 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: very low birth weight infants, brain damage, sepsis, child development, newborn, preterm infant
INTRODUCTION
Neonatal sepsis has been associated with poor neurodevelopmental outcome in very low birth weight infants (VLBW infants). The impact of neonatal sepsis on neurodevelopment in very low birth weight infants discharged from Cuban neonatal intensive care units is unknown.
OBJECTIVE
To determine the impact of neonatal sepsis as a risk factor of neurodevelopmental disorders in a Cuban very low birth weight infants’ population.
METHODS
A cohort study was carried out that enrolled 89 infants with birth weight less than 1500 g who were admitted during the period 2006-2010 to the Teaching Provincial Gynecological and Obstetrical Hospital of Matanzas. All patients were followed-up at the outpatient clinic until two years of corrected gestational age. Then they were divided into two groups: those who had been diagnosed with neonatal sepsis (n=19) and those who had not (n=70). The association power of neonatal sepsis with neurodevelopmental disorders was determined with calculation of relative risk (RR) and their confidence intervals at 95% (CI95%). A multivariate analysis with logistic regression enabled us to compare sepsis with other neonatal variables as risk factors.
RESULTS
Very low birth weight infants with neonatal sepsis had an increased risk of neurodevelopmental disorders (47.4 vs 17.1%; RR 2.7 CI95% 1.3-5.5; p=0.005). This risk was significant after correction for other variables (male sex, mechanical respiratory assistance, bronchopulmonary dysplasia and hyperbilirrubinemia >15 mg/dl) (odds ratio 4.0; CI95% 1.1-14.3; p=0.03).
CONCLUSION
Neonatal sepsis should be considered an important factor among the multiple events related to poor neurodevelopmental outcome in the preterm newborn.
Preterm birth is a phenomenon that has reached social dimensions due to growing survival rates of very low birthweight or <1500 grams, and extremely preterm infants (<1000 grams). For instance, in 2010 it was estimated that 15 million of infants were born before 37 gestational weeks worldwide; of whom 13 million survived. From these, 2.7% had moderate or severe neurodevelopmental impairment [1].
Nowadays, survival rate of very low birthweight infants is higher or equal to 90% and between five to 10% of them present motor impairments. Other disabilities occur in between 25 and 50% of cases and involve cognitive and behavior disorders [2]. Cerebral palsy incidence is even higher in extreme preterm infants, with 17 or 19%; according to whether they were less than 26 gestational weeks old or extremely low birthweight [3],[4].
Some of the most important risk factors for the occurrence of neurodevelopmental disorders in very low birthweight infants, and especially in extremely low birth weight infants include male sex, no maternal steroid administration, presence of periventricular leukomalacia, neonatal convulsions, retinopathy of prematurity, bronchopulmonary dysplasia, prolonged mechanical ventilation, persistent ductus arteriosus, postnatal steroids use, malnutrition, extended parenteral nutrition, necrotizing enterocolitis and/or intestinal perforation [5],[6],[7].
Diverse studies have found association between presence of maternal infection, specially clinical or histological chorioamnionitis, and presence of white matter damage or cerebral palsy, in both preterm and at term children [8],[9].
Adverse neurological outcome in preterm infants not only has been associated to the presence of intrauterine maternal infections or chorioamnionitis, but also neonatal sepsis per se. The first two studies which have found a strong association between presence of neonatal infection and worse neurological outcome in extremely preterm infant populations, were published only few years ago [10],[11].
Bacterial infections continue being an important cause of morbidity and mortality in the neonatal period. About 1.5% of all very low birthweight infants present early-onset sepsis and until about 21% present late-onset sepsis, with a mortality rate between 10 and 30%, even when incidences varies from regions and years [12].
Most studies that have evaluated neonatal sepsis association with neurodevelopmental sequels have been carried out in developed countries [12],[13]. None of the studies published in Cuba about the relationship between factors that take place in the neonatal period and neurodevelopment in very low birthweight infants [14],[15],[16], has been focused in the role of neonatal sepsis as a risk factor of the occurrence of neurodevelopmental disorders, despite the high neonatal sepsis incidence in this neonatal group, as reported by some studies performed in this country [17],[18].
As expressed here, it is inferred that the impact of neonatal sepsis on neurodevelopment in very low birth weight infants discharged from Cuban neonatal intensive care units is unknown, being Cuba a developing country that has achieved low infant mortality rates.
The Teaching Provincial Gynecological and Obstetrical Hospital of Matanzas Dr. Julio Alfonso Medina is located in the capital city of the same name province, and constitutes a reference center for management of infants born under 1,500 grams. A neurodevelopment follow-up program is carried out in the outpatient clinic of this center, where high neurological risk infants are evaluated during the first years of life with a method described in other works [19].
Beginning with the hypothesis that neonatal sepsis seems to be a risk factor associated with poor neurodevelopmental outcome in very low birth weight infants, we made this research work, with the main aim of determining the impact of neonatal sepsis as a risk factor of neurodevelopmental disorders in very low birthweight infants discharged alive from a Cuban tertiary hospital.
A cohort study including 89 infants with birth weight <1500 g was carried out. Infants were born during the period 2006-2010 in the Province of Matanzas and were discharged alive from the Teaching Provincial Gynecological and Obstetrical Hospital of Matanzas Dr. Julio Alfonso Medina. All patients were born with less than 37 weeks of gestational age (according to last menstrual period, ultrasound fetal measurements at the beginning of pregnancy or modified Ballard score in absence of the former); and were followed-up in a neurodevelopment program at the outpatient clinic of this center until 24 months of corrected gestational age (months age beginning at term of gestation, for 40 weeks gestation estimation).
Major malformations, hereditary syndromes, neonatal and post neonatal deaths were excluded from the study.
The study sample was constituted by 89 very low birthweight infants out from a total of 134 newborns with birth weight <1500 grams, born in the Province of Matanzas during the period 2006-2010. Ninety of them were born in the Teaching Provincial Gynecological and Obstetrical Hospital of Matanzas Dr. Julio Alfonso Medina. The rest were referred to this center during the neonatal period from other hospitals of the province. Out of 134 newborns with birth weight <1500 grams, 26 resulted in neonatal deaths. Thus, 108 were discharged alive. Four of them were excluded from the study due to major malformations, hereditary syndromes and post neonatal deaths; and 104 entered the follow-up program. Eighty nine of them completed the follow-up until two years of corrected gestational age, so they constituted the study sample.
Study groups
With the 89 patients who met the study criteria, two groups were conformed: one group of neonatal sepsis (exposed), composed by those who had been diagnosed with clinical sepsis during neonatal period (n=19); and a second group without sepsis (not exposed), composed by patients who did not have sepsis during neonatal period (n=70).
For neonatal sepsis diagnosis Haque KN criteria were taken into account [20], which include clinical, hemodynamic, perfusion tissue and inflammatory variables, with the exception that the last ones included neither C-reactive protein values, procalcitonin nor interleukines 6 or 8, because they are not routinely used in the center where the research wotk took place.
Sepsis was considered proven when any germ species was isolated from blood cultures, but when these cultures were not carried out or were negative; it was considered not proven sepsis. In this work were included both, proven and not proven neonatal sepsis.
Besides variables involved on Haque KN criteria (leukocytosis>34,000x109/l, leukopenia<5,000x109/l, immature neutrophils >10%, ratio of immature over total neutrophils ≥0.2 and thrombocytopenia <100,000x109/l), there were other contained on Rodwell et al criteria [21] that were taken into account for including patients in the neonatal sepsis group. Those were: presence of leukocytosis (≥25,000x109/l at birth or ≥30,000x109/l between 12-24 hours of postnatal period, or ≥21,000x109/l beyond 48 hours of postnatal period), neutrophilia or neutropenia, increased neutrophilic index, ratio of immature over segmented neutrophils ≥ 0.3 and presence of neutrophils with toxic granulation and vacuolization.
The neonatal sepsis group involved not only patients without localized neonatal sepsis, but also those who presented a localized infection plus two or more signs of systemic inflammatory response, established by international consent as criteria for neonatal systemic inflammatory response syndrome. These signs were: presence of heart rate abnormalities (>180 or <100 beats per minute), respiratory rate abnormalities (>50 breaths per minute in neonates during the first week of life or <40 per minute between eight and 30 days of life), temperature disturbances (<36 o >38.5 °C), total leukocyte count abnormalities (>34 000 in the first week of life or >19,500 o <5,000 between eight and 30 days of life), and presence of band cells (>10% of total leukocyte count) [22].
Research stages:
This research had three stages:
Studied variables
Any deviation from normal neurodevelopment during the first 24 months of corrected gestational age, demonstrated by neurological exam, Bayley scale II [23] or neurophysiologic tests was considered a neurodevelopmental disorder.
In the neurodevelopmental outcome classification during the first two years of corrected age, other categories were used. They were:
Cerebral palsy was considered by the presence of a permanent or chronic motor function disorder, originated on brain or cerebellum, with early onset, attributed to non-progressive disturbances in a child with a minimum of two years of age at the time of evaluation [24]. Severe and bilateral visual disability was defined as the impossibility for useful vision on both eyes. Mild or unilateral blindness was considered as a visual acuity diminished in one or both eyes, not making impossible the total visual function. Deafness was considered bilateral and severe when audition by both ears was impossible and patients required amplification in order to hear; and unilateral and mild, when the hearing impossibility affected only one ear, or diminished hearing capacity did not require any amplification equipment to reach the audition function.
Independent variables included in bivariate analysis were: male sex (versus female), birth weight (grams), gestational age (according to last menstrual period, or by default, foetal ultrasound at the beginning of pregnant or neonatal exam by modified Ballard score), low birthweight for gestational age (birth for gestational age less than the 10th percentile according to Dueñas curves et al. [25]), low Apgar score at first and fifth minute (score 0-6), mode of delivery (vaginal vs. caesarean section), respiratory distress syndrome, bronchopulmonary dysplasia, (present when, at least at 28 days of postnatal age, patient requires oxygen therapy) [26], not physiologic hyperbilirubinemia (presence of total serum bilirubin levels ≥15 mg/dl or 256.5 μmol/l), antenatal steroids use (one or more doses) and mechanical ventilation (conventional or high frequency ventilation).
Neonatal sepsis were classified, according to the onset of symptoms and signs, in early (onset during the first 72 hours of life), late (onset beyond 72 hours after birth), and early sepsis with late re-infection (when sepsis appear during the first 72 hours of life and after that another sepsis emerges).
On the final analysis, corresponding to exposition level to sepsis and its association with presentation of neurodevelopmental disorders, the variable “neonatal sepsis episodes” was classified in three categories: without sepsis, one sepsis episode and more than one sepsis episode (independently of time of its onset).
Follow-up
All infants underwent a neurological exam at term (when they reached 38 to 42 weeks, corrected gestational age), by means of the methods of Amiel Tison et al., Prechtl and Fenichel [14],[19]. At that moment they were classified in one of the following categories:
All patients were examined during the first year of corrected age at the first, second, third, sixth, ninth and twelfth month, and during each trimester of the second year. Each one underwent neurologically assessment by Amiel-Tison method [14],[19] during the first year. Classic neurological exam was used during the second year.
Psychomotor and mental assessment was carried out by means of Bayley scale II [23], which was applied at the end of the first and the second year of corrected age. Clinical follow-up was completed using brain ultrasound series at first month, end of the third and sixth month of corrected age; as well as brainstem auditory evoked potentials.
Data collection
Data about perinatal evolution of patients were obtained from maternal and neonatal charts. That information and the one obtained during follow-up were summarized in a data collection form.
Statistical analysis
All the above information was entered in a database using statistic package SPSS version 17.0, with which all the statistical processing was performed. To achieve the objective of the first stage of this research, relative risk (RR) and its 95% confidence interval was the main measure. In a similar way, the association between neonatal sepsis and specific neurodevelopmental disorders was evaluated.
In the second stage of the study, to select candidate variables to be included further in the logistic regression model, media and standard deviation were used as summary measures of continuous quantitative variables. Absolute and relative frequencies were used for qualitative variables. In the bivariate analysis, Chi square or Fisher exact tests were applied for nominal qualitative variables, the latter when expected frequencies were less than five or if they were equal to cero. With quantitative variables, t-test was applied for comparison of media between two populations. For all the cases, p value <0.05 was considered significant.
Afterward, a logistic regression analysis was performed. In this analysis, odds ratios (OR) and their 95% confidence intervals were calculated by means of the omnibus test. All p values <0.05 were considered significant. Previous to logistic regression analysis, a collinearity analysis among independent covariates candidates to be included in the former was performed, with the Pearson correlation coefficient. Covariates included in the logistic regression analysis were chosen under the principle that there was not a high correlation between them. Thus, when a Pearson correlation coefficient of any pair of variables was over 0.5, only the most important of both was selected, according to literature review and objectives of the study. Hence, covariate mechanical ventilation was selected and respiratory distress syndrome and use of surfactant were excluded, due to the high correlation between the last two and the former.
So, in the logistic regression model were included four covariates resulting from the above explained selection: neonatal sepsis, mechanical ventilation, not physiologic hyperbilirubinemia and bronchopulmonary dysplasia; and also male sex. Presence of a neurodevelopmental disorder was included in the model as the dependent variable.
To determine association between the moment of sepsis onset and the presentation of neurodevelopmental disorders, the categories early neonatal sepsis, late neonatal sepsis and early sepsis with late re-infection were managed as dummy variables.
Finally, to determine a possible dose-response relation between neonatal sepsis episodes and occurrence of neurodevelopmental disorders, RR and 95% confidence intervals were calculated for each category.
Ethical aspects
Patients’ enrollment on the follow-up study was performed under informed parental consent. Parents were free to abandon the study whenever they wanted. The research work was approved by institutional board and ethics committee on research of the center.
Table 1 presents general characteristics of 89 very low birthweight infants included in this study, in which female sex was predominant. The mean value for birthweight was 1,278 grams (minimum 700 and maximum 1,490 grams) and for gestational age was 31.4 weeks (minimum 26 and maximum 36 weeks). Neonates with <1000 grams were nearly 8%. Most infants had a normal Apgar score and about 40% received some mode of mechanical ventilation. Neonatal sepsis was present in 21.3% of studied infants.
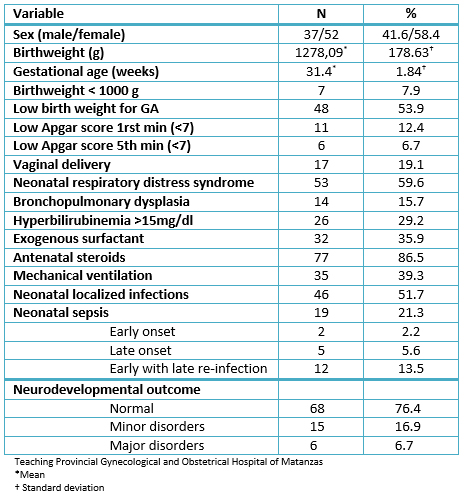
Table 1: General characteristics of very low birthweight infants included in the study (N=89).
When analyzing neonatal sepsis association with neurodevelopmental disorders occurrence on the first two years of corrected age, it was observed that risk of neurodevelopmental disorders was greater in very low birthweight infants presenting neonatal sepsis than in those who did not present sepsis (47.4 versus 17.1%; RR 2.7 95% CI: 1.3-5.5; p=0.005).
Results about neurodevelopment of studied infants, according to having or not sepsis, are shown in detail in Table 2. According to this analysis, neonatal sepsis was associated to a higher risk of major neurodevelopmental disorders, even when this association was not significant. Meanwhile, neonatal sepsis association with increased risk of minor neurodevelopmental disorders resulted significant.
Table 2 also shows the frequency and risk of occurrence of specific neurodevelopmental disorders in studied patients. Patients with neonatal sepsis presented an increased risk of cerebral palsy, moderate to severe motor developmental delay (PDI<70) and moderate to severe mental developmental delay (MDI<70), but these associations were not statistically significant. About minor disorders, the same table highlights neonatal sepsis was significantly associated to a higher risk of mild or transitory hypotonia and mild or transitory motor developmental delay, while it was not significantly associated to mild or unilateral visual disability.
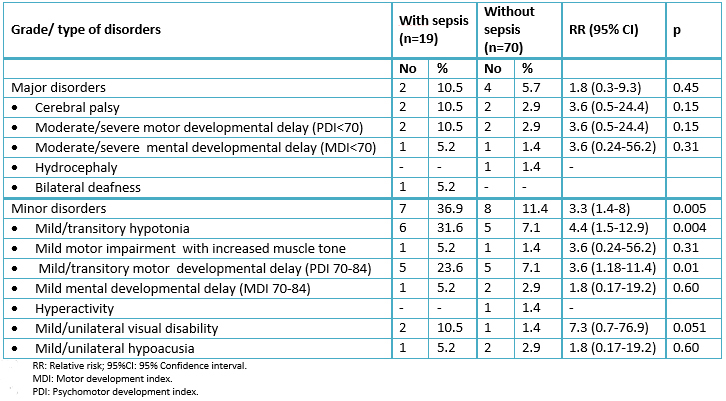
Table 2: Developmental disorders during the first two years of corrected age found in the studied infants (N=89).
Table 3 shows the main results of bivariate risks analysis, with which the association between some variables and neonatal sepsis was ascertained. From analyzed variables, only neonatal respiratory distress syndrome, bronchopulmonary dysplasia, not physiologic hyperbilirubinemia, exogenous surfactant use and mechanical ventilation had a significant association with neonatal sepsis.
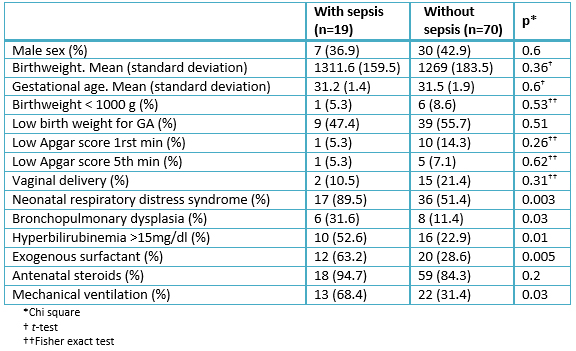
Table 3: Association between studied variables with neonatal sepsis, according to bivariate analysis (N=89).
Results of logistic regression analysis, performed in order to determine independent association between variables included in the model and the presence of neurodevelopmental disorders, are shown in Table 4. This analysis showed that neonatal sepsis was the only significant variable associated to a four-fold increase in the risk of neurodevelopmental disorders. Mechanical ventilation in neonatal period and bronchopulmonary dysplasia were associated to an increased risk of neurodevelopmental disorders, the same as male sex, but these associations were not significant.
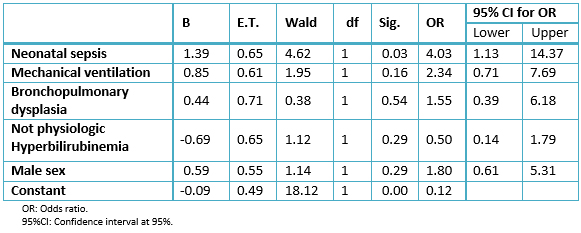
Table 4: Association of neonatal sepsis with the presence of neurodevelopment disorders, according to logistic regression analysis (N=89; cases=21, controls=68).
When the above risk analysis was carried out, but now including the type of neonatal sepsis instead of the covariate neonatal sepsis, result was early neonatal sepsis with late re-infection was associated to significant increase on the risk of neurodevelopmental disorders (odds ratio 4.5 95% CI: 1.02-20.3), while late neonatal sepsis was associated to an increased risk, but not significant (odds ratio 7.5, 95% CI: 0.82-69.5). Early neonatal sepsis, when occurred alone, was not associated to neurodevelopmental disorders.
Finally, the association between exposure number to neonatal sepsis episodes and neurodevelopmental disorders occurrence was analyzed. As a result, it was found that the higher the number of exposures to sepsis episodes the greater the risk of neurodevelopmental disorders, as shown in Figure 1.
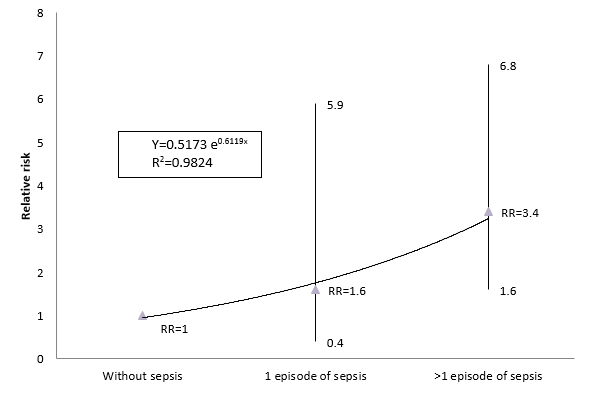
Figure 1: Risk of neurodevelopmental disorders according to neonatal sepsis episode number. Relative risk and confidence interval.
Characteristics of study sample
Among total of very low birthweight infants enrolled in this study, 23.5% presented disorders during their neurodevelopment in the first two years of corrected age, very similar result as that reported by Moll et al. in Germany [27], but differs from those obtained in other studies. Two of them [5],[28], show lower percent of neurodevelopmental disorders than this; while the other [16] was higher, with 38% of sequels.
Percentage of major disorders found in this study is on the range of that found in other studies of foreign authors (between 19 and 25%) [29],[30].
If some characteristics of the population enrolled in this work (Table 1) are compared with those of a multicenter study performed in Spain [5], it is remarkable that in our study the percentage of infants with birthweight <1000 grams is lower, just as the frequencies of Apgar score <7 and exogenous surfactant use; although the frequencies of antenatal steroids use and bronchopulmonary dysplasia are higher. In relation to other studies made in the United Kingdom and Switzerland, in ours the frequency of presentation of infection was higher [31],[32].
Incidence of neonatal sepsis in very low birthweight infants
Global incidence of neonatal sepsis in developed countries is between one and 12 per 1000 live births, although in developing countries it reaches higher figures as 20 to 30% of all live births. Risk of neurodevelopmental sequels is greater in infants with sepsis, but if they are of very low birthweight, the risk is even higher [33].
Birth weight–specific incidence rate of neonatal sepsis in infants with birthweight <1,500 grams during the study period in the center where this research took place, was 33% (data obtained from Medical Register Department and Morbidity Register from the Neonatology Service of the Teaching Provincial Gynecological and Obstetrical Hospital of Matanzas Dr. Julio Alfonso Medina). Comparing these figures to the incidence of neonatal sepsis reported in studies carried out in developed countries [32],[34],[35], where neonatal sepsis is found between 9.8 and 31.7% of all infants with <1500 grams, it is obvious that incidence in this center is much higher.
Incidence of sepsis in this study refers to proven as well as not proven sepsis. This could influence some results of this study like early onset sepsis had higher incidence than late onset sepsis, conversely to what most studies refer. An Australian study shows how, when considering not proven or clinical sepsis, frequency of early onset is higher than the late onset one (32 versus 26.6%); while when only proved sepsis are considered, occurs the contrary (1.3 versus 17.4%) [35].
Neonatal sepsis and neurodevelopmental disorders
The association between neonatal sepsis and greater risk of neurodevelopmental disorders has been found in multiple studies in very low birthweight infants or with gestational age <34 weeks, and with birthweight <1000 grams or <28 weeks [12],[31],[33],[36],[37],[38]. Most of those studies have been carried out on high or middle income nations. Risk of neurodevelopmental disorders at two years of corrected age in very low birthweight and extremely low birthweight infants with neonatal sepsis, is nearly two to three fold greater than the risk in neonates of the same weight range without neonatal sepsis (odds ratio 2.09; 95% CI:1.65-2.65) [12],[13]. Relative risk to present neurodevelopmental disorders in the first two years of corrected age in very low birthweight infants with neonatal sepsis, compared with those without sepsis, in this study was on the range reported by these authors [12],[13],[33].
Sepsis with or without meningitis is associated to an increment of two to 10 fold in the risk of cerebral palsy [12],[33],[39], a fact that has been also demonstrated in some studies performed in Cuba [40],[41].
Adverse neurological outcome associated to sepsis in neonatal survivors born with very low birthweight, has been stated not only in relation to the occurrence of cerebral palsy and other neuromotor impairments, but also to the occurrence of intellectual developmental disorders (mental retardation or cognitive impairment) [12],[37], although results about this last group of disorders are controversial [9],[36],[38].
In the study of the National Institute of Child Health and Human Development Neonatal Research Network, in United States, very low birthweight infants with infection had greater risk for microcephaly, cerebral palsy, psychomotor developmental index and mental developmental index <70 and visual impairment [11]. These results have been corroborated by a recent meta-analysis [33], which shows that very low birthweight infants and with gestational age <34 weeks who present neonatal sepsis have greater risk of cerebral palsy (RR 2; 95% CI: 1.7-2.3), cognitive delay (RR 1.6; 95% CI: 1.4-1.8), psychomotor delay (RR 1,9; 95% CI: 1,5-2,3), visual impairment (RR 2.2; 95% CI: 1.6-3.2) and auditory impairment (RR 3.2; 95% CI: 2.3- 4.4).
Other meta-analysis has shown an average decrease equivalent to 3.75 and 5.55 in mental development index and psychomotor development index, respectively, in very low birthweight or very preterm infants with perinatal infections, when they were compared with infants of the same weight range and gestational age, but who have not had this type of infections [9]. Neonatal infections (sepsis, necrotizing enterocolitis and meningitis), all together, attaches an additional risk to that in extremely low birthweight infants with three morbidities like bronchopulmonary dysplasia, brain injury and retinopathy of prematurity, with respect to their adverse outcomes (death or neurological impairments) on the first 18 months of corrected age [10].
In the present study, the greater risk of neurodevelopmental disorders in patients with neonatal sepsis resulted statistically significant only for all neurodevelopmental disorders together and for minor disorders, but not for major disorders. This result could be explained by the low potency of the study when low frequency phenomena were analyzed, compared with results obtained in other multicenter collaborative studies or meta-analysis [5],[9],[13],[29],[33].
Other probable explanation for this feature could be related to pathogenesis of brain injury in the preterm infant. From some years ago, the hypothesis of multiple hits on the occurrence of brain damage has been stated, especially in preterm infants [3]. Neonatal sepsis acts as one of the latest links of the causal events chain for neurodevelopmental disorders. For this reason its effect, on the case of major disorders, could be considered a worsening factor beginning with a pre-established antenatal damage. These antenatal factors have not been analyzed in this study, but it has been demonstrated they have a major contribution on the occurrence of cerebral palsy and other disorders of neurodevelopment [42],[43]. However, in the case of minor disorders, the effect of neonatal sepsis could be considered closer in the chain of events that could yield these disorders, all which could imply that the latter association was easier to demonstrate statistically.
Anyway, the results of this study show that sepsis per se constituted a perinatal risk factor of the occurrence of neurodevelopmental disorders in very low birthweight infants, which corroborated results of other studies [12],[13],[33],[36],[37],[38]. The sepsis episodes in preterm infants are associated to periventricular leukomalacia, which results in neurological abnormalities between 12 and 14 months in about 90% of these infants [39].
Type of sepsis and neurodevelopmental disorders
In the present study, early onset sepsis with late re-infection was associated to increased risk of neurodevelopmental disorders, which is coincident with the results of Mitha et al. in one study performed in France [44]. Also, it has been found a significant association of late onset sepsis with an increased risk of neurological sequels [12],[38],[44], which was found in this study, even when was not significant. Nevertheless, the association of type of neonatal sepsis, according to its time of onset, with the presence of neurodevelopmental disorders in very low birthweight infants still results controversial [5].
The association between infection by specific etiological agents and the occurrence of neurological sequels has been studied too. This association has been significant for late onset sepsis by gram positive bacteria [38], as well as fungal systemic infections [45].
But in this study such association was not assessed. Association between number of sepsis episodes and the results of neurodevelopment in very low birthweight infants was evaluated (Figure 1), and a dose-response relation between occurrence of neurological sequels and a growing exposition to sepsis episodes, independently of the time of onset of sepsis. This is a remarkable feature, which is in accordance with the work of Glass et al., where exposition to multiple episodes of proven infection increases the risk of progressive white matter damage [46].
The main strength of this study is its contribution with epidemiological evidence over time, to demonstrate the probable causal relationship between neonatal sepsis and neurodevelopmental disorders in very low birthweight infants. Moreover, this contribution takes place in the context of a developing country. Nonetheless it is necessary to accumulate more experimental evidence, in order to demonstrate this relationship, because the study sample was small. That constituted a limitation when anybody wishes extrapolates results, particularly in events of low presentation frequency.
The strength of the association of neonatal sepsis with adverse neurodevelopmental outcomes in very low birth weight infants found in this study was similar to that from other studies performed in developed countries. Neonatal sepsis should be considered an important cause, among the multiple events of brain damage in the preterm newborn. It is possible that incidence of neurodevelopmental sequels in very low birth weight infants could be diminished with implementation of more effective interventional measures aimed at prevention of neonatal sepsis.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
Patients’ enrollment on the follow-up study was performed under informed parental consent. Parents were free to abandon the study whenever they wanted. The research work was approved by institutional board and ethics committee on research of the center.
Conflicts of interest
The authors completed the ICMJE conflict of interest declaration form, translated into Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare there were no financing from external sources.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Neonatal sepsis has been associated with poor neurodevelopmental outcome in very low birth weight infants (VLBW infants). The impact of neonatal sepsis on neurodevelopment in very low birth weight infants discharged from Cuban neonatal intensive care units is unknown.
OBJECTIVE
To determine the impact of neonatal sepsis as a risk factor of neurodevelopmental disorders in a Cuban very low birth weight infants’ population.
METHODS
A cohort study was carried out that enrolled 89 infants with birth weight less than 1500 g who were admitted during the period 2006-2010 to the Teaching Provincial Gynecological and Obstetrical Hospital of Matanzas. All patients were followed-up at the outpatient clinic until two years of corrected gestational age. Then they were divided into two groups: those who had been diagnosed with neonatal sepsis (n=19) and those who had not (n=70). The association power of neonatal sepsis with neurodevelopmental disorders was determined with calculation of relative risk (RR) and their confidence intervals at 95% (CI95%). A multivariate analysis with logistic regression enabled us to compare sepsis with other neonatal variables as risk factors.
RESULTS
Very low birth weight infants with neonatal sepsis had an increased risk of neurodevelopmental disorders (47.4 vs 17.1%; RR 2.7 CI95% 1.3-5.5; p=0.005). This risk was significant after correction for other variables (male sex, mechanical respiratory assistance, bronchopulmonary dysplasia and hyperbilirrubinemia >15 mg/dl) (odds ratio 4.0; CI95% 1.1-14.3; p=0.03).
CONCLUSION
Neonatal sepsis should be considered an important factor among the multiple events related to poor neurodevelopmental outcome in the preterm newborn.
 Autores:
Gerardo Rogelio Robaina Castellanos[1], Solangel de la Caridad Riesgo Rodríguez[2]
Autores:
Gerardo Rogelio Robaina Castellanos[1], Solangel de la Caridad Riesgo Rodríguez[2]

Citación: Robaina Castellanos GR, Riesgo Rodríguez SC. Neonatal sepsis and neurodevelopment in very low birth weight infants in Matanzas, Cuba 2006-2010: a prospective cohort study. Medwave 2016 Abr;16(3):e6422 doi: 10.5867/medwave.2016.03.6422
Fecha de envío: 26/1/2016
Fecha de aceptación: 24/3/2016
Fecha de publicación: 7/4/2016
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Blencowe H, Lee AC, Cousens S, Bahalim A, Narwal R, Zhong N, et al. Preterm birth-associated neurodevelopmental impairment estimates at regional and global levels for 2010. Pediatr Res. 2013 Dec;74 Suppl 1:17-34. | CrossRef | PubMed |
Blencowe H, Lee AC, Cousens S, Bahalim A, Narwal R, Zhong N, et al. Preterm birth-associated neurodevelopmental impairment estimates at regional and global levels for 2010. Pediatr Res. 2013 Dec;74 Suppl 1:17-34. | CrossRef | PubMed | Robaina Castellanos GR, Riesgo Rodríguez SC. La encefalopatía de la prematuridad: una entidad nosológica en expansión. Rev Cub Pediatr. 2015 Apr-Jun;87(2):224-40. | Link |
Robaina Castellanos GR, Riesgo Rodríguez SC. La encefalopatía de la prematuridad: una entidad nosológica en expansión. Rev Cub Pediatr. 2015 Apr-Jun;87(2):224-40. | Link | Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR; EPICure Study Group. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed. 2005 Mar;90(2):F134-40. | PubMed |
Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR; EPICure Study Group. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed. 2005 Mar;90(2):F134-40. | PubMed | Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993-1994. Pediatrics. 2000 Jun;105(6):1216-26. | PubMed |
Vohr BR, Wright LL, Dusick AM, Mele L, Verter J, Steichen JJ, et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993-1994. Pediatrics. 2000 Jun;105(6):1216-26. | PubMed | García P, San Feliciano L, Benito F, García R, Guzmán J, Salas S, et al. [Outcome at two years corrected age of a cohort of very low birth weight infants from hospitals within the neonatal SEN1500 network]. An Pediatr (Barc). 2013 Nov;79(5):279-87. | CrossRef | PubMed |
García P, San Feliciano L, Benito F, García R, Guzmán J, Salas S, et al. [Outcome at two years corrected age of a cohort of very low birth weight infants from hospitals within the neonatal SEN1500 network]. An Pediatr (Barc). 2013 Nov;79(5):279-87. | CrossRef | PubMed | Neubauer AP, Voss W, Kattner E. Outcome of extremely low birth weight survivors at school age: the influence of perinatal parameters on neurodevelopment. Eur J Pediatr. 2008 Jan;167(1):87-95. | PubMed |
Neubauer AP, Voss W, Kattner E. Outcome of extremely low birth weight survivors at school age: the influence of perinatal parameters on neurodevelopment. Eur J Pediatr. 2008 Jan;167(1):87-95. | PubMed | Kugelman A, Bader D, Lerner-Geva L, Boyko V, Levitzki O, Riskin A, et al. Poor outcomes at discharge among extremely premature infants: a national population-based study. Arch Pediatr Adolesc Med. 2012 Jun 1;166(6):543-50. | CrossRef | PubMed |
Kugelman A, Bader D, Lerner-Geva L, Boyko V, Levitzki O, Riskin A, et al. Poor outcomes at discharge among extremely premature infants: a national population-based study. Arch Pediatr Adolesc Med. 2012 Jun 1;166(6):543-50. | CrossRef | PubMed | Martinelli P, Sarno L, Maruotti GM, Paludetto R. Chorioamnionitis and prematurity: a critical review. J Matern Fetal Neonatal Med. 2012 Oct;25 Suppl 4:29-31. | CrossRef | PubMed |
Martinelli P, Sarno L, Maruotti GM, Paludetto R. Chorioamnionitis and prematurity: a critical review. J Matern Fetal Neonatal Med. 2012 Oct;25 Suppl 4:29-31. | CrossRef | PubMed | van Vliet EO, de Kieviet JF, Oosterlaan J, van Elburg RM. Perinatal infections and neurodevelopmental outcome in very preterm and very low-birth-weight infants: a meta-analysis. JAMA Pediatr. 2013 Jul;167(7):662-8. | CrossRef | PubMed |
van Vliet EO, de Kieviet JF, Oosterlaan J, van Elburg RM. Perinatal infections and neurodevelopmental outcome in very preterm and very low-birth-weight infants: a meta-analysis. JAMA Pediatr. 2013 Jul;167(7):662-8. | CrossRef | PubMed | Bassler D, Stoll BJ, Schmidt B, Asztalos EV, Roberts RS, Robertson CM, et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics. 2009 Jan;123(1):313-8. | CrossRef | PubMed |
Bassler D, Stoll BJ, Schmidt B, Asztalos EV, Roberts RS, Robertson CM, et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics. 2009 Jan;123(1):313-8. | CrossRef | PubMed | Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004 Nov 17;292(19):2357-65. | PubMed |
Stoll BJ, Hansen NI, Adams-Chapman I, Fanaroff AA, Hintz SR, Vohr B, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004 Nov 17;292(19):2357-65. | PubMed | Schlapbach LJ, Aebischer M, Adams M, Natalucci G, Bonhoeffer J, Latzin P, et al. Impact of sepsis on neurodevelopmental outcome in a Swiss National Cohort of extremely premature infants. Pediatrics. 2011 Aug;128(2):e348-57. | CrossRef | PubMed |
Schlapbach LJ, Aebischer M, Adams M, Natalucci G, Bonhoeffer J, Latzin P, et al. Impact of sepsis on neurodevelopmental outcome in a Swiss National Cohort of extremely premature infants. Pediatrics. 2011 Aug;128(2):e348-57. | CrossRef | PubMed | Alshaikh B, Yusuf K, Sauve R. Neurodevelopmental outcomes of very low birth weight infants with neonatal sepsis: systematic review and meta-analysis. J Perinatol. 2013 Jul;33(7):558-64. | CrossRef | PubMed |
Alshaikh B, Yusuf K, Sauve R. Neurodevelopmental outcomes of very low birth weight infants with neonatal sepsis: systematic review and meta-analysis. J Perinatol. 2013 Jul;33(7):558-64. | CrossRef | PubMed | Robaina Castellanos G, Ruiz Tellechea Y, Domínguez Dieppa F, Roca Molina MC, Riesgo Rodríguez S, Berdayes Millián JD. Neurodesarrollo en recién nacidos ventilados con menos de 1 500 gramos. Rev Cubana Pediatr. 2000 Oct-Dic;72(4):267-74. | Link |
Robaina Castellanos G, Ruiz Tellechea Y, Domínguez Dieppa F, Roca Molina MC, Riesgo Rodríguez S, Berdayes Millián JD. Neurodesarrollo en recién nacidos ventilados con menos de 1 500 gramos. Rev Cubana Pediatr. 2000 Oct-Dic;72(4):267-74. | Link | Armas-Guerra D, Oset-Rodríguez GR; Velázquez-Rodríguez G, López-Santiesteban M. Evaluación neurosensorial de neonatos menores de 1500g a los dos años de edad corregida. Ciencias Holguín. 2012;18(1). | Link |
Armas-Guerra D, Oset-Rodríguez GR; Velázquez-Rodríguez G, López-Santiesteban M. Evaluación neurosensorial de neonatos menores de 1500g a los dos años de edad corregida. Ciencias Holguín. 2012;18(1). | Link | Cejas G, Gómez Y, Roca Mdel C, Domínguez F. Neurodevelopment of very low birth weight infants in the first two years of life in a Havana tertiary care hospital. MEDICC Rev. 2015 Jan;17(1):14-7. | PubMed |
Cejas G, Gómez Y, Roca Mdel C, Domínguez F. Neurodevelopment of very low birth weight infants in the first two years of life in a Havana tertiary care hospital. MEDICC Rev. 2015 Jan;17(1):14-7. | PubMed | Cárdenas González L, Méndez Alarcón L, Moreno Vázquez O, Díaz Álvarez M. Morbilidad y mortalidad del recién nacido pretérmino menor de 1 500 gramos. Rev Cubana Pediatr. 2012 Ene-Mar;84(1): 47-57. | Link |
Cárdenas González L, Méndez Alarcón L, Moreno Vázquez O, Díaz Álvarez M. Morbilidad y mortalidad del recién nacido pretérmino menor de 1 500 gramos. Rev Cubana Pediatr. 2012 Ene-Mar;84(1): 47-57. | Link | Alvarado Bermúdez KB, Broughton Ferriol J, Ortega Sardón M, Pina A. Estudio de cinco años sobre recién nacidos de muy bajo peso en el Hospital Provincial de Ciego de Ávila. Medi Ciego. 2011 Jul;17(2):1-8.
| Link |
Alvarado Bermúdez KB, Broughton Ferriol J, Ortega Sardón M, Pina A. Estudio de cinco años sobre recién nacidos de muy bajo peso en el Hospital Provincial de Ciego de Ávila. Medi Ciego. 2011 Jul;17(2):1-8.
| Link | Robaina Castellanos GR, Riesgo Rodríguez SC. Propuesta de programa de seguimiento de recién nacidos de alto riesgo en Cuba. Rev Méd Electrón. 2011 Sep-Oct;33(5):645-655. | Link |
Robaina Castellanos GR, Riesgo Rodríguez SC. Propuesta de programa de seguimiento de recién nacidos de alto riesgo en Cuba. Rev Méd Electrón. 2011 Sep-Oct;33(5):645-655. | Link | Haque KN. Definitions of bloodstream infection in the newborn. Pediatr Crit Care Med. 2005 May;6(3 Suppl):S45-9. | PubMed |
Haque KN. Definitions of bloodstream infection in the newborn. Pediatr Crit Care Med. 2005 May;6(3 Suppl):S45-9. | PubMed | Rodwell RL, Leslie AL, Tudehope DI. Early diagnosis of neonatal sepsis using a hematologic scoring system. J Pediatr. 1988 May;112(5):761-7. | PubMed |
Rodwell RL, Leslie AL, Tudehope DI. Early diagnosis of neonatal sepsis using a hematologic scoring system. J Pediatr. 1988 May;112(5):761-7. | PubMed | Infectología. En: Colectivo de autores. Neonatología. Diagnóstico y tratamiento. La Habana: Ecimed; 2012:278-342.
Infectología. En: Colectivo de autores. Neonatología. Diagnóstico y tratamiento. La Habana: Ecimed; 2012:278-342.  Bayley N. Bayley Scales of Infant Development II. San Antonio, TX: Psychological Corp; 1993.
Bayley N. Bayley Scales of Infant Development II. San Antonio, TX: Psychological Corp; 1993.  Robaina Castellanos GR, Riesgo Rodríguez SC. Etiología de la parálisis cerebral en niños cubanos (Matanzas, años de nacimiento 1996-2002). Bol Med Hosp Infant Mex. 2010 Nov-Dic; 67(6):507-17. | Link |
Robaina Castellanos GR, Riesgo Rodríguez SC. Etiología de la parálisis cerebral en niños cubanos (Matanzas, años de nacimiento 1996-2002). Bol Med Hosp Infant Mex. 2010 Nov-Dic; 67(6):507-17. | Link | Recién nacido de alto riesgo. En: Colectivo de autores. Neonatología. Diagnóstico y tratamiento. La Habana: Editorial Ciencias Médicas; 2012:35-68.
Recién nacido de alto riesgo. En: Colectivo de autores. Neonatología. Diagnóstico y tratamiento. La Habana: Editorial Ciencias Médicas; 2012:35-68.  Giubergia V, Renteria F, Bauer G, González Pena H, Vila F, et al. Seguimiento neumológico de los niños con displasia broncopulmonar al alta de la Unidad de Cuidados Intensivos Neonatal. Parte 1: Epidemiología, fisiopatología y clínica. Arch Argent Pediatr 2013 Abr;111(2):165-72. | Link |
Giubergia V, Renteria F, Bauer G, González Pena H, Vila F, et al. Seguimiento neumológico de los niños con displasia broncopulmonar al alta de la Unidad de Cuidados Intensivos Neonatal. Parte 1: Epidemiología, fisiopatología y clínica. Arch Argent Pediatr 2013 Abr;111(2):165-72. | Link | Moll M, Schöning M, Gölz R, Döbler-Neumann M, Arand J, Krägeloh-Mann I, et al. [2-year follow-up examinations (Bayley II) in infants born at <32 weeks in a German perinatal center]. Klin Padiatr. 2011 Jul;223(4):251-4. | CrossRef | PubMed |
Moll M, Schöning M, Gölz R, Döbler-Neumann M, Arand J, Krägeloh-Mann I, et al. [2-year follow-up examinations (Bayley II) in infants born at <32 weeks in a German perinatal center]. Klin Padiatr. 2011 Jul;223(4):251-4. | CrossRef | PubMed | Orcesi S, Olivieri I, Longo S, Perotti G, La Piana R, Tinelli C, et al. Neurodevelopmental outcome of preterm very low birth weight infants born from 2005 to 2007. Eur J Paediatr Neurol. 2012 Nov;16(6):716-23. | CrossRef | PubMed |
Orcesi S, Olivieri I, Longo S, Perotti G, La Piana R, Tinelli C, et al. Neurodevelopmental outcome of preterm very low birth weight infants born from 2005 to 2007. Eur J Paediatr Neurol. 2012 Nov;16(6):716-23. | CrossRef | PubMed | Escobar GJ, Littenberg B, Petitti DB. Outcome among surviving very low birthweight infants: a meta-analysis. Arch Dis Child. 1991 Feb;66(2):204-11. | PubMed |
Escobar GJ, Littenberg B, Petitti DB. Outcome among surviving very low birthweight infants: a meta-analysis. Arch Dis Child. 1991 Feb;66(2):204-11. | PubMed | Sharma PK, Sankar MJ, Sapra S, Saxena R, Karthikeyan CV, Deorari A, et al. Growth and neurosensory outcomes of preterm very low birth weight
infants at 18 months of corrected age. Indian J Pediatr. 2011 Dec;78(12):1485-90. | CrossRef | PubMed |
Sharma PK, Sankar MJ, Sapra S, Saxena R, Karthikeyan CV, Deorari A, et al. Growth and neurosensory outcomes of preterm very low birth weight
infants at 18 months of corrected age. Indian J Pediatr. 2011 Dec;78(12):1485-90. | CrossRef | PubMed | The Vermont-Oxford Trials Network: very low birth weight outcomes for 1990. Investigators of the Vermont-Oxford Trials Network Database Project. Pediatrics. 1993 Mar;91(3):540-5. | PubMed |
The Vermont-Oxford Trials Network: very low birth weight outcomes for 1990. Investigators of the Vermont-Oxford Trials Network Database Project. Pediatrics. 1993 Mar;91(3):540-5. | PubMed | Rüegger C, Hegglin M, Adams M, Bucher HU; Swiss Neonatal Network. Population based trends in mortality, morbidity and treatment for very preterm- and very low birth weight infants over 12 years. BMC Pediatr. 2012 Feb 22;12:17. | CrossRef | PubMed |
Rüegger C, Hegglin M, Adams M, Bucher HU; Swiss Neonatal Network. Population based trends in mortality, morbidity and treatment for very preterm- and very low birth weight infants over 12 years. BMC Pediatr. 2012 Feb 22;12:17. | CrossRef | PubMed | Bakhuizen SE, de Haan TR, Teune MJ, van Wassenaer-Leemhuis AG, van der Heyden JL, van der Ham DP, et al. Meta-analysis shows that infants who have suffered neonatal sepsis face an increased risk of mortality and severe complications. Acta Paediatr. 2014 Dec;103(12):1211-8. | CrossRef | PubMed |
Bakhuizen SE, de Haan TR, Teune MJ, van Wassenaer-Leemhuis AG, van der Heyden JL, van der Ham DP, et al. Meta-analysis shows that infants who have suffered neonatal sepsis face an increased risk of mortality and severe complications. Acta Paediatr. 2014 Dec;103(12):1211-8. | CrossRef | PubMed | Lean WL, Kamlin CO, Garland SM, Jacobs SE. Stable rates of neonatal sepsis in a tertiary neonatal unit. J Paediatr Child Health. 2015 Mar;51(3):294-9. | CrossRef | PubMed |
Lean WL, Kamlin CO, Garland SM, Jacobs SE. Stable rates of neonatal sepsis in a tertiary neonatal unit. J Paediatr Child Health. 2015 Mar;51(3):294-9. | CrossRef | PubMed | Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N Engl J Med. 2002 Jul 25;347(4):240-7. | PubMed |
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA, et al. Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. N Engl J Med. 2002 Jul 25;347(4):240-7. | PubMed | Ferreira RC, Mello RR, Silva KS. Neonatal sepsis as a risk factor for neurodevelopmental changes in preterm infants with very low birth weight. J Pediatr (Rio J). 2014 May-Jun;90(3):293-9. | CrossRef | PubMed |
Ferreira RC, Mello RR, Silva KS. Neonatal sepsis as a risk factor for neurodevelopmental changes in preterm infants with very low birth weight. J Pediatr (Rio J). 2014 May-Jun;90(3):293-9. | CrossRef | PubMed | Díllí D, Eras Z, Dilmen U, Sakrucu ED. Neurodevelopmental evaluation of very low birth weight infants with sepsis at 18 to 24 months corrected age. Indian Pediatr. 2013 Mar;50(3):327-30. | PubMed |
Díllí D, Eras Z, Dilmen U, Sakrucu ED. Neurodevelopmental evaluation of very low birth weight infants with sepsis at 18 to 24 months corrected age. Indian Pediatr. 2013 Mar;50(3):327-30. | PubMed | Hentges CR, Silveira RC, Procianoy RS, Carvalho CG, Filipouski GR, Fuentefria RN, et al. Association of late-onset neonatal sepsis with late neurodevelopment in the first two years of life of preterm infants with very low birth weight. J Pediatr (Rio J). 2014 Jan-Feb;90(1):50-7. | CrossRef | PubMed |
Hentges CR, Silveira RC, Procianoy RS, Carvalho CG, Filipouski GR, Fuentefria RN, et al. Association of late-onset neonatal sepsis with late neurodevelopment in the first two years of life of preterm infants with very low birth weight. J Pediatr (Rio J). 2014 Jan-Feb;90(1):50-7. | CrossRef | PubMed | Ergaz Z, Ornoy A. Perinatal and early postnatal factors underlying developmental delay and disabilities. Dev Disabil Res Rev. 2011;17(2):59-70. | CrossRef | PubMed |
Ergaz Z, Ornoy A. Perinatal and early postnatal factors underlying developmental delay and disabilities. Dev Disabil Res Rev. 2011;17(2):59-70. | CrossRef | PubMed | Robaina Castellanos GR. Prevalencia y factores de riesgo de parálisis cerebral en Matanzas. La Habana: Editorial Universitaria; 2012. | Link |
Robaina Castellanos GR. Prevalencia y factores de riesgo de parálisis cerebral en Matanzas. La Habana: Editorial Universitaria; 2012. | Link | Robaina Castellanos GR, Riesgo Rodríguez SC. Factores de riesgo independientes de la edad gestacional asociados a parálisis cerebral congénita. Saludarte 2012 Ene-May; 10(1):23-37.
Robaina Castellanos GR, Riesgo Rodríguez SC. Factores de riesgo independientes de la edad gestacional asociados a parálisis cerebral congénita. Saludarte 2012 Ene-May; 10(1):23-37.  Robaina Castellanos GR, Riesgo Rodríguez SC, Robaina Castellanos MS. Parálisis cerebral: ¿Triste herencia o hipoxia al nacer?. Panorama Cuba y Salud. 2014;9(2). | Link |
Robaina Castellanos GR, Riesgo Rodríguez SC, Robaina Castellanos MS. Parálisis cerebral: ¿Triste herencia o hipoxia al nacer?. Panorama Cuba y Salud. 2014;9(2). | Link | Feldman HM, Reiff MI. Clinical practice. Attention deficit-hyperactivity disorder in children and adolescents. N Engl J Med. 2014 Feb 27;370(9):838-46. | CrossRef | PubMed |
Feldman HM, Reiff MI. Clinical practice. Attention deficit-hyperactivity disorder in children and adolescents. N Engl J Med. 2014 Feb 27;370(9):838-46. | CrossRef | PubMed | Mitha A, Foix-L'Hélias L, Arnaud C, Marret S, Vieux R, Aujard Y, Thiriez G, et al. Neonatal infection and 5-year neurodevelopmental outcome of very preterm infants. Pediatrics. 2013 Aug;132(2):e372-80. | CrossRef | PubMed |
Mitha A, Foix-L'Hélias L, Arnaud C, Marret S, Vieux R, Aujard Y, Thiriez G, et al. Neonatal infection and 5-year neurodevelopmental outcome of very preterm infants. Pediatrics. 2013 Aug;132(2):e372-80. | CrossRef | PubMed |