 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: postpartum depression, epidemiology, social support, neonatal intensive care units
Introduction
Postpartum depression has increased significantly worldwide, but in the central Peruvian mountain, there are no studies that address this problem.
Objectives
To identify and to establish risk factors for postpartum depression in mothers whose children are hospitalized in pediatrics/neonatology units in Huancayo.
Methods
This is a case-control study. Medical records of mothers whose children were hospitalized in pediatrics/neonatology units during 2017 were included. The cases were defined as patients who “had symptoms of postpartum depression." This variable was crossed with other variables using logistical regression, odds ratio were obtained, their confidence intervals were set to 95%, and the p values were calculated.
Results
Sixty-one medical records of mothers with postpartum depression (cases) and 61 medical records of mothers without postpartum depression (control) were evaluated. In the multivariate analysis, the unemployed mothers had a bigger chance of postpartum depression (p < 0.001), as well as single mothers (p < 0.001), and those with an unplanned pregnancy (p = 0.003). Conversely, mothers who reported having serious problems with their partner had a smaller chance of postpartum depression (p = 0.003).
Conclusions
Different factors were found to be related to postpartum depression: marital situation, relationship with their partners, work conditions, and having an unplanned pregnancy.
Affective disorders are the second most common form of mental illness worldwide. According to the Global Burden of Disease study (World Health Organization / World Bank), by 2020, depression will be the second leading cause of disability[1]. There is a high risk of emotional disorders during the puerperium or postpartum period due to the emotional vulnerability experienced by mothers[2]. Postpartum depression is one of the most common complications during this period, with prevalence ranging from 10%–20%[3] and increasing in mothers whose children are hospitalized[4] and with the presence of various other factors[5], including psychological, organic, family, and socio-demographic variables[6].
Prevalence of postpartum depression and its risk factors (previous depression, low socioeconomic level, living in a developing country, family violence, low level of education, and poor relationship with family environment, among others) has been studied in various populations. A study in Canada reported a prevalence of 4%–15%[7]; in the United States, it was 13%–22%[8]; in Ireland, 13%[9]; and in Qatar, 18%[10].
Similar prevalence levels were found in Latin American countries. In Chile, prevalence varied from 22% to 51%[11]; in Argentina, it was 37%[12]; and in Colombia, 40%[13]. According to a study conducted in Lima, Peru, in 2008, this condition was found in 33% of puerperal women[2]. The risk of postpartum depression increases considerably in puerperal women whose children have been hospitalized, and reaches as high as 40% in mothers with a preterm child[4],[14],[15]. The objective of this research was to identify and establish risk factors for postpartum depression in mothers whose children were hospitalized in pediatric/neonatal units in Huancayo, a city in the central highlands of Peru.
Methods
Design and population
An observational analytical study with a case–control design was carried out. The information was collected from the medical records of puerperal women admitted to pediatric/neonatal units of two hospitals in Huancayo — Hospital Nacional Ramiro Prialé Prialé, part of the public social health insurance (Seguro Social de Salud or EsSalud) network, and Hospital Regional Docente Materno Infantil El Carmen, a Ministry of Health (MINSA) facility. The sample size was calculated using the formula for case–control studies. The values were obtained from a previous report16 for the exposure of interest in the controls and the proportion of exposed cases17, using the following equation:
n = [Zα2 pq + Zβ p1 q1 + p0 q 0] 2
(p1 - p0)2
Where:
n = sample size.
Zα = 95% confidence level, standardized value: 1.96, which is equivalent to a type I (α) error probability of 5%
p = ½ (p1 + p0)
q = 1 – p
Zβ = type II (β) error probability of 15%
p1 = p 0R ÷ [1 + p0 (R – 1)]
q1 = 1 – p1
p0 = expected relative frequency (or expected proportion) of the exposure of interest in controls: 40%
Proportion of exposed cases = 67%
R = expected odds ratio of the association = 3
Number of controls per case: 1
According to the analysis of the sampling formula for case–control studies, with 85% statistical power, 61 cases and 61 controls were required. Therefore, access to 122 hospital medical records — 61 for mothers with postpartum depression and 61 for mothers without the condition — was requested.
Selection of participants
The study was based on the medical records of the biological mothers of children less than 1 year old who were hospitalized in pediatric/neonatal units from January 1 to December 31, 2017. The inclusion criteria were: puerperal women who wished to participate in the study, agreed to sign the informed consent form, and had either a vaginal delivery or cesarean section. Exclusion criteria were: puerperal women who had impairment and/or speech problems, were hospitalized in intensive care units, did not agree to sign the informed consent form, and/or had been diagnosed with psychiatric pathologies. Once the study participants signed the informed consent form, the first instrument (Edinburgh Test) was administered. The case group included women who scored greater than or equal to 13 and the control group included puerperal women who scored less than 13.
Variables
The variable of interest was the presence of symptoms of postpartum depressive (according to the diagnosis these mothers had received, the psychiatric evaluation, and correct diagnosis in the respective clinical history). Other variables analyzed included obstetric variables (parity (ordinal), antecedent of abortion (dichotomous), pregnancy planning (dichotomous), type of delivery (dichotomous), prenatal care (polytomic), and weight gain (dichotomous)); psychological variables (family support (dichotomous) and relationship with partner (polytomy)); and social variables (age (ordinal), marital status (polytomics), schooling (polytomics), origin (polytomics), and employment status (dichotomous)). These variables were identified in previous studies[1],[2],[3],[4],[5],[7],[8],[10],[11],[13],[14],[15].
Data analysis
A database was developed for each hospital using Microsoft Excel® (Windows version 2013) and subsequently reviewed, debugged, and analyzed. IBM® SPSS® Statistics version 23 was used to analyze the data. A descriptive analysis of the categorical variables was carried out using absolute and relative frequencies. The bivariate statistics were generated, analyzing the risk factors and variable of interest (“presence of symptoms of postpartum depression”), and epidemiological associations determined, applying the cross-product (odds) ratios, with 95% confidence intervals (CIs) and p values. The multivariate analysis included all variables statistically significant in the bivariate analysis. The final model included 13 variables with odds ratios, 95% CIs, and p values. P values < 0.05 were considered significant.
Ethical aspects
This study was reviewed by the ethics committee of a maternal and child hospital (registration number: OFICIO No0678-2017-OADI-HONADOMANI-SB). To ensure study participants’ confidentiality and privacy, an anonymous list was used for the analysis; names were eliminated from the database once patient information was collected. To protect study participants’ well-being and integrity, data collection was limited to medical records, ensuring no physical or psychological damage was caused by the investigation.
The median age of the 122 mothers evaluated was 25 years (average 26.2), and the majority were 21 years old. Overall 71.3% (n = 87) were under 30 years old; 68.0% (n = 83) were married or living with a partner; 52.5% (n = 64) had a higher technical or university education; and 94.3% (n = 115) came from the provinces. The analysis of psychological variables showed that 27.9% (n = 34) did not have psychological support and 19.7% (n = 24) had serious problems in the relationship with their partner. The analysis of obstetric variables showed that 59.0% (n = 72) were multiparous; 30.3% (n = 37) had a history of abortion; 50.8% (n = 62) had an unplanned pregnancy; 50% (n = 61) delivered via caesarean section; 71.3% (n = 87) had either no prenatal care or only received it during the first trimester of pregnancy; and 75.4% (n = 92) gained more than 8 kilos during pregnancy (Table 1).
The bivariate analysis showed higher odds of postpartum depression in mothers who were unemployed (OR: 6.838, 95% CI: 2.588–18.067, p < 0.001); single (OR: 4.385, 95% CI: 1.948–9.870, p < 0.001); and/or had an unplanned pregnancy (OR: 3.279, 95% CI: 1.544–6.964, p = 0.002) and lower odds of the condition in those who reported having serious problems in their partner relationship (OR: 0.286, 95% CI: 0.099–0.826, p = 0.016) (Table 2).
In the final multivariate model, the dependent variable (having postpartum depression) was adjusted by other variables shown to be significant in the bivariate analysis. The multivariate analysis showed higher odds of postpartum depression in mothers who were unemployed (OR: 25.716, 95% CI: 5.706–115.903, p < 0.001); single (OR: 10.884, 95% CI: 3.117–38.003, p < 0.001); and/or had an unplanned pregnancy (OR: 11.369, 95% CI: 3.097–41.741, p = 0.003) and lower odds of the condition in those who reported having serious problems in their partner relationship (OR: 0.098, 95% CI: 0.021–0.452, p = 0.003) (Table 3).
Hospitalization of a newborn creates an extremely high level of stress in mothers, who perceive the situation as non-fulfillment of their expectations, and maternal role, due to physical and emotional isolation[18]. This leads to symptoms associated with postpartum depression, mainly in the initial stage of the child’s hospitalization[19].
Postpartum depression may also affect the mother–child relationship. Compared with mothers who do not have depressive symptoms, mothers with postpartum depression may have a more negative attitude toward their children, whom they may perceive as difficult to raise[12], especially mothers who do not receive treatment for depression. Likewise, children of mothers with postpartum depression may interact less, be less expressive, and, in general, present more negative emotions compared to children of mothers without the condition[20]. The effects on both mothers and children underscore the importance of identifying the factors associated with the development of postpartum depression in mothers whose children are hospitalized. Identifying the risk factors will help address the problem and support the planning and implementing of strategies for educational interventions to manage similar cases.
A study carried out in a Lima population showed that socioeconomic level was related to postpartum depression[21]. These results were similar to those found in a study in Piura in 2017[22]. In international studies, however, specifically in Chile, no significant relationship was found between postpartum depression and this variable[23].
A strong association was found between marital status and postpartum depression, with four times higher frequency of the signs and symptoms of this clinical condition in single women versus women who were married or living with a partner. This result is similar to what has been found elsewhere, including research in Italy[24], and India[25],[26], and a multicenter investigation of neonatal intensive care units in Argentina, Brazil, Chile, Paraguay, Peru, and Uruguay[27]. These studies found that maternal adaptation to the stressful aspects of neonatal hospitalization is strongly associated with socioeconomic, educational, and marital status. This effect might be related to reduced availability of resources or difficulty in understanding the information that is disseminated due to low socioeconomic/educational levels and/or lack of support. On the other hand, some studies found no association with these factors[28]. Therefore, each postpartum population needs to be evaluated, considering the above-mentioned factors, which can increase postpartum women’s vulnerability, and lead to unhealthy behaviors during the prenatal period.
In a Colombian study, prevalence of postpartum depression was 10.5%, similar to the findings of other studies in Latin America, which reported underdiagnosis of this pathology as well as poor treatment[29],[30],[31],[32].
Work status was another factor associated with postpartum depression, with sixfold higher odds of the condition in mothers who had no paid employment or were unemployed. This finding is understandable given that extra expenditures are required to support childen, and lack of paid work affects their needs as well as those of other family members, which makes the mother more prone to depression.
Socioeconomic disadvantages are most likely a factor in postpartum mothers’ emotional vulnerability, which lowers the threshold for depression in the face of various types of adversity. Several studies have shown that the unfavorable economic situation created by unemployment has a strong association with postpartum depression, including research in Spain by Sierra, who found an odds ratio of 9.7 for this variable[33], a study in Portugal by Augusto[34], and a study in Iran by Taherifard, who found an odds ratio of 2.0[35]. Our study found an even higher odds ratio for this variable (25.71).
In our study, pregnancy planning turned out to be another factor linked to postpartum depression, with those with unplanned pregnancies having three times higher odds of experiencing this condition compared to those who had planned their pregnancy. This finding concurs with results reported in studies carried out in Chile[23], Brazil[36], and Ecuador[37] but is contrary to what was found in other studies[29],[38] where women who had wanted to be pregnant presented psychological conditions such as psychosis, anguish, and uncertainty about providing postnatal care effectively. Therefore, the effect of pregnancy planning seems to vary by population, indicating the need for evaluation of each group.
Our study also evaluated the effect of the mother’s relationship with her partner. Our results showed an inverse relationship between postpartum depression and problems in the partner relationship. However, other studies have found the opposite result. For example, a study in Venezuela[28] showed that mothers without support from family or a partner were more likely to develop postpartum depression; a study in Chile showed that mothers separated from their partner had an increased probability of experiencing the condition[39]; and a study in metropolitan Lima[2] showed that psychiatric and psychosocial factors were the most important in predicting this little-known yet highly prevalent problem. Support of mothers in the postpartum stage is crucial for meeting the challenges and changes they experience during this period, and in many cases having a stable partner relationship seems to provide the mother with more security. Some research has shown that support from friends and family can also act as a protective factor against this form of mental illness[14].
With regard to education level, the results are mixed. A Venezuelan study[39] found that having less than a secondary education increased the risk of postpartum depression sevenfold. A study in Chile[28] found a similar result, with low level of education linked to this condition. However, a study in Lima[21] found that education level did not affect the odds of this form of depression, a finding that concurs with the results of our study.
In our study, mental health status, work status, and family variables (limited or lack of work opportunities outside the home, or loss of work during pregnancy or the puerperium period; pregnancy planning; marital status; status of partner relationship) had the most effect on the odds of postpartum depression. This suggests that social factors are the most important protection against postpartum depression. Another finding of the study was that having a hospitalized newborn child did not significantly impact the presence or absence of depressive symptoms.
Several variables were related to postpartum depression in the Peruvian central highlands. Most significant were marital status, work status, pregnancy planning, and status of partner relationship, with single and unemployed mothers and those who had not planned their pregnancy more likely to develop the condition, and mothers who reported serious problems in the relationship with their partner less likely to develop the condition.
From the editors
The original article was submitted in Spanish. This is the translated version of the article as provided by the authors, and has not been copyedited by the Journal.
Roles and authorship contributions
KMP: conceptualization, data management, formal analysis, research, methodology, project management, data presentation, manuscript preparation (development of the original draft), writing (revisions and editing).
GMQ: conceptualization, data management, formal analysis, research, methodology, project administration, data presentation, manuscript preparation (development of the original draft), writing (revisions and editing).
IECR: formal analysis, research, methodology, supervision, data presentation, manuscript preparation (development of the original draft), writing (revisions and editing).
CRM: conceptualization, data management, formal analysis, research, methodology, project management, supervision, data presentation, manuscript preparation (development of the original draft), writing (revisions and editing).
Competing interests
The authors have completed the ICMJE conflict of interest declaration form and declare that they have not received financing for the completion of this report; have no financial relationships with organizations that might have an interest in the published article, in the last three years; and have other relationships or activities that could influence the published article. The forms can be requested from the lead author or the Journal editor.
Financial disclosure
The authors declare that there were no external sources of funding.
Ethical aspects disclosure
This study was reviewed by the ethics committee of a maternal and child hospital (registration number: OFICIO No0678-2017-OADI-HONADOMANI-SB). An anonymous list was used for the analysis, and the confidentiality and privacy of the study participants was respected. The data is available upon request.
From the editors
The original article was submitted in Spanish. This is the translated version of the article as provided by the authors.

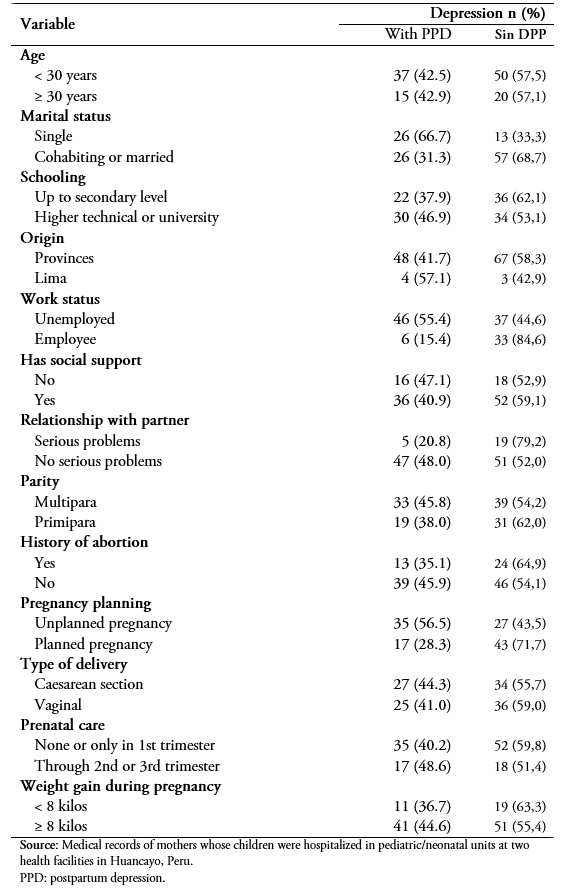 Table 1. Socio-demographic characteristics of mothers whose children were hospitalized in pediatric/neonatal units of two health facilities in Huancayo, Peru, 2017.
Table 1. Socio-demographic characteristics of mothers whose children were hospitalized in pediatric/neonatal units of two health facilities in Huancayo, Peru, 2017.

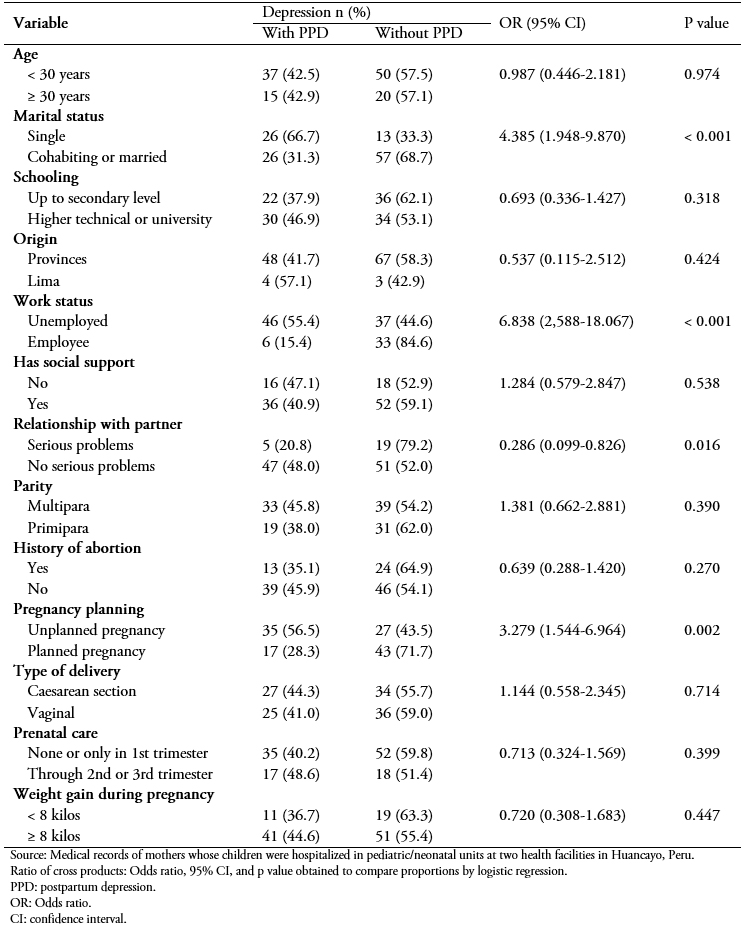 Table 2. Bivariate analysis of factors associated with the presence of postpartum depression in puerperium mothers evaluated at two hospitals in Huancayo, Peru, 2017
Table 2. Bivariate analysis of factors associated with the presence of postpartum depression in puerperium mothers evaluated at two hospitals in Huancayo, Peru, 2017

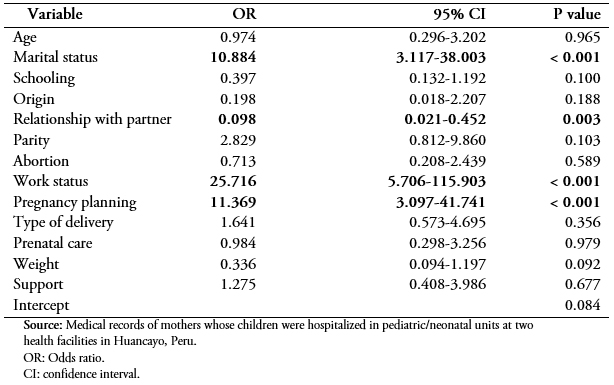 Table 3. Multivariate analysis of factors associated with the presence of postpartum depression in mothers seen in one of two hospitals in Huancayo, Peru, 2017
Table 3. Multivariate analysis of factors associated with the presence of postpartum depression in mothers seen in one of two hospitals in Huancayo, Peru, 2017
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introduction
Postpartum depression has increased significantly worldwide, but in the central Peruvian mountain, there are no studies that address this problem.
Objectives
To identify and to establish risk factors for postpartum depression in mothers whose children are hospitalized in pediatrics/neonatology units in Huancayo.
Methods
This is a case-control study. Medical records of mothers whose children were hospitalized in pediatrics/neonatology units during 2017 were included. The cases were defined as patients who “had symptoms of postpartum depression." This variable was crossed with other variables using logistical regression, odds ratio were obtained, their confidence intervals were set to 95%, and the p values were calculated.
Results
Sixty-one medical records of mothers with postpartum depression (cases) and 61 medical records of mothers without postpartum depression (control) were evaluated. In the multivariate analysis, the unemployed mothers had a bigger chance of postpartum depression (p < 0.001), as well as single mothers (p < 0.001), and those with an unplanned pregnancy (p = 0.003). Conversely, mothers who reported having serious problems with their partner had a smaller chance of postpartum depression (p = 0.003).
Conclusions
Different factors were found to be related to postpartum depression: marital situation, relationship with their partners, work conditions, and having an unplanned pregnancy.
 Autores:
Kelly Macedo-Poma[1], Pavel Gustavo Marquina-Curasma[1], Ibraín Enrique Corrales-Reyes[2], Christian R. Mejía[1]
Autores:
Kelly Macedo-Poma[1], Pavel Gustavo Marquina-Curasma[1], Ibraín Enrique Corrales-Reyes[2], Christian R. Mejía[1]

Citación: Macedo-Poma K, Marquina-Curasma PG, Corrales-Reyes IE, Mejía CR. Factors associated to depressive symptoms in mothers with children hospitalized in pediatric and neonatology units of Peru: a case-control study. Medwave 2019;19(5):7649 doi: 10.5867/medwave.2019.05.7649
Fecha de envío: 30/11/2018
Fecha de aceptación: 1/4/2019
Fecha de publicación: 10/6/2019
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Latorre-Latorre JF, Contreras-Pezzotti LM, Herrán-Falla OF. [Postnatal depression in a Colombian city. Risk factors]. Aten Primaria. 2006 Apr 15;37(6):332-8. | CrossRef | PubMed |
Latorre-Latorre JF, Contreras-Pezzotti LM, Herrán-Falla OF. [Postnatal depression in a Colombian city. Risk factors]. Aten Primaria. 2006 Apr 15;37(6):332-8. | CrossRef | PubMed | Aramburú P, Arellano R, Jáuregui S, Pari L, Salazara P, Sierra O. Prevalencia y factores asociados a depresión posparto en mujeres atendidas en establecimientos de salud del primer nivel de atención en Lima Metropolitana, junio 2004. Rev Peru Epidemiol 2008;12(3):1-5. | Link |
Aramburú P, Arellano R, Jáuregui S, Pari L, Salazara P, Sierra O. Prevalencia y factores asociados a depresión posparto en mujeres atendidas en establecimientos de salud del primer nivel de atención en Lima Metropolitana, junio 2004. Rev Peru Epidemiol 2008;12(3):1-5. | Link | Carrillo M. Factores asociados a depresión postparto en mujeres que acuden al Hospital General de Ecatepec "Dr. José María Rodríguez". México: Universidad Autónoma del Estado de México. Facultad de Medicina; 2013. | Link |
Carrillo M. Factores asociados a depresión postparto en mujeres que acuden al Hospital General de Ecatepec "Dr. José María Rodríguez". México: Universidad Autónoma del Estado de México. Facultad de Medicina; 2013. | Link | Plasencia V, Analy G, Díaz R, Rene D, Arangoitia C, Cáceres A, et al. Disfuncionalidad familiar y violencia familiar como factores de riesgo de depresión puerperal. Hospital Regional de Cajamarca, Perú2014. Scientia. 2017;9(2):145-52. | Link |
Plasencia V, Analy G, Díaz R, Rene D, Arangoitia C, Cáceres A, et al. Disfuncionalidad familiar y violencia familiar como factores de riesgo de depresión puerperal. Hospital Regional de Cajamarca, Perú2014. Scientia. 2017;9(2):145-52. | Link | Silverman ME, Reichenberg A, Savitz DA, Cnattingius S, Lichtenstein P, Hultman CM, et al. The risk factors for postpartum depression: A population-based study. Depress Anxiety. 2017 Feb;34(2):178-187. | CrossRef | PubMed |
Silverman ME, Reichenberg A, Savitz DA, Cnattingius S, Lichtenstein P, Hultman CM, et al. The risk factors for postpartum depression: A population-based study. Depress Anxiety. 2017 Feb;34(2):178-187. | CrossRef | PubMed | Hernandez-Gomez C, Brummitt PA, Canny DJ, Clarke RJ, Collier J, Danson CN, et al. Vulcan petawatt-operation and development. J Phys IV. 2006;133:555-9.
| Link |
Hernandez-Gomez C, Brummitt PA, Canny DJ, Clarke RJ, Collier J, Danson CN, et al. Vulcan petawatt-operation and development. J Phys IV. 2006;133:555-9.
| Link | Dois A, Uribe C, Villarroel L, Contreras A. [Risk factors for post partum depression]. Rev Med Chil. 2012 Jun;140(6):719-25. | CrossRef | PubMed |
Dois A, Uribe C, Villarroel L, Contreras A. [Risk factors for post partum depression]. Rev Med Chil. 2012 Jun;140(6):719-25. | CrossRef | PubMed | Konradt CE, Silva RA da, Jansen K, Vianna DM, Quevedo L de A, Souza LD de M, et al. Depressão pós-parto e percepção de suporte social durante a gestação. Rev Psiquiatr do Rio Gd do Sul. 2011;33(2):76-9. | Link |
Konradt CE, Silva RA da, Jansen K, Vianna DM, Quevedo L de A, Souza LD de M, et al. Depressão pós-parto e percepção de suporte social durante a gestação. Rev Psiquiatr do Rio Gd do Sul. 2011;33(2):76-9. | Link | Leahy-Warren P, McCarthy G, Corcoran P. Postnatal depression in first-time mothers: prevalence and relationships between functional and structural social support at 6 and 12 weeks postpartum. Arch Psychiatr Nurs. 2011 Jun;25(3):174-84. | CrossRef | PubMed |
Leahy-Warren P, McCarthy G, Corcoran P. Postnatal depression in first-time mothers: prevalence and relationships between functional and structural social support at 6 and 12 weeks postpartum. Arch Psychiatr Nurs. 2011 Jun;25(3):174-84. | CrossRef | PubMed | Bener A, Burgut FT, Ghuloum S, Sheikh J. A study of postpartum depression in a fast developing country: prevalence and related factors. Int J Psychiatry Med. 2012;43(4):325-37. | PubMed |
Bener A, Burgut FT, Ghuloum S, Sheikh J. A study of postpartum depression in a fast developing country: prevalence and related factors. Int J Psychiatry Med. 2012;43(4):325-37. | PubMed | Cuero-Vidal OL, Díaz-Marín AM . Prevalencia de depresión posparto en el Hospital San Juan de Dios, Cali , Colombia. Septiembre-Diciembre, 2011. Rev Colomb Obstet Ginecol. 2013 [citado 7 de febrero de 2019];64(4):371-8.
| Link |
Cuero-Vidal OL, Díaz-Marín AM . Prevalencia de depresión posparto en el Hospital San Juan de Dios, Cali , Colombia. Septiembre-Diciembre, 2011. Rev Colomb Obstet Ginecol. 2013 [citado 7 de febrero de 2019];64(4):371-8.
| Link | Jadresic EM. Depresión perinatal: Detección y tratamiento. Rev Médica Clínica Las Condes. 2014;25(6):1019-28. | Link |
Jadresic EM. Depresión perinatal: Detección y tratamiento. Rev Médica Clínica Las Condes. 2014;25(6):1019-28. | Link | Ortiz Martinez RA, Gallego Betancourt CX, Buitron Zuñiga EL, Meneses Valdés YD, Muñoz Fernandez NF, Gonzales Barrera MA. [Prevalence of Positive Screen for Postpartum Depression in a Tertiary Hospital and Associated Factors]. Rev Colomb Psiquiatr. 2016 Oct - Dec;45(4):253-261. | CrossRef | PubMed |
Ortiz Martinez RA, Gallego Betancourt CX, Buitron Zuñiga EL, Meneses Valdés YD, Muñoz Fernandez NF, Gonzales Barrera MA. [Prevalence of Positive Screen for Postpartum Depression in a Tertiary Hospital and Associated Factors]. Rev Colomb Psiquiatr. 2016 Oct - Dec;45(4):253-261. | CrossRef | PubMed | Cherry AS, Blucker RT, Thornberry TS, Hetherington C, McCaffree MA, Gillaspy SR. Postpartum depression screening in the Neonatal Intensive Care Unit: program development, implementation, and lessons learned. J Multidiscip Healthc. 2016 Feb 18;9:59-67. | CrossRef | PubMed |
Cherry AS, Blucker RT, Thornberry TS, Hetherington C, McCaffree MA, Gillaspy SR. Postpartum depression screening in the Neonatal Intensive Care Unit: program development, implementation, and lessons learned. J Multidiscip Healthc. 2016 Feb 18;9:59-67. | CrossRef | PubMed | Mendoza B C, Saldivia S. [An update on postpartum depression]. Rev Med Chil. 2015 Jul;143(7):887-94. | CrossRef | PubMed |
Mendoza B C, Saldivia S. [An update on postpartum depression]. Rev Med Chil. 2015 Jul;143(7):887-94. | CrossRef | PubMed | Romero R D, Orozco R LA, Ybarra S JL, Gracia R BI. Sintomatología depresiva en el post parto y factores psicosociales asociados. Rev Chil Obstet Ginecol. 2017;82(2):63-73. | Link |
Romero R D, Orozco R LA, Ybarra S JL, Gracia R BI. Sintomatología depresiva en el post parto y factores psicosociales asociados. Rev Chil Obstet Ginecol. 2017;82(2):63-73. | Link | Casillas IH, Tite PL. Depresión postparto en madres de neonatos hospitalizados en la unidad de cuidados intensivos neonatal (UCIN) y no hospitalizados, en los hospitales un Canto a la Vida y Maternidad Nueva Aurora, un seguimiento desde la etapa gestacional.. Ecuador: Pontificia Universidad Católica del Ecuador. Facultad de Medicina; 2017. | Link |
Casillas IH, Tite PL. Depresión postparto en madres de neonatos hospitalizados en la unidad de cuidados intensivos neonatal (UCIN) y no hospitalizados, en los hospitales un Canto a la Vida y Maternidad Nueva Aurora, un seguimiento desde la etapa gestacional.. Ecuador: Pontificia Universidad Católica del Ecuador. Facultad de Medicina; 2017. | Link | González D, Ballesteros N, Serrano M. Determinantes estresores presentes en madres de neonatos pretérmino hospitalizados en las Unidades de Cuidados Intensivos. Cienc Cuid. 2012;(1)9:43-53. | Link |
González D, Ballesteros N, Serrano M. Determinantes estresores presentes en madres de neonatos pretérmino hospitalizados en las Unidades de Cuidados Intensivos. Cienc Cuid. 2012;(1)9:43-53. | Link | Carvalho AE, Linhares MB, Padovani FH, Martinez FE. Anxiety and depression in mothers of preterm infants and psychological intervention during hospitalization in neonatal ICU. Span J Psychol. 2009 May;12(1):161-70. | PubMed |
Carvalho AE, Linhares MB, Padovani FH, Martinez FE. Anxiety and depression in mothers of preterm infants and psychological intervention during hospitalization in neonatal ICU. Span J Psychol. 2009 May;12(1):161-70. | PubMed | Jadresic ME. Depresión Posparto En El Contexto Del Hospital General. Rev Médica Clínica Las Condes. 2017 [citado 7 de febrero de 2019];28(6):874-80. | Link |
Jadresic ME. Depresión Posparto En El Contexto Del Hospital General. Rev Médica Clínica Las Condes. 2017 [citado 7 de febrero de 2019];28(6):874-80. | Link | Luna Matos ML, Salinas Piélago J, Luna Figueroa A. [Major depression in pregnant women served by the National Materno-Perinatal Institute in Lima, Peru]. Rev Panam Salud Publica. 2009 Oct;26(4):310-4. | PubMed |
Luna Matos ML, Salinas Piélago J, Luna Figueroa A. [Major depression in pregnant women served by the National Materno-Perinatal Institute in Lima, Peru]. Rev Panam Salud Publica. 2009 Oct;26(4):310-4. | PubMed | Romero GE, De la Cruz JA, Lozano J. Relación entre características sociodemográficas y riesgo de depresión postparto en puérperas de la Clínica Good Hope, noviembre de 2015. Perú: Universidad Ricardo Palma. Facultad de Medicina Humana; 2016. | Link |
Romero GE, De la Cruz JA, Lozano J. Relación entre características sociodemográficas y riesgo de depresión postparto en puérperas de la Clínica Good Hope, noviembre de 2015. Perú: Universidad Ricardo Palma. Facultad de Medicina Humana; 2016. | Link | Bustos S, Jiménez N. Factores de riesgo asociados a la depresión postparto en mujeres que asisten a centros de atención primaria en la ciudad de Arica-Chile. Psiquiatría Salud Ment. 2013;30(1):38-49. | Link |
Bustos S, Jiménez N. Factores de riesgo asociados a la depresión postparto en mujeres que asisten a centros de atención primaria en la ciudad de Arica-Chile. Psiquiatría Salud Ment. 2013;30(1):38-49. | Link | Alkozei A, McMahon E, Lahav A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J Matern Fetal Neonatal Med. 2014 Nov;27(17):1738-43. | CrossRef | PubMed |
Alkozei A, McMahon E, Lahav A. Stress levels and depressive symptoms in NICU mothers in the early postpartum period. J Matern Fetal Neonatal Med. 2014 Nov;27(17):1738-43. | CrossRef | PubMed | Montirosso R, Provenzi L, Calciolari G, Borgatti R; NEO-ACQUA Study Group. Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr. 2012 Feb;101(2):136-42. | CrossRef | PubMed |
Montirosso R, Provenzi L, Calciolari G, Borgatti R; NEO-ACQUA Study Group. Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr. 2012 Feb;101(2):136-42. | CrossRef | PubMed | Chourasia N, Surianarayanan P, Bethou A, Bhat V. Stressors of NICU mothers and the effect of counseling-experience from a tertiary care teaching hospital, India. J Matern Fetal Neonatal Med. 2013 Apr;26(6):616-8. | CrossRef | PubMed |
Chourasia N, Surianarayanan P, Bethou A, Bhat V. Stressors of NICU mothers and the effect of counseling-experience from a tertiary care teaching hospital, India. J Matern Fetal Neonatal Med. 2013 Apr;26(6):616-8. | CrossRef | PubMed | Wormald F, Tapia L, Torres G, Gonz A, Rodr D, Escobar M, et al. Estrés en padres de recién nacidos prematuros de muy bajo peso hospitalizados en unidades de cuidados intensivos neonatales. Estudio multicéntrico. Arch Argent Pediatr. 2015;113(4):303-9. | Link |
Wormald F, Tapia L, Torres G, Gonz A, Rodr D, Escobar M, et al. Estrés en padres de recién nacidos prematuros de muy bajo peso hospitalizados en unidades de cuidados intensivos neonatales. Estudio multicéntrico. Arch Argent Pediatr. 2015;113(4):303-9. | Link | Urdaneta J, Rivera A, García J, Guerra M, Baabel N, Contreras A. Factores de riesgo de depresión posparto en puérperas venezolanas valoradas por medio de la escala de Edimburgo. Rev Chil Obstet Ginecol. 2011;76(2):102-12. | Link |
Urdaneta J, Rivera A, García J, Guerra M, Baabel N, Contreras A. Factores de riesgo de depresión posparto en puérperas venezolanas valoradas por medio de la escala de Edimburgo. Rev Chil Obstet Ginecol. 2011;76(2):102-12. | Link | Rincón-Pabón D, Ramírez-Vélez R. Determinantes sociales, cuidado prenatal y depresión posparto: Resultados de la Encuesta Nacional de Salud 2010: Estudio transversal. Progresos Obstet y Ginecol. 2013;56(10):508-14. | CrossRef |
Rincón-Pabón D, Ramírez-Vélez R. Determinantes sociales, cuidado prenatal y depresión posparto: Resultados de la Encuesta Nacional de Salud 2010: Estudio transversal. Progresos Obstet y Ginecol. 2013;56(10):508-14. | CrossRef | Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81(8):609-15. | PubMed |
Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81(8):609-15. | PubMed | Lara A, Navarro C, Navarrete L, Cabrera A, Almanza J, Morales F, et al. Síntomas depresivos en el embarazo y factores asociados, en pacientes de tres instituciones de salud de la ciudad de México. Salud Ment. 2006;29(4):55-62. | Link |
Lara A, Navarro C, Navarrete L, Cabrera A, Almanza J, Morales F, et al. Síntomas depresivos en el embarazo y factores asociados, en pacientes de tres instituciones de salud de la ciudad de México. Salud Ment. 2006;29(4):55-62. | Link | Mafra V, de Nobrega CV, Freitas C, MAtos JM, de Nobrega FJ. Multiprofessional care and mental health in pregnant women. Rev Saude Publica. 2005;39(4):612-8. | Link |
Mafra V, de Nobrega CV, Freitas C, MAtos JM, de Nobrega FJ. Multiprofessional care and mental health in pregnant women. Rev Saude Publica. 2005;39(4):612-8. | Link | Sierra JM, Carro T, Ladrón E. Variables asociadas al riesgo de depresión posparto. Edinburgh Postnatal Depression Scale. Aten Primaria. 2002;30(2):103-11. | CrossRef |
Sierra JM, Carro T, Ladrón E. Variables asociadas al riesgo de depresión posparto. Edinburgh Postnatal Depression Scale. Aten Primaria. 2002;30(2):103-11. | CrossRef | Augusto A, Kumar R, Calheiros JM, Matos E, Figueiredo E. Post-natal depression in an urban area of Portugal: comparison of childbearing women and matched controls. Psychol Med. 1996 Jan;26(1):135-41. | PubMed |
Augusto A, Kumar R, Calheiros JM, Matos E, Figueiredo E. Post-natal depression in an urban area of Portugal: comparison of childbearing women and matched controls. Psychol Med. 1996 Jan;26(1):135-41. | PubMed | Taherifard P, Delpisheh A, Shirali R, Afkhamzadeh A, Veisani Y. Socioeconomic, psychiatric and materiality determinants and risk of postpartum depression in border city of ilam, Western iran. Depress Res Treat. 2013;2013:653471. | CrossRef | PubMed |
Taherifard P, Delpisheh A, Shirali R, Afkhamzadeh A, Veisani Y. Socioeconomic, psychiatric and materiality determinants and risk of postpartum depression in border city of ilam, Western iran. Depress Res Treat. 2013;2013:653471. | CrossRef | PubMed | Moreno A, Domínguez L, França PS. Depresión postparto: prevalencia de test de rastreo positivo en puérperas del Hospital Universitario de Brasilia, Brasil. Rev Chil Obstet Ginecol. 2004;69(3):209-213. | CrossRef |
Moreno A, Domínguez L, França PS. Depresión postparto: prevalencia de test de rastreo positivo en puérperas del Hospital Universitario de Brasilia, Brasil. Rev Chil Obstet Ginecol. 2004;69(3):209-213. | CrossRef | Almeida AB, Toscano DF. Prevalencia de depresión postparto en madres hospitalizadas en el servicio de adolescencia del Hospital Gineco Obstétrico Maternidad Isidro Ayora en el primer trimestre del año 2013. Ecuador: Pontificia Universidad Católica del Ecuador. Facultad de Medicina; 2013. | Link |
Almeida AB, Toscano DF. Prevalencia de depresión postparto en madres hospitalizadas en el servicio de adolescencia del Hospital Gineco Obstétrico Maternidad Isidro Ayora en el primer trimestre del año 2013. Ecuador: Pontificia Universidad Católica del Ecuador. Facultad de Medicina; 2013. | Link | Csatordai S, Kozinszky Z, Devosa I, Tóth E, Krajcsi A, Sefcsik T, Pál A. Obstetric and sociodemographic risk of vulnerability to postnatal depression. Patient Educ Couns. 2007 Jul;67(1-2):84-92. | PubMed |
Csatordai S, Kozinszky Z, Devosa I, Tóth E, Krajcsi A, Sefcsik T, Pál A. Obstetric and sociodemographic risk of vulnerability to postnatal depression. Patient Educ Couns. 2007 Jul;67(1-2):84-92. | PubMed |