 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: biohazard release, needlestick injuries, body fluids, medical students, universal precautions
OBJECTIVE
To determine the frequency and characteristics of biological accidents in last-year medical students from three hospitals in Lima.
METHODS
Cross-sectional study performed at three Public Health Insurance hospitals in Lima, in December 2014. The study population comprised last-year medical interns. Biological accidents were recorded with a questionnaire of exposure to blood and body fluids based on the formats used by the Exposure Prevention Information Network system and the Centers for Disease Control and Prevention. We inquired about occurrence and number of biological accidents as well as the characteristics of the last accident. Categorical data are presented as absolute and percentage frequencies and numeric data, as median and interquartile ranges.
RESULTS
We collected 100 respondents; 85% of them had had a biological accident during the last year, with a median of 2 and interquartile range of 3. The most frequent type of exposure was percutaneous (71.8%) and the most common device was the hollow needle (54.1%). The most frequent place of occurrence and activities at the moment of exposure were at the delivery room (44.7%), while supervising a vaginal delivery (24.7%), and during suturing (24.7%). Three accidents involved high-risk patients, but only one student received antiviral prophylaxis; 49.4% attributed the cause of the accident to fatigue, and 75.3% of accidents are not reported. Gloves are the most used protective barrier (95%).
CONCLUSIONS
The frequency of biological accidents among last-year medical students is high. Underreporting and inappropriate use of protective barriers increase the risk of medical students for biological accidents.
Medical practice involves biological risks caused by the frequent handling of sharp objects as well as biological fluids, which are strong risks for serious diseases among health workers and medical students [1],[2],[3].
The internship in Medicine is made during the seventh and last year of the medical career study plan in Peru. During the internship, the student does hospital practices having a more close contact with the patient, while doing different clinical-surgical procedures. Some of these are lumbar puncture, arterial and venal blood withdrawal (analysis of arterial gases), paracentesis and birth assistance. The objectives of these activities are to provide an appropriate training so that the students can acquire the motor skills needed for a good professional exercise [1].
Medical students, because of the fact that they are training, added to their inexperience and lack of development of skills inherent to their training period [1],[4],[5]; are exposed to a greater risk of suffering biological accidents with exposition to blood pathogens such as the human immunodeficiency virus (HIV), hepatitis B and hepatitis C. Also, the practice of biosecurity measures and the adequate report of the accidents are irregularly followed by medical students [5],[6],[7].
There are very few study cases in Peru about biological accidents in last-year medical students [4]. This group has the highest risk while doing their internship, given the closer and more real contact with the patients. Statistical data in Peru and other countries about biological accidents in medical students are the expression of the huge sub registry and the students´ poor sensibility for the recognition and handling of these accidents [1],[2],[3],[4],[5]. Because of this, we decided to carry out the present study in our environment, its objective being to describe the frequency and characteristics of the biological accidents in last-year medical students in three Lima hospitals.
The present is a cross-sectional study. It was made on December 2014 in three Public Health Insurance Hospitals in Lima: Hospital Nacional Edgardo Rebagliati Martins, Hospital Nacional Guillermo Almenara Irigoyen and Hospital de Emergencias Grau.
In Peru, the health establishments are categorized according to their attention levels. In the first level of attention, low-complexity health problems are taken care of, with less specialization and modernization of their resources. The main activities in these establishments are promotion and protection. The second level takes care of health needs that require attention of intermediate complexity. In the third level, high-complexity health care is needed, as well as high specialization and modernization. The categorization of each health establishment is determined by the quantitative and response capacity (ability to produce the type of services needed to solve the severity of the population needs), and the technological level of the resources (grade of specialization and modernization) [8].
Rebagliati Hospital and Almenara Hospital are categorized as third level of attention Specialized Health Institutes, category III-2, being this the maximum level given by the Health Ministry of Peru [9],[10]. The Grau Emergencies Hospital is also a third level, but category III-1, given that it does not have sub-specializations [11]. These institutions were chosen by convenience, anticipating that they are located at a central place and are hospitals that have agreements with all the Universities, allowing the rotation of medical students and medical residents through their installations.
The population consisted on the last-year medical students of the three aforementioned hospitals. Students that were coursing through the medical internships of the 2014 Health Social Service were also included, of both genders and with rotations in the services of Internal Medicine, Obstetrics and Gynecology, Pediatrics and Surgery. Students that were from other hospitals and those that with sick or other leaves were excluded. No specific sampling methods were used.
Study participants were located during their clinic rotations, with the authorization of the corresponding Chief of Service so that they could fill the instrument in the needed time. Also, it was explained to the students that completing the data was voluntary and confidential; that it would be used for academic purposes and that they could walk away from the process at any time. The instrument did not have any sections allowing the participant´s identification.
The recollection and registering of biological accidents was made through the administration of a questionnaire about the exposition to blood and body fluids. The questionnaire was made from two formats. The first one was based on the system Exposure Prevention Information Network (EPINet), for the registry of needle or sharp objects-related accidents [12]. The second one was based on the form of the Centers for Disease Control and Prevention (CDC) for exposition to blood and body fluids [13]. A questionnaire was made by selecting 19 questions that were translated to Spanish. Some questions about contractual job situation and open questions were not included because they did not correspond to the characteristics of the study population.
Questions were made about the occurrence of biological accidents, defined as any sudden process with the probability to acquire a transmissible infection due to the exposition to biological fluids [14] such as blood, tissue or any other bodily fluid potentially infectious through a percutaneous wound (needle or inflicted by a sharp object), contact with mucous membrane or skin [15]. If the answer was affirmative, the participant was further questioned about the frequency of this kind of accidents from the start of the internship until the moment of the survey, the characteristics of the last accident, protection measures used and number of doses he or she had received against hepatitis B. If the answer was negative, only the last two questions about protection measures and doses against hepatitis B were posed.
Categorical data are presented as absolute numbers and percentages. Quantitative data are shown as medians and interquartile ranges. Microsoft Excel 2013 was used for the database and SPSS version 20 for the statistical analysis.
We included 105 students, from which three were excluded because they were on sick or other leaves and there was a loss rate of two, being 100 students the total number surveyed.
The occurrence of biological accidents according to demographic characteristics is presented in Table 1. There was a dominance of the masculine gender (61%). Eighty five percent of the students presented some kind of biological accident during their first year-internship.
During the internship year of the interviewed students, there were a total of 297 biological accidents: mucous-cutaneous 44.8% (133) and percutaneous 55.2% (164). The amount of biological accidents during the internship year has a median of 2 and an interquartile range of 3.
Regarding the description of the characteristics of the last accident, we found that the most frequent type of exposition was also the percutaneous one with 71.8% (61). The biological fluid more frequently involved was blood with 72.9% (62), followed by amniotic/vaginal liquid visibly bloody with 18.8% (16).
Table 3. Characteristics of the last biological accident in medical students.
The 98.9% (84) of the source patients were identifiable. The 18.8% (16) of the students did not know if the identifiable patient was a considered high risk. Three of the accidents happened with high risk patients, however, only one involved student received antiviral prophylaxis.
Table 4. Self-perceived factors considered as the reason of the last biological accident.
The 75.3% (64) of the students that suffered exposition in the last accident did not report it. The most frequent reason they gave was that the patient was a zero-risk 73.4% (47), followed by lack of time 54.7% (35).
When asked about the protection barriers used to minimize the risk of biological accidents, they answered that the most used measure were gloves (95%), followed by apron (67%) and mask (50%). The least used were the protection glasses (14%) and hat (22%).
The 87% of the interviewed students said they have had the three doses of vaccines against hepatitis B and the 13% only had two doses.
Eighty five percent of last-year medical students presented some kind of biological accident (Table 1). Ramos et al. also registered a high frequency, 96% of the interviewed students suffered at least one accident during their internship year in Lima on the year 2000 [4]. However, other studies reveal that the frequency might be lower like the one by Flores et al., where the 73% of the last-year students suffered accidents by sharp objects [16]. Inga et al., in their study based on Medicine students of a public University in Lima, revealed that 32% of the ones that suffered some kind of biological accident were last-year students, having 75 times more probability of suffering and accident than the first-year students [1]. The high frequency of biological accidents in last-year medical students can be explained given the activities and procedures that they progressively perform, according to their academic level and the great demand of patients requesting for attention in the studied hospitals.
The most frequent type of exposition presented in the last biological accident was percutaneous (72%). According to the recommendations of the Centers for Disease Control and Prevention and the New York State Department of Health, the accidents related to wounds by sharp objects are considered as high risk of acquiring an infection [17]. This result is lower than the observed by Ramos et al., where the 87% of the accidents were high risk [4].
The most frequently biological liquid involved in the last accident was blood, in the range found by several studies [1],[2]. The amniotic/vaginal visibly bloody liquid was second (16%). Herrera et al. reported a lower percentage (5.8%) for the amniotic liquid without specifying if it was bloody or not [2]. This higher percentage can be explained by the place with the most occurrences of this kind of accidents: the delivery room.
Among the characteristics of the percutaneous exposition in the last accident (Table 2), we found that the most frequent device causing the wound was the hollow needle, similar to that observed by other studies [1],[7],[18], which represents a higher risks of acquiring an infectious disease.
In 92% of the percutaneous accidents, the wound-causing device passed through a pair of gloves, indicating that most students were using this protection barrier. In the studied hospitals, due to their higher financial capacity compared to public hospitals, gloves are the protection barrier most frequently found in any work environment.
The bibliography refers that the usage of two pairs of gloves has shown to significantly reduce the perforations of the internal gloves and even more the contamination risk [19]. This is why this practice is recommended as a routine [5]. However, we found that only one student used double gloves. Consequently, it is observed that this practice is not widely known. This is because the work conditions in the health sector are not adequate in Peru, there is a lack of economic resources in the hospital not allowing to provide the staff with the minimum protection equipment needed.
The place with the highest occurrence was the delivery room, followed by the hospitalization floor and the operation room (Table 3). Medical literature notifies that the risk of exposition is higher in areas with the highest number of invasive procedures and more direct contact with patients. The practices with the highest risk are surgical specialties, especially obstetrics and gynecology [1],[5],[20].
In the present study, birth attention and application of stitches were the procedures most frequently accomplished. This is similar to what Tapias et al. found, where the most frequent procedure was birth attention, followed by surgical assistance [5]. This can be explained because last-year medical students in our country have the possibility to perform a big variety of invasive procedures under supervision, such as birth attention and surgical assistance of different complexity, as Tapias et al. expressed [5]. Furthermore, the majority of students perform their first delivery during their internship, and they try to assist the highest amount of births, while also doing their first episiorrhaphies.
The fourth part of the accidents happened in the hospitalization floor. This is correlated with the extraction of arterial gases analysis, being the third most frequent activity done at the moment of the accident. There is a high risk of exposition in this activity, since the hypodermic needle device is used as a direct contact with the artery of the source patient [14].
Almost two thirds of the interns consider that the accident was self-inflicted, which coincides with the findings of other studies [1],[5],[7],[20].
Three accidents happened with high-risk patients, defined as patients with a history of risk factors for HIV infection, Hepatitis B and/or Hepatitis C virus [14]. But only one of the students suffering this accident received antiviral prophylaxis. Tapias et al. informed that five of the accidents suffered by students, involved high-risk patients and only two of them received prophylaxis [5]. This might be explained through of the poor culture of reporting, disinformation and the poorly established risk management system, since there are no or very few protocols to follow when an accident like this happens.
The presence of tiredness or fatigue is the most important factor as the cause of the accident (Table 4). This differs with what Tapia et al. reported, they found that 39% of the students answered the accident happened because of a lack of skill, 23% said because of bad workplace conditions and 18% said the reason was fatigue [5]. This could be because the last-year medical students in our environment, more than pre-professional activities, do tasks far beyond what is considered as academic, as Galán et al. mentioned [20]. Among these tasks are back to back shifts, lack of resting places and lack of rest post-shift. The literature indicates that long work hours and lack of sleep among the aspiring doctors result on fatigue, which is associated with a raise of three times in the risk of wounds by needles [21]. Furthermore, the places in the hospital where most accidents happen are environments where guard shifts are principally made.
The report of the accident is very important, since it allows the person to receive advice about the risks of the exposition and secondary prevention of the infection [5]. Not only should the data in the clinical history of the source patient about the risk of infection by HIV, Hepatitis B or C be considered. Therefore, every accident should be reported to get the injured person tested by all the pertinent tests. Despite this, we found that three fourths of the accidents were not reported, arguing that the patient was a zero-risk one. This was similar to the findings of Tapias et al., where more than half of the students did not report the accident, arguing that the exposition had no risk [5].
A substantial aspect is active immunization, which constitutes the most effective measure for the prevention of occupational Hepatitis B infection, being recommended to medical students before starting the practices according to their career [1]. In our study, 87% of the interviewed students informed having received the three recommended doses, far superior to the findings of other studies [1],[4],[7]. This higher coverage could mostly be because these vaccines are free and are also pre-requisites to enter the university. However, there is a 13% not fully protected. This is worrying because of the close contact that they have with the patients, the high frequency of high-risk accidents and because in Peru there are areas with high occurrence of the virus.
It should be mentioned that this work presents limitations, such as the heterogeneity of the studied population and the belonging to private hospitals (Social Health Insurance). More studies are needed where the frequency and the characteristics of the biological accidents of medical interns that belong to public and private schools can be compared. We also consider the present study is not representative of what happens in the whole country, since this issue was not considered in its design. Because of this it would be recommended to carry out a national level study, to evaluate the differences presented in each province.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
As for the approval of the ethics committee we have the disadvantage that the hospitals where the study was conducted, did not have a consolidated ethics research committee in December 2014. However, we requested authorization from the department heads of Internal Medicine, Surgery, Obstetrics and Gynecology and Pediatrics of the three hospitals before the administration of the questionnaire. Students were placed in the services where they performed their last rotation, they were invited to participate in the study after they were informed the questionnaire was anonymous and voluntary and informed verbal consent was obtained. This study did not mean any risk to participants, the information gathered had no impact on the evaluation of medical internship and no personal questions were asked.
Conflicts of interest
The authors completed the ICMJE conflict of interest declaration form, translated to Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare that there was no funding coming from external sources.

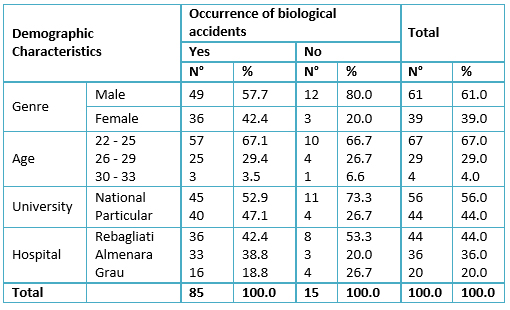 Table 1. Occurrence of biological accidents according to demographic characteristics of the medical students.
Table 1. Occurrence of biological accidents according to demographic characteristics of the medical students.

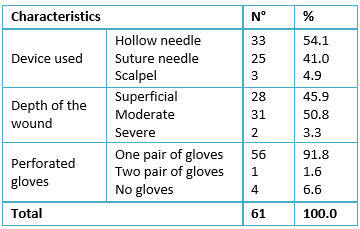 Table 2. Characteristics of percutaneous exposition of the last biological accident in medical students.
Table 2. Characteristics of percutaneous exposition of the last biological accident in medical students.

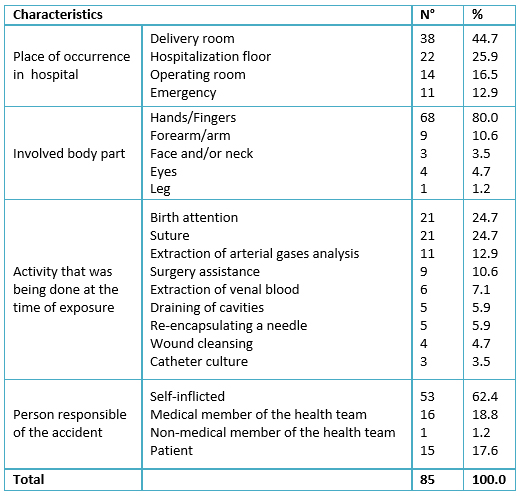 Table 3. Characteristics of the last biological accident in medical students.
Table 3. Characteristics of the last biological accident in medical students.

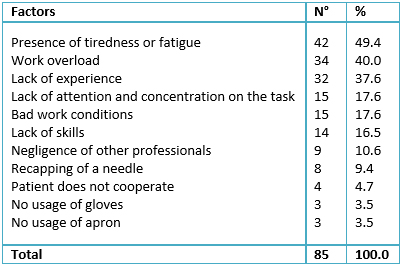 Table 4. Self-perceived factors considered as the reason of the last biological accident.
Table 4. Self-perceived factors considered as the reason of the last biological accident.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

OBJECTIVE
To determine the frequency and characteristics of biological accidents in last-year medical students from three hospitals in Lima.
METHODS
Cross-sectional study performed at three Public Health Insurance hospitals in Lima, in December 2014. The study population comprised last-year medical interns. Biological accidents were recorded with a questionnaire of exposure to blood and body fluids based on the formats used by the Exposure Prevention Information Network system and the Centers for Disease Control and Prevention. We inquired about occurrence and number of biological accidents as well as the characteristics of the last accident. Categorical data are presented as absolute and percentage frequencies and numeric data, as median and interquartile ranges.
RESULTS
We collected 100 respondents; 85% of them had had a biological accident during the last year, with a median of 2 and interquartile range of 3. The most frequent type of exposure was percutaneous (71.8%) and the most common device was the hollow needle (54.1%). The most frequent place of occurrence and activities at the moment of exposure were at the delivery room (44.7%), while supervising a vaginal delivery (24.7%), and during suturing (24.7%). Three accidents involved high-risk patients, but only one student received antiviral prophylaxis; 49.4% attributed the cause of the accident to fatigue, and 75.3% of accidents are not reported. Gloves are the most used protective barrier (95%).
CONCLUSIONS
The frequency of biological accidents among last-year medical students is high. Underreporting and inappropriate use of protective barriers increase the risk of medical students for biological accidents.
 Autores:
Lilyan Consuelo Charca-Benavente[1], Grozny Howell Huanca-Ruelas[1], Oscar Moreno-Loaiza[1]
Autores:
Lilyan Consuelo Charca-Benavente[1], Grozny Howell Huanca-Ruelas[1], Oscar Moreno-Loaiza[1]

Citación: Charca-Benavente LC, Huanca-Ruelas GH, Moreno-Loaiza O. Biological accidents in last-year medical students from three hospitals in Lima Peru. Medwave 2016 Ago;16(7):e6514 doi: 10.5867/medwave.2016.07.6514
Fecha de envío: 24/5/2016
Fecha de aceptación: 1/8/2016
Fecha de publicación: 11/8/2016
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Inga E, López G, Kamiya C. Accidentes biológicos en estudiantes de medicina de una universidad peruana: prevalencia, mecanismos y factores de riesgo. An Fac Med. 2010; 71(1):37-42. | Link |
Inga E, López G, Kamiya C. Accidentes biológicos en estudiantes de medicina de una universidad peruana: prevalencia, mecanismos y factores de riesgo. An Fac Med. 2010; 71(1):37-42. | Link | Herrera A, Gómez R. Accidentes biológicos en estudiantes de medicina y médicos internos de la Universidad Tecnológica de Pereyra. Rev Méd de Risaralda. 2003;9(1):1-10.
| Link |
Herrera A, Gómez R. Accidentes biológicos en estudiantes de medicina y médicos internos de la Universidad Tecnológica de Pereyra. Rev Méd de Risaralda. 2003;9(1):1-10.
| Link | Cortijo J, Gómez M. Cambios en conocimientos, actitudes y aptitudes sobre bioseguridad en estudiantes de los últimos años de medicina. Rev.Méd Hered. 2010;21:27-31. | Link |
Cortijo J, Gómez M. Cambios en conocimientos, actitudes y aptitudes sobre bioseguridad en estudiantes de los últimos años de medicina. Rev.Méd Hered. 2010;21:27-31. | Link | Ramos S, Castillo C, Reyes N. Accidentes laborales con exposición a fluidos corporales en internos de medicina de Lima Metropolitana. Rev Cient CIMEL. 2001;6:26-30. | Link |
Ramos S, Castillo C, Reyes N. Accidentes laborales con exposición a fluidos corporales en internos de medicina de Lima Metropolitana. Rev Cient CIMEL. 2001;6:26-30. | Link | Tapias LF, Tapias L, Torres S, Vega A, Valencia L, Orosco L. Accidentes biológicos en estudiantes de medicina de la Universidad Industrial de Santander, Bucaramanga, Colombia. Rev Salud UIS. 2007;39(3):192-199. | Link |
Tapias LF, Tapias L, Torres S, Vega A, Valencia L, Orosco L. Accidentes biológicos en estudiantes de medicina de la Universidad Industrial de Santander, Bucaramanga, Colombia. Rev Salud UIS. 2007;39(3):192-199. | Link | Lee JM, Botteman MF, Xanthakos N, Nicklasson L. Needlestick injuries in the United States. Epidemiologic, economic, and quality of life issues. AAOHN J. 2005 Mar;53(3):117-33. | PubMed |
Lee JM, Botteman MF, Xanthakos N, Nicklasson L. Needlestick injuries in the United States. Epidemiologic, economic, and quality of life issues. AAOHN J. 2005 Mar;53(3):117-33. | PubMed | Díaz L, Cadena L. Riesgo de infección por hepatitis B entre estudiantes de medicina peruanos luego de exposición a sangre y líquidos corporales. Rev. de Gastroenterología 2004; 23(2):107-110. | Link |
Díaz L, Cadena L. Riesgo de infección por hepatitis B entre estudiantes de medicina peruanos luego de exposición a sangre y líquidos corporales. Rev. de Gastroenterología 2004; 23(2):107-110. | Link | Ministerio de Salud del Perú. Norma técnica categorías de establecimientos de sector salud. Lima, Perú: MINSA; 2004. | Link |
Ministerio de Salud del Perú. Norma técnica categorías de establecimientos de sector salud. Lima, Perú: MINSA; 2004. | Link | Resolución de Gerencia General N° 1471 “Definición, características y funciones generales de los establecimientos de salud del Seguro Social de Salud (ESSALUD)”. [on line] | Link |
Resolución de Gerencia General N° 1471 “Definición, características y funciones generales de los establecimientos de salud del Seguro Social de Salud (ESSALUD)”. [on line] | Link | Seguro Social de Salud del Perú. Categorizacióndel Hospital Guillermo Almenara Irigoyen de EsSalud. [on line]. | Link |
Seguro Social de Salud del Perú. Categorizacióndel Hospital Guillermo Almenara Irigoyen de EsSalud. [on line]. | Link | Seguro Social de Salud del Perú. Centros AsistencialesEsSalud. Hospital III Emergencias Grau - La Victoria. [on line]. | Link |
Seguro Social de Salud del Perú. Centros AsistencialesEsSalud. Hospital III Emergencias Grau - La Victoria. [on line]. | Link | The Centers for Disease Control and Prevention (CDC). Sharps Injury Prevention Workbook. [on line]. | Link |
The Centers for Disease Control and Prevention (CDC). Sharps Injury Prevention Workbook. [on line]. | Link | U.S. Public Health Service. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001 Jun 29;50(RR-11):1-52. | PubMed |
U.S. Public Health Service. Updated U.S. Public Health Service Guidelines for the Management of Occupational Exposures to HBV, HCV, and HIV and Recommendations for Postexposure Prophylaxis. MMWR Recomm Rep. 2001 Jun 29;50(RR-11):1-52. | PubMed | Loscos L, Colomer R, Marco Ú, Bel R. Actitud a seguir en el caso de accidente biológico. MEDIFAM. 2002;12(9):538-549. | Link |
Loscos L, Colomer R, Marco Ú, Bel R. Actitud a seguir en el caso de accidente biológico. MEDIFAM. 2002;12(9):538-549. | Link | Flores C, Samalvides F. Conocimientos sobre bioseguridad en estudiantes de medicina de una universidad peruana. Rev Méd Hered. 2005;16(4):253-259. | Link |
Flores C, Samalvides F. Conocimientos sobre bioseguridad en estudiantes de medicina de una universidad peruana. Rev Méd Hered. 2005;16(4):253-259. | Link | U.S. Public Health Service. Public Health Service Guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001 Jun 29;50(RR-11):1-52. | PubMed |
U.S. Public Health Service. Public Health Service Guidelines for the management of occupational exposures to HBV, HCV, and HIV and recommendations for postexposure prophylaxis. MMWR Recomm Rep. 2001 Jun 29;50(RR-11):1-52. | PubMed | Boletín epidemiológico: Vigilancia epidemiológica de accidentes ocupacionales en el año 2013. Lima, Perú: Hospital Nacional Dos de Mayo; 2013. | Link |
Boletín epidemiológico: Vigilancia epidemiológica de accidentes ocupacionales en el año 2013. Lima, Perú: Hospital Nacional Dos de Mayo; 2013. | Link | Tanner J, Parkinson H. Double gloving to reduce surgical cross-infection. Cochrane Database Syst Rev. 2006 Jul 19;(3):CD003087. | CrossRef | PubMed |
Tanner J, Parkinson H. Double gloving to reduce surgical cross-infection. Cochrane Database Syst Rev. 2006 Jul 19;(3):CD003087. | CrossRef | PubMed | Galán E, Díaz C, Maguiña C, Villena J. Bioseguridad durante el internado de medicina en hospitales de Trujillo-La Libertad 2010: a propósito de la muerte de un estudiante de medicina. Acta Med Per. 2010;27(2):119-122. | Link |
Galán E, Díaz C, Maguiña C, Villena J. Bioseguridad durante el internado de medicina en hospitales de Trujillo-La Libertad 2010: a propósito de la muerte de un estudiante de medicina. Acta Med Per. 2010;27(2):119-122. | Link | Bartlett J, Weber D. Management of healthcare personnel exposed to HIV. UpToDate. 2012:1-26. | Link |
Bartlett J, Weber D. Management of healthcare personnel exposed to HIV. UpToDate. 2012:1-26. | Link |