 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: health-related quality of life, hip fracture, surgery, adult population, follow-up, Mexico
INTRODUCTION
Hip fractures are an important cause of morbidity and mortality and one of the main causes of disability in the older population. The lifetime risk for any type of osteoporotic fracture is very high and falls within the range of 40 - 50% in women and 13 - 22% for men. In Mexico, the lifetime likelihood of having a hip fracture at 50 years of age is 8.5% in Mexican women and 3.8% in Mexican men, but this is expected to rise in upcoming years.
AIM
This study aims to report the Health-Related Quality of Life over the first six months after a hip fracture in two public and two private tertiary care hospitals in Mexico City.
METHOD
Changes over time were evaluated through visual observation of each patient's development trajectory using the graphic representation of the EQ-5D global score. The trajectories were grouped by affinity into five levels of progress according to clinical course. The identified descriptive options were analyzed using the multinomial logistic regression model (LR).
RESULTS
One-hundred-and-thirty-six (136) patients with a hip fracture were followed after surgery. Their mean age was 77 ± 10 years. During the first month, mobility, daily activities, and self-care were the most affected. The group aged between 80 and 84 years reported extreme problems regarding anxiety and depression (21%), and those aged between 50 and 74 years described having issues concerning pain and discomfort (27%). At the 6-month follow-up, only those aged > 85 years of age showed worsening of their condition, a high proportion of these ranking at level 3 in mobility, self-care, and anxiety/depression. Toward the end of the follow-up period, this last group reported having extreme problems (being unable to carry out everyday activities) and worsening of their mobility (9.2%) (inability to walk about) (LR test, p = 0.06).
DISCUSSION
Patients with hip fracture showed difficulties in different areas during the first month after surgery, with steady recuperation up to month six. Age was an important factor in the recovery of all evaluated domains. This graphical tool facilitates classification, identification, and monitoring Health-Related Quality of Life in patients with hip fractures.
Hip fractures are an important cause of morbidity and mortality [1] and one of the main causes of disability in the older population. The lifetime risk for any type of osteoporotic fracture is very high and falls within the range of 40–50% in women and 13–22% for men [2].
In Mexico, the lifetime probability of having a hip fracture after 50 years of age was 8.5% in women and 3.8% in men, but this is expected to rise in upcoming years. From 2000–2006, a 24.8% increase in fractures was reported at the Mexican Institute of Social Security (IMSS) in Mexico. Projections for the following decades have been estimated by Johansson and Clark [3],[4]. Demographic changes estimated for Mexico indicate that the annual number of hip fractures will rise from 29,732 in 2005 to 155,874 in 2050. If the age-specific incidence of hip fracture is maintained, the number of hip fractures would increase by a further 46%. [4]
Although all types of fragility fractures are associated with significant pain, decrease of physical and social functionality, and loss of well-being [5],[6], hip fractures account for the most serious disabilities [7],[8],[9]. Nearly one-half of patients with a hip fracture will be permanently disabled and will not regain their independence, and 25% of them will require full-time nursing-home care. About 40% of individuals are unable to walk independently 1 year after hip fracture, 60% have difficulty with at least one essential activity of daily life, and nearly 80% have a limitation in activities such as driving and shopping [10]. Moreover, because it has been identified that an initial fracture greatly increases the risk of subsequent fractures, 5–10% of patients experience a recurrent hip fracture in the next 3 years [11],[12],[13]. In addition, persons sustaining a hip fracture often experience anxiety and depression that leads to a loss of Health-Related Quality of life (HRQOL) and may also increase the risk of subsequent fractures [14],[15].
The economic impact is considerable. A quite conservative estimate of the worldwide direct and indirect annual costs of hip fracture for the year 2050 is US$131.5 billion [16] and the majority of these costs are related with acute and rehabilitative care after the fracture as well as with nursing facilities [17],[18]. For the year 2006, the estimated direct cost of healthcare for acute treatment of hip fractures in Mexico was over US$97 million, an amount similar to the annual expenses incurred in the acquisition of insulin during the same period [19],[3].
Although hip fractures are frequent in Mexico, to our knowledge there has not been any study focusing on HRQOL following a hip fracture in Mexican population. Therefore, the objective of this study was to identify the HRQOL using the European Quality of Life 5 Dimensions Index: EuroQoL-5 Dimensions (EQ-5D) of the first 6 months after a hip fracture in a group of men and women from different institutions in the Mexican healthcare system and to evaluate changes over time during the same period.
This study aims to report the Health-Related Quality of Life (HRQOL) over the first six months after a hip fracture in two public and two tertiary care private hospitals in Mexico City.
A total of 136 patients with a hip fracture were recruited from four different hospitals in Mexico City: two tertiary-care centers of the public healthcare system, including the National Institute of Rehabilitation (INR) of the Ministry of Health (SS) and the Victorio de la Fuente Hospital of the Mexican Institute of Social Security (IMSS), and two private hospitals, the MOCEL Ángeles and Trinidad.
A case series study was designed to include hip fracture cases after undergoing surgery, and HRQOL was measured at 1-, 3- and 6-month follow-up visits, with the subsequent inclusion criteria: men and women aged 50 years and over with a hip fracture sustained from a light fall (fall from standing position) and who underwent a surgical procedure at any of the participating hospitals. Patients suffering from non-union-consolidated fractures or those who rejected the surgical material were excluded from the study.
HRQOL was measured using the EQ-5D descriptive system. This is a generic tool that measures HRQOL based on five dimensions: mobility, self-care, daily activities (work, study, housework, family, leisure time), pain/discomfort, and anxiety/depression. Each dimension or domain is divided into three degrees of severity: no problem; some problem, and a major problem [20],[21]. To fill out the instrument three pollsters were trained; they applied the instrument at three different times: at month one, at month three, and at month six after the fracture. We chose this instrument for its simplicity and ease of application. The Iberic Spanish version was analyzed by a group of experts, who found conceptual, semantic and functional equivalencies between both cultures, and construct and content validation was carried out. [22]. EQ-5D scores were obtained for each time period using the United Kingdom Time Trade-Off algorithm.
Missing values of the degree of severity in each EQ-5D domain were assigned by using a deterministic hot deck method. Hot deck imputation involves replacing missing values of one or more variables for a non-respondent (labeled as “the recipient”) with observed values from a respondent (“the donor”) that is similar to that of the non-respondent regarding characteristics observed by both cases [23]. The procedure was as follows: first, the patients were divided into two groups: Group A comprised patients who completed the descriptive system of the EQ-5D at all of the three moments (One, three, and six months after the hip fracture occurred), and Group B comprised patients with partial data (i.e. those with missing information either in the second, or the third, or in both follow-up interviews). Patients were lost due to change of address or phone number and could not be located.
Sex, surgery type, comorbidity, and age (range, ±5 years) were employed as control fields to match patients from Group A with those in Group B, forming several strata. For each stratum, the most frequent value reported by patients in Group A was imputed to missing information in Group B. In the case of more than one mode being present, we conventionally assigned a value of 2 (i.e. some problem) for that domain [23].
During the course of the study, 89% of the questionnaires were filled out completely, and 11% had at least one answer missing and were completed using the hot deck method.
Conducting the study
Patients with a hip fracture identified and treated at one of the four previously mentioned hospitals were monitored from months one through six following surgery. During the admission process, patients and family members were interviewed in order to obtain sociodemographic and clinical data, which were corroborated by reviewing clinical files. The questionnaire was administered over the telephone for all patients included, obtaining responses for months one, three, and six following surgery. The EQ-5D was applied to each individual in order to obtain information about HRQOL throughout the follow-up period.
We had two study groups: for the first group, 72% of cases, we applied the EQ-5D by telephone six months after surgery and we asked patients to remember how they felt at months one and three in terms of the HRQOL instrument regarding difficulties in carrying out activities. The remaining 28% of patients were evaluated prospectively during months one, three, and six post-surgery by telephone.
Central tendency, dispersion measurements, and relative frequencies were utilized to describe sociodemographic variables such as age, sex, education, place of residency, and work; as well as to identify the distribution of each of the dimensions over time.
By means of visual observation, the individual development trajectories of each patient were followed and the EQ-5D global score was represented graphically over time. These trajectories were then grouped by affinity into five levels of progress according to the patient’s clinical course: “progressive and sustained improvement”; “early and continuous improvement”; “slow improvement”; “same or no improvement”, and “worse”.
To estimate differences among EQ-5D domains over time, the McNemar test was calculated with a < 0.05 significance level.
The variables measured were the following: age, sex, hospital of origin, type of surgery, marital status, schooling, comorbidities, and hospital readmission.
We stratified the following variables for their analysis: age in two groups with the first group between 50 and 70 years of age (23%), and the second group, ≥71 years (77%); public (86.7%) and private (13.3%) institution, and surgery type, arthroplasty/hemiarthroplasty (29%) closed reduction internal fixation and open reduction internal fixation (70%). We estimated the Student t test for independent samples with a significance level of < 0.05, calculating these at months one and six of follow-up to estimate differences between the groups and the EQ-5D.
The descriptive options identified were later analyzed by means of a multinomial logistic regression model with the following variables as predictors: age; sex; marital status; EQ-5D score in the first month; surgery type; comorbidities; hospital readmissions, follow-up type (prospective or retrospective). The statistical software program employed was STATA version 8 (StataCorp LP, College Station, TX, USA).
Written informed consent was obtained from each patient. The protocol was evaluated and approved by the research committee of each of the participating hospitals.
In total, 136 patients with hip fracture were included in this study and followed for a period of 6 months. The average age for the group was 77 ± 10 years, and 70% were women. Of all included patients, 41% were married; average number of years of formal education was 6 ± 5 years. In terms of the hospital breakdown, 59% were treated at the Victorio de la Fuente Hospital (IMSS), 28% at the National Institute of Rehabilitation (SS), and 13% at the two private hospitals. In total, 71% of patients underwent internal fixation surgery and 29% had a full-hip replacement. At least one comorbidity was observed in 63% of the patients, 9% were readmitted to the hospital. Six-percent of hospital readmissions were due to complications arising from the original hip fracture.
Demographic and clinical characteristics by age can be seen in Table I.
Regarding the EQ-5D questionnaire, the percentage of patients with any type of problem in each domain during any of the three evaluations is depicted in Figure 1. As can be observed, follow-up identified mobility is the most affected domain followed by usual activities and self-care in > 90% of cases in the first evaluation. It is noteworthy that the five dimensions were affected in nearly 60% of the patients
During the first month, all participants reported having issues with mobility; however the most affected group was that composed of patients > 85 years of age; 56% of this group was confined to bed; 56% cited deterioration in self-care; 59% had problems carrying out their regular activities; 29% had pain and discomfort, and 23.5% reported anxiety and depression.
The group aged between 80 and 84 years reported extreme problems regarding anxiety and depression (21%), and those aged between 50 and 74 years described having issues concerning pain and discomfort (27%) (See Table II).
Table II. Distribution of perceived problems by EQ-5D dimension 1 month after fracture (%).
At 6-month follow-up, there was a considerable increase in the number of patients reporting no problems in various areas of the HRQOL. Only those aged > 85 years of age showed worsening of their condition, a high proportion of these ranking at level 3 in mobility, self-care, and anxiety/depression, as illustrated in Table III.
Table III. Distribution of perceived problems by EQ-5D dimension 6 after months fracture (%).
Furthermore, we were able to observe significant differences between the age groups and anxiety and depression up to month 6 of follow-up (p = 0.021); between surgery type and mobility domains (p = 0.047) and daily activities (p = 0.034) at month 1 after surgery, and between public or private institution type in mobility (p = 0.002), self-care (p =0.004), and carrying out daily activities (p = 0.001) to months 1 and 6 and pain (p =0.017) and anxiety and depression (p = 0.05).
Table IV shows the differences in the first month of both types of survey: retrospective and prospective, in mobility (p= 0.002), personal care (p= 0.001), daily activities (p= 0.005), and pain (p= 0.000). In the sixth month follow-up, differences were found in personal care (p= 0.044)
On the other hand, when subjects were analyzed using visual observation to monitor trajectories in individual progress, we were able to identify five levels of improvement defined as follows:
These last two levels of progress (“same or no improvement” and “worse”) were represented by the group of patients aged 85 years and over). (Figure 2).
Figure 2. Levels of improvement identified during the monitoring period. Global EQ-5D score.
Predictors included in the multinomial logistic regression model comprised the following age; sex; marital status; surgery type; follow-up type (prospective or retrospective); comorbidities; hospital readmission, and EQ-5D score.
The most relevant predictors presented in Table V show that the youngest age group (50–74 years) showed “early and continuous improvement” in the first three months after surgery (47.8%) and “continued improvement” over the entire six-month follow-up period (31.7%). In the 75–79 years-of-age group, 33.8% of patients, and in the group aged 80–84 years, 43.6% of patients showed no change over the follow-up period, remaining static in their condition. The > 85 years-of-age group showed improvement from the start that was slow but constant (35.7%); however, this was also the group that contained the highest percentage of patients exhibiting worsening in their HRQOL (9.2%) (LR test, p = 0.06).
In terms of follow-up type, patients interviewed prospectively showed continued improvement over the whole follow-up period (49.2%) while the retrospective group demonstrated early and continuous improvement in the first three months (42.3%) that ceased over time (RL test, p = 0.17).
Surgery type was another predictor in the model, and patients who had arthroplasty surgery showed progressive and sustained improvement (32.7%) over the six-month follow-up period. Those who underwent hemiarthroplasty (35.4%) showed early and continuous improvement in the first three months after surgery with static progress thereafter until the end of the follow-up period. The same occurred with patients that had open reduction internal fixation (47.1%) and closed reduction internal fixation (45.4%). We are able to state that the patients reporting the worst HRQOL were the ones who had undergone arthroplasty (18%).
The present study describes the changes in HRQOL following a hip fracture in patients > 50 years of age over a 6-month follow-up period in four designated hospitals of the public and private health sectors of Mexico City.
Generally speaking, the HRQOL of patients with a hip fracture after a surgical procedure improves from months one through six in all five domains. Mobility is the most affected domain, changing from 98.5% to 74.3% in month 6 (the McNemar χ2 test = 95.16; p < 0.001). The same can be observed in self-care, from 95.6% to 56.6% (McNemar χ2 = 60.73; p < 0.001), in daily activities, from 95.6% to 61% (McNemar χ2 = 66.62; p < 0.001), in pain, from 89.7% to 52.9% (McNemar χ2 = 39.12; p < 0.001), and in anxiety and depression, from 58.1% to 40.4% (McNemar χ2 = 0.04; p < 0.001). That is, initially all domains that evaluate HRQOL are affected, but as time goes by, these lost functions are regained. However, age is a factor that must be considered.
The results show a reduction in the HRQOL of patients following a hip fracture. Many follow-up studies of this fracture type have shown deterioration in the domains related with HRQOL physical and social function. In our study, mobility was the most affected domain, which is similar to the findings by Randell et al. [24], who reported that at three-month follow-up after a hip fracture, there was a significant reduction in HRQOL in terms of physical and social function, social activity, and general health.
Patients with a hip fracture showed worse HRQOL with significant deterioration. Physical, emotional, and psychological instability of patients, as well as increased pain, are a consequence of a hip fracture due to osteoporosis, all of which can influence HRQOL. According to Adachi, during the follow-up of patients experiencing a hip fracture, nearly 33% of patients depend on others to perform their basic daily activities [25],[26]. In the current study, at the end of the follow-up period, 28.6% depended on others to carry out these activities.
Conversely, differing levels of deterioration in HRQOL were observed depending on the treatment type received (internal fixation), with patients receiving arthroplasty presenting progressive HRQOL improvement.
Tidermark [27] and Blomfeldt [28] mention that patients with total hip replacement report an improvement in their HRQOL four to twelve months after surgery; this, in comparison with those with internal fixation in the pain and ability-to-walk domains. Comparison in the remaining dimensions showed no statistical significance. Furthermore, they suggest that older patients with osteoporosis with a displaced fracture of the femoral neck cannot improve significantly with internal fixation techniques. In this study, the surgery type appears to be a prognosis factor. It can be observed that patients who underwent arthroplasty showed continuous improvement, as is the case with those with hemiarthroplasty and closed/open fixation during the first 3 months.
Also, it can be observed that in public institutions such as the Mexican Institute of Social Security (65.0%) and the SSA (74.4%), the closed reduction with internal fixation (CRIF) is the most commonly practiced surgery, while orthopedists in private hospitals frequently perform arthroplasty (52.9%) and hemiarthroplasty (47.1%).
Notwithstanding this, on conducting data stratification, we found differences between public and private institutions and HRQOL during month one post surgery in aspects such as mobility, self-care, and daily life activities, and the end of follow-up, only in daily activities and pain. Furthermore, we found that surgery type is significant at month one post surgery in mobility and daily activities; however, at month six, we did not observe significant differences in these.
Within our context, choice of surgery type in hip fractures will depend on fracture type [29], the patient’s age, and treatment and hospital stay costs(It has been reported [30] that costs are higher for arthroplasty than for internal fixation), and finally, the protocol type of each institution. In the Mexican Health Sector (to which IMSS and Ministry of Health hospitals belong), the use of clinical practice guidelines has been established [29], while in private hospitals, treatment is left to the criteria of the orthopedist in charge.
In addition, the current study shows that HRQOL differs depending on the study type, whether prospective or retrospective. Progress reports are different and could be due to patients’ selective memory or to sample size. Regarding follow-up, hospitals that are part of the Mexican Institute of Social Security (IMSS) and private hospitals have either retrospective (71.3%) or prospective (28.7%) (Ministry of Health, SSA) follow-ups.
In older adults involved in the study, deterioration in HRQOL was greatest, and although not statistically significant, it is a determining factor in HRQOL progress. Some previous studies [25] show that fractures in older people negatively impact HRQOL, and comorbidities should be regarded as clinically relevant. For patients studied retrospectively, certain diseases were identified, such as diabetes mellitus (22.7%), systemic blood pressure (35.1%), gastritis and heart failure (2.1%), and other type of illnesses (14.4%) while 23.7 did not report comorbidities. Patients followed up prospectively reported that 23.1% had diabetes, 30.8% high systemic blood pressure, 5.1% gastritis and heart failure, 2.6% other illnesses, and 33.3% did not report any maladies (χ2, 6.457; p = 0.264).
Age is a determining factor in HRQOL. The group of patients aged > 85 years reported extreme problems in mobility during the first postoperative month. Furthermore, these patients were the most affected in the daily life and self-care domains. Patients in this age group continued to report extreme issues in the previously mentioned domain (except for daily life activities, as their activities are limited) during the sixth postoperative month. In the visual trajectories, this same age group falls under “same or no improvement” and “worsening” conditions. Inversely, the group comprised of 50–59-year-olds is the least affected in mobility and daily life activities, but this group had the highest scores in anxiety/depression and pain. This can be best explained by the fact that at this age, the person is still part of the working force and is limited in returning to it, and this combines with anguish, anxiety, and fear of permanent disability.
The strength of this study was the ability to analyze the individual graphs of EQ-5D scores and, through the observational design the visual progress in each case, to enable various HRQOL behaviors to be identified during the follow-up period. In addition, using graphs allows ease in identifying each patient’s behavior during follow-ups. This permits decision-making regarding treatment and rehabilitation, as well as early detection of risks such as infections, etc. Another strength of the study is the use of methodological techniques for lost data (11% of patients were not localized), such as use of the imputed technique, which allows assigning values to lost data, thus utilizing and assigning data of the same population according to age and sex.
Study limitations were the following: short follow-up time (only six months), gathering of the retrospective data, the large percentage of retrospective cases, and the inability to refer to a baseline measurement taken prior to the fracture. Other limitation to the study is the use of the hot deck imputation technique: the imputed values can be good estimations but they are not real data and once the imputation is done, in the analysis one cannot differentiate between the characteristics of those who were surveyed and those who were not.
To our knowledge, this is the first HRQOL study in Mexican patients suffering from a hip fracture that identifies different levels of progress in HRQOL. Patients showed an improvement in HRQOL between months 1 and 6 following the fracture, with one of the most important predictors being age. Future studies are required in Mexican population with a longer follow-up period to compare deterioration in HRQOL after a hip fracture with that of other populations.
The authors thank the authorities of the National Institute of Rehabilitation, Hospital Victorio de la Fuente, the Mexican Institute of Social Security, MOCEL Angeles-Orthopedic Hospital and Trinity Hospital, for their important support to conduct this research.
Declaration of conflicts of interest
The authors have completed the ICMJE conflicts of interest form translated into Spanish by Medwave. PC reports having received funding for the study (see below). All authors declare no financial relationships with organizations in the past three years that might have an interest in the article, and no other relationships or activities that could influence the published article. Forms are available by contacting the corresponding author or the Journal.
Funding
PC reports having received funding from CONACYT (National Council of Science and Technology) for this study.
Ethical issues
The Commissions on Research Ethics and Biosafety of the Children's Hospital of Mexico "Federico Gomez", National Institute of Health, and the National Health Department, approved the study protocol registered as HIM/2009/046. The certificate may be obtained from the Journal, upon request.

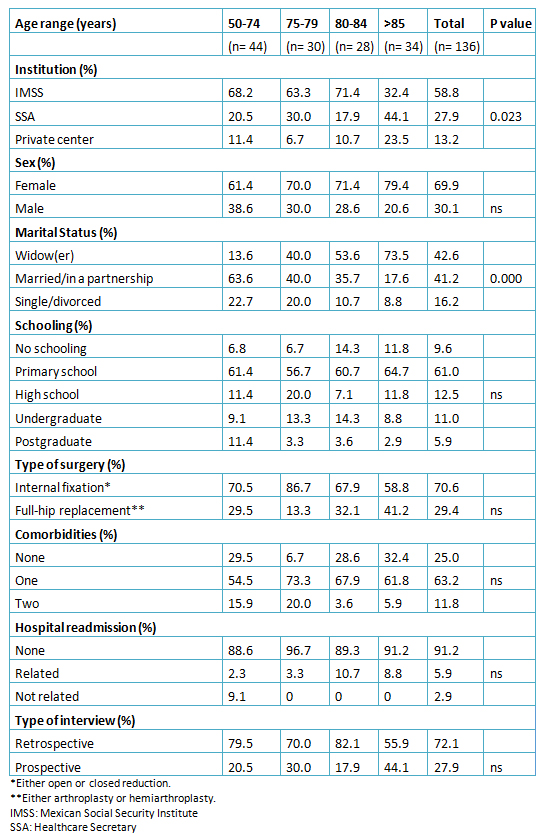 Table I. Baseline socio-demographic and clinical characteristics by age group at the time of hip fracture.
Table I. Baseline socio-demographic and clinical characteristics by age group at the time of hip fracture.

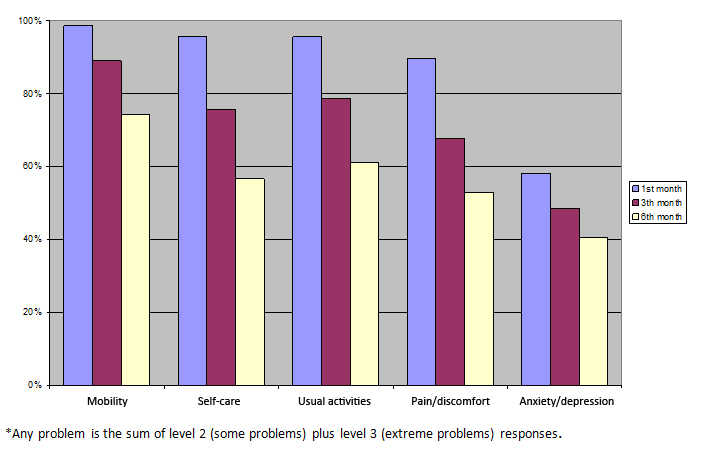 Figure 1. Percentage of patients reporting any problem* in each EQ-5D dimension over post-fracture time
Figure 1. Percentage of patients reporting any problem* in each EQ-5D dimension over post-fracture time

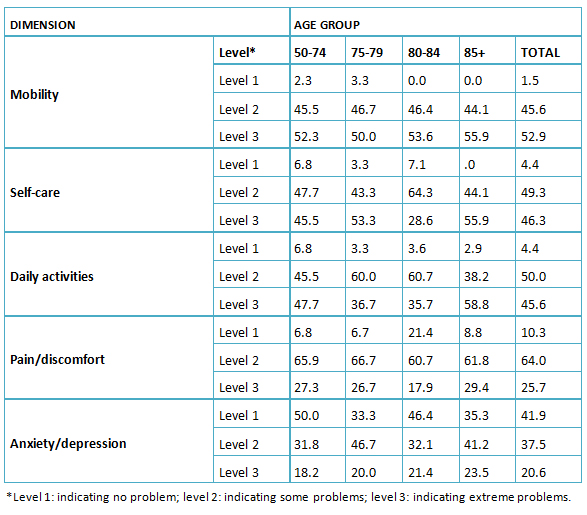 Table II. Distribution of perceived problems by EQ-5D dimension 1 month after fracture (%).
Table II. Distribution of perceived problems by EQ-5D dimension 1 month after fracture (%).

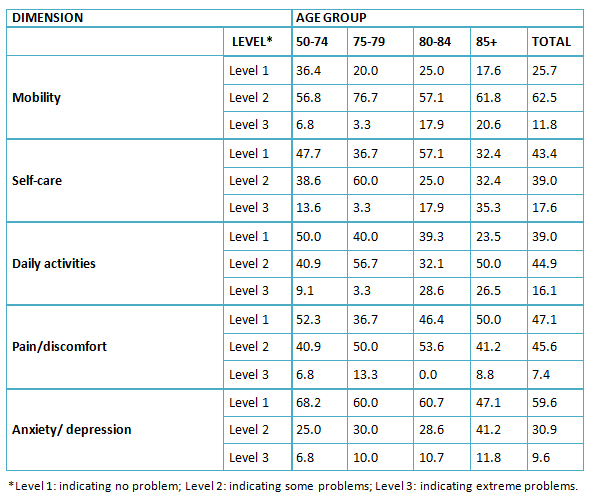 Table III. Distribution of perceived problems by EQ-5D dimension 6 after months fracture (%).
Table III. Distribution of perceived problems by EQ-5D dimension 6 after months fracture (%).

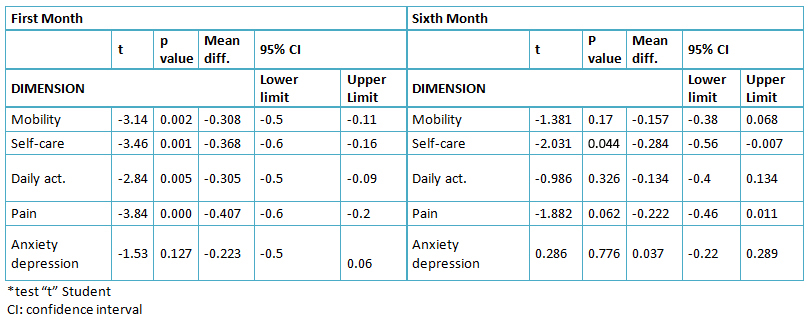 Table IV Differences in quality of life related to health by application type (prospective versus retrospective) at 1 and 6 months*.
Table IV Differences in quality of life related to health by application type (prospective versus retrospective) at 1 and 6 months*.

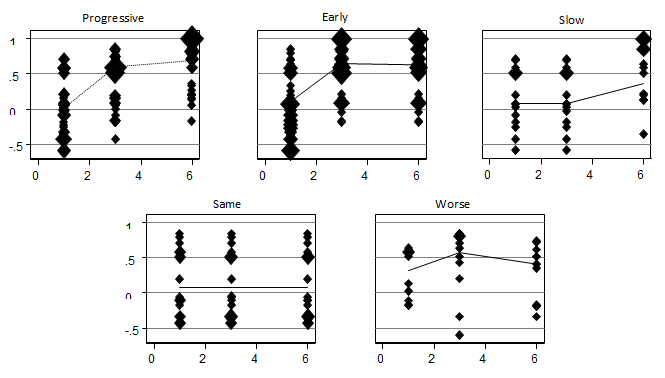 Figure 2. Levels of improvement identified during the monitoring period. Global EQ-5D score.
Figure 2. Levels of improvement identified during the monitoring period. Global EQ-5D score.

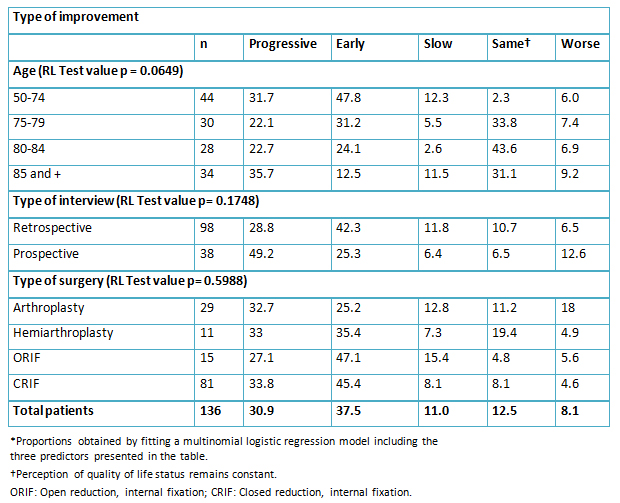 Table V. Adjusted proportions* of patients following specific 6 month quality of life trajectories as measured by EQ5-D score.
Table V. Adjusted proportions* of patients following specific 6 month quality of life trajectories as measured by EQ5-D score.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
Hip fractures are an important cause of morbidity and mortality and one of the main causes of disability in the older population. The lifetime risk for any type of osteoporotic fracture is very high and falls within the range of 40 - 50% in women and 13 - 22% for men. In Mexico, the lifetime likelihood of having a hip fracture at 50 years of age is 8.5% in Mexican women and 3.8% in Mexican men, but this is expected to rise in upcoming years.
AIM
This study aims to report the Health-Related Quality of Life over the first six months after a hip fracture in two public and two private tertiary care hospitals in Mexico City.
METHOD
Changes over time were evaluated through visual observation of each patient's development trajectory using the graphic representation of the EQ-5D global score. The trajectories were grouped by affinity into five levels of progress according to clinical course. The identified descriptive options were analyzed using the multinomial logistic regression model (LR).
RESULTS
One-hundred-and-thirty-six (136) patients with a hip fracture were followed after surgery. Their mean age was 77 ± 10 years. During the first month, mobility, daily activities, and self-care were the most affected. The group aged between 80 and 84 years reported extreme problems regarding anxiety and depression (21%), and those aged between 50 and 74 years described having issues concerning pain and discomfort (27%). At the 6-month follow-up, only those aged > 85 years of age showed worsening of their condition, a high proportion of these ranking at level 3 in mobility, self-care, and anxiety/depression. Toward the end of the follow-up period, this last group reported having extreme problems (being unable to carry out everyday activities) and worsening of their mobility (9.2%) (inability to walk about) (LR test, p = 0.06).
DISCUSSION
Patients with hip fracture showed difficulties in different areas during the first month after surgery, with steady recuperation up to month six. Age was an important factor in the recovery of all evaluated domains. This graphical tool facilitates classification, identification, and monitoring Health-Related Quality of Life in patients with hip fractures.
 Autores:
Esperanza Ramírez-Pérez[1], Patricia Clark[2], Fernando Carlos[2], Araceli Camacho[2], Francisco Franco-Marina[3]
Autores:
Esperanza Ramírez-Pérez[1], Patricia Clark[2], Fernando Carlos[2], Araceli Camacho[2], Francisco Franco-Marina[3]

Citación: Ramírez-Pérez E, Clark P, Carlos F, Camacho A, Franco-Marina F. Health-related quality of life after surgery for hip fracture: a multicentric study in Mexican population. Medwave 2014;14(5)5972 doi: 10.5867/medwave.2014.05.5972
Fecha de envío: 24/4/2014
Fecha de aceptación: 9/6/2014
Fecha de publicación: 18/6/2014
Origen: no solicitado
Tipo de revisión: con revisión por cuatro pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Nombre/name: Sandra Don oso
Fecha/date: 2014-10-09 15:56:50
Comentario/comment:
xcxcxzc
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15(11):897-902. | CrossRef | PubMed |
Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15(11):897-902. | CrossRef | PubMed | J Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl 2):S3-7. | CrossRef | PubMed |
J Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl 2):S3-7. | CrossRef | PubMed | Clark P, Carlos F, Vázquez JL. Epidemiology, costs and burden of osteoporosis in Mexico. Arch Osteoporos. 2010;5:9-17. | CrossRef |
Clark P, Carlos F, Vázquez JL. Epidemiology, costs and burden of osteoporosis in Mexico. Arch Osteoporos. 2010;5:9-17. | CrossRef | Johansson H, Clark P, Carlos F, Oden A, McCloskey EV, Kanis JA. Increasing age-and sex-specific rates of hip fracture in Mexico: a survey of the Mexican Institute of Social Security. Osteoporos Int. 2011;22:2359-2364. | CrossRef |
Johansson H, Clark P, Carlos F, Oden A, McCloskey EV, Kanis JA. Increasing age-and sex-specific rates of hip fracture in Mexico: a survey of the Mexican Institute of Social Security. Osteoporos Int. 2011;22:2359-2364. | CrossRef | Lips P, van Schoor NM. Quality of life in patients with osteoporosis. Osteoporos Int. 2005;16:447-455. | CrossRef |
Lips P, van Schoor NM. Quality of life in patients with osteoporosis. Osteoporos Int. 2005;16:447-455. | CrossRef | Rabenda V, Manette C, Lemmens R, Mariani AM, Struvay N, Reginster JY. Prevalence and impact of osteoarthritis and osteoporosis on health-related quality of life among active subjects. Aging Clin Exp Res. 2007;19(1):55-60. | PubMed |
Rabenda V, Manette C, Lemmens R, Mariani AM, Struvay N, Reginster JY. Prevalence and impact of osteoarthritis and osteoporosis on health-related quality of life among active subjects. Aging Clin Exp Res. 2007;19(1):55-60. | PubMed | Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ 3rd. Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int. 2001;12(12):1042-9. | CrossRef | PubMed |
Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ 3rd. Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int. 2001;12(12):1042-9. | CrossRef | PubMed | Taylor BC, Schreiner PJ, Stone KL, Fink HA, Cummings SR, Nevitt MC, et al. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatrics Soc. 2004;52(9):1479-1486. | CrossRef | PubMed |
Taylor BC, Schreiner PJ, Stone KL, Fink HA, Cummings SR, Nevitt MC, et al. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatrics Soc. 2004;52(9):1479-1486. | CrossRef | PubMed | Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA. The human cost of fracture. Osteoporos Int 2005;16(12):2046-2052. | CrossRef | PubMed |
Pasco JA, Sanders KM, Hoekstra FM, Henry MJ, Nicholson GC, Kotowicz MA. The human cost of fracture. Osteoporos Int 2005;16(12):2046-2052. | CrossRef | PubMed | Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103(2A):S12-S17; discussion S17-S19. | CrossRef | PubMed |
Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997;103(2A):S12-S17; discussion S17-S19. | CrossRef | PubMed | Madhok R, Melton III LJ, Atkinson EJ, O'Fallon WM, Lewallen DG. Urban vs rural increase in hip fracture incidence. Age and sex of 901 cases 1980-89 in Olmsted County, U.S.A. Acta Orthop Scand. 1993;64(5):543-548. | CrossRef | PubMed |
Madhok R, Melton III LJ, Atkinson EJ, O'Fallon WM, Lewallen DG. Urban vs rural increase in hip fracture incidence. Age and sex of 901 cases 1980-89 in Olmsted County, U.S.A. Acta Orthop Scand. 1993;64(5):543-548. | CrossRef | PubMed | Schroder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the second hip fracture. Clin Orthop Relat Res. 1993;(289):166-169. | PubMed |
Schroder HM, Petersen KK, Erlandsen M. Occurrence and incidence of the second hip fracture. Clin Orthop Relat Res. 1993;(289):166-169. | PubMed | Lawrence TM, Wenn R, Boulton CT, Moran CG. Age-specific incidence of first and second fractures of the hip. J Bone Joint Surg. 2010;92(2):258-261. | CrossRef | PubMed |
Lawrence TM, Wenn R, Boulton CT, Moran CG. Age-specific incidence of first and second fractures of the hip. J Bone Joint Surg. 2010;92(2):258-261. | CrossRef | PubMed | Mezuk B, Eaton WW, Golden SH. Depression and osteoporosis: epidemiology and potential mediating pathways. Osteoporos Int. 2008;19(1):1-12. | CrossRef | PubMed |
Mezuk B, Eaton WW, Golden SH. Depression and osteoporosis: epidemiology and potential mediating pathways. Osteoporos Int. 2008;19(1):1-12. | CrossRef | PubMed | Gold DT, Solimeo S. Osteoporosis and depression: a historical perspective. Curr Osteoporos Rep. 2006;4(4):134-139. | CrossRef | PubMed |
Gold DT, Solimeo S. Osteoporosis and depression: a historical perspective. Curr Osteoporos Rep. 2006;4(4):134-139. | CrossRef | PubMed | Johnell O. The socioeconomic burden of fractures: today and in the 21st century. Am J Med. 1997;103(2A):20S-25S;discussion 25S-26S. | PubMed |
Johnell O. The socioeconomic burden of fractures: today and in the 21st century. Am J Med. 1997;103(2A):20S-25S;discussion 25S-26S. | PubMed | Becker DJ, Kilgore ML, Morrisey MA. The societal burden of osteoporosis. Curr Rheumatol Rep. 2010;12(3):186-191. | CrossRef | PubMed |
Becker DJ, Kilgore ML, Morrisey MA. The societal burden of osteoporosis. Curr Rheumatol Rep. 2010;12(3):186-191. | CrossRef | PubMed | Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364-370. | CrossRef | PubMed |
Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc. 2003;51(3):364-370. | CrossRef | PubMed | Clark P, Carlos F, Barrera C, Guzman J, Maetzel A, Lavielle P, et al. Direct costs of osteoporosis and hip fracture: an analysis for the Mexican healthcare system. Osteoporos Int. 2008;19(3):269-276.
| CrossRef | PubMed |
Clark P, Carlos F, Barrera C, Guzman J, Maetzel A, Lavielle P, et al. Direct costs of osteoporosis and hip fracture: an analysis for the Mexican healthcare system. Osteoporos Int. 2008;19(3):269-276.
| CrossRef | PubMed | Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337-343. | CrossRef | PubMed |
Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337-343. | CrossRef | PubMed | Butcher JN, Kyonghee H. Chapter 3. Methods of establishing cross-cultural equivalence. En: International adaptations of the MMPI-2: research and clinical applications, Minneapolis, USA: University of Minnesota Press, 1996.
Butcher JN, Kyonghee H. Chapter 3. Methods of establishing cross-cultural equivalence. En: International adaptations of the MMPI-2: research and clinical applications, Minneapolis, USA: University of Minnesota Press, 1996.  Andridge RR, Little RJ. A review of hot deck imputation for survey non-response. Int Stat Rev. 2010;78(1):40-64. | CrossRef | PubMed |
Andridge RR, Little RJ. A review of hot deck imputation for survey non-response. Int Stat Rev. 2010;78(1):40-64. | CrossRef | PubMed | Randell AG, Nguyen TV, Bhalerao N, Silverman SL, Sambrook PN, Eisman JA. Deterioration in quality of life following hip fracture: a prospective study. Osteoporos Int. 2000;11(5):460-466. | CrossRef | PubMed |
Randell AG, Nguyen TV, Bhalerao N, Silverman SL, Sambrook PN, Eisman JA. Deterioration in quality of life following hip fracture: a prospective study. Osteoporos Int. 2000;11(5):460-466. | CrossRef | PubMed | Adachi JD, Loannidis G, Berger C, Joseph L, Papaioannou A, Pickard L, et al. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int. 2001;12(11):903-908. | CrossRef | PubMed |
Adachi JD, Loannidis G, Berger C, Joseph L, Papaioannou A, Pickard L, et al. The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int. 2001;12(11):903-908. | CrossRef | PubMed | Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, et al. Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis. Osteoporos Int. 1997;7(1):36-38.
| CrossRef | PubMed |
Lips P, Cooper C, Agnusdei D, Caulin F, Egger P, Johnell O, et al. Quality of life as outcome in the treatment of osteoporosis: the development of a questionnaire for quality of life by the European Foundation for Osteoporosis. Osteoporos Int. 1997;7(1):36-38.
| CrossRef | PubMed | Tidermark J, Ponzer S, Svensson O, Soderqvist A, Tornkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br. 2003;85(3):380-388. | CrossRef | PubMed |
Tidermark J, Ponzer S, Svensson O, Soderqvist A, Tornkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br. 2003;85(3):380-388. | CrossRef | PubMed | Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87(4):523-529. | CrossRef | PubMed |
Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87(4):523-529. | CrossRef | PubMed | Prevención y diagnóstico de fractura de cadera en el adulto en el primer nivel de atención. Guía de referencia rápida. Catálogo Maestro de Guías de práctica clínica SSA-017-08. México, 2012. | Link |
Prevención y diagnóstico de fractura de cadera en el adulto en el primer nivel de atención. Guía de referencia rápida. Catálogo Maestro de Guías de práctica clínica SSA-017-08. México, 2012. | Link | Parker MJ, Handoll HHG. Artroplastia de reemplazo versus fijación interna para la fractura extracapsular de cadera en adultos (Revisión Cochrane traducida). La Biblioteca Cochrane Plus, 2008 Número 4. update-software.com [on line] | Link |
Parker MJ, Handoll HHG. Artroplastia de reemplazo versus fijación interna para la fractura extracapsular de cadera en adultos (Revisión Cochrane traducida). La Biblioteca Cochrane Plus, 2008 Número 4. update-software.com [on line] | Link | Osteoporosis en América Latina: revisión de panel de expertos
Osteoporosis en América Latina: revisión de panel de expertos