals of surgery. 1976 183(6):667-71. | PubMed |
Finch WT, Sawyers JL, Schenker S. A prospective study to determine the efficacy of antibiotics in acute pancreatitis. Annals of surgery. 1976 183(6):667-71. | PubMed | García-Barrasa A, Borobia FG, Pallares R, Jorba R, Poves I, Busquets J, et al. A double-blind, placebo-controlled trial of ciprofloxacin prophylaxis in patients with acute necrotizing pancreatitis. J Gastrointest Surg. 2009 Apr;13(4):768-74. | CrossRef | PubMed |
García-Barrasa A, Borobia FG, Pallares R, Jorba R, Poves I, Busquets J, et al. A double-blind, placebo-controlled trial of ciprofloxacin prophylaxis in patients with acute necrotizing pancreatitis. J Gastrointest Surg. 2009 Apr;13(4):768-74. | CrossRef | PubMed | Howes R, Zuidema GD, Cameron JL. Evaluation of prophylactic antibiotics in acute pancreatitis. The Journal of surgical research. 1975;18(2):197-200. | CrossRef | PubMed |
Howes R, Zuidema GD, Cameron JL. Evaluation of prophylactic antibiotics in acute pancreatitis. The Journal of surgical research. 1975;18(2):197-200. | CrossRef | PubMed | Isenmann R, Rünzi M, Kron M, Kahl S, Kraus D, Jung N, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology. 2004;126(4):997-1004. | CrossRef | PubMed |
Isenmann R, Rünzi M, Kron M, Kahl S, Kraus D, Jung N, et al. Prophylactic antibiotic treatment in patients with predicted severe acute pancreatitis: a placebo-controlled, double-blind trial. Gastroenterology. 2004;126(4):997-1004. | CrossRef | PubMed | Luiten EJ, Hop WC, Lange JF, Bruining HA. Controlled clinical trial of selective decontamination for the treatment of severe acute pancreatitis. Annals of surgery. 1995;222(1):57-65. | PubMed |
Luiten EJ, Hop WC, Lange JF, Bruining HA. Controlled clinical trial of selective decontamination for the treatment of severe acute pancreatitis. Annals of surgery. 1995;222(1):57-65. | PubMed | Nordback I, Sand J, Saaristo R, Paajanen H. Early treatment with antibiotics reduces the need for surgery in acute necrotizing pancreatitis--a single-center randomized study. J Gastrointest Surg. 2001 Mar-Apr;5(2):113-8; discussion 118-20. | PubMed |
Nordback I, Sand J, Saaristo R, Paajanen H. Early treatment with antibiotics reduces the need for surgery in acute necrotizing pancreatitis--a single-center randomized study. J Gastrointest Surg. 2001 Mar-Apr;5(2):113-8; discussion 118-20. | PubMed | Pederzoli P, Bassi C, Vesentini S, Campedelli A. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surgery, gynecology & obstetrics. 1993;176(5):480-3. | PubMed |
Pederzoli P, Bassi C, Vesentini S, Campedelli A. A randomized multicenter clinical trial of antibiotic prophylaxis of septic complications in acute necrotizing pancreatitis with imipenem. Surgery, gynecology & obstetrics. 1993;176(5):480-3. | PubMed | Røkke O, Harbitz TB, Liljedal J, Pettersen T, Fetvedt T, Heen L, et al. Early treatment of severe pancreatitis with imipenem: a prospective randomized clinical trial. Scand J Gastroenterol. 2007 Jun;42(6):771-6. | CrossRef | PubMed |
Røkke O, Harbitz TB, Liljedal J, Pettersen T, Fetvedt T, Heen L, et al. Early treatment of severe pancreatitis with imipenem: a prospective randomized clinical trial. Scand J Gastroenterol. 2007 Jun;42(6):771-6. | CrossRef | PubMed | Sainio V, Kemppainen E, Puolakkainen P, Taavitsainen M, Kivisaari L, Valtonen V, et al. Early antibiotic treatment in acute necrotising pancreatitis. Lancet. 1995;346(8976):663-7. | PubMed |
Sainio V, Kemppainen E, Puolakkainen P, Taavitsainen M, Kivisaari L, Valtonen V, et al. Early antibiotic treatment in acute necrotising pancreatitis. Lancet. 1995;346(8976):663-7. | PubMed | Schwarz M, Isenmann R, Meyer H, Beger HG. Antibiotic use in necrotizing pancreatitis. Results of a controlled study. Dtsch Med Wochenschr. 1997 Mar 21;122(12):356-61. | CrossRef | PubMed |
Schwarz M, Isenmann R, Meyer H, Beger HG. Antibiotic use in necrotizing pancreatitis. Results of a controlled study. Dtsch Med Wochenschr. 1997 Mar 21;122(12):356-61. | CrossRef | PubMed | Spicak J, Hejtmankova S, Hubaczova M, Antos F, Bartova J, Cech P, et al. Antibiotic prophylaxis of infectious complications of acute pancreatitis-the results of a randomised study. Ceská a Slovenská Gastroenterologie a Hepatologie. 2003;57(6):222–7.
Spicak J, Hejtmankova S, Hubaczova M, Antos F, Bartova J, Cech P, et al. Antibiotic prophylaxis of infectious complications of acute pancreatitis-the results of a randomised study. Ceská a Slovenská Gastroenterologie a Hepatologie. 2003;57(6):222–7.  Spicak J, Hubaczova M, Antos F, Bartova J, Cech P, Kasalicky M. Antibiotics in the treatment of acute pancreatitis - findings from a randomized multi-centre prospective study. Ceská a Slovenská Gastroenterologie a Hepatologie. 2002;56(5):183–9.
Spicak J, Hubaczova M, Antos F, Bartova J, Cech P, Kasalicky M. Antibiotics in the treatment of acute pancreatitis - findings from a randomized multi-centre prospective study. Ceská a Slovenská Gastroenterologie a Hepatologie. 2002;56(5):183–9.  Spicak J, Hejtmankova S, Cech P, Hoskovec D, Kostka R, Leffler J, et al. Antibiotic prophylaxis in large pancreatic necrosis: multicenter randomized trial with ciprofloxacin and metronidazole or meropenem. Gastroenterology. 2004;126(A229):S1497.
Spicak J, Hejtmankova S, Cech P, Hoskovec D, Kostka R, Leffler J, et al. Antibiotic prophylaxis in large pancreatic necrosis: multicenter randomized trial with ciprofloxacin and metronidazole or meropenem. Gastroenterology. 2004;126(A229):S1497.  Spicak JHS, Cech P, Hoskovec D, Kostka R, Leffler J. Antibiotic prophylaxis in severe acute pancreatitis: randomised multicenter prospective trial with meropenem. Pancreatology. 2003;3:220.
Spicak JHS, Cech P, Hoskovec D, Kostka R, Leffler J. Antibiotic prophylaxis in severe acute pancreatitis: randomised multicenter prospective trial with meropenem. Pancreatology. 2003;3:220.  Xue P, Deng LH, Zhang ZD, Yang XN, Wan MH, Song B, et al. Effect of antibiotic prophylaxis on acute necrotizing pancreatitis: results of a randomized controlled trial. J Gastroenterol Hepatol. 2009 May;24(5):736-42. | CrossRef |
Xue P, Deng LH, Zhang ZD, Yang XN, Wan MH, Song B, et al. Effect of antibiotic prophylaxis on acute necrotizing pancreatitis: results of a randomized controlled trial. J Gastroenterol Hepatol. 2009 May;24(5):736-42. | CrossRef | Yang XN, Deng LH, Xue P, Zhao L, Jin T, Wan MH, et al. [Non-preventive use of antibiotics in patients with severe acute pancreatitis treated with integrated traditional Chinese and Western medicine therapy: a randomized controlled trial. Zhong Xi Yi Jie He Xue Bao. 2009 Apr;7(4):330-3. | CrossRef | PubMed |
Yang XN, Deng LH, Xue P, Zhao L, Jin T, Wan MH, et al. [Non-preventive use of antibiotics in patients with severe acute pancreatitis treated with integrated traditional Chinese and Western medicine therapy: a randomized controlled trial. Zhong Xi Yi Jie He Xue Bao. 2009 Apr;7(4):330-3. | CrossRef | PubMed | Ho HS, Frey CF. The role of antibiotic prophylaxis in severe acute pancreatitis. Arch Surg. 1997 May;132(5):487-92; discussion 492-3. | CrossRef | PubMed |
Ho HS, Frey CF. The role of antibiotic prophylaxis in severe acute pancreatitis. Arch Surg. 1997 May;132(5):487-92; discussion 492-3. | CrossRef | PubMed | Ignatavicius P, Vitkauskiene A, Pundzius J, Dambrauskas Z, Barauskas G. Effects of prophylactic antibiotics in acute pancreatitis. HPB (Oxford). 2012 Jun;14(6):396-402. | CrossRef | PubMed |
Ignatavicius P, Vitkauskiene A, Pundzius J, Dambrauskas Z, Barauskas G. Effects of prophylactic antibiotics in acute pancreatitis. HPB (Oxford). 2012 Jun;14(6):396-402. | CrossRef | PubMed | Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416. | CrossRef | PubMed |
Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013 Sep;108(9):1400-15; 1416. | CrossRef | PubMed | AGA Institute medical position statement on acute pancreatitis. Gastroenterology. 2007 May;132(5):2019-21. | CrossRef | PubMed |
AGA Institute medical position statement on acute pancreatitis. Gastroenterology. 2007 May;132(5):2019-21. | CrossRef | PubMed |