 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: type 2 diabetes mellitus, quality of life, self-efficacy, microvascular complications
Quality of life and self-efficacy assessments are increasingly applied in research with type 2 diabetes mellitus patients due to the impact of the disease on their lives. This study aimed to describe the quality of life and self-efficacy in type 2 diabetes mellitus patients and describe the association of quality of life and self-efficacy with demographic, metabolic, and clinical variables. This is a secondary data analysis from a cross-sectional study: “Metabolic control in patients with type 2 diabetes mellitus in a public hospital in Peru: a cross-sectional study in a low-middle income country”. Data were obtained by standardized interviews and evaluation of medical records. The evaluation tools used were the Diabetes 39 questionnaire (D-39) to measure the quality of life and the General Self-Efficacy scale (GSE) for self-efficacy. The median scores of the D-39 and GSE were 34.6 and 34, respectively. The D-39 dimension with the highest score was “anxiety and concern.” Better quality of life was associated with being older than 65 years old, not having complications, and the absence of depression. No significant association was found between self-efficacy and the quality of life score. Results suggest patients with type 2 diabetes mellitus have a poor quality of life. Patient-centered strategies for type 2 diabetes mellitus care must consider these psychosocial factors to improve disease control and quality of life.
Main messages
|
Type 2 diabetes mellitus is a chronic disease with a growing worldwide prevalence that greatly impacts patients’ quality of life[1]. According to the International Diabetes Federation (IDF), in 2019, 463 million adults were living with diabetes; it has been estimated that by 2045 this number will rise to 700 million people, with type 2 diabetes mellitus as its majority, with 90% of cases[2] and low- and middle-income countries the most affected[2],[3]. In Peru, the current prevalence is 7.1%[4], which represents the people at risk of type 2 diabetes-related complications, disabilities[2], and psychosocial impairments[1],[5] that will decrease their quality of life.
Quality of life studies in chronic diseases has gained interest in the diabetes epidemic due to the importance of health interventions in improving physical wellness and a more holistic approach in patient care of improving overall well-being[1],[2]. Moreover, it is used as a patient-important outcome in clinical trials[6]. The World Health Organization (WHO) defines quality of life as an individual’s perception of their position in life in the context of the culture and value systems they live, having to do with their goals, expectations, standards, and concerns[7]. For example, studies have found clinical and metabolic factors, such as the presence of two or more complications, inadequate glycemic control, and more invasive treatment; harm quality of life[8], affecting medical, social, economic, and psychological factors in each patient[9]. However, psychological factors, such as depression, could be more important in predicting quality of life since these have proved to be stronger predictors of hospitalization and mortality[5].
Patients with type 2 diabetes mellitus may develop distress due to a sense of loss of control in their lives, overwhelming self-care stress, feelings of loneliness, and the fear of disease complications and death[10],[11]. Self-management activities, such as glycemic control or adherence to a new diet, may be perceived as mentally and physically exhausting, highly influenced by internal (mood, energy, etc.) and external stressors (economics, family issues, etc.)[11], which are subsequently associated with glucose control impairment[12]. Diabetes management requires time and emotional work from patients and their families. It has been estimated that practicing the self-care activities recommended by the American Diabetes Association (ADA), e.g., checking feet, monitoring glucose, and exercising, requires more than two hours per day[13].
On the other hand, a positive attitude and resilience are associated with better clinical outcomes such as lower overall mortality and lower one-year glycosylated hemoglobin (HbA1c) levels in patients with diabetes[14]. Therefore, quality of life assessments should be included and considered essential in these patients’ medical management. The main goal in medical practice is to minimize the deterioration of quality of life[15].
Another crucial factor that affects every human endeavor is self-efficacy. It has a strong predictive association with morbidity and mortality in type 2 diabetes mellitus[16]. Self-efficacy is a psychological concept defined as the self-perception of one’s ability to perform and achieve goals[17]. High self-efficacy is associated with less reported pain, better self-care performance, more frequent healthy behaviors, and higher quality of life in patients with[18],[19] or without type 2 diabetes mellitus[20].
There are limited studies on the effect of psychosocial factors like quality of life and self-efficacy on type 2 diabetes mellitus patients in low- and middle-income countries, where external stressors such as poverty, healthcare access limitations, and family issues are frequent. This study aims to measure the quality of life and self-efficacy in type 2 diabetes mellitus patients at a public hospital in Lima, Peru, and examine the association between quality of life and self-efficacy with demographic, metabolic, clinical variables, and laboratory parameters.
Study design and participants
We conducted a secondary analysis of a cross-sectional study: “Metabolic control in patients with type 2 diabetes mellitus in a public hospital in Peru: a cross-sectional study in a low-middle income country”[21]. The study recruited participants with a type 2 diabetes mellitus diagnosis between March and July of 2012 in the Endocrinology Unit of the Cayetano Heredia Hospital in Lima, Peru.
Patients were recruited by convenience sampling. Inclusion criteria were as follows: diagnosis of type 2 diabetes mellitus for at least 12 months, being older than 18 years old, and more than one visit to the Endocrinology Unit in the previous year. Patients were excluded if they had secondary or gestational diabetes, chronic non-cardio-metabolic diseases (systemic lupus erythematosus, rheumatoid arthritis, chronic obstructive pulmonary disease), major complications of type 2 diabetes mellitus (stroke, coronary heart disease, hyperglycemic/hypoglycemic crisis) in the previous year, hospitalization in the last six months, or a diagnosed mental illness or incapability.
Procedures
Information was collected by a standardized interview and evaluation of medical records. Data for demographic variables, clinical factors related to treatment, and chronic diabetic complications defined as microvascular (retinopathy, nephropathy, and neuropathy) and macrovascular (coronary heart disease, stroke, and peripheral artery disease) were also obtained.
The evaluation forms and standardized tools used were: Diabetes 39 questionnaire (D-39)[22] and the General Self-Efficacy scale of Schwarzer and Baessler[23].
Laboratory measurements for fasting glucose, HbA1c, and lipid profile were taken in the morning after, at minimum, an 8-hour fast. Evaluation forms and standardized interviews were assessed during the endocrinology visit.
Outcomes and variables definition
The D-39 item questionnaire assesses five dimensions: energy and motility, diabetes control, anxiety and concern, social and peer burden, and sexual functioning. The D-39 also contains two final items that rate the patients’ perception of their overall quality of life and diabetes severity. The answers reflect the degree of affectation that diabetes had on the previous month for each of the five items named previously. The participant expressed answers on a visual analogic scale from 1 to 7, where 1 means “not affected at all” and 7 means “extremely affected.” In the case of overall quality of life and diabetes severity, 1 means “lowest quality of life,” and 7 means “highest quality of life,” or 1 means “less severe” and 7 “extremely severe,” respectively. Once finished, each section’s partial scores are transformed into a scale from 0 to 100, and the median determines the cutoff points. The patient is considered to have a better quality of life if the individual total score is lower than the median and poor quality of life if the score is equal or greater than the median[22].
Schwarzer and Baessler’s GSE evaluation consists of ten items with four possible answers: “not true at all,” “hardly true,” “moderately true,” and “exactly true.” The “not true at all” alternative is given a value of 1, whereas “exactly true” received a value of 4. The participant gets a total score on a range from 10 to 40. A higher score represents a higher self-efficacy[23]. There is no cutoff point to define if a subject is considered self-efficacious, but the subject’s score is compared to the mean scores of those in other groups.
“Good metabolic control” was defined according to ADA recommendations: good glycemic control (HbA1c < 7%), controlled blood pressure (BP < 140/90mmHg), and controlled LDL-cholesterol (LDL < 100 mg/dL)[24].
A detailed explanation of variables and scales can be seen in Table 1.
Table 1. Variables and score definition
Statistical analysis
Statistical analysis was performed using Stata 13.0. Chi-square test was used for estimating the association between demographic (age, gender, marital status), metabolic (BMI, HbA1c, LDL, BP), and clinical (disease duration, treatment, complications) variables compared to the quality of life (D-39). The non-parametric Mann-Whitney test was used to examine the association between demographic and clinical variables with GSE score. A Spearman correlation test was performed to examine the association between each quality of life dimension and the GSE score.
Multivariable models were generated using Poisson regression reporting prevalence ratios and 95% confidence interval. This model evaluated the independent association among quality of life and demographic, metabolic, and clinical variables. Crude and adjusted analyses were performed.
Ethics
The Institutional Review Boards of the Universidad Peruana Cayetano Heredia and Hospital Cayetano Heredia both approved the study protocol. Written consent was obtained from all participants.
The sample was composed of 42 men (34.2%) and 81 women (65.9%). The mean age was 61.8 ± 11.1 years old. Further characteristics are described in Supplementary material 1.
Quality of life dimensions and self-efficacy
The overall median for the total score of D-39 was 34.6 (IQR 19.7 to 51.3). The D-39 dimension with the highest score, almost doubling the total score median, was “anxiety and concern” with a median of 66.7 (IQR: 33.3 to 83.3); the dimension with the lowest score was “sexual functioning” with a median of 0 (IQR: 0.0 to 50.0). On the general self-efficacy score, the sample median was 34. In table 2, we reported in detail the scores of every item for D-39 and GSE.
Table 2. Quality of life dimensions and self-efficacy
Quality of life and self-efficacy associated with co-variables
In the bivariate analysis, we found a significant association between better quality of life and being older than 65 years old (p = 0.01), not having microvascular diabetes complications (p = 0.02), and not having depression (p < 0.001). There were no significant associations between self-efficacy and demographic, clinical, or metabolic variables; all p-values > 0.05 (Table 3).
Table 3. Characteristics of the study population according to quality of life and self-efficacy
Multivariate analysis of quality of life
In the crude analysis, the proportion of poor quality of life was 46% higher in people with either microvascular or macrovascular complications (PR = 1.46, 95% CI 1.03 to 2.07, p = 0.03). In the adjusted multivariate analysis, poor quality of life was two times higher compared to those living without depression (PR = 2.34, 95% CI 1.62 to 3.31); 45% higher in people living more than ten years with diabetes (PR = 1.45, 95% CI 1.01 to 2.13); two times higher in people treated only with insulin compared to no pharmacological treatment (PR = 2.02, 95% CI = 1.01 to 4.07); and 34% lower in people older than 65 years (PR = 0.66, 95% CI 0.43 to 1.00) (Table 4).
Table 4. Factors associated with quality of life
Association between quality of life dimensions and self-efficacy
We did not find an association between the general self-efficacy score and the overall quality of life score (p = 0.690), but there were significant associations between some quality of life dimensions. For example, there was a negative correlation between self-efficacy and “anxiety and concern” (rho = -0.20, p < 0.05), as well as with diabetes severity (rho = -0.22, p < 0.05), and a positive correlation with the overall perception of the quality of life (rho = +0.25, p < 0.01) (Table 5). Graphics are shown in Supplementary material 2.
Table 5. Quality of life and self-efficacy correlation
Patients with type 2 diabetes mellitus presented low quality scores (median of 34.62 for D-39), “anxiety and concern” and “energy and motility” being the most frequently reported dimensions. Even though there are different patterns within Latin American publications, “anxiety and concern” is one of the most commonly reported[22],[25],[26]. Also, we found that quality of life was associated with depression, which has been reported as an associated factor to poor metabolic outcomes[27],[28],[29]. These findings suggest that diabetes hurts the psychological domain of quality of life, which must be addressed to avoid mental health disorders like depression associated with poor metabolic outcomes[30].
We also found higher quality of life scores among patients older than 65, suggesting that greater distress is experienced by young adults with type 2 diabetes mellitus than among the elderl[31],[32],[33].
Our model found that the association between diabetic complications and quality of life was no longer significant when controlling by years of disease and insulin therapy variables. This confounder effect is explained by previous studies that report the association between years of diabetes and insulin therapy with the appearance of complications[34] and worse quality of life scores[35],[36].
We did not find significant associations between quality of life and marital status, metabolic control, years of disease, or any treatment. Some studies found that quality of life was positively associated with being in a couple. Furthermore, they emphasized that family members or other social support should be addressed as a predictor for quality of life[36]. The associations between metabolic control or comorbidities with quality of life have been inconsistent in the literature, but it is known that a poor metabolic control leads to complications that may affect the quality of life. Nonetheless, there is no consensus over its direct effect[1],[26],[35],[37].
We found a median for general self-efficacy of 31.7, which means that type 2 diabetes mellitus patients are less likely to feel empowered to achieve goals related to their disease. Similar values have been reported in an ethnically diverse study with patients with diabetes performed in the United States[38]. There was no association found between self-efficacy and other variables, unlike other scales designed to measure self-efficacy in a patient with diabetes such as IMDSES (Insulin Management Diabetes Self-Efficacy Scale), DSE (Diabetes Self-Efficacy), and DDS2 (Diabetic Distress Score) that reported associations between self-efficacy and demographic and clinical variables. Diabetic-specific self-efficacy scales may be more sensitive about finding differences with other variables among patients with diabetes[39],[40],[41],[42].
The general self-efficacy score was not significantly associated with the quality of life score. However, we have seen that an increase in the self-efficacy points was associated with a parallel increase in the points of “quality of life perception” and fewer points over “diabetes severity” and “anxiety and concern.” The findings are similar to those reported by Kim G, et al., where self-efficacy is correlated with less psychological distress, which is important for adjusting healthier lifestyles necessary for diabetes control[40].
One of the study limitations, as a cross-sectional study, is the causality in the association between quality of life and self-efficacy with other variables that could not be determined. Also, our sample was limited to the Endocrinology clinic of a public hospital, which lowers the findings’ external validity. Potentially important variables were not included, such as language, comorbidities, family support, number of family members living with the patient, education, knowledge of diabetes, or number of hospitalizations. These variables have been reported to be relevant to the quality of life and self-efficacy and may act as a confounder in some studies.
Our findings revealed the complexity of managing various social and psychological stressors that can affect the quality of metabolic control and quality of life in the medium- or long-term. Clinicians tend to focus on symptoms, signs, medications, and evaluation of laboratory parameters to determine the next steps for managing people with type 2 diabetes mellitus. Few clinicians apply for patient-centered medicine, an approach defined as “taking into account patients’ preferences, objectives, and values, as well as the available economic resources”[43]. In this context, an approach like “Minimally disruptive medicine,” a patient-centered approach that seeks reduction of a patient’s life disruption due to medical treatment by taking into account the patient’s health and general life goals, could influence in reducing “anxiety and concern” that harm a patient’s quality of life[44]. Our goal with this study is to fill the gap in understanding diabetes’s impact on patients’ quality of life. This study, performed in a public hospital that receives patients of diverse socioeconomic status, shows the reality our patients are facing with the burden of the disease and what should be considered for diabetes care.
The quality of life in patients with type 2 diabetes mellitus is poor, “anxiety and concern” being the most affected dimension. Poor quality of life was associated with being younger than 65 and with having depression. There was no association found between self-efficacy and quality of life. Our findings emphasized the impact that diabetes has on the patient’s psychology and life. A patient-centered approach is needed to improve quality of life, which is as important as glycemic control and complication prevention from the patient’s perspective.
Notes
Authorship contributions
All authors contributed equally to this study.
Competing interests
The authors declare there is no competing interests to declare regarding this work.
Funding
The main study was supported by a research fund from the Faculty of Medicine Alberto Hurtado, Universidad Peruana Cayetano Heredia (No. 02231001). The funders had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Acknowledgments
The authors thank Dr. Ray Ticse, Dr. Miguel Pinto, and Dr. Valerie Paz Soldan for their valuable comments and review on this article and Mariela Florez and Carmela Costta for their help in patient recruitment.
Data availability statement
The raw data of the main study is available in 10.7717/peerj.2577/supp-2.

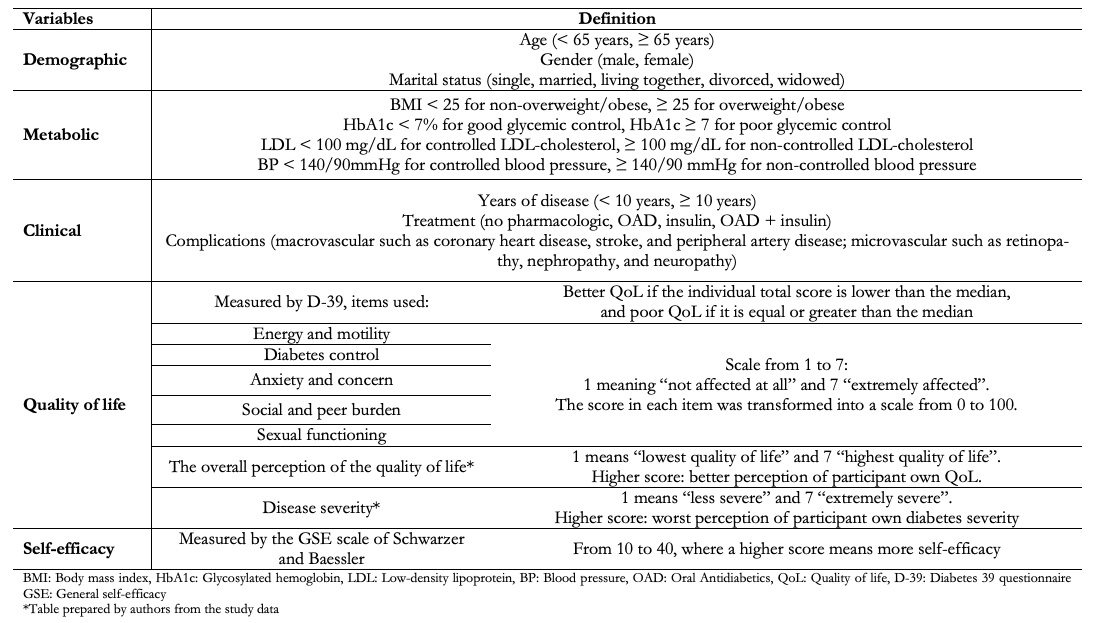 Table 1. Variables and score definition
Table 1. Variables and score definition

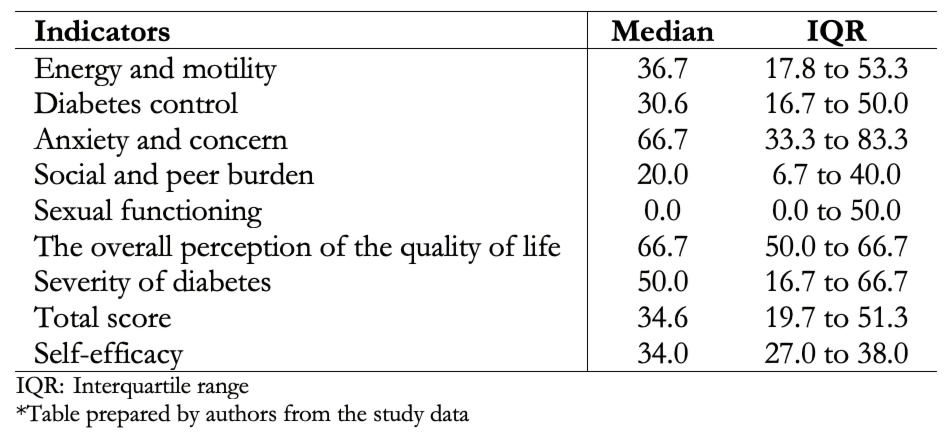 Table 2. Quality of life dimensions and self-efficacy
Table 2. Quality of life dimensions and self-efficacy

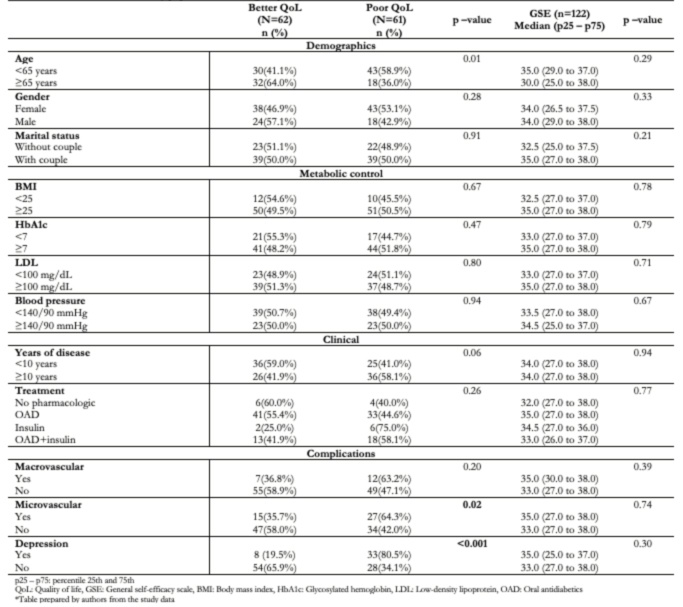 Table 3. Characteristics of the study population according to quality of life and self-efficacy
Table 3. Characteristics of the study population according to quality of life and self-efficacy

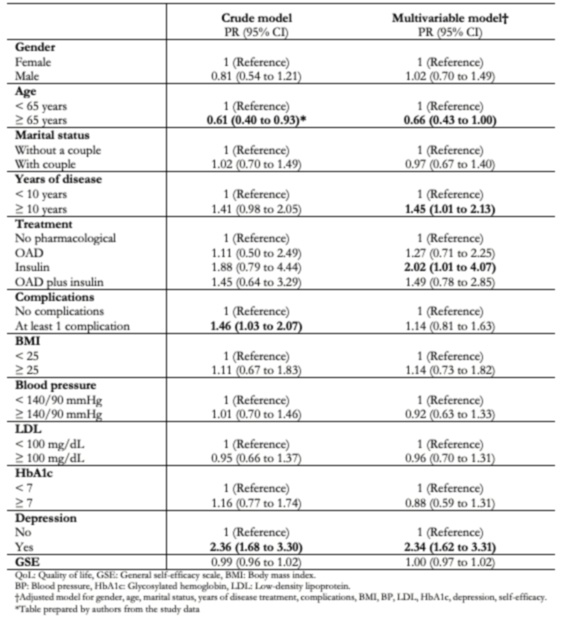 Table 4. Factors associated with quality of life
Table 4. Factors associated with quality of life

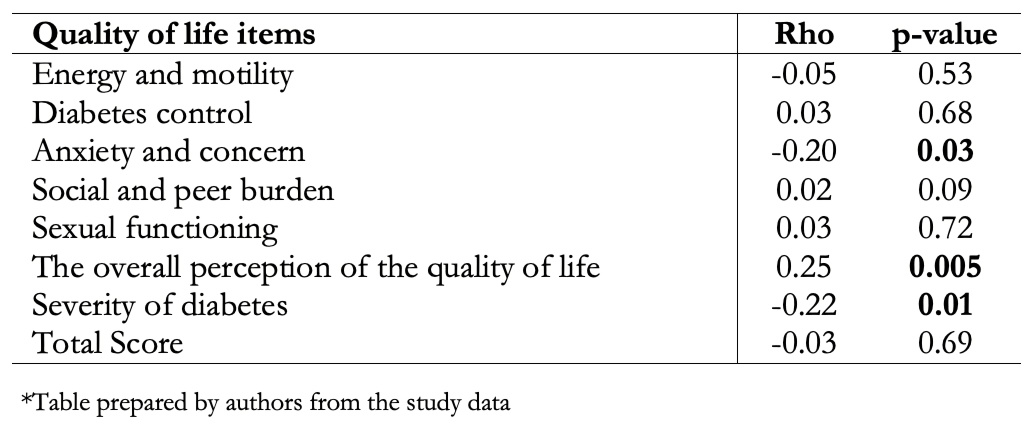 Table 5. Quality of life and self-efficacy correlation
Table 5. Quality of life and self-efficacy correlation
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Quality of life and self-efficacy assessments are increasingly applied in research with type 2 diabetes mellitus patients due to the impact of the disease on their lives. This study aimed to describe the quality of life and self-efficacy in type 2 diabetes mellitus patients and describe the association of quality of life and self-efficacy with demographic, metabolic, and clinical variables. This is a secondary data analysis from a cross-sectional study: “Metabolic control in patients with type 2 diabetes mellitus in a public hospital in Peru: a cross-sectional study in a low-middle income country”. Data were obtained by standardized interviews and evaluation of medical records. The evaluation tools used were the Diabetes 39 questionnaire (D-39) to measure the quality of life and the General Self-Efficacy scale (GSE) for self-efficacy. The median scores of the D-39 and GSE were 34.6 and 34, respectively. The D-39 dimension with the highest score was “anxiety and concern.” Better quality of life was associated with being older than 65 years old, not having complications, and the absence of depression. No significant association was found between self-efficacy and the quality of life score. Results suggest patients with type 2 diabetes mellitus have a poor quality of life. Patient-centered strategies for type 2 diabetes mellitus care must consider these psychosocial factors to improve disease control and quality of life.
 Autores:
Irma Elizabeth Huayanay-Espinoza[1], Felix Guerra-Castañon[1], Michael Reyes-Diaz[1], María Lazo-Porras[1,2], Celso de la Cruz-Luque[1], Diego Adrianzen Herrera[1,3], Germán Málaga[1,2,4,5]
Autores:
Irma Elizabeth Huayanay-Espinoza[1], Felix Guerra-Castañon[1], Michael Reyes-Diaz[1], María Lazo-Porras[1,2], Celso de la Cruz-Luque[1], Diego Adrianzen Herrera[1,3], Germán Málaga[1,2,4,5]

Citación: Huayanay-Espinoza IE, Guerra-Castañon F, Reyes-Diaz M, Lazo-Porras M, de la Cruz-Luque C, Herrera DA, et al. Quality of life and self-efficacy in patients with type 2 diabetes mellitus in a Peruvian public hospital. Medwave 2021;21(02):e8132 doi: 10.5867/medwave.2021.02.8132
Fecha de envío: 30/3/2020
Fecha de aceptación: 12/12/2020
Fecha de publicación: 22/3/2021
Origen: No solicitado.
Tipo de revisión: Con revisión externa por cuatro revisores, a doble ciego.

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999 May-Jun;15(3):205-18. | CrossRef | PubMed |
Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999 May-Jun;15(3):205-18. | CrossRef | PubMed | Federation, I. Idf diabetes atlas. International Diabetes Federation: Brussels, Belgium 2018.
Federation, I. Idf diabetes atlas. International Diabetes Federation: Brussels, Belgium 2018.  Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011 Jul 2;378(9785):31-40. | CrossRef | PubMed |
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2·7 million participants. Lancet. 2011 Jul 2;378(9785):31-40. | CrossRef | PubMed | Bernabé-Ortiz A, Carrillo-Larco RM, Gilman RH, Miele CH, Checkley W, Wells JC, et al. Geographical variation in the progression of type 2 diabetes in Peru: The CRONICAS Cohort Study. Diabetes Res Clin Pract. 2016 Nov;121:135-145. | CrossRef | PubMed |
Bernabé-Ortiz A, Carrillo-Larco RM, Gilman RH, Miele CH, Checkley W, Wells JC, et al. Geographical variation in the progression of type 2 diabetes in Peru: The CRONICAS Cohort Study. Diabetes Res Clin Pract. 2016 Nov;121:135-145. | CrossRef | PubMed | Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults. A 3-year prospective study. Diabetes Care. 1998 Feb;21(2):231-5. | CrossRef | PubMed |
Rosenthal MJ, Fajardo M, Gilmore S, Morley JE, Naliboff BD. Hospitalization and mortality of diabetes in older adults. A 3-year prospective study. Diabetes Care. 1998 Feb;21(2):231-5. | CrossRef | PubMed | Gandhi GY, Murad MH, Fujiyoshi A, Mullan RJ, Flynn DN, Elamin MB, et al. Patient-important outcomes in registered diabetes trials. JAMA. 2008 Jun 4;299(21):2543-9. | CrossRef | PubMed |
Gandhi GY, Murad MH, Fujiyoshi A, Mullan RJ, Flynn DN, Elamin MB, et al. Patient-important outcomes in registered diabetes trials. JAMA. 2008 Jun 4;299(21):2543-9. | CrossRef | PubMed | The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998 Jun;46(12):1569-85. | CrossRef | PubMed |
The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998 Jun;46(12):1569-85. | CrossRef | PubMed | Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L. Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care. 1997 Apr;20(4):562-7. | CrossRef | PubMed |
Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L. Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care. 1997 Apr;20(4):562-7. | CrossRef | PubMed | Levterova B, Levterov G, Dragova E. Quality of Life in Patients with Type 2 Diabetes Mellitus in Bulgaria: A Cross - Sectional Study, European Journal of Preventive Medicine. 2016;4(1):7-12. | CrossRef |
Levterova B, Levterov G, Dragova E. Quality of Life in Patients with Type 2 Diabetes Mellitus in Bulgaria: A Cross - Sectional Study, European Journal of Preventive Medicine. 2016;4(1):7-12. | CrossRef | Hughes LC, Keith SE, Byars A, Wiginton KL. Cognitive mapping in persons newly diagnosed with type 2 diabetes. Diabetes Educ. 2012 Nov-Dec;38(6):845-54. | CrossRef | PubMed |
Hughes LC, Keith SE, Byars A, Wiginton KL. Cognitive mapping in persons newly diagnosed with type 2 diabetes. Diabetes Educ. 2012 Nov-Dec;38(6):845-54. | CrossRef | PubMed | Svedbo Engström M, Leksell J, Johansson UB, Gudbjörnsdottir S. What is important for you? A qualitative interview study of living with diabetes and experiences of diabetes care to establish a basis for a tailored Patient- Reported Outcome Measure for the Swedish National Diabetes Register. BMJ Open. 2016 Mar 24;6(3):e010249. | CrossRef | PubMed |
Svedbo Engström M, Leksell J, Johansson UB, Gudbjörnsdottir S. What is important for you? A qualitative interview study of living with diabetes and experiences of diabetes care to establish a basis for a tailored Patient- Reported Outcome Measure for the Swedish National Diabetes Register. BMJ Open. 2016 Mar 24;6(3):e010249. | CrossRef | PubMed | Liang H, Cheng J, Shen X, Chen P, Tong G, Chai J, et al. Relationships between stressful life events and impaired fasting glucose among left-behind farmers in rural China. J Psychosom Res. 2015 Feb;78(2):178-83. | CrossRef | PubMed |
Liang H, Cheng J, Shen X, Chen P, Tong G, Chai J, et al. Relationships between stressful life events and impaired fasting glucose among left-behind farmers in rural China. J Psychosom Res. 2015 Feb;78(2):178-83. | CrossRef | PubMed | Russell LB, Suh DC, Safford MA. Time requirements for diabetes self- management: too much for many? J Fam Pract. 2005 Jan;54(1):52-6. | PubMed |
Russell LB, Suh DC, Safford MA. Time requirements for diabetes self- management: too much for many? J Fam Pract. 2005 Jan;54(1):52-6. | PubMed | Robertson SM, Stanley MA, Cully JA, Naik AD. Positive emotional health and diabetes care: concepts, measurement, and clinical implications. Psychosomatics. 2012 Jan-Feb;53(1):1-12. | CrossRef | PubMed |
Robertson SM, Stanley MA, Cully JA, Naik AD. Positive emotional health and diabetes care: concepts, measurement, and clinical implications. Psychosomatics. 2012 Jan-Feb;53(1):1-12. | CrossRef | PubMed | Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. 2018 Sep 19;16(1):189. | CrossRef | PubMed |
Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. 2018 Sep 19;16(1):189. | CrossRef | PubMed | Aalto AM, Uutela A, Aro AR. Health related quality of life among insulin- dependent diabetics: disease-related and psychosocial correlates. Patient Educ Couns. 1997 Mar;30(3):215-25. | CrossRef | PubMed |
Aalto AM, Uutela A, Aro AR. Health related quality of life among insulin- dependent diabetics: disease-related and psychosocial correlates. Patient Educ Couns. 1997 Mar;30(3):215-25. | CrossRef | PubMed | Contreras F, Espinosa JC, Esguerra GA. Calidad de vida, autoeficacia, estrategias de afrontamiento y adhesión al tratamiento en pacientes con insuficiencia renal crónica sometidos a hemodiálisis. Psicología y salud. 2013;18(2): 165-79.
Contreras F, Espinosa JC, Esguerra GA. Calidad de vida, autoeficacia, estrategias de afrontamiento y adhesión al tratamiento en pacientes con insuficiencia renal crónica sometidos a hemodiálisis. Psicología y salud. 2013;18(2): 165-79.  Borhaninejad V, Shati M, Bhalla D, Iranpour A, Fadayevatan R. A Population- Based Survey to Determine Association of Perceived Social Support and Self- Efficacy With Self-Care Among Elderly With Diabetes Mellitus (Kerman City, Iran). Int J Aging Hum Dev. 2017 Dec;85(4):504-517. | CrossRef | PubMed |
Borhaninejad V, Shati M, Bhalla D, Iranpour A, Fadayevatan R. A Population- Based Survey to Determine Association of Perceived Social Support and Self- Efficacy With Self-Care Among Elderly With Diabetes Mellitus (Kerman City, Iran). Int J Aging Hum Dev. 2017 Dec;85(4):504-517. | CrossRef | PubMed | Hurley AC, Shea CA. Self-efficacy: strategy for enhancing diabetes self-care. Diabetes Educ. 1992 Mar-Apr;18(2):146-50. | CrossRef | PubMed |
Hurley AC, Shea CA. Self-efficacy: strategy for enhancing diabetes self-care. Diabetes Educ. 1992 Mar-Apr;18(2):146-50. | CrossRef | PubMed | Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol. 2005 Sep;139(5):439-57. | CrossRef | PubMed |
Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol. 2005 Sep;139(5):439-57. | CrossRef | PubMed | Huayanay-Espinoza IE, Guerra-Castañon F, Lazo-Porras M, Castaneda-Guarderas A, Thomas NJ, Garcia-Guarniz AL, et al. Metabolic control in patients with type 2 diabetes mellitus in a public hospital in Peru: a cross-sectional study in a low-middle income country. PeerJ. 2016 Oct 13;4:e2577. | CrossRef | PubMed |
Huayanay-Espinoza IE, Guerra-Castañon F, Lazo-Porras M, Castaneda-Guarderas A, Thomas NJ, Garcia-Guarniz AL, et al. Metabolic control in patients with type 2 diabetes mellitus in a public hospital in Peru: a cross-sectional study in a low-middle income country. PeerJ. 2016 Oct 13;4:e2577. | CrossRef | PubMed | López-Carmona JM, Rodríguez-Moctezuma R. Adaptación y validación del instrumento de calidad de vida Diabetes 39 en pacientes mexicanos con diabetes mellitus tipo 2 [Adaptation and validation of quality of life instrument Diabetes 39 for Mexican patients with type 2 diabetes mellitus]. Salud Publica Mex. 2006 May-Jun;48(3):200-11. | CrossRef | PubMed |
López-Carmona JM, Rodríguez-Moctezuma R. Adaptación y validación del instrumento de calidad de vida Diabetes 39 en pacientes mexicanos con diabetes mellitus tipo 2 [Adaptation and validation of quality of life instrument Diabetes 39 for Mexican patients with type 2 diabetes mellitus]. Salud Publica Mex. 2006 May-Jun;48(3):200-11. | CrossRef | PubMed | Baessler J, Schwarcer R. Evaluación de la autoeficacia: Adaptación española de la escala de Autoeficacia General. Ansiedad y Estrés.1996;2:1-8.
Baessler J, Schwarcer R. Evaluación de la autoeficacia: Adaptación española de la escala de Autoeficacia General. Ansiedad y Estrés.1996;2:1-8.  Summary of Revisions: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S4-S6. | CrossRef | PubMed |
Summary of Revisions: Standards of Medical Care in Diabetes-2018. Diabetes Care. 2018 Jan;41(Suppl 1):S4-S6. | CrossRef | PubMed | Ríos CJL, Sánchez SJJ, Barrios SP, et al. Calidad de vida en pacientes con diabetes mellitus tipo 2. Rev Med Inst Mex Seguro Soc. 2004;42(2):109-116.
Ríos CJL, Sánchez SJJ, Barrios SP, et al. Calidad de vida en pacientes con diabetes mellitus tipo 2. Rev Med Inst Mex Seguro Soc. 2004;42(2):109-116.  Machado-Alba JE, Medina-Morales DA, Echeverri-Cataño LF. Evaluation of the quality of life of patients with diabetes mellitus treated with conventional or analogue insulins. Diabetes Res Clin Pract. 2016 Jun;116:237-43. | CrossRef | PubMed |
Machado-Alba JE, Medina-Morales DA, Echeverri-Cataño LF. Evaluation of the quality of life of patients with diabetes mellitus treated with conventional or analogue insulins. Diabetes Res Clin Pract. 2016 Jun;116:237-43. | CrossRef | PubMed | Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007 Sep;30(9):2222-7. | CrossRef | PubMed |
Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007 Sep;30(9):2222-7. | CrossRef | PubMed | Stanković Z, Jašović-Gašić M, Zamaklar M. Psycho-social and clinical variables associated with depression in patients with type 2 diabetes. Psychiatr Danub. 2011 Mar;23(1):34-44. | PubMed |
Stanković Z, Jašović-Gašić M, Zamaklar M. Psycho-social and clinical variables associated with depression in patients with type 2 diabetes. Psychiatr Danub. 2011 Mar;23(1):34-44. | PubMed | Zuberi SI, Syed EU, Bhatti JA. Association of depression with treatment outcomes in Type 2 Diabetes Mellitus: a cross-sectional study from Karachi, Pakistan. BMC Psychiatry. 2011 Feb 15;11:27. | CrossRef | PubMed |
Zuberi SI, Syed EU, Bhatti JA. Association of depression with treatment outcomes in Type 2 Diabetes Mellitus: a cross-sectional study from Karachi, Pakistan. BMC Psychiatry. 2011 Feb 15;11:27. | CrossRef | PubMed | Egede LE, Ellis C. The effects of depression on metabolic control and quality of life in indigent patients with type 2 diabetes. Diabetes Technol Ther. 2010 Apr;12(4):257-62. | CrossRef | PubMed |
Egede LE, Ellis C. The effects of depression on metabolic control and quality of life in indigent patients with type 2 diabetes. Diabetes Technol Ther. 2010 Apr;12(4):257-62. | CrossRef | PubMed | Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998 Mar 7;316(7133):736-41. | CrossRef | PubMed |
Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998 Mar 7;316(7133):736-41. | CrossRef | PubMed | Leventhal EA, Prohaska TR. Age, symptom interpretation, and health behavior. J Am Geriatr Soc. 1986 Mar;34(3):185-91. | PubMed |
Leventhal EA, Prohaska TR. Age, symptom interpretation, and health behavior. J Am Geriatr Soc. 1986 Mar;34(3):185-91. | PubMed | Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002 Mar;25(3):458-63. | CrossRef | PubMed |
Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002 Mar;25(3):458-63. | CrossRef | PubMed | Hu Y, Bakhotmah BA, Alzahrani OH, Wang D, Hu FB, Alzahrani HA. Predictors of diabetes foot complications among patients with diabetes in Saudi Arabia. Diabetes Res Clin Pract. 2014 Nov;106(2):286-94. | CrossRef | PubMed |
Hu Y, Bakhotmah BA, Alzahrani OH, Wang D, Hu FB, Alzahrani HA. Predictors of diabetes foot complications among patients with diabetes in Saudi Arabia. Diabetes Res Clin Pract. 2014 Nov;106(2):286-94. | CrossRef | PubMed | Eiser C, Flynn M, Green E, Havermans T, Kirby R, Sandeman D, et al. Quality of life in young adults with type 1 diabetes in relation to demographic and disease variables. Diabet Med. 1992 May;9(4):375-8. | CrossRef | PubMed |
Eiser C, Flynn M, Green E, Havermans T, Kirby R, Sandeman D, et al. Quality of life in young adults with type 1 diabetes in relation to demographic and disease variables. Diabet Med. 1992 May;9(4):375-8. | CrossRef | PubMed | Urzúa M A, Chirino A, Valladares G. Autoreporte de la calidad de vida relacionada con la salud en diabetes mellitus tipo 2. Rev. méd. Chile [Internet]. 2011 Mar;139(3):313-320. | CrossRef |
Urzúa M A, Chirino A, Valladares G. Autoreporte de la calidad de vida relacionada con la salud en diabetes mellitus tipo 2. Rev. méd. Chile [Internet]. 2011 Mar;139(3):313-320. | CrossRef | Klein BE, Klein R, Moss SE. Self-rated health and diabetes of long duration. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Diabetes Care. 1998 Feb;21(2):236-40. | CrossRef | PubMed |
Klein BE, Klein R, Moss SE. Self-rated health and diabetes of long duration. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. Diabetes Care. 1998 Feb;21(2):236-40. | CrossRef | PubMed | Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006 Apr;29(4):823-9. | CrossRef | PubMed |
Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006 Apr;29(4):823-9. | CrossRef | PubMed | Bernal H, Woolley S, Schensul JJ, Dickinson JK. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Educ. 2000 Jul-Aug;26(4):673-80. | CrossRef | PubMed |
Bernal H, Woolley S, Schensul JJ, Dickinson JK. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Educ. 2000 Jul-Aug;26(4):673-80. | CrossRef | PubMed | Kim G, Shim R, Ford KL, Baker TA. The relation between diabetes self-efficacy and psychological distress among older adults: do racial and ethnic differences exist? J Aging Health. 2015 Mar;27(2):320-33. | CrossRef | PubMed |
Kim G, Shim R, Ford KL, Baker TA. The relation between diabetes self-efficacy and psychological distress among older adults: do racial and ethnic differences exist? J Aging Health. 2015 Mar;27(2):320-33. | CrossRef | PubMed | Mansyur CL, Rustveld LO, Nash SG, Jibaja-Weiss ML. Hispanic Acculturation and Gender Differences in Support and Self-Efficacy for Managing Diabetes. Diabetes Educ. 2016 Jun;42(3):315-24. | CrossRef | PubMed |
Mansyur CL, Rustveld LO, Nash SG, Jibaja-Weiss ML. Hispanic Acculturation and Gender Differences in Support and Self-Efficacy for Managing Diabetes. Diabetes Educ. 2016 Jun;42(3):315-24. | CrossRef | PubMed | Martinez Y, Campbell SM, Hann M, Bower P. The relationship between quality of care and self-management in patients with type 2 diabetes: a cross-sectional survey in primary care in Mexico. Qual Prim Care. 2014;22(6):262-9. | PubMed |
Martinez Y, Campbell SM, Hann M, Bower P. The relationship between quality of care and self-management in patients with type 2 diabetes: a cross-sectional survey in primary care in Mexico. Qual Prim Care. 2014;22(6):262-9. | PubMed |