 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: acute kidney injury, hospital mortality, risk factors, renal dialysis
INTRODUCTION
The worldwide incidence of acute kidney injury is 18% and the overall hospital mortality can rise above 50%. In Peru, there are few series about mortality of acute kidney injury in hemodialysis patients.
OBJECTIVES
To identify risk factors associated to hospital mortality of acute kidney injury in hemodialysis patients.
METHODS
This is a retrospective cohort of patients with acute kidney injury in hemodialysis of Hospital Nacional Edgardo Rebagliati Martins gathered between January 2013 and December 2015. The sample size was 154 patients which allowed a power of 80% and a CI of 95%. ICD-10 codes were used to identify medical records of patients with acute kidney injury (N.17) and hemodialysis (Z.49). The independent variable was oliguria, and the primary outcome was hospital mortality. Poisson regression was used for multivariate analysis.
RESULTS
We identified a total of 285 patients; 212 medical records were analyzed and 44 were excluded. Out of the 168 medical records, 129 belonged to living patients and 39 to deceased ones. The overall mortality incidence was 17.2%. The principal etiologies of acute kidney injury while in hemodialysis were sepsis (39.2%), and severe dehydration (10.8%). In the adjusted model, the risk factors associated to hospital mortality of acute kidney injury while in hemodialysis were elevated serum lactate (RR 1.09), elevated serum potassium (RR 0.93), and mean arterial pressure (RR 0.97).
CONCLUSIONS
Lactate is an objective parameter that can predict prognosis and contributes to a better management of acute kidney injury in hemodialysis patients.
Acute kidney injury is defined as an abrupt and reversible decrease of the renal function [1],[2]. This disease is under-registered because of difficulties in the access to health services, lack of knowledge of general population and lack of bloodwork in hospitals [3]. However, these patients have a high mortality rate and this leads to a rise in health expenditures [4].
The global incidence of acute kidney injury is around 18% in hospitalized patients and 30-60% in intensive care unit patients [5],[6]. Bagshaw found an in-hospital mortality of 51.9% in this population and the principal risk factors were high values of serum creatinine and urea, oliguria and multi-organ failure [7]. On the other hand, Chih-Chung found a mortality rate of 58.2% and main risk factors were aging, congestive heart failure and a high value in Sequential Organ Failure Assessment score [8]. This score predicts mortality rate based on clinical and laboratory data. Also, there are other scores that can be used in acute kidney injury patients like the Acute Physiology and Chronic Health Evaluation II and the Simplified Acute Physiologic Score [9],[10], finding a correlation between higher score values and risk of death.
On the other hand, hemodialysis is a renal replacement therapy that is initiated depending of several factors. Nowadays, there is no clinical guideline specifying when to start this treatment, although some authors indicate that an increase of serum creatinine or urea and hyperkalemia, metabolic acidosis, or fluid overload can influence in the decision to start hemodialysis [11].
In Peru, there are few series about mortality of acute kidney injury patients in hemodialysis. In 2013, one series at Hospital Nacional Dos de Mayo, a public institution, evaluated patients with similar characteristics and found a mortality rate of 39.5% [12]. However, there are no series in a third level hospital of EsSalud, in which there could be different results due to their infrastructure.
The aim of the study was to identify risk factors associated to hospital mortality of acute kidney injury patients in hemodialysis in the Hospital Nacional Edgardo Rebagliati Martins. The specific aims were to quantify the incidence of hospital mortality in acute kidney injury patients, determine their main risk factors and their etiology as well.
This is a retrospective cohort study and the information was collected from the mentioned hospital, Lima, Peru. This is a national reference high-complex hospital that receives patients from different parts of the country. Every patient diagnosed with acute kidney injury on hemodialysis in the period from January to December 2015 in the Hospital Nacional Edgardo Rebagliati Martins was included in the study.
Sample size was calculated with information from Loza et al. study, which revealed that 48% of oliguric versus only 24% of the non-oliguric patients died, finding a RR of 1.9 [13]. Using Epidat 4.0, oliguria was the independent variable and hospital mortality the dependent one (outcome). A power of 80% and 95% confidence level was used, resulting in 154 patients. Considering a 10% error for lost or erroneous medical histories, 169 people were included.
We included every patient above eighteen years old diagnosed with acute kidney injury (CIE-10 N17) and hemodialysis (CIE-10 Z49) submitted to this treatment after a nephrologist indication. Exclusion criteria were renal malformations or renal transplant, pregnancy (for women), history of chronic kidney disease and patients who didn’t have a creatinine value after their last hemodialysis.
Patients who were diagnosed with acute kidney injury in hemodialysis participated in the study and were followed during the next 28 days. Hospital mortality was defined as a patient’s death in the first 28 days after acute kidney injury in hemodialysis diagnosis. Time between the diagnosis of acute kidney injury and the beginning of hemodialysis was defined in hours after the nephrologist indication.
Glomerular filtration rate at acute kidney injury diagnosis and at the beginning of hemodialysis were measured with the Modification of Diet in Renal Disease formula using the value of creatinine in those respective moments. Blood urea nitrogen was obtained with standardized formula: BUN=Urea/2.1428 [14]. Laboratory exams were performed in two opportunities: at acute kidney injury in hemodialysis diagnosis and after the last hemodialysis.
A file was developed for each patient with the information collected from his or her medical history obtained in the Medical Records Department. This information was logged in Microsoft Excel by double digitation.
The Ethics Committee of the Universidad Peruana de Ciencias Aplicadas and the Hospital Nacional Edgardo Rebagliati Martins approved the study. Personal contact with patients was not necessary for the development of this study and informed consent was not applied. Medical histories were identified by a number code, in order not to jeopardize the patient’s privacy.
Collected data were analyzed with Stata 13.0. Categorical variables were reported as proportions (percentages). After using Shapiro-Wilk test for assessing normality of quantitative variables, the majority did not meet this request and all these variables were summarized as medians. In bivariate analysis, the mentioned variables were compared to hospital mortality. Chi-square test or Fisher exact test were used as appropriate. Quantitative variables were compared with Mann-Whitney test. Variables with a p value less than or equal to 0.05 in bivariate analysis and those directly related to the pathophysiological mechanism of mortality were included in multivariate Poisson regression, so RR´s were adjusted for these same variables and mechanic ventilation.
The total number of medical records was 285. Seventy three of them were not found due to different reasons and 14 of these records met exclusion criteria. In total, 212 medical records were reviewed and 44 also met exclusion criteria. Thus, we included 227 patients for the calculation of incidence, but we only analyzed data from 168 patients, 129 alive and 39 deceased. See Figure 1.
Figure 1. Patients´ fluxogram.
Age median was 69 (55 to 77.5) and 61.9% of patients were men. Mortality incidence was 17.2%. The demographic, clinical and laboratory data are shown in Table 1. Length of stay median was 15 days (10 to 23.5) and the period of time between hospital admission and the day of diagnosis was 4 hours (1 to 9). Hemodialysis median was three sessions (2 to 4). At diagnosis, urine output less than 400ml/day was quantified in 43.5% of patients and glomerular filtration rate was 12ml/min/1.73m2 (7.5 to 17). Also, 20% of patients presented fluid overload at diagnosis and 51.2% presented shock. Septic shock was the main type of shock (39.9%), followed by cardiogenic (9%) and hypovolemic (6%) shock. Seventy four percent of patients were admitted to the intensive care unit.
Table 2 shows information of living and deceased patients. The comorbidities and Acute Physiologic And Chronic Health Evaluation II score were similar in both groups, but Sequential Organ Failure Assessment and Simplified Acute Physiologic Score had a higher value in deceased patients, showing statistical association. Sepsis was the most frequent etiology of acute kidney injury in both groups, and it had a higher incidence in deceased patients (p<0.05). Length of stay in living patients was higher than in deceased patients, but the period of time between the day of diagnosis and start of hemodialysis was similar in both (p<0.05). Serum creatinine values before hemodialysis were higher in living patients. Serum lactate and potassium values were lower in living patients, and pH and bicarbonate during hospital stay were lower in deceased patients, presenting significant association. Presence of shock was higher in deceased patients, although septic shock was the most frequent type of shock in both groups. Intensive care unit admission and mechanical ventilation were higher in deceased patients showing statistical association.
Table 3 shows the multivariate analysis, which included those variables and mechanical ventilation in Intensive Care Unit. Urine output, which was part of the initial hypothesis, did not showed significant association (p=0.374). However, lactate and potassium did, with a RR 1.09 (95% CONFIDENCE INTERVAL: 1.04-1.15) and RR 0.93 (CI95%: 0.87-0.99), respectively. Finally, Media Arterial Pressure also showed significant association in adjusted model RR 0.97 (95% confidence interval: 0.96-0.98).
Table 3. Risk factors associated to hospital mortality in hemodialysis Acute Kidney Injury patients.
In this study, the mortality incidence was 17.2%. In other series taken in Peru, the incidence mortality in acute kidney injury patients was 10% at the Hospital Arzobispo Loayza in 2004 [15]. A Spanish article showed that the mortality varies from 7% in patients with prerenal azotemia to 80% in intensive care unit patients, while other studies show that it varies from 20 to 80% depending on the etiology, the clinical course and the severity of the acute kidney injury [16],[17],[18]. The rise of mortality incidence in this study is probably due to an higher age mean of 69 years; unlike Soto et al. that had a mean age of 45.8 years. This statement is based on Brady et al. [19], who described a relationship between older age and mortality rate in acute kidney injury patients.
The multivariate analysis of this series had statistic modelling, reason why only the significant variables of the bivariate analysis were adjusted. Furthermore, the initial hypothesis of this article was the variable oliguria, shown on the final results of the multivariate analysis.
The presence of oliguria in acute kidney injury patients is a previously established risk factor associated to mortality [20]; however, this study did not reveal a statistically significant association in the multivariate analysis (RR 1.00 95% confidence interval: 0.99-1.00). On the other hand, mean arterial pressure was found as a protective factor (RR 0.97 95% confidence interval: 0.96-0.98). Raimundo et al. described, in a retrospective study with intensive care unit patients, that a higher mean arterial pressure in the first 12 hours from acute kidney injury diagnosis is associated with a lower risk of developing stage III acute kidney injury of Acute Kidney Injury Network classification [21]. For this reason, maintaining a mean arterial pressure in adequate values contributes to prevent or reduce the duration of acute kidney injury [22].
Searching for an objective parameter to predict the prognosis of the population of this study, a statistically significant association was found in the adjusted model with serum lactate (RR 1.09 95% confidence interval: 1.04-1.15). The 9% higher probability of hospital death is supported by the results of Husain et al., who found elevated levels of serum lactate in deceased intensive care unit patients compared to living patients (4.2 vs. 2.8 mmol/L, p=0.002) [23]. Also, Allegreti et al. found that one of the risk factors associated to mortality of acute kidney injury in hemodialysis patients was serum lactate levels higher than 4 mmol/L [24]. In this study, deceased patients had a mean serum lactate of 2.3 mmol/l with an upper limit of 3.4 mmol/L, and associated with mortality as described before. In the study of Barreto et al. it was found that acute kidney injury after and hepatic graft dysfunction is associated with high levels of lactate, as this is a poor tissue perfusion marker, being present hemodynamic instability, hypotension and consequently kidney involvement, thereby increasing levels of lactate [25]. However, according to Vashistha et al. the mechanism whereby metabolic acidosis increases the mortality risk of these patients is not clear. It is known that hyperkalemia, increased protein catabolism, increased insulin resistance, systemic inflammation, a rapid loss of renal function and calcium efflux from the bone contribute to mortality of dialysis patients [26].
We found that the elevation of 1 mEq/l of potassium lowered the risk of mortality by 7%. This result contrasts with other series [27],[28], who refer that hyperkalemia is an independent predictor of the severity and mortality of acute kidney injury in intensive care unit patients. However, in our study we found a median level of potassium of 4.6 mEq/l in living patients, and 4.8 mEq/L in deceased patients, with a normal value range between 3.5 to 5.0 mEq/L [29]. This can be explained by the trending management of the health center studied to initiate early hemodialysis. As described by Thakar et al., the decision of early initiation of hemodialysis is based on avoiding acute kidney injury complications, such as hyperkalemia [30].
The weakness of this study was that not all medical records of living patients were found, because they were not available at the moment of the data gathering. However, the study accomplished the sample size necessary to corroborate the hypothesis and significant variables in the adjusted model. The strength is that a cohort study is ideal to respond questions about the prognosis of patients. Also, finding associated risk factors, like serum lactate, which would allow us to predict which patients need early hemodialysis.
The mortality incidence was 17.2%. In the lab variables, serum lactate was found as a risk factor associated to hospital mortality. This is an objective and measurable parameter that should be used more frequently to know the prognosis of this specific population.
We suggest similar studies with an expanded population, which should include other health institutions in Peru such as Ministerio de Salud, military health centers and other EsSalud health centers in order to compare the behavior of the specific populations in different type of health centers. It is important to determine more clinical and laboratory parameters that can predict the clinical course of acute kidney injury in hemodialysis patients.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal is aware that the Ethics Committee of the Peruvian University of Applied Sciences and the Edgardo Rebagliati Martins National Hospital were aware of and approved this study and its possible publication in a biomedical dissemination journal.
Conflicts of interest
The authors have completed the ICMJE declaration of conflicts of interests form, and declare that they have not received funding for the report; not having financial relationships with organizations that might have interests in the published article in the past three years; and not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.
Acknowledgement
We thank the Hemodialysis Center and Medical Record Registry Department of the Hospital Nacional Edgardo Rebagliati Martins for their help.

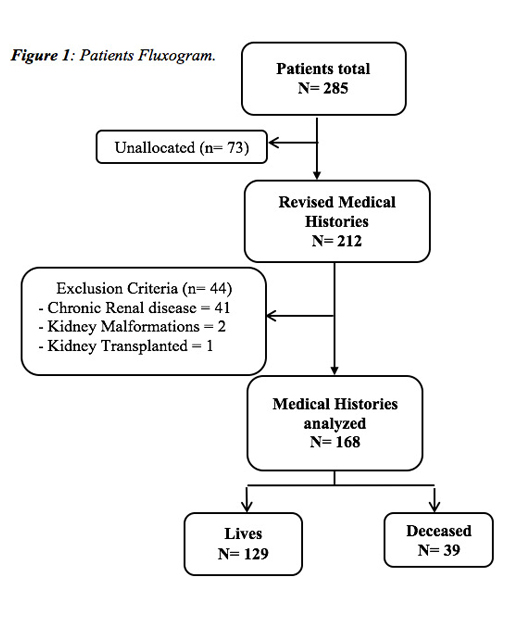 Figure 1. Patients´ fluxogram.
Figure 1. Patients´ fluxogram.

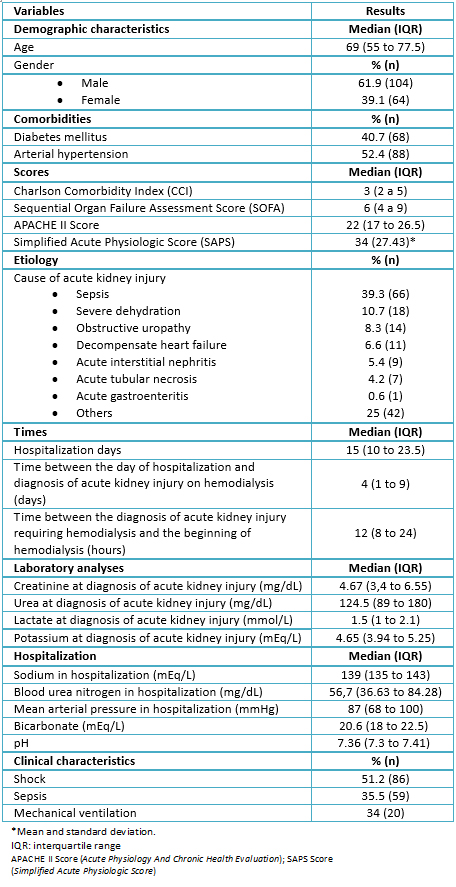 Table 1. Demographics and clinical characteristic of acute kidney injury patients subjected to hemodialysis at the Hospital Nacional Edgardo Rebagliati Martins in Lima, Peru from 2013 to 2015.
Table 1. Demographics and clinical characteristic of acute kidney injury patients subjected to hemodialysis at the Hospital Nacional Edgardo Rebagliati Martins in Lima, Peru from 2013 to 2015.

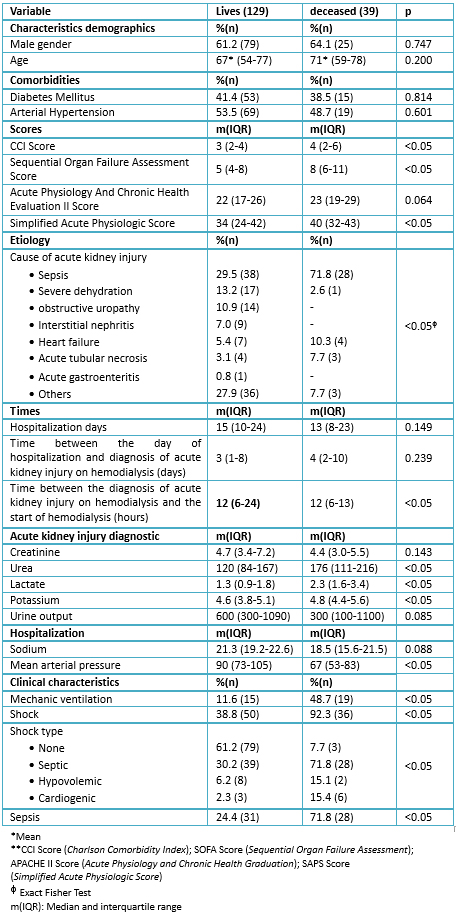 Table 2. Comparison of demographics, clinical and physiological characteristics between living and deceased patients with acute kidney injury on hemodialysis in Hospital Nacional Edgardo Rebagliati Martins in Lima, Peru 2013-2015.
Table 2. Comparison of demographics, clinical and physiological characteristics between living and deceased patients with acute kidney injury on hemodialysis in Hospital Nacional Edgardo Rebagliati Martins in Lima, Peru 2013-2015.

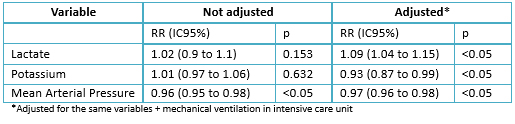 Table 3. Risk factors associated to hospital mortality in hemodialysis Acute Kidney Injury patients.
Table 3. Risk factors associated to hospital mortality in hemodialysis Acute Kidney Injury patients.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
The worldwide incidence of acute kidney injury is 18% and the overall hospital mortality can rise above 50%. In Peru, there are few series about mortality of acute kidney injury in hemodialysis patients.
OBJECTIVES
To identify risk factors associated to hospital mortality of acute kidney injury in hemodialysis patients.
METHODS
This is a retrospective cohort of patients with acute kidney injury in hemodialysis of Hospital Nacional Edgardo Rebagliati Martins gathered between January 2013 and December 2015. The sample size was 154 patients which allowed a power of 80% and a CI of 95%. ICD-10 codes were used to identify medical records of patients with acute kidney injury (N.17) and hemodialysis (Z.49). The independent variable was oliguria, and the primary outcome was hospital mortality. Poisson regression was used for multivariate analysis.
RESULTS
We identified a total of 285 patients; 212 medical records were analyzed and 44 were excluded. Out of the 168 medical records, 129 belonged to living patients and 39 to deceased ones. The overall mortality incidence was 17.2%. The principal etiologies of acute kidney injury while in hemodialysis were sepsis (39.2%), and severe dehydration (10.8%). In the adjusted model, the risk factors associated to hospital mortality of acute kidney injury while in hemodialysis were elevated serum lactate (RR 1.09), elevated serum potassium (RR 0.93), and mean arterial pressure (RR 0.97).
CONCLUSIONS
Lactate is an objective parameter that can predict prognosis and contributes to a better management of acute kidney injury in hemodialysis patients.
 Autores:
Mariela Alejandra Linares-Linares[1], Jorge Arturo Figueroa-Tarrillo[1], Renato Cerna Viacava[1], Nilton Yhuri Carreazo[1,2], Renzo P. Valdivia-Vega[1,3]
Autores:
Mariela Alejandra Linares-Linares[1], Jorge Arturo Figueroa-Tarrillo[1], Renato Cerna Viacava[1], Nilton Yhuri Carreazo[1,2], Renzo P. Valdivia-Vega[1,3]

Citación: Linares-Linares MA, Figueroa-Tarrillo JA, Cerna Viacava R, Carreazo NY, Valdivia-Vega RP. Risk factors associated to hospital mortality in patients with acute kidney injury on hemodialysis. Medwave 2017 Mar;17(2):e6879 doi: 10.5867/medwave.2017.02.6879
Fecha de envío: 26/10/2016
Fecha de aceptación: 26/1/2017
Fecha de publicación: 6/3/2017
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Wang HE, Muntner P, Chertow GM, Warnock DG. Acute kidney injury and mortality in hospitalized patients. Am J Nephrol. 2012;35(4):349-55. | CrossRef | PubMed |
Wang HE, Muntner P, Chertow GM, Warnock DG. Acute kidney injury and mortality in hospitalized patients. Am J Nephrol. 2012;35(4):349-55. | CrossRef | PubMed | Tao Li P, Burdmann E, Mehta R. Acute kidney injury: Global health alert. Int J Org Transplant Med. 2013; 4 (1): 1-8. | Link |
Tao Li P, Burdmann E, Mehta R. Acute kidney injury: Global health alert. Int J Org Transplant Med. 2013; 4 (1): 1-8. | Link | Lewington AJ, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013 Sep;84(3):457-67. | CrossRef | PubMed |
Lewington AJ, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013 Sep;84(3):457-67. | CrossRef | PubMed | Wang R, Ma X. Clarification on the categorization of comorbidities. Leuk Res. 2010 Feb;34(2):e74. | CrossRef | PubMed |
Wang R, Ma X. Clarification on the categorization of comorbidities. Leuk Res. 2010 Feb;34(2):e74. | CrossRef | PubMed | Singbartl K, Kellum JA. AKI in the ICU: definition, epidemiology, risk stratification, and outcomes. Kidney Int. 2012 May;81(9):819-25. | CrossRef | PubMed |
Singbartl K, Kellum JA. AKI in the ICU: definition, epidemiology, risk stratification, and outcomes. Kidney Int. 2012 May;81(9):819-25. | CrossRef | PubMed | Piccinni P, Cruz DN, Gramaticopolo S, Garzotto F, Dal Santo M, Aneloni G, et al. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol. 2011 Nov;77(11):1072-83. | PubMed |
Piccinni P, Cruz DN, Gramaticopolo S, Garzotto F, Dal Santo M, Aneloni G, et al. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol. 2011 Nov;77(11):1072-83. | PubMed | Bagshaw SM, Wald R, Barton J, Burns KE, Friedrich JO, House AA, et al. Clinical factors associated with initiation of renal replacement therapy in critically ill patients with acute kidney injury-a prospective multicenter observational study. J Crit Care. 2012 Jun;27(3):268-75. | CrossRef | PubMed |
Bagshaw SM, Wald R, Barton J, Burns KE, Friedrich JO, House AA, et al. Clinical factors associated with initiation of renal replacement therapy in critically ill patients with acute kidney injury-a prospective multicenter observational study. J Crit Care. 2012 Jun;27(3):268-75. | CrossRef | PubMed | Shiao CC, Wu VC, Li WY, Lin YF, Hu FC, Young GH, et al. Late initiation of renal replacement therapy is associated with worse outcomes in acute kidney injury after major abdominal surgery. Crit Care. 2009;13(5):R171. | CrossRef | PubMed |
Shiao CC, Wu VC, Li WY, Lin YF, Hu FC, Young GH, et al. Late initiation of renal replacement therapy is associated with worse outcomes in acute kidney injury after major abdominal surgery. Crit Care. 2009;13(5):R171. | CrossRef | PubMed | Chang CH, Fan PC, Chang MY, Tian YC, Hung CC, Fang JT, et al. Acute kidney injury enhances outcome prediction ability of sequential organ failure assessment score in critically ill patients. PLoS One. 2014 Oct 3;9(10):e109649. | CrossRef | PubMed |
Chang CH, Fan PC, Chang MY, Tian YC, Hung CC, Fang JT, et al. Acute kidney injury enhances outcome prediction ability of sequential organ failure assessment score in critically ill patients. PLoS One. 2014 Oct 3;9(10):e109649. | CrossRef | PubMed | Demirjian S, Chertow GM, Zhang JH, O'Connor TZ, Vitale J, Paganini EP, et al. Model to predict mortality in critically ill adults with acute kidney injury. Clin J Am Soc Nephrol. 2011 Sep;6(9):2114-20. | CrossRef | PubMed |
Demirjian S, Chertow GM, Zhang JH, O'Connor TZ, Vitale J, Paganini EP, et al. Model to predict mortality in critically ill adults with acute kidney injury. Clin J Am Soc Nephrol. 2011 Sep;6(9):2114-20. | CrossRef | PubMed | Joannidis M, Forni LG. Renal replacement therapy: to treat, or not to treat, that is the question... Crit Care. 2013 Mar 19;17(2):125. | CrossRef | PubMed |
Joannidis M, Forni LG. Renal replacement therapy: to treat, or not to treat, that is the question... Crit Care. 2013 Mar 19;17(2):125. | CrossRef | PubMed | Herrera P, Palacio M, Chipayo D, Gavidia J, Silveira M. Características clínicas de los pacientes con injuria renal aguda en diálisis en un hospital general. An Fac Med. 2013;74(4):307-10. | Link |
Herrera P, Palacio M, Chipayo D, Gavidia J, Silveira M. Características clínicas de los pacientes con injuria renal aguda en diálisis en un hospital general. An Fac Med. 2013;74(4):307-10. | Link | Loza R, Estremadoyro L, Loza C, Cieza J. Factors associated with mortality in acute renal failure (ARF) in children. Pediatr Nephrol. 2006 Jan;21(1):106-9. | PubMed |
Loza R, Estremadoyro L, Loza C, Cieza J. Factors associated with mortality in acute renal failure (ARF) in children. Pediatr Nephrol. 2006 Jan;21(1):106-9. | PubMed | Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-84. | CrossRef | PubMed |
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179-84. | CrossRef | PubMed | Soto A, Rodríguez V, Escudero E, Hurtado A. [Evaluation of individual risk and mortality related factors in acute renal failure]. Nefrologia. 2004;24(3):239-45. | PubMed |
Soto A, Rodríguez V, Escudero E, Hurtado A. [Evaluation of individual risk and mortality related factors in acute renal failure]. Nefrologia. 2004;24(3):239-45. | PubMed | Martinez T, Delgado V, D’Achiardi R. Insuficiencia Renal Aguda. Universitas Médica. 2004;45(2):57-64. | Link |
Martinez T, Delgado V, D’Achiardi R. Insuficiencia Renal Aguda. Universitas Médica. 2004;45(2):57-64. | Link | de Mendonça A, Vincent JL, Suter PM, Moreno R, Dearden NM, Antonelli M, et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 2000 Jul;26(7):915-21. | PubMed |
de Mendonça A, Vincent JL, Suter PM, Moreno R, Dearden NM, Antonelli M, et al. Acute renal failure in the ICU: risk factors and outcome evaluated by the SOFA score. Intensive Care Med. 2000 Jul;26(7):915-21. | PubMed | Corwin HL, Teplick RS, Schreiber MJ, Fang LS, Bonventre JV, Coggins CH. Prediction of outcome in acute renal failure. Am J Nephrol. 1987;7(1):8-12. | PubMed |
Corwin HL, Teplick RS, Schreiber MJ, Fang LS, Bonventre JV, Coggins CH. Prediction of outcome in acute renal failure. Am J Nephrol. 1987;7(1):8-12. | PubMed | Raimundo M, Crichton S, Syed Y, Martin JR, Beale R, Treacher D, et al. Low Systemic Oxygen Delivery and BP and Risk of Progression of Early AKI. Clin J
Am Soc Nephrol. 2015 Aug 7;10(8):1340-9. | CrossRef | PubMed |
Raimundo M, Crichton S, Syed Y, Martin JR, Beale R, Treacher D, et al. Low Systemic Oxygen Delivery and BP and Risk of Progression of Early AKI. Clin J
Am Soc Nephrol. 2015 Aug 7;10(8):1340-9. | CrossRef | PubMed | Ahmed W, Memon JI, Rehmani R, Al Juhaiman A. Outcome of patients with acute kidney injury in severe sepsis and septic shock treated with early goal-directed therapy in an intensive care unit. Saudi J Kidney Dis Transpl. 2014 May;25(3):544-51. | PubMed |
Ahmed W, Memon JI, Rehmani R, Al Juhaiman A. Outcome of patients with acute kidney injury in severe sepsis and septic shock treated with early goal-directed therapy in an intensive care unit. Saudi J Kidney Dis Transpl. 2014 May;25(3):544-51. | PubMed | Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003 May;185(5):485-91. | PubMed |
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003 May;185(5):485-91. | PubMed | Allegretti AS, Steele DJ, David-Kasdan JA, Bajwa E, Niles JL, Bhan I. Continuous renal replacement therapy outcomes in acute kidney injury and end-stage renal disease: a cohort study. Crit Care. 2013 Jun 20;17(3):R109. | CrossRef | PubMed |
Allegretti AS, Steele DJ, David-Kasdan JA, Bajwa E, Niles JL, Bhan I. Continuous renal replacement therapy outcomes in acute kidney injury and end-stage renal disease: a cohort study. Crit Care. 2013 Jun 20;17(3):R109. | CrossRef | PubMed | Barreto AG, Daher EF, Silva Junior GB, Garcia JH, Magalhães CB, Lima JM, et al. Risk factors for acute kidney injury and 30-day mortality after liver transplantation. Ann Hepatol. 2015 Sep-Oct;14(5):688-94. | PubMed |
Barreto AG, Daher EF, Silva Junior GB, Garcia JH, Magalhães CB, Lima JM, et al. Risk factors for acute kidney injury and 30-day mortality after liver transplantation. Ann Hepatol. 2015 Sep-Oct;14(5):688-94. | PubMed | Vashistha T, Kalantar-Zadeh K, Molnar MZ, Torlén K, Mehrotra R. Dialysis modality and correction of uremic metabolic acidosis: relationship with all-cause and cause-specific mortality. Clin J Am Soc Nephrol. 2013 Feb;8(2):254-64. | CrossRef | PubMed |
Vashistha T, Kalantar-Zadeh K, Molnar MZ, Torlén K, Mehrotra R. Dialysis modality and correction of uremic metabolic acidosis: relationship with all-cause and cause-specific mortality. Clin J Am Soc Nephrol. 2013 Feb;8(2):254-64. | CrossRef | PubMed | Samimagham HR, Kheirkhah S, Haghighi A, Najmi Z. Acute kidney injury in intensive care unit: incidence, risk factors and mortality rate. Saudi J Kidney Dis Transpl. 2011 May;22(3):464-70. | PubMed |
Samimagham HR, Kheirkhah S, Haghighi A, Najmi Z. Acute kidney injury in intensive care unit: incidence, risk factors and mortality rate. Saudi J Kidney Dis Transpl. 2011 May;22(3):464-70. | PubMed | Mataloun SE, Machado FR, Senna AP, Guimarães HP, Amaral JL. Incidence, risk factors and prognostic factors of acute renal failure in patients admitted to an intensive care unit. Braz J Med Biol Res. 2006 Oct;39(10):1339-47. | PubMed |
Mataloun SE, Machado FR, Senna AP, Guimarães HP, Amaral JL. Incidence, risk factors and prognostic factors of acute renal failure in patients admitted to an intensive care unit. Braz J Med Biol Res. 2006 Oct;39(10):1339-47. | PubMed | Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison principios de medicina interna. Vol 2. México: McGraw‐Hill; 2012.
Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison principios de medicina interna. Vol 2. México: McGraw‐Hill; 2012.