 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: physical therapy specialty, physical therapy department, hospital, critical care, organization and administration, hospital rapid response team, workload
Introduction
The European Society of Intensive Care Medicine recommends the presence of a specialist physiotherapist, available every five beds, seven days a week in the high complexity Intensive Care Unit. However, in Chile the adherence of adult Intensive Care Units to this recommendation is unknown.
Objective
To describe the organizational characteristics and the physiotherapist availability in adult Intensive Care Units in Chile, and according to the adherence to international recommendations, inform health decision-makers.
Methods
Observational study based on a telephone survey. All adult Intensive Care Units institutions of high complexity, private hospitals and teaching health centers in Chile were eligible (n = 74). The primary outcome measures were the proportion of institutions with physiotherapist availability 24 hours a day and seven days a week (24/7 physiotherapist), a maximum caseload per physiotherapist of five patients and the presence of a specialist physiotherapist.
Results
Response rate was 86.5%, with 59% of responding units being public and 83% offering level III care. 70% of the adult Intensive Care Units in Chile have 24/7 physiotherapist (87% of the public and 46% of the private sector). 41% of the centers had a maximum caseload per physiotherapist of five patients during the day on weekdays. This number decreased on weekends and during night shifts. 23% of the Intensive Care Units had a specialist physiotherapist, being more common in the private sector (31%).
Conclusions
In Chilean adult ICU, 24/7 physiotherapist availability is high, the prevalence of physiotherapists with specialist training is low. Future efforts should focus on promoting the uptake of specialist training.
|
Key ideas
|
Patients with a reversible medical condition affecting one or more systems, that puts their life at severe risk, need special treatment in units that can monitor, surveil and provide the advanced vital support necessary to ensure patient recovery[1] In Chile in medical institutions of greater complexity, the care for those patients is organized in Critical Patient Units which provide intensive care for critically ill patients (Intensive Care Unit) and step-down facilities (High Dependency Unit)[1],[2]. The Intensive Care Unit is intended to provide permanent and timely care to unstable, critical patients; while stable patients are admitted to the High Dependency Unit for non-invasive monitoring, surveillance and continuous management[1],[3]. These units are classified according to their level of care. Level I (low) takes care of patients with organ dysfunction that requires continuous monitoring, and a minor need for pharmaceuticals and medical devices. Level II (medium) is intended for patients requiring higher pharmaceutical support and a greater need for medical devices in case of acute organ or system failure. Level III (high) units admit patients at risk or with two or more organs failing and those who require hemodynamic, renal or respiratory support[4],[5].
In 2011, the European Society of Intensive Care Medicine issue a guideline with the basic requirements for Intensive Care Units. It recommended that level III units (high complexity) should be staffed with one specialist physiotherapist every five beds, seven days a week[4]. This patient: staff ratio should allow delivering efficient and cost-effective care. Evidence suggests that early rehabilitation in the Intensive Care Units can improve patient quality of life, physical function and muscular strength[6]. It can also decrease the number of days of respiratory support, the length of stay in hospital, mortality of adult patients in the Intensive Care Unit[6],[7],[8],[9],[10],[11],[12]. In Chile, the Chilean Society of Intensive Medicine recommends having a physiotherapist available 24 hours a day in Intensive Care Units without referring to a safe staffing level[3].
As a standard of care, the Chilean Ministry of Health recommends having four physiotherapists in a rotation system for continuous coverage, assuming a caseload of six patients in the adult Intensive Care Unit per physiotherapist. However, this recommendation seeks to standardize the number of beds available depending on the level of care required, without being enforceable[1]. The Chilean Society of Intensive Medicine recommends, as the European Society of Intensive Care Medicine does, that physiotherapists should have the capabilities for and be licensed to care for patients in the intensive care environment. Moreover, physiotherapists should undergo continuous training in respiratory care, neurological care, respiratory support, and respiratory therapy, with a minimum of one year of certified experience in these areas[3].
This study aims to describe the organizational characteristics and the physiotherapist availability in adult Intensive Care Units at a national level in Chile, and according to the adherence to international recommendations. This will provide key stakeholders in the private and public sectors with objective, high-quality information for decision-making.
Study design
This observational analytic cross-sectional study is based on a telephone survey. Adult Intensive Care Units, were the unit of analysis, identified through the website of the Chilean Ministry of Health. All units were contacted telephonically, verbal consent was sought, and a physiotherapist representative of the adult Intensive Care Unit responded a 40-minute survey to describe the organizational characteristics and the physiotherapist availability in adult Intensive Care Units, which consisted in 26 questions that included multiple choice, open-ended and Likert scale questions (Supplementary Material 1).
Sample
Of 3 028 health institutions in Chile, 74 were found to be eligible. All adult Intensive Care Units from institutions of greater complexity, private hospitals and university-associated health centers with adult Intensive Care Units that functioned independently of the High Dependency Unit were considered for inclusion in the study. Institutions with units treating patients with lower severity (i.e. High Dependency Unit only) were excluded.
Protocol
In July 2016, the registry of health institutions available at the Ministry of Health’s webpage (http://www.deis.cl/estadisticas-recursossalud/) was retrieved. The institutions of higher complexity belonging to the National Health Services System that contained an adult Intensive Care Unit were selected. It was also included private hospitals and clinical centers associated with state and private universities not belonging to the National Health Services System.
Recruitment took place in the following steps: (i) Initial telephone contact was made inviting an Intensive Care Unit physiotherapist to participate in the study, during which an e-mail address was requested for sending the informed consent form and other information useful for answering the survey as number of beds, level of complexity of the Intensive Care Unit, number of physiotherapists per working hours and shift system, and number of specialist physiotherapists in the unit. A date to administer the survey was also arranged; (ii) A second call was made two days before the selected date to answer any queries regarding the consent and confirm the date of the survey; (iii) a third call was made for the completion of the survey. All the contacts for the data collection process took place between October 4, 2016, and February 23, 2017. The survey was based on the tool developed by Skinner and cols in 2008[13] in Australia, and the recommendations of physiotherapy interventions published by European Society of Intensive Care Medicine the same year[14]. To improve the face and construct validity of the survey, a group of experts (clinicians and epidemiologists) and pollsters from the area of physical therapy (i.e. undergraduate and postgraduate students) assessed a previous version of the instrument. A pilot study that included three centers was also conducted to ensure adequate comprehension and to improve the quality of the questions. To improve the precision of the survey, administrative information was requested in advance (level of Intensive Care Unit complexity, number of physiotherapists available per working hours and shift system, and the number of specialists) to give time to the respondents to collect these data.
Study variables
The characteristics of the included Intensive Care Units are described according to location, type of administration, the number of beds, the level of complexity of the Intensive Care Unit, and the most common medical conditions treated in these units.
The organizational characteristics of physiotherapist availability in the Intensive Care Unit are: the number of physiotherapists per working hours and shift system, technical-administrative unit, contractual system, caseload per physiotherapist, physiotherapist availability 24 hours a day and seven days a week (24/7 physiotherapist), and the number of specialist physiotherapists in the unit. The definition of each variable measured is described in the Table 1.
Table 1. Information collected with the national survey and its definition.
Data analysis
The categorical variables are presented in absolute and relative frequency; while the numerical variables; number of beds, physiotherapists per work shift and caseload per physiotherapist according to work shift are presented as median and interquartile range (P25-P75), given that they exhibited a non-parametric distribution (i.e. p-value of Shapiro Wilk distribution test < 0.05). The number of specialist physiotherapists is presented as minimum-maximum. The statistical package Stata/SE 13.0 was used for the data analyses.
Ethical review board
The current study was approved by the Scientific Ethics Committee of the Faculty of Medicine at the Clínica Alemana Universidad del Desarrollo (2016-35/2018-29) in Santiago, Chile. Participant consent was verbally given during the third phone call, before beginning the survey. This study adheres to the STROBE declaration.
The response rate obtained was 86.5% (n = 64). Five institutions rejected participation, and another five institutions could not be reached (Figure 1).
Figure 1. Flowchart of adult Intensive Care Units in Chile.
A minimum of one and a maximum of three calls were required to complete the survey, with a median time (P25-P75) of 40 (36-45) minutes per institution. Public institutions were 59% (n = 38) of the sample and 41% (n = 26) were located in the Metropolitan Region. The health institutions reported a median (P25-P75) of eight (6-14) Intensive Care Unit beds and mainly treated patients with medical, neurological or cardiological conditions. 83% of the units surveyed are high complexity (level III) (Table 2).
Physiotherapist availability in Intensive Care Units is achieved by the 44-hour weekly system (41%) and fourth shift system (58%), with the latter being the dominant system in public units (84%). In those institutions using another rotation system, 43% (n = 9) had availability between 11-36 weekly hours, 14% (n = 3) had 11 hours, 24% (n = 5) used bank staff and 19% (n = 4) used a system based on unit necessity.
The technical-administrative unit for physiotherapists in public institutions corresponded to the Critical Patient Unit (60%); while in private centers physiotherapists mainly belonged to the Physical Medicine, Rehabilitation or Physical Therapy Service (61.5%). In both public and private Intensive Care Units, the most common contractual system was the use of a contract (89% nationally). A median (P25-P75) of one (1-2) physiotherapist available during night and weekend shifts was found. The median (P25-P75) caseload per physiotherapist during weekdays varied between six (5-8) and five (3-6) patients in public and private institutions, respectively, with higher numbers found during night shifts. Concerning professional training, respondents reported a maximum of two and four specialist physiotherapists in public and private Intensive Care Units, respectively (Table 3).
Regarding the adherence to international recommendations, 70% (n = 45) of the adult Intensive Care Units surveyed had 24/7 physiotherapist availability; from which 47% were located within the Metropolitan Region, and 73% were publically administered. Units that do not have 24/7 physiotherapist availability were more likely to be located outside of the metropolitan region (74%) and be private centers (74%). In 41% of the institutions, a maximum of 5 patients per physiotherapist during the day shift on weekdays was observed, decreasing on weekends and during night shifts. Physiotherapists with specialized training in intensive care were present in 23% of the Intensive Care Units, with the largest concentration found in the private sector (31%) (Table 3). Only one center adheres to all three criteria of the international recommendations of physiotherapist availability in adult Intensive Care Units.
There was a greater number of beds in the unit when the Intensive Care Unit accomplish with 24/7 physiotherapist availability and when they do not accomplish with the maximum of five patients per physiotherapist. There were more units that complies with 24/7 physiotherapist availability when the physiotherapists belong to the Intensive Care Unit vs the physical therapy service. Level III of complexity of the Intensive Care Unit is more prevalent in units that complies with 24/7 physiotherapist availability (Table 4).
In Chile, 70% of high-complexity intensive care units had a physiotherapist available 24 hours seven days, 41% meets the standard of five patients per physiotherapists during day shifts on weekdays and 23% had at least one physiotherapist specialized in Intensive Care Unit treatment. High uncertainty remains whether this provision is enough to ensure safe and cost-effective delivery of physiotherapy services in our hospitals.
Evidence suggests that is not clear whether physiotherapy 24/7 in intensive care unit improves patients’ outcomes. Merino-Osorio et al (2018) conducted a systematic review analyzing the effect 24/7 availability of chest physiotherapy on healthcare-associated infections, length of stay and mortality, finding no difference compared with physiotherapy during business hours only[15]. In the case of additional rehabilitation services during the weekend in Intensive Care Unit, there is insufficient evidence to make a judgement. However, Haines et al (2018) suggest that additional weekend allied health services reduce the length of stay in subacute rehabilitation settings16. In acute general medical and surgical wards is not clear if these additional services are effective or cost-effective[16],[17]. Despite the conflicting evidence, standards for intensive care units recommend the presence of a physiotherapist 24 hours[4],[18]. These standards are based on the premise that increasing availability should increase the volume (length, frequency, and/or intensity) of early rehabilitation provided in Intensive Care Units, but again, it is not clear if more intensive or earlier rehabilitation yields better patients’ outcomes[19],[20] in the long-term.
The case for safe staffing levels relies on the premise that care can be delivered more safely and cost-effectively with a given amount of staff. In reality, the mix and number of staff members needed depend on the complexity of patients, skills mix available, role development in the longer term, team working, integration of services, and the service delivery model[21]. The standard of five patients per physiotherapist is just indicative and it is not based on strong evidence[22], since the literature on staffing levels for allied health professions is less developed (in quantity and quality) than that for nurses and physicians[23]. Johnson et al (2017) suggest that increasing staffing levels in a cardiovascular Intensive Care Unit improved marginally the duration of each rehabilitation session with significant improvements in length of stay in Intensive Care Unit and hospital. Nonetheless, no impact on mobility or level of care required after discharge were detected20. This suggests that our effort should focus not only on increasing availability of physiotherapy services but in improving multidisciplinary work and the type of activities physiotherapist perform with patients in the Intensive Care Unit. Evidence from one-day point prevalence studies of mobility practices in Australia, New Zealand and Germany suggest that physiotherapists performed active mobilization between 45%[24],[25] and 81% of occasions[26]. These findings question how intensive rehabilitation sessions are and how long patients spend in bed resting in a regular day in the Intensive Care Unit. Observational studies of actual practice suggest that patient in the Intensive Care Unit spend between seven and 11 hours in bed[27],[28], and, outside rehabilitation, patients rarely got involved in ambulation activities[27].
Availability of physiotherapists in the night are reported between 0% and 79% in public hospitals, with Greece, Germany, Portugal and Sweden having the lowest availability[29],[30]; however, this information is more than 20 years old. Availability in the weekends raged from 21 % in Greece[29] and 97% in Canada[31]. Our results put Chile in an intermediate position regarding out-of-hours availability. The next step would be to determine the relationship between the staffing ratios reported and long-term patients’ outcomes accounting for the size of the Intensive Care Unit, team working, level of activity achieved during rehabilitation sessions, active time in the Intensive Care Unit and availability of other allied health professionals in the unit. This would provide information into the best way to plan our workforce in an individual center and nationally.
Staff skills mix and administrative dependency are two other factors that should be considered when planning staffing levels. Although nurses and doctors staffing levels are associated with lower mortality rates[32], it is not clear what skills mix combination yields better results[18],[33]. The skills mix has to enable delivering safe care that is efficient while allowing professional development according to seniority[33]. We found that 23% of centers had at least one physiotherapist with specialist training. Although it is not clear from the literature what the ideal skills mix is for physiotherapists, our findings suggest that a high proportion of our physiotherapists working in Intensive Care Units might lack the training to treat critically ill patients. The American College of Critical Care Medicine recommends that a respiratory therapist be present 24 hours a day in level III Intensive Care Units[34]; while the Chilean Society of Intensive Medicine recommends that physiotherapists have accredited training in intensive care physical therapy and complete at least one training activity annually[3]. This is an area where future efforts should be directed to ensure the delivery of safe care.
In terms of administrative dependence, we found that in 60% of public centers physiotherapists belonged to the Critical Patient Unit, while in private centers 61.5% belonged to the Physical Medicine and Rehabilitation Service. In Canada, 42% of tertiary care hospitals reported a centrally organized physiotherapy department that serviced the entire hospital, while a departmental organization of services was used in 17% of hospitals[31]. Specialized Intensive Care Unit physiotherapists in trauma units report that a departmental organization favors a more equitable distribution of professionals throughout the hospital, allowing for a greater quantity of sessions per patient[35]. Fisher et al (2012) also note that dependence on the Physical Medicine and Rehabilitation Service would be a feasible alternative for optimizing the use of human resources[35]. This suggests that in practice several models for organizing the delivery of physiotherapy services exist. However, it is unclear whether one is superior to the others in terms of efficiency, safety, patient’s satisfaction, and clinical outcomes.
The intensive care units that have 24/7 physiotherapist present a higher median of beds per unit, that could be translated as a possible overload of personnel. This could be reflected when considering the number of physiotherapists, where there is a difference in the proportion of patients per professional among intensive care units that comply and do not comply with this recommendation. In relation to the level of complexity of the units, there are similar between the centers that comply or not with each recommendation, which would be explained because the most prevalent complexity in Chilean intensive care units corresponding to level III.
On the other hand, the difference observed in the accomplishment with the recommendation of physiotherapist 24 hours a day, 7 days a week, could only guide us towards future studies that inquire about the possible strategies that the Critical Patients Units, with their technical and administrative faculties, could be performing in order to comply with this recommendation. The presence of physiotherapist specialist does not differ in any case; however, it is evidenced there is a need for specialized physiotherapists in intensive care evidenced.
The reporting bias that involves the extraction of information through a telephone survey, and not face-to-face, constitutes a possible limitation of this study; although the quality control of the database was carried out and the biological plausibility of the results was determined. Additionally, our results were similar to those observed in studies that possessed lower response rates – such as in Europe[30] - and in which cases an overestimation of the results could be possible due to the interest of the participating institutions. This non-differential bias was controlled as the results of the primary outcomes were confirmed through a process of response triangulation in which all of the centers that reported to have physiotherapist 24/7 also reported having a physiotherapist on weekends and during nights, and as public and private centers reported similar results. Although, the survey was carried out by only one representative-physiotherapist per ICU, the response bias was controlled; since the questions asked were objective, that is, limiting the fact that the answer refers to a different vision to the real practice. The response rate of 86.5% of the adult Intensive Care Units in Chile, conforms a strength of our study, as it is a much higher response rate than those obtained in studies conducted in Canada (84%)[31], Greece (68.7%)[29], and Europe (22%)[30], and establishes a useful and representative information base of adult Intensive Care Units at a national level; exposing a reality that could be generalized to all the health centers in the country. In addition, of the total of units that were not included in the study, half corresponded to public centers and their remaining proportion to private centers; as well as its location, being located half within the Metropolitan Region and the other half outside the national capital.
One of the weaknesses of our study is that we do not have information about the activities that physiotherapists perform on a daily basis, preventing us from drawing conclusions regarding the adequacy of the current staffing levels. Future research in our country should focus on examining the effect of different staffing levels and service delivery models on patient’s outcomes.
In Chile, 24/7 physiotherapist availability in adult ICU is high, with the highest deficit of coverage in the private sector. Prevalence of physiotherapists with specialist training is low in public and the private sector; therefore, incentivizing the uptake and creating of this type of training could be pivotal to improve the delivery of rehabilitation and respiratory therapy services in the adult Intensive Care Unit. Our findings are relevant for health professionals, decision- and policy-makers working on staffing policies and planning of the workforce according to the needs of their catchment population. Future research should focus on the relationship between administrative organization, staffing levels and skills mix with patients’ outcomes. Economic evaluations assessing the impact of increasing staffing levels in the Intensive Care Unit should be conducted to guide the management of human resources at a national level.
Author’s contributor role
NA: Conceptualization, Methodology, Formal Analysis, Investigation, Resources, Data Curation, Writing – Original Draft Preparation, Writing – Review & Editing. JM: Conceptualization, Investigation, Resources, Writing – Review & Editing, Funding Acquisition. JP: Conceptualization, Methodology, Software, Validation, Formal Analysis, Investigation, Resources, Data Curation, Writing – Original Draft Preparation, Writing – Review & Editing, Project Administration, Funding Acquisition. ACCA: Conceptualization, Methodology, Resources, Writing – Original Draft Preparation, Writing – Review & Editing, Funding Acquisition. CF: Conceptualization, Resources, Writing – Review & Editing. CMO: Conceptualization, Methodology, Software, Validation, Formal Analysis, Investigation, Resources, Data Curation, Writing – Original Draft Preparation, Writing – Review & Editing, Visualization, Supervision, Project Administration, Funding Acquisition.
Acknowledgements
The University of York provided the infrastructure, time and access to scien-tific repositories for the author ACCA to develop the work.
Competing interests
The authors have completed the declaration form of conflicts of interest of the ICMJE, and declare not having received financing for the completion of the article; do not have financial relationships with organizations that could have interests in the published article; and not have other relationships or activities that could Influence the published article. The forms can be requested by contacting the responsible author or the editorial direction of the Journal.
Funding
This research did not receive any specific grants from funding agencies in the public, commercial, or non-profit sectors.
Ethical approval
This study was approved by the Scientific Ethics Committee of the Medical Staff at the Clínica Alemana Universidad del Desarrollo in Santiago, Chile (approval certificate 2016-35/2018-29). Participants verbally consented to participate voluntarily and immediately proceed to respond to the survey, a procedure that was made explicit in the informed consent documentation.
From the editor
This article was submitted in English. The journal has not copyedited this version.

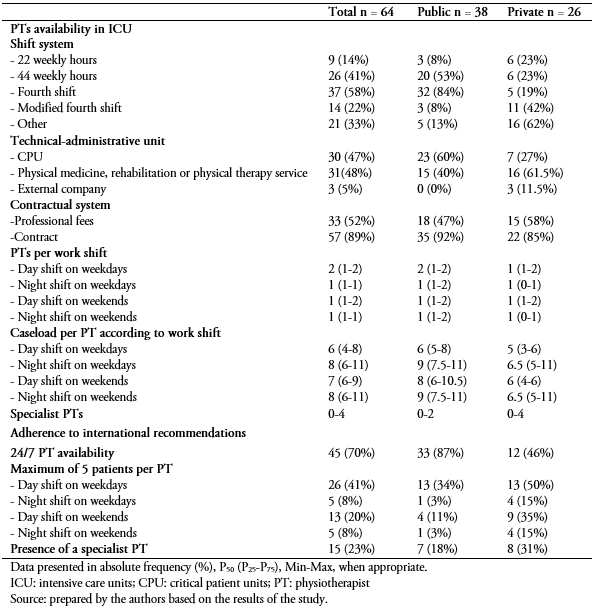 Table 1. Information collected with the national survey and its definition.
Table 1. Information collected with the national survey and its definition.

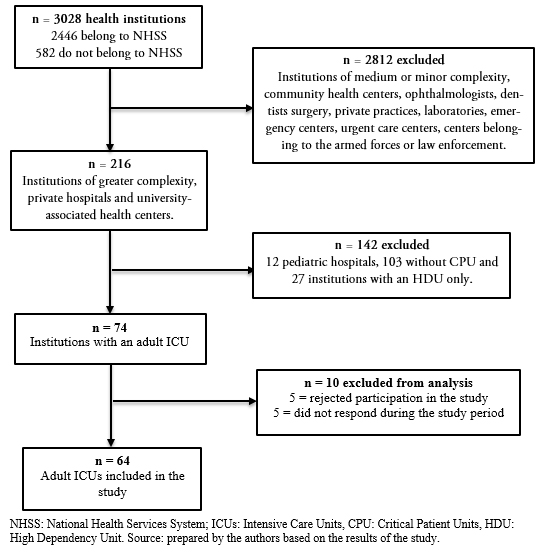 Figure 1. Flowchart of adult Intensive Care Units in Chile.
Figure 1. Flowchart of adult Intensive Care Units in Chile.

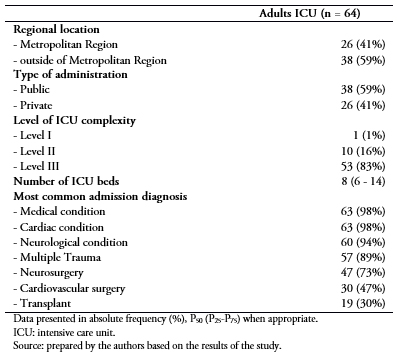 Table 2. Administrative characteristics of adult Intensive Care Units included in the study (n = 64).
Table 2. Administrative characteristics of adult Intensive Care Units included in the study (n = 64).

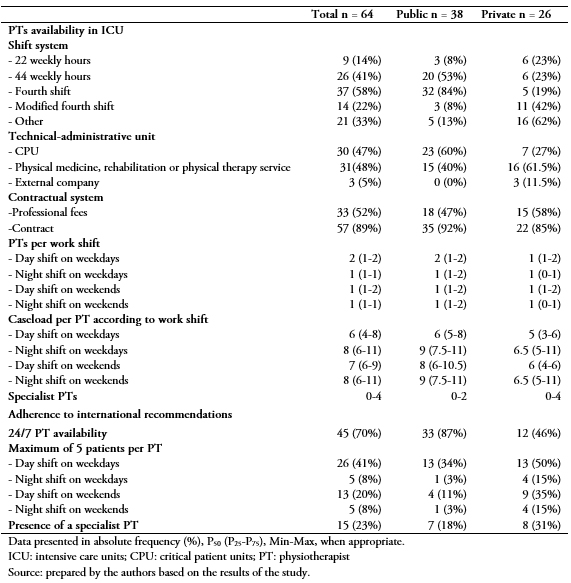 Table 3. Characteristics of physiotherapist availability and proportion of institution adhering to international recommendations in Chilean adult Intensive Care Units according to the type of administration.
Table 3. Characteristics of physiotherapist availability and proportion of institution adhering to international recommendations in Chilean adult Intensive Care Units according to the type of administration.

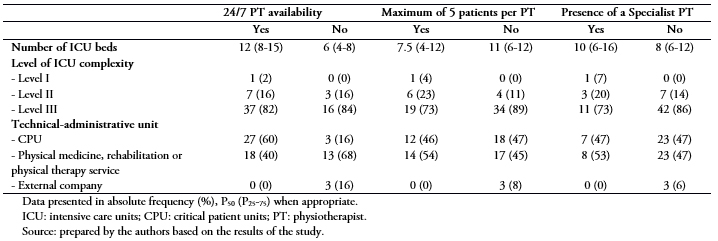 Table 4. Description of the number of beds, level of complexity and technical-administrative unit according to the adherence to international recommen-dations in adult Intensive Care Units (n = 64).
Table 4. Description of the number of beds, level of complexity and technical-administrative unit according to the adherence to international recommen-dations in adult Intensive Care Units (n = 64).
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introduction
The European Society of Intensive Care Medicine recommends the presence of a specialist physiotherapist, available every five beds, seven days a week in the high complexity Intensive Care Unit. However, in Chile the adherence of adult Intensive Care Units to this recommendation is unknown.
Objective
To describe the organizational characteristics and the physiotherapist availability in adult Intensive Care Units in Chile, and according to the adherence to international recommendations, inform health decision-makers.
Methods
Observational study based on a telephone survey. All adult Intensive Care Units institutions of high complexity, private hospitals and teaching health centers in Chile were eligible (n = 74). The primary outcome measures were the proportion of institutions with physiotherapist availability 24 hours a day and seven days a week (24/7 physiotherapist), a maximum caseload per physiotherapist of five patients and the presence of a specialist physiotherapist.
Results
Response rate was 86.5%, with 59% of responding units being public and 83% offering level III care. 70% of the adult Intensive Care Units in Chile have 24/7 physiotherapist (87% of the public and 46% of the private sector). 41% of the centers had a maximum caseload per physiotherapist of five patients during the day on weekdays. This number decreased on weekends and during night shifts. 23% of the Intensive Care Units had a specialist physiotherapist, being more common in the private sector (31%).
Conclusions
In Chilean adult ICU, 24/7 physiotherapist availability is high, the prevalence of physiotherapists with specialist training is low. Future efforts should focus on promoting the uptake of specialist training.
 Authors:
Nadine Aranis[1], Jorge Molina[2], Jaime Leppe[2], Ana Cristina Castro-Ávila[2,3], Carolina Fu[4], Catalina Merino-Osorio[2]
Authors:
Nadine Aranis[1], Jorge Molina[2], Jaime Leppe[2], Ana Cristina Castro-Ávila[2,3], Carolina Fu[4], Catalina Merino-Osorio[2]

Citación: Aranis N, Molina J, Leppe J, Castro-Ávila AC, Fu C, Merino-Osorio C. Characteristics of physiotherapy staffing levels and caseload: a cross-sectional survey of Chilean adult Intensive Care Units. Medwave 2019;19(1):e7576 doi: 10.5867/medwave.2019.01.7576
Fecha de envío: 6/11/2018
Fecha de aceptación: 21/1/2019
Fecha de publicación: 26/2/2019
Origen: not commissioned
Tipo de revisión: external peer review by three external, double-blind reviewers

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Gobierno de Chile, Ministerio de Salud, Subsecretaría de Redes Asistenciales M. Nivel de Complejidad en Atención Cerrada. Santiago, Chile: MINSAL; 2012.
Gobierno de Chile, Ministerio de Salud, Subsecretaría de Redes Asistenciales M. Nivel de Complejidad en Atención Cerrada. Santiago, Chile: MINSAL; 2012.  Gobierno de Chile, Ministerio de Salud. Criterios clasificación según nivel de complejidad de establecimientos hospitalarios; 2013 [on line]. | Link |
Gobierno de Chile, Ministerio de Salud. Criterios clasificación según nivel de complejidad de establecimientos hospitalarios; 2013 [on line]. | Link | Saez E. Guías 2004 de organización y funcionamiento de unidades de pacientes críticos. Rev Chil Med Intensiva. 2004;19(4):209-23. | Link |
Saez E. Guías 2004 de organización y funcionamiento de unidades de pacientes críticos. Rev Chil Med Intensiva. 2004;19(4):209-23. | Link | Valentin A, Ferdinande P; ESICM Working Group on Quality Improvement. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. 2011 Oct;37(10):1575-87. | CrossRef | PubMed |
Valentin A, Ferdinande P; ESICM Working Group on Quality Improvement. Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. 2011 Oct;37(10):1575-87. | CrossRef | PubMed | Danbury C, Gould T, Baudouin S, Berry A, Bolton S, Borthwick M, et al. Guidelines for Provision of Intensive Care Services. Intensive Care Society; 2015. [on line]. | Link |
Danbury C, Gould T, Baudouin S, Berry A, Bolton S, Borthwick M, et al. Guidelines for Provision of Intensive Care Services. Intensive Care Society; 2015. [on line]. | Link | Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013 Jun;41(6):1543-54. | CrossRef | PubMed |
Kayambu G, Boots R, Paratz J. Physical therapy for the critically ill in the ICU: a systematic review and meta-analysis. Crit Care Med. 2013 Jun;41(6):1543-54. | CrossRef | PubMed | Castro AA, Calil SR, Freitas SA, Oliveira AB, Porto EF. Chest physiotherapy effectiveness to reduce hospitalization and mechanical ventilation length of stay, pulmonary infection rate and mortality in ICU patients. Respir Med. 2013 Jan;107(1):68-74. | CrossRef | PubMed |
Castro AA, Calil SR, Freitas SA, Oliveira AB, Porto EF. Chest physiotherapy effectiveness to reduce hospitalization and mechanical ventilation length of stay, pulmonary infection rate and mortality in ICU patients. Respir Med. 2013 Jan;107(1):68-74. | CrossRef | PubMed | Adler J, Malone D. Early mobilization in the intensive care unit: a systematic review. Cardiopulm Phys Ther J. 2012 Mar;23(1):5-13. | PubMed |
Adler J, Malone D. Early mobilization in the intensive care unit: a systematic review. Cardiopulm Phys Ther J. 2012 Mar;23(1):5-13. | PubMed | Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011 Apr 7;364(14):1293-304. | CrossRef | PubMed |
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011 Apr 7;364(14):1293-304. | CrossRef | PubMed | Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003 Feb 20;348(8):683-93. | CrossRef | PubMed |
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003 Feb 20;348(8):683-93. | CrossRef | PubMed | Calvo-Ayala E, Khan BA, Farber MO, Ely EW, Boustani MA. Interventions to improve the physical function of ICU survivors: a systematic review. Chest. 2013 Nov;144 (5):1469-1480. | CrossRef | PubMed |
Calvo-Ayala E, Khan BA, Farber MO, Ely EW, Boustani MA. Interventions to improve the physical function of ICU survivors: a systematic review. Chest. 2013 Nov;144 (5):1469-1480. | CrossRef | PubMed | Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of Early Rehabilitation during Intensive Care Unit Stay on Functional Status: Systematic Review and Meta-Analysis. PLoS One. 2015 Jul 1;10(7):e0130722. | CrossRef | PubMed |
Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of Early Rehabilitation during Intensive Care Unit Stay on Functional Status: Systematic Review and Meta-Analysis. PLoS One. 2015 Jul 1;10(7):e0130722. | CrossRef | PubMed | Skinner EH, Berney S, Warrillow S, Denehy L. Rehabilitation and exercise prescription in Australian intensive care units. Physiotherapy. 2008 Sep;94(3):220-9. | CrossRef |
Skinner EH, Berney S, Warrillow S, Denehy L. Rehabilitation and exercise prescription in Australian intensive care units. Physiotherapy. 2008 Sep;94(3):220-9. | CrossRef | Gosselink R, Bott J, Johnson M, Dean E, Nava S, Norrenberg M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008 Jul;34(7):1188-99. | CrossRef | PubMed |
Gosselink R, Bott J, Johnson M, Dean E, Nava S, Norrenberg M, et al. Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med. 2008 Jul;34(7):1188-99. | CrossRef | PubMed | Merino-Osorio C, Castro-Ávila AC, Arias-Gutiérrez R, Arriagada MJ, Villanueva C, Leppe J, et al. Effects of 24-hours/day versus business hours physical therapy intervention in adult intensive care unit patients: a systematic review. Int Phys Med Rehabil J. 2018;3(1):100-6. | CrossRef |
Merino-Osorio C, Castro-Ávila AC, Arias-Gutiérrez R, Arriagada MJ, Villanueva C, Leppe J, et al. Effects of 24-hours/day versus business hours physical therapy intervention in adult intensive care unit patients: a systematic review. Int Phys Med Rehabil J. 2018;3(1):100-6. | CrossRef | Haines TP, Bowles KA, Mitchell D, O'Brien L, Markham D, Plumb S, et al. Impact of disinvestment from weekend allied health services across acute medical and surgical wards: 2 stepped-wedge cluster randomised controlled trials. PLoS Med. 2017 Oct 31;14(10):e1002412. | CrossRef | PubMed |
Haines TP, Bowles KA, Mitchell D, O'Brien L, Markham D, Plumb S, et al. Impact of disinvestment from weekend allied health services across acute medical and surgical wards: 2 stepped-wedge cluster randomised controlled trials. PLoS Med. 2017 Oct 31;14(10):e1002412. | CrossRef | PubMed | Mills E, Hume V, Stiller K. Increased allied health services to general and acute medical units decreases length of stay: comparison with a historical cohort. Aust Health Rev. 2018 Jun;42(3):327-333. | CrossRef | PubMed |
Mills E, Hume V, Stiller K. Increased allied health services to general and acute medical units decreases length of stay: comparison with a historical cohort. Aust Health Rev. 2018 Jun;42(3):327-333. | CrossRef | PubMed | Intensive Care Society. Core Standards for Intensive Care Units. Core Stand Intensive Care Units. 2013;1:1-27. | Link |
Intensive Care Society. Core Standards for Intensive Care Units. Core Stand Intensive Care Units. 2013;1:1-27. | Link | Wright SE, Thomas K, Watson G, Baker C, Bryant A, Chadwick TJ, et al. Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): a multicentre, parallel-group, randomised controlled trial. Thorax. 2018 Mar;73(3):213-221. | CrossRef | PubMed |
Wright SE, Thomas K, Watson G, Baker C, Bryant A, Chadwick TJ, et al. Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): a multicentre, parallel-group, randomised controlled trial. Thorax. 2018 Mar;73(3):213-221. | CrossRef | PubMed | Johnson AM, Henning AN, Morris PE, Tezanos AGV, Dupont-Versteegden EE. Timing and Amount of Physical Therapy Treatment are Associated with Length of Stay in the Cardiothoracic ICU. Sci Rep. 2017 Dec 14;7(1):17591. | CrossRef | PubMed |
Johnson AM, Henning AN, Morris PE, Tezanos AGV, Dupont-Versteegden EE. Timing and Amount of Physical Therapy Treatment are Associated with Length of Stay in the Cardiothoracic ICU. Sci Rep. 2017 Dec 14;7(1):17591. | CrossRef | PubMed | Stone SA. Staffing levels: give us a tool for optimum staffing levels. 2018. csp.org.uk [on line]. | Link |
Stone SA. Staffing levels: give us a tool for optimum staffing levels. 2018. csp.org.uk [on line]. | Link | Cartmill L, Comans TA, Clark MJ, Ash S, Sheppard L. Using staffing ratios for workforce planning: Evidence on nine allied health professions. Hum Resour Health. 2012;10:1-8. | Link |
Cartmill L, Comans TA, Clark MJ, Ash S, Sheppard L. Using staffing ratios for workforce planning: Evidence on nine allied health professions. Hum Resour Health. 2012;10:1-8. | Link | Skinner EH, Haines KJ, Berney S, Warrillow S, Harrold M, Denehy L. Usual Care Physiotherapy During Acute Hospitalization in Subjects Admitted to the ICU: An Observational Cohort Study. Respir Care. 2015 Oct;60(10):1476-85. | CrossRef | PubMed |
Skinner EH, Haines KJ, Berney S, Warrillow S, Harrold M, Denehy L. Usual Care Physiotherapy During Acute Hospitalization in Subjects Admitted to the ICU: An Observational Cohort Study. Respir Care. 2015 Oct;60(10):1476-85. | CrossRef | PubMed | Nydahl P, Ruhl AP, Bartoszek G, Dubb R, Filipovic S, Flohr HJ, et al. Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med. 2014 May;42(5):1178-86. | CrossRef | PubMed |
Nydahl P, Ruhl AP, Bartoszek G, Dubb R, Filipovic S, Flohr HJ, et al. Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med. 2014 May;42(5):1178-86. | CrossRef | PubMed | Berney SC, Harrold M, Webb SA, Seppelt I, Patman S, Thomas PJ, et al. Intensive care unit mobility practices in Australia and New Zealand: a point prevalence study. Crit Care Resusc. 2013 Dec;15(4):260-5. | PubMed |
Berney SC, Harrold M, Webb SA, Seppelt I, Patman S, Thomas PJ, et al. Intensive care unit mobility practices in Australia and New Zealand: a point prevalence study. Crit Care Resusc. 2013 Dec;15(4):260-5. | PubMed | Berney SC, Rose JW, Bernhardt J, Denehy L. Prospective observation of physical activity in critically ill patients who were intubated for more than 48 hours. J Crit Care. 2015 Aug;30(4):658-63. | CrossRef | PubMed |
Berney SC, Rose JW, Bernhardt J, Denehy L. Prospective observation of physical activity in critically ill patients who were intubated for more than 48 hours. J Crit Care. 2015 Aug;30(4):658-63. | CrossRef | PubMed | Connolly BA, Mortimore JL, Douiri A, Rose JW, Hart N, Berney SC. Low Levels of Physical Activity During Critical Illness and Weaning: The Evidence-Reality Gap. J Intensive Care Med. 2017 Jan 1:885066617716377. | CrossRef | PubMed |
Connolly BA, Mortimore JL, Douiri A, Rose JW, Hart N, Berney SC. Low Levels of Physical Activity During Critical Illness and Weaning: The Evidence-Reality Gap. J Intensive Care Med. 2017 Jan 1:885066617716377. | CrossRef | PubMed | Grammatopoulou E, Charmpas TN, Strati EG, Nikolaos T, Evagelodimou A, Vlassia Belimpasaki, Skordilis EK. The scope of physiotherapy services provided in public ICUs in Greece: A pilot study. Physiother Theory Pract. 2017 Feb;33(2):138-146. | CrossRef | PubMed |
Grammatopoulou E, Charmpas TN, Strati EG, Nikolaos T, Evagelodimou A, Vlassia Belimpasaki, Skordilis EK. The scope of physiotherapy services provided in public ICUs in Greece: A pilot study. Physiother Theory Pract. 2017 Feb;33(2):138-146. | CrossRef | PubMed | Norrenberg M, Vincent JL. A profile of European intensive care unit physiotherapists. European Society of Intensive Care Medicine. Intensive Care Med. 2000 Jul;26(7):988-94. | CrossRef | PubMed |
Norrenberg M, Vincent JL. A profile of European intensive care unit physiotherapists. European Society of Intensive Care Medicine. Intensive Care Med. 2000 Jul;26(7):988-94. | CrossRef | PubMed | Campbell L, Bunston R, Colangelo S, Kim D, Nargi J, Hill K, et al. The provision of weekend physiotherapy services in tertiary-care hospitals in Canada. Physiother Can. 2010 Fall;62(4):347-54. | CrossRef | PubMed |
Campbell L, Bunston R, Colangelo S, Kim D, Nargi J, Hill K, et al. The provision of weekend physiotherapy services in tertiary-care hospitals in Canada. Physiother Can. 2010 Fall;62(4):347-54. | CrossRef | PubMed | Griffiths P, Ball J, Murrells T, Jones S, Rafferty AM. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open. 2016 Feb 9;6(2):e008751. | CrossRef | PubMed |
Griffiths P, Ball J, Murrells T, Jones S, Rafferty AM. Registered nurse, healthcare support worker, medical staffing levels and mortality in English hospital trusts: a cross-sectional study. BMJ Open. 2016 Feb 9;6(2):e008751. | CrossRef | PubMed |