 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: empathy, medical students, character
Introduction
Medical empathy is a characteristic that allows us to understand the subjective experiences and the perspective of the patient. Empathy can improve the clinical outcomes of our clinical actions. However, it is not easy to teach this ability in a medical school program.
Objective
We aimed to identify the level of empathy and related factors in students enrolled in medicine in 2019.
Methods
We conducted a cross-sectional, descriptive study. We used a questionnaire with sociodemographic questions, and Jefferson's Medical Empathy Scale to measure the variables.
Results
We surveyed 189 medical students. The mean score was 118,01 (range: 20 to 140), standard deviation, 11,61; median, 120; and a Cronbach's alpha coefficient of 0,76. We found that the year of the enrollment is inversely related to the level of empathy (p = 0,0095), that the female sex has a higher level of empathy (p = 0,0123) and that practicing a religious denomination is related to a higher level of empathy (p = 0,0001).
Conclusion
Medical students have an above-average level of empathy when compared to other local studies. We describe higher levels of empathy according to sex, and religious beliefs, and an inverse relation to the year of enrollment.
“One of the most common tasks of each physician is communication with patients and family members, regardless of whether their field is in surgery, internal medicine or family medicine” – (Kappauf HW, 2004[1]).
Empathy is a psychological concept that allows humans to understand another person's emotions and feelings, recognizing them as similar[2]. This varies according to each individual, whether by education, social context or personal experiences. Likewise, empathy is an interpersonal skill and is tied to professional competence. As a concept, empathy encompasses many dimensions, having four basic components: emotional, cognitive, moral, and behavioral[3].
Viewed from a medical perspective, empathy is a cognitive attribute that must be emphasized in medical schools so as to achieve the education of altruistic, compassionate and empathetic physicians who, while caring for patients, understand the patient's perspective and are able to transmit this understanding. Similarly, empathy is an important aspect of “professionalism” in medical practice[4]. Empathy is crucial because it allows the strengthening and development of a positive doctor to patient relationship, generating greater satisfaction for the consultation; it also facilitates the obtaining of information when elaborating the clinical record, which with a correct and relevant diagnosis ends up improving medical care[5].
Despite its importance, empathy is one of the most difficult characteristics to teach and is affected by the educational model applied to each school, being considered by some authors as a selection criteria for the aspiring medical student[6],[7]. Different characteristics in each person, such as age, sex, marital status, and other factors may also affect empathy[8],[9]. However, there is still no conclusive association among the factors, as many of the results of studies with similar methodology are discordant, as is the case when having or not having children. Some authors point out that it affects positively while others point out that it affects negatively[9],[10].
In the research field, publications on empathy are scarce. Nevertheless, in recent years more frequent research has been carried out due to the development of new tools. In our country, publications are still meager and focus on three groups: medical students, stomatology students and resident physicians[11],[12],[13]. Of these, only the study of stomatology students and resident physicians was conducted in our local environment, while the group of medical students was studied in another region of the country, so it becomes important to carry out additional studies that can complement the findings.
One of the tools that has helped measure the level of empathy is the Jefferson Empathy Scale, a survey validated in different countries around the world, including Latin American countries, that has previously been used in studies already referred to in our country[11],[12],[13]. The tool has construction, convergent, and discriminating validity. In addition, it has a Cronbach coefficient of 0.82 in our medium, attributes that make it a reliable measuring tool[11].
In this context, we carried out this study with the aim of assessing the level of empathy of medical students in our environment. Additionally, we explored certain variables that may be related to the level of empathy in medicine, with an emphasis on three of the four stages of the medical career in our country: preclinical, clinical and pre-professional[14]. We decided to exclude the first stage, integral basic formation, since it is not exclusive to the medical career in our country. In this way, the study seeks to establish a precedent that can serve to strengthen empathy in the curriculum mesh of students.
Study design
This paper is a cross-sectional descriptive study of medical students enrolled in Universidad Peruana Cayetano Heredia.
Population
Undergraduate medical students of Universidad Peruana Cayetano Heredia who have completed the stages of preclinical, clinical, or pre-professional training from 2018-2.
Inclusion criteria
Students enrolled in term 7 (the term immediately after finishing the preclinical training stage), term 11 (the term immediately after finishing the clinical training stage) of the medical career from 2019-1 or who have completed term 14 (last term of pre-professional training) in the period 2018-2.
Exclusion criteria
Students who do not agree to participate in the study
Sample
A population of 417 students is divided into three groups: 154 students in the 7th term, 137 students in the 11th term, and 126 students who completed the 14th term. Non-probabilistic sampling is performed according to Fuentelsaz[15], following the following formula:
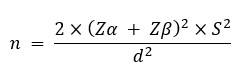
Where it is considered:
Z = 0.01 (2.576)
Z = 0.10 (1.282)
S = 14.51, based on a study carried out earlier in our medium[11].
D = 10, which is the minimum difference we expect to find in each group to consider it as significant[16].
Replacing the values gets us 62.67 as a result and approximated to the nearest integer we get a sample size of 63 participants per group.
Type of sampling
Non-probabilistic sampling—participants entered the study until the sample size was completed.
Variables
The following variables were chosen as they are relevant in the revised literature, finding that they might have a relationship with empathy.
Techniques and procedures
Upon approval of the ethics committee and acceptance by the participant to be a part of the study, data from study participants were collected through the use of a tool, the Jefferson Medical Empathy Scale in its “S” version of student translated into the Spanish language[16], and a data collection sheet to obtain the values of independent variables (age, sex, religious confession, child tenure, school and curriculum mesh empathy course).
The Jefferson Medical Empathy Scale is a 20-question questionnaire scored in a 7-point Likert scale, where 1 corresponds to “totally disagree” and 7 to “totally agree” respectively. The scale has a minimum score of 20 and maximum of 140. In addition, it allows the measurement of empathy in three components: attention with compassion, taking perspective, and the ability to walk in the patient’s shoes.
As for its interpretation, the score obtained has a direct relationship with the level of empathy; that is, a higher score equates to a higher level of empathy. The authors of the tool do not set cut-off points to determine at which intervals the level of empathy is “good” or “bad”; however, several authors have attempted to categorize the results so that a statistical analysis is performed as if it were an ordinal qualitative variable[11],[12]. In this study, the score is taken as a discrete quantitative variable.
The data collection sheet is an instrument designed by the researchers of this study to collect sociodemographic data from participants; it has not been validated. Both instruments were applied via a web interface provided by the Universidad Peruana Cayetano Heredia, thus ensuring the correct filling of the formats, and avoiding possible biases, either due to lack of time, lack of confidentiality or other eventualities.
Ethical aspects of the study
Each participant was identified with an anonymous code to ensure the confidentiality of the participant, no information that could be linked to the participants was kept.
This work was reviewed and approved by the Institutional Committee for Research Ethics of the Universidad Peruana Cayetano Heredia. An information sheet setting out participant rights was provided to participants prior to the completion of the survey.
Analysis plan
The data was collected into a database for processing and analysis with STATA/SE© v15, provided by the Universidad Peruana Cayetano Heredia. A descriptive analysis of the dependent variable was performed to determine mean, standard deviation, confidence intervals, and distribution. The Shapiro-Wilk test was subsequently used, which determined that it did not follow a normal distribution, thus opting to use non-parametric tests: Mann-Whitney U test for dichotomous variables, Kruskal-Wallis test for polychotomous variables, and the Spearman correlation test for continuous variables. The value of p < 0.05 was considered as significant.
The study consisted of 189 participants divided into 3 groups of 63 people for each of the established sub-groups. The average age of the study participants is 23.05 years, while the average age of each sub-group (students who have completed preclinical, clinical, and pre-professional studies) was 20.92 years, 23.29 years and 24.94 years, respectively. Of the total participants, 35.45% were males, 99.47% had no children, 37.57% did not practice any religion, and 95.24% went to private school (see Table 1).
Table 1. Distribution of variables in the total population and in each of the subgroups.
As for the Jefferson Empathy Scale, the results show that the average empathy score for all participants is 118.01 (standard deviation: 11.61; 95% confidence interval: 116.34 to 119.68). The descriptive analysis is also performed for each sub-group, and the results can be seen in Table 2 and Table 3. Additionally, a Cronbach alpha coefficient of 0.76 was obtained.
Table 2. Descriptive statistics and percentiles of the score obtained by UPCH medical students.
The Shapiro-Wilk test was applied to the dependent variable (empathy level). As it did not present a normal distribution, non-parametric tests were used in the data analysis.
To assess the level of empathy in the different sub-groups, the Kruskal-Wallis test was applied, finding a statistically significant difference (p = 0.0095) between the three groups. Additional analyses were performed with the Mann-Whitney U test to compare the groups, finding a statistically significant difference between preclinical and clinical students (p = 0.004), and between preclinical and pre-professional students (p = 0.022); however, no statistically significant difference was found between clinical and pre-professional students (p = 0.45) (see Table 4).
In addition, the analysis for each of the three components of measured by the Jefferson Empathy Scale showed that there is no significant difference in the component of compassionate care (p = 0.0696); there is a significant difference in the component of perspective taking (p = 0.0406), finding a higher level in the group of pre-clinical students compared to the rest; and that there is a significant difference in the component of walking in the patient's shoes (p = 0.0167), with a higher level in the preclinical and pre-professional group compared to the clinical group. (See Table 5).
Table 4. Characteristics of UPCH medical students, JSE empathy level and respective statistics.
Female participants scored an average of 120.24 and male participants averaged 113.96, with a statistically significant difference (p = 0.01) when Mann-Whitney's U test was applied.
Spearman's correlation test was used to assess whether the age and score obtained by the participants are variables independent of each other, obtaining a weak relationship (rho = -0,125) that was not statistically significant (p = 0.087).
As for the religion practiced by the participants, because no significant sample of several responses was obtained (Evangelical s 1%, Buddhist < 1%, Adventist < 1%), it was decided to analyze religious belief as a whole. Thus, the non-religious group of participants scored an average of 113.46 while the group practicing any religion scored an average of 120.75, finding a statistically significant difference (p = 0.0001).
Finally, as to whether or not students received any courses or workshops focused on empathy, it was found that the group that received some course or workshop on empathy (preclinical and clinical students) has an average of 118.30 on the Jefferson Empathy Scale, while the group that did not receive any course or workshop on empathy (pre-professional students) have an average of 117.43, which is not statistically significant (p = 0.3777).
This study found that the average score obtained by medical students on the Jefferson Empathy Scale was 118.01 (standard deviation: 11.61; 95% confidence interval: 116.34 to 119.68) and that there is a significant difference between the different stages of study, showing a lower score on the more advanced stages of the career. Although this study, due to its nature, does not allow a temporal analysis, it is consistent with multiple studies conducted in medical students in which empathy level decreases with time[17],[18],[19]. This phenomenon has been described by some authors as “heart hardening” or “dehumanization” of the medical student, referring to the decrease throughout the medical career in the level of empathy, and that it requires additional qualitative studies to understand the underlying cause[20],[21].
Comparing the results obtained by the Universidad Peruana Cayetano Heredia medical students with other local studies, we found that the score obtained (average: 118.01, standard deviation: 11.61) is higher than that found by Gutierrez-Ventura F in 2012[13] on 258 private university stomatology students who scored 109.63 (standard deviation: 13.69), which is higher than that found by Morales-Concha in 2017[12] in 206 medical students from another Peruvian university who scored 87.77 (standard deviation: 15.16) and higher than that found by Mayo G in 2018[11] in 100 resident physicians of a national hospital of 3rd-level care who scored 112.88 (from: 14.51). This difference could be due to the different types of training that these populations received (medical students, stomatology students, resident physicians); however, another type of methodology is required to validate these findings.
Age is a factor that could influence the level of empathy. However, the results are contradictory—some studies describe a direct relationship between the level of empathy and the age of the participants[22],[23], while other studies found the opposite[24]. One problem with the interpretation of these contradictory results is that most studies are conducted in populations of similar ages and confusion factors from interference of other variables is a possibility, which makes it difficult to determine the influence of age as a factor. In the case of this study, no statistically significant differences were found with respect to the age of the participants and the Jefferson Empathy Score (p = 0.0865) when the correlation coefficient of Spearman (rho = -0.125) was calculated.
Empathy has already been recognized as dependent on sex, with the female sex being more empathic than its male counterpart[8],[19],[25]. The present study found that there is a statistically significant difference between the two sexes (p = 0.012), with the female population obtaining an average score on the Jefferson Empathy Scale of 120.24 (standard deviation: 8.97) and the male population a score of 113.96 (standard deviation: 14.51). This difference can be explained by a few factors. First, it has been suggested that women are more receptive to emotional cues than males, leading to a better understanding and a relationship of greater empathy[26]. It has also been proposed that these differences are the result of the cultural expectations on gender roles[8]. Finally, it is believed that women, through the evolutionary process, have developed attitudes of care towards children that can then be extrapolated to patient care[8].
Religion is not often explored as a variable when studying empathy; however, there are certain studies that suggest that empathy and religious beliefs are not related[27],[28]. In a Latin American study on medical students in 2016, Parra G indicates that students with Catholic beliefs scored higher than that of non-religious students, but this finding was not statistically significant[24]. In this study we found a statistically significant difference (p = 0.0001) in the Jefferson Empathy Score when comparing students with any religious belief (average: 120.75, standard deviation: 9.61) to students without a religious belief (average: 113.46, standard deviation: 13.19). In our context, these differences could be explained due to the fact that some religious private schools (predominantly catholic) often teach some aspects that expose students to other realities of the country or promotes awareness about the existence of them, promoting in one way or another the development of an attitude of greater empathy. However, this cannot be confirmed because within our variables the type of school was not considered, whether it was a religious school, parochial school, non-religious school, evangelical or other.
Finally, whether students have received an empathy course or workshop was explored, without finding statistically significant difference in the level of empathy according to the Jefferson Empathy Score (p = 0.3777). This is consistent with previous local studies, in which the same variable was explored but in residency doctors in a local hospital[11]. While no statistically significant differences were found in receiving an empathy course or workshop, this could explain the difference in the taking perspective component, in which preclinical students, who received multiple empathy workshops, were found to have obtained significantly greater value than the rest. Nonetheless, our result is exploratory and additional studies with the appropriate design are required to establish the impact of an intervention within a homogeneous population.
Limitations
Like other studies carried out on the same subject, the main limitation lies in the chosen design: being a cross-sectional study, it does not allow the tracking of the evolution of empathy throughout a career or to establish a temporal link. In addition, the groups studied have been subjected to different curricular plans following the new Peruvian University Law 30220 and the international validation processes within the Universidad Peruana Cayetano Heredia, which makes it difficult to extrapolate or generalize the data obtained in this study[29]. As researchers, we recommend studying medical empathy as a changing process, following a single cohort over time and qualitative studies to understand the dynamics of it over time.
On the other hand, variables such as school of origin or parenting could not be explored since exceedingly small populations (less than 10 participants of the total) were obtained. Another limitation is that the impact of other factors or variables—such as the personality of students, the conduct of volunteering activities, artistic inclinations, the inclination of medical specialty, performing extra-curricular activities and the burnout or professional wear and tear—were not explored. Burnout is a pathological syndrome in which emotional exhaustion and detachment develop in response to prolonged work stress; depending on the working context, up to four out of five health professionals can suffer from burnout[30]. There is evidence that empathy and burnout have an inverse relationship, which could give another explanation to the findings of this study, especially the differences in the component of walking in the patient's shoes[6],[31].
The level of medical empathy of Universidad Peruana Cayetano Heredia medical students according to the Jefferson Empathy Scale is high compared to populations of other studies.
The level of medical empathy of preclinical medical students is significantly higher than the empathy recorded in clinical and pre-professional students, which could be explained by the fact that this group has taken courses of empathy and have not been exposed to the clinical environment.
The level of empathy has a direct relationship to the female sex and having a religious belief, while it has an inverse relationship with the year of study. No relation in the rest of the variables was found.
Roles and contributions of authorship
GM: conceptualization, formal analysis, research, methodology, administration, resources, supervision, visualization, drafting and review. DG: conceptualization, data healing, formal analysis, research, methodology, visualization, writing, review and editing. NV: conceptualization, formal analysis, research, visualization, writing and review.
Competing interests
The authors declare that they have no conflicts of interest with the subject matter in this article.
Funding
There were no sources of funding for this work.
Ethical aspects
This study was approved by the Institutional Committee of Ethics in Research of the Universidad Peruana Cayetano Heredia.
Data availability statement
The authors state that the data obtained from this investigation is available upon request. This study was carried out to obtain the professional title of “Medical Doctor” of DG and NV, and is published in the repository of the Universidad Peruana Cayetano Heredia.

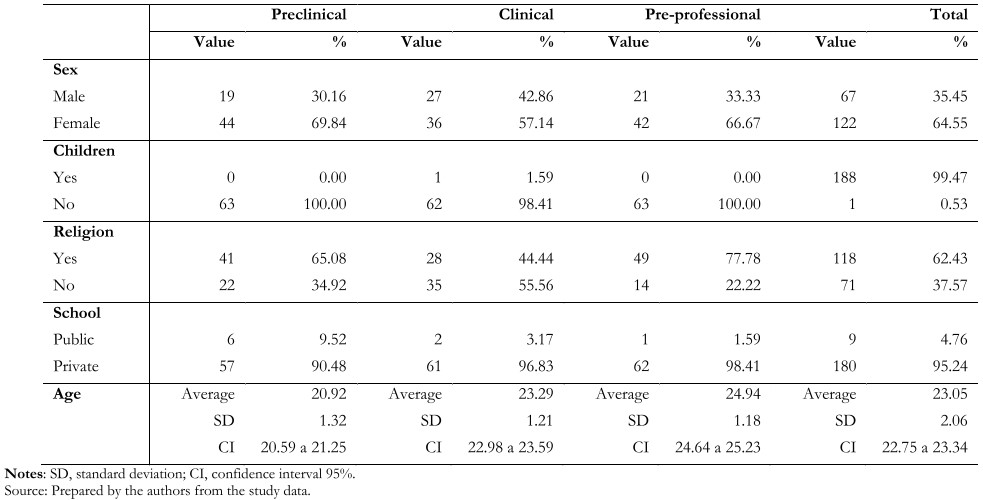 Table 1. Distribution of variables in the total population and in each of the subgroups.
Table 1. Distribution of variables in the total population and in each of the subgroups.

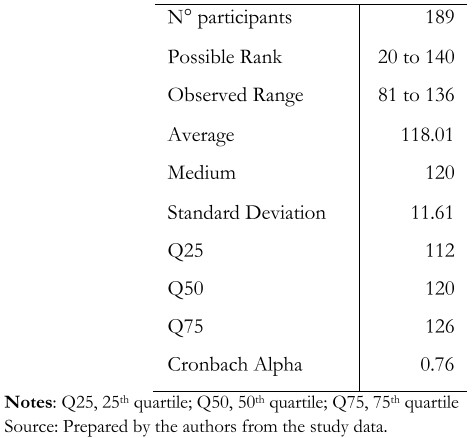 Table 2. Descriptive statistics and percentiles of the score obtained by UPCH medical students.
Table 2. Descriptive statistics and percentiles of the score obtained by UPCH medical students.

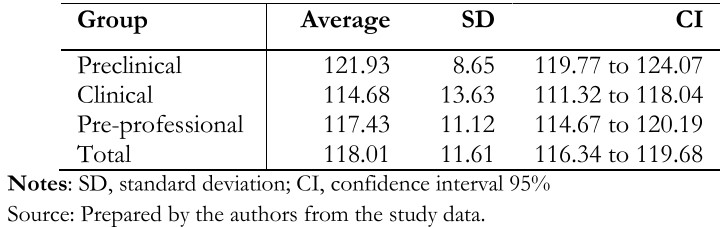 Table 3. Distribution of the variable “empathy level” in the total population and in each of the subgroups.
Table 3. Distribution of the variable “empathy level” in the total population and in each of the subgroups.

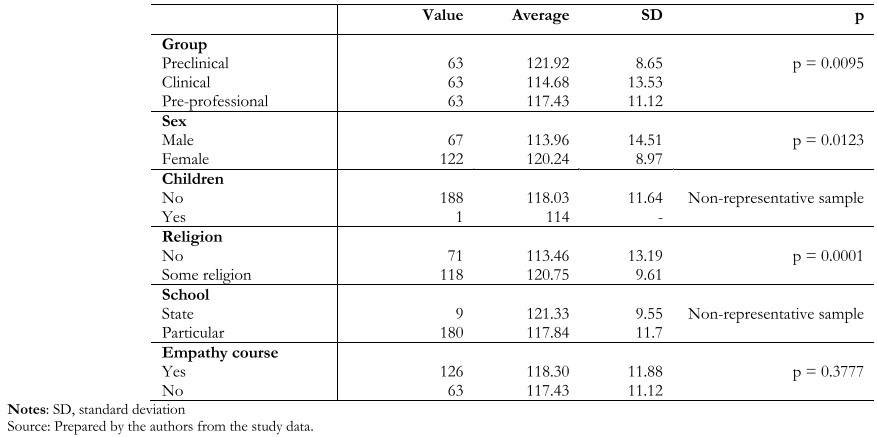 Table 4. Characteristics of UPCH medical students, JSE empathy level and respective statistics.
Table 4. Characteristics of UPCH medical students, JSE empathy level and respective statistics.

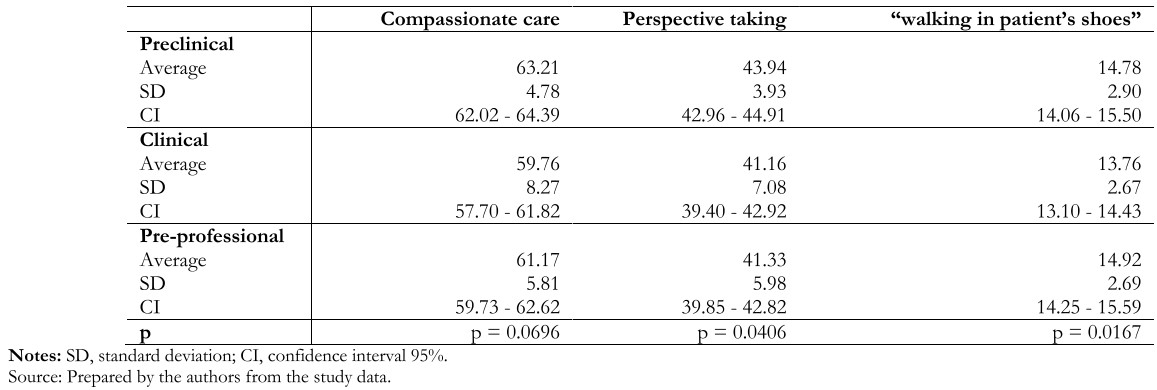 Table 5. Distribution of the JSE score according to each of its components in the 3 subgroups of studies.
Table 5. Distribution of the JSE score according to each of its components in the 3 subgroups of studies.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introduction
Medical empathy is a characteristic that allows us to understand the subjective experiences and the perspective of the patient. Empathy can improve the clinical outcomes of our clinical actions. However, it is not easy to teach this ability in a medical school program.
Objective
We aimed to identify the level of empathy and related factors in students enrolled in medicine in 2019.
Methods
We conducted a cross-sectional, descriptive study. We used a questionnaire with sociodemographic questions, and Jefferson's Medical Empathy Scale to measure the variables.
Results
We surveyed 189 medical students. The mean score was 118,01 (range: 20 to 140), standard deviation, 11,61; median, 120; and a Cronbach's alpha coefficient of 0,76. We found that the year of the enrollment is inversely related to the level of empathy (p = 0,0095), that the female sex has a higher level of empathy (p = 0,0123) and that practicing a religious denomination is related to a higher level of empathy (p = 0,0001).
Conclusion
Medical students have an above-average level of empathy when compared to other local studies. We describe higher levels of empathy according to sex, and religious beliefs, and an inverse relation to the year of enrollment.
 Autores:
Germán Málaga[1], Diego Gayoso[1], Nikole Vásquez[1]
Autores:
Germán Málaga[1], Diego Gayoso[1], Nikole Vásquez[1]

Citación: Málaga G, Gayoso D, Vásquez N. Empathy in medical students of a private university in Lima, Peru: A descriptive study. Medwave 2020;20(4):e7905 doi: 10.5867/medwave.2020.04.7905
Fecha de envío: 31/10/2019
Fecha de aceptación: 3/3/2020
Fecha de publicación: 25/5/2020
Origen: No solicitado
Tipo de revisión: Con revisión por pares externa, por cuatro árbitros a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Rozengway Vijil H, García Reyes AM, Vallecillo Amador LI. Niveles de empatía según la escala de Jefferson en estudiantes de Medicina, Enfermería y Odontología de Honduras. Rev Cient Cienc Méd. 2016;19(2):14-9. [On line]. | Link |
Rozengway Vijil H, García Reyes AM, Vallecillo Amador LI. Niveles de empatía según la escala de Jefferson en estudiantes de Medicina, Enfermería y Odontología de Honduras. Rev Cient Cienc Méd. 2016;19(2):14-9. [On line]. | Link | Neumann M, Scheffer C, Tauschel D, Lutz G, Wirtz M, Edelhäuser F. Physician empathy: definition, outcome-relevance and its measurement in patient care and medical education. GMS Z Med Ausbild. 2012;29(1):Doc11. | CrossRef | PubMed |
Neumann M, Scheffer C, Tauschel D, Lutz G, Wirtz M, Edelhäuser F. Physician empathy: definition, outcome-relevance and its measurement in patient care and medical education. GMS Z Med Ausbild. 2012;29(1):Doc11. | CrossRef | PubMed | Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002 Oct;77(10 Suppl):S58-60. | PubMed |
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002 Oct;77(10 Suppl):S58-60. | PubMed | Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005 Mar 2;293(9):1100-6. | PubMed |
Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005 Mar 2;293(9):1100-6. | PubMed | Ramírez-Villaseñor I. La infelicidad de los médicos: un fenómeno complejo y un intento por comprenderla. Rev Mex Med Fam. 2018;1:37-44. [On line]. | Link |
Ramírez-Villaseñor I. La infelicidad de los médicos: un fenómeno complejo y un intento por comprenderla. Rev Mex Med Fam. 2018;1:37-44. [On line]. | Link | Sade RM, Stroud MR, Levine JH, Fleming GA. Criteria for selection of future physicians. Ann Surg. 1985 Feb;201(2):225-30. | PubMed |
Sade RM, Stroud MR, Levine JH, Fleming GA. Criteria for selection of future physicians. Ann Surg. 1985 Feb;201(2):225-30. | PubMed | Bratek A, Bulska W, Bonk M, Seweryn M, Krysta K. Empathy among physicians, medical students and candidates. Psychiatr Danub. 2015 Sep;27 Suppl 1:S48-52. | PubMed |
Bratek A, Bulska W, Bonk M, Seweryn M, Krysta K. Empathy among physicians, medical students and candidates. Psychiatr Danub. 2015 Sep;27 Suppl 1:S48-52. | PubMed | Park C, Lee YJ, Hong M, Jung CH, Synn Y, Kwack YS, et al. A Multicenter Study Investigating Empathy and Burnout Characteristics in Medical Residents with Various Specialties. J Korean Med Sci. 2016 Apr;31(4):590-7. | CrossRef | PubMed |
Park C, Lee YJ, Hong M, Jung CH, Synn Y, Kwack YS, et al. A Multicenter Study Investigating Empathy and Burnout Characteristics in Medical Residents with Various Specialties. J Korean Med Sci. 2016 Apr;31(4):590-7. | CrossRef | PubMed | Moralle M, Preston J, Chen L, Berberian W. An Exploratory Study of Empathy in Resident Physicians at an Urban Medical Center. Int J Caring Sci. 2016;9(2):526-33. [On line]. | Link |
Moralle M, Preston J, Chen L, Berberian W. An Exploratory Study of Empathy in Resident Physicians at an Urban Medical Center. Int J Caring Sci. 2016;9(2):526-33. [On line]. | Link | Mayo G, Ponce D, Quijano E. Empatía y factores relacionados en médicos residentes de un hospital nivel de atención III según la escala de empatía médica de Jefferson en el año 2018 en Lima, Perú [Tesis de grado]. Perú: Universidad Peruana Cayetano Heredia; 2018. [On line]. | Link |
Mayo G, Ponce D, Quijano E. Empatía y factores relacionados en médicos residentes de un hospital nivel de atención III según la escala de empatía médica de Jefferson en el año 2018 en Lima, Perú [Tesis de grado]. Perú: Universidad Peruana Cayetano Heredia; 2018. [On line]. | Link | Morales-Concha L, Ccarita-Yucra K, Marroquin-Santa Cruz JA, Atamari-Anahui N. Evaluación de la empatía en estudiantes de medicina humana en una universidad pública de la sierra sur del Perú. Educ Med. 2018;19(6):327-332. | CrossRef |
Morales-Concha L, Ccarita-Yucra K, Marroquin-Santa Cruz JA, Atamari-Anahui N. Evaluación de la empatía en estudiantes de medicina humana en una universidad pública de la sierra sur del Perú. Educ Med. 2018;19(6):327-332. | CrossRef | Gutierrez-Ventura F, Huerta BQ, Pinedo ML, Vergaray JM, Narváez VPD, Zamorano A, et al. Medición del nivel de percepción empática de los estudiantes de la Facultad de Estomatología Roberto Beltrán. Universidad Peruana Cayetano Heredia. Rev Estomatológica Hered. 2014;22(2):91. | CrossRef |
Gutierrez-Ventura F, Huerta BQ, Pinedo ML, Vergaray JM, Narváez VPD, Zamorano A, et al. Medición del nivel de percepción empática de los estudiantes de la Facultad de Estomatología Roberto Beltrán. Universidad Peruana Cayetano Heredia. Rev Estomatológica Hered. 2014;22(2):91. | CrossRef | Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia. Pregrado Medicina. Universidad Peruana Cayetano Heredia, Lima, Perú; 2019. [On line]. | Link |
Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia. Pregrado Medicina. Universidad Peruana Cayetano Heredia, Lima, Perú; 2019. [On line]. | Link | Fuentelsaz C. Formación continuada: Cálculo del tamano de la muestra. Matronas Profesión. 2004;5(18):5-13.
Fuentelsaz C. Formación continuada: Cálculo del tamano de la muestra. Matronas Profesión. 2004;5(18):5-13.  Hojat, M. Empathy in health professions education and patient care. New York: Springer International; 2016.
Hojat, M. Empathy in health professions education and patient care. New York: Springer International; 2016.  Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004 Sep;38(9):934-41. | PubMed |
Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004 Sep;38(9):934-41. | PubMed | Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007 Oct;22(10):1434-8. | PubMed |
Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007 Oct;22(10):1434-8. | PubMed | Kataoka HU, Koide N, Ochi K, Hojat M, Gonnella JS. Measurement of empathy among Japanese medical students: psychometrics and score differences by gender and level of medical education. Acad Med. 2009 Sep;84(9):1192-7. | CrossRef | PubMed |
Kataoka HU, Koide N, Ochi K, Hojat M, Gonnella JS. Measurement of empathy among Japanese medical students: psychometrics and score differences by gender and level of medical education. Acad Med. 2009 Sep;84(9):1192-7. | CrossRef | PubMed | Newton BW, Barber L, Clardy J, Cleveland E, O'Sullivan P. Is there hardening of the heart during medical school? Acad Med. 2008 Mar;83(3):244-9. | CrossRef | PubMed |
Newton BW, Barber L, Clardy J, Cleveland E, O'Sullivan P. Is there hardening of the heart during medical school? Acad Med. 2008 Mar;83(3):244-9. | CrossRef | PubMed | Silver HK, Glicken AD. Medical student abuse. Incidence, severity, and significance. JAMA. 1990 Jan 26;263(4):527-32. | PubMed |
Silver HK, Glicken AD. Medical student abuse. Incidence, severity, and significance. JAMA. 1990 Jan 26;263(4):527-32. | PubMed | Ubillús G, Sidia M, Rentería D, Reátegui C, Rodríguez C, Sotelo J. La orientación empática en los estudiantes de medicina humana de la Universidad de San Martín de Porres. Horizonte Médico. 2010;10(2):37-43. [On line]. | Link |
Ubillús G, Sidia M, Rentería D, Reátegui C, Rodríguez C, Sotelo J. La orientación empática en los estudiantes de medicina humana de la Universidad de San Martín de Porres. Horizonte Médico. 2010;10(2):37-43. [On line]. | Link | Remón-Torres MA, Remón-Torres MM, Tataje-Lavanda MK. Características del nivel de empatía hacia el paciente en internos de medicina de dos hospitales nacionales. Rev Méd Panacea. 2013;3(1):2-5. | CrossRef |
Remón-Torres MA, Remón-Torres MM, Tataje-Lavanda MK. Características del nivel de empatía hacia el paciente en internos de medicina de dos hospitales nacionales. Rev Méd Panacea. 2013;3(1):2-5. | CrossRef | Parra G, Cámara R. Nivel de empatía médica y factores asociados en estudiantes de medicina. Inv Ed Med. 2017;6(24):221-227. | CrossRef |
Parra G, Cámara R. Nivel de empatía médica y factores asociados en estudiantes de medicina. Inv Ed Med. 2017;6(24):221-227. | CrossRef | Suh DH, Hong JS, Lee DH, Gonnella JS, Hojat M. The Jefferson Scale of Physician Empathy: a preliminary psychometric study and group comparisons in Korean physicians. Med Teach. 2012;34(6):e464-8. | CrossRef | PubMed |
Suh DH, Hong JS, Lee DH, Gonnella JS, Hojat M. The Jefferson Scale of Physician Empathy: a preliminary psychometric study and group comparisons in Korean physicians. Med Teach. 2012;34(6):e464-8. | CrossRef | PubMed | Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002 Sep;159(9):1563-9. | PubMed |
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002 Sep;159(9):1563-9. | PubMed | Dehning S, Girma E, Gasperi S, Meyer S, Tesfaye M, Siebeck M. Comparative cross-sectional study of empathy among first year and final year medical students in Jimma University, Ethiopia: steady state of the heart and opening of the eyes. BMC Med Educ. 2012 May 24;12:34. | CrossRef | PubMed |
Dehning S, Girma E, Gasperi S, Meyer S, Tesfaye M, Siebeck M. Comparative cross-sectional study of empathy among first year and final year medical students in Jimma University, Ethiopia: steady state of the heart and opening of the eyes. BMC Med Educ. 2012 May 24;12:34. | CrossRef | PubMed | Waqas A, Rehman A, Sohail A, Kamal O, Bukhari H, Munir F. Association of the religious orthodoxy and emotional empathy in pakistan muslim medical students. J Pak Psych Soc. 2015;12(2):43-6. [On line]. | Link |
Waqas A, Rehman A, Sohail A, Kamal O, Bukhari H, Munir F. Association of the religious orthodoxy and emotional empathy in pakistan muslim medical students. J Pak Psych Soc. 2015;12(2):43-6. [On line]. | Link | Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia. Plan de estudios. Universidad Peruana Cayetano Heredia, Lima, Perú; 2019. [On line]. | Link |
Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia. Plan de estudios. Universidad Peruana Cayetano Heredia, Lima, Perú; 2019. [On line]. | Link | Yuguero O. Estudio de la empatía y burnout de los médicos y enfermeras de Atención Primaria de la Región Sanitaria de Lleida y su relación con las variables clínicas [Tesis doctoral]. Lleida, España: Universitat de Lleida; 2015. [On line]. | Link |
Yuguero O. Estudio de la empatía y burnout de los médicos y enfermeras de Atención Primaria de la Región Sanitaria de Lleida y su relación con las variables clínicas [Tesis doctoral]. Lleida, España: Universitat de Lleida; 2015. [On line]. | Link |