 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: universal newborn hearing screening program, parental knowledge, qualitative research
INTRODUCTION
The Universal Newborn Hearing Screening Program in Mexico began in 2010. Its results, published in 2013 by the National Council for the Development and Inclusion of Persons with Disabilities (CONADIS), report low coverage and, currently, there is a dearth of information about its activities. This study describes the process of the program from the epistemological perspective of women whose children participated in the program, evaluating it under the sustenance of the constructivist-respondent model in search of aspects that could help explain its results.
METHODS
Descriptive study with a qualitative approach based on the constructivist–respondent paradigm. We elected the 14 women who participated in the study through trial and number until theoretical saturation. After signing an informed consent form and respecting the confidentiality and anonymity, these women underwent semi-structured interviews that were audio-recorded and transcribed as were conducted. The researchers separately analyzed and coded categories and conjointly summarized categories and subcategories. Validity and reliability were obtained through the credibility, transferability and triangulation.
RESULTS
From the speeches, we obtained the general profile of the interviewed, evolution of their children in the program process and four categories with 15 subcategories related to the reconstruction of the process: knowledge, needs, feelings and attitudes. One was evaluated as favorable, six without agreement and eight as unfavorable. The latter refer to our own context.
CONCLUSIONS
The epistemological perspective of the interviewed women showed aspects that could help explain the low coverage of the program. Attention from public policies could improve this feature. With the establishment of the program, children with deafness are diagnosed and treated at a lower age than before the program.
The creation of universal neonatal hearing screening programs started in developed countries between 1964 and 1996. In Latin-America, this happened in 1993 [1], and in Mexico, specifically, in 2010 as a political action within its 2007-2012 Development Plan and the “Insurance for a new generation” initiative, as an economic support for children born after 2006 [2].
At the moment, there are 18 hospital of the City of Mexico Government which are applying the Neonatal Hearing Screening (NHS)–7 general hospitals: La Villa, Iztapalapa, Ticomán, “Enrique Cabrera”, Milpa Alta, “Gregorio Salas” and Xoco; 7 maternal-infantile hospitals: Inguarán, Tláhuac, Magdalena Contreras, Topilejo, Cuajimalpa, “Nicolás M. Cedillo” y Cuautepec; the specialties hospital “Belisario Domínguez”; the maternal-pediatric hospital Xochimilco; and the pediatric hospitals Peralvillo and Coyoacan. Also, there are five diagnostic confirming units, and eight surgical treatment units.
In the states of the Mexican Republic, almost 500 maternal-infantile hospitals from the Health Secretariat, and 49 diagnostic medical units were considered for the inform. The activities of these sites were reported in the Consejo Nacional de Discapacidad (CONADIS) (National Council on Incapacities) bulletin, and the assessment of the program was carried out in 2013. The published results, contrasting the objectives and the indicators (percentage of infants screened, diagnosed, and treated) showed a low coverage as well as inconsistencies in the information [3],[4]; and at the moment, the reports on those activities are only available through journalist notes and a few published articles [5],[6],[7].
The activity of evaluating programs and systems started in the United States 50 years ago in the areas of work training and education, and later in some health programs (addictions, family planning, reproductive health, and recently, public health) [8]. In Latin-America, the incorporation of these assessment activities has been rather slow, and in Mexico, it became apparent in the 60’s, and finally systematized in 1997 in the areas of education, health, and alimentation [9].
In general, the evaluation consists in making judgments about the object, situation or process but these should be systematic and should use procedures which can guarantee the validity and reliability with methods used for social research [10]. The process of evaluating has been supported by diverse studies which, during the years 60’s fostered different initiatives to re-conceptualize the term; proposing new evaluation models, a situation which resulted in five generations of different models which have been changing their assessing methodologies, and which have triggered a consequent war of paradigms [11] - understanding the term paradigm as a basic system of beliefs based on ontological, epistemological, and methodological suppositions which represent the vision of the world or its parts, and which inform the researchers for what they are doing and what is in and out of the limits of a legitimate research [12].
The constructivist-respondent assessment model proposed by E. Guba and I. Lincoln in 1984 belongs to the 4th generation of evaluative models. It has a qualitative approach and follows a paradigm with an ontology that presents the reality by means of multiple mental constructions based on the social experience and local nature which can be shared by different individuals and cultures. It has a transactional and subjectivist epistemology (links the researchers with the objects of study). The findings are built as a result of the research advancing; and its methodology is characterized by being: holistic – the study of the reality from a global perspective; inductive – the categories, patterns, and interpretations are based on the data obtained from the participants, and not from previous theories or hypotheses; and ideographic – the interpretation of social phenomena is based on hermeneutical and dialectical tools. Its social and individual constructions are variables produced and refined through the interaction among the researchers and the objects of study. All these characteristics allow the interpretation, comparison, and dialectic interchange to constitute the ETIC from the EMIC of participants [13].
Young, A. & Tattersall, H.,(2005) considered that the prenatal perspective has an special epistemological value, and further commented on the few studies related to assessing research on neonatal hearing screening programs [14], suggesting that the majority of the publications have been based on a quantitative focus, using questionnaires, telephonic surveys, and interviews [15],[16],[17],[18], and that the few studies based on a qualitative focus [19],[20],[21],[22] have not been about the global process of neonatal hearing screening, in other words, its screening, diagnostic, intervention, cochlear implants, etcetera. This study was carried out with the objective of qualitatively assessing this global process from the parental perspective, looking for aspects which could help explain its results. The model used was the constructivist-respondent. Also, a quantitative analysis of the characteristics of the participants, and the evolution of their infants in any or all four program stages was carried out.
Design
This is a mixed study in which the qualitative focus is based on the constructivist-respondent evaluative model of Guba and Lincoln, and the quantitative aspect is based on the description of demographic characteristics of the participants and the evolution of their infants during the program. The participants were selected by convenience [23] with an informant profile based on the following criteria: women whose children were born in 2010 or later in any of the child and maternal hospitals included in the Neonatal Hearing Screening Program, or who were included in any of the stages of this program. The number of interviewed was determined according to the theoretical saturation criteria [24]. The main researcher has a 12-year experience on the topic which includes theoretical and practical knowledge related to the programs of hearing screening. The relation with the participants was respectful allowing freedom to express any emotions.
Considering that the process of the program is carried out in different medical units, it was necessary to visit several of them in the City of Mexico upon authorization of the corresponding personnel responsible of the audiology areas and screening procedures of two maternal-child hospitals, one general hospital, and an institute of third level of attention belonging to the Health Secretariat. With the informed-consents, we visited the waiting wards, the screening rooms, and the language therapy rooms. Fourteen women were semi-structurally interviewed through a guide without a specific order. Each interview lasted approximately 40-50 minutes. The interviews were performed between August 2014 and March 2015. All interviews were recorded and transcribed as expressed (EMIC). The participants who were taking their infants to language therapy had the opportunity to confirm or rejected their statements (ETIC). Separately, each researcher carried out a latent content analysis in order to identify, code, and categorize primary patterns related to process of the program. Alphabet letters were used to ensure the participants anonymity, confidentiality, and privacy. Categories and sub-categories were tagged according to respondent model in: problems – when there was not an agreement among the interviewed in relation to some aspects of the process; worries – when the aspects were assessed as not favorable; and agreements when the aspects were considered favorable. Scientific rigor was obtained through the criteria of credibility - construction of the participants and re-construction of the main researcher in relation to what they think and feel; transferability – analyzing the adjustments of the results within other contexts; and triangulation – contrasting the differences in agreements and disagreements among discourses, and verifying the infant’s data on their screening daily results.
Descriptive statistics were used to analyze and present the demographic profile of the 14 women interviewed. Data showed the women had ages between 19 and 38 years old with an average of 26; 10 of them (72%) were married; 13 of them were housewives (93%); 6 (42%) had a high school level; 6 (42%) stated having had problems during pregnancy, and 12 delivered by caesarean section, nine of these were not programmed. The hospitals were they were attended are located in the state of Mexico (6), other states (4), and the City of Mexico (4).
The data related to the infants were: age at the moment of this study: between one month and four years, average 1.8 years old; eight (57%) male and six (43%) female; two (14%) had a family history of deafness, age at the moment of the screening: between four and 180 days after being born, average 43 days; seven of them (50%) were screened two or three times; average age of the diagnosis: 7.57 months; five of them (36%) showed deep bilateral diminished hearing; two of them (14%) showed deep unilateral diminished hearing; four of them (28%) were diagnosed with probable diminished hearing (remain under study), and three of them showed normal bilateral audition; the average age of the implementation of audition auxiliary aids was 18 months; the average age of language therapy initiation was 13.4 months; two infants received cochlear implants at two years and six months respectively. See Table 2.
The qualitative analysis of the constructions made from the parental perspective about the process of the program of hearing screening, under the assessment criteria of the constructivist model, showed the emergence of four categories: knowledge, necessities, feelings, and attitudes, with three, seven, three, and two sub-categories respectively, seven corresponding to hearing screening stage, one to the diagnosis, four to the treatment, and three to the general program. From the total, eight were organized as unfavorable (worries) where five correspond to the screening stage, and two to the treatment stage, these last related to our context in Mexico. All this is shown in Table 3.
The category Knowledge included 3 sub-categories, the first linked to knowledge obtained from the information given to the interviewed about what is the neonatal hearing screening and its sequence. The results showed lack of agreement because some said having received complete information with brochures and chats in some hospitals of the City of Mexico and the state of Mexico, but others were not informed, a situation which even resulted in their infants not being screened:
[…] “in the hospital where my child was born, they did the hearing screening; there offer brochures with information”, and they receive children from other hospitals” […] D
[…] “I became aware thanks to my brother because his son and my son were born in the same hospital, but his son was hearing-screened and my son was not” […] A
The second sub-category did not have agreement either. It was related to the knowledge of what is the hearing screening. The information was given in special rooms, but only to some of them, the others just received instructions that the screening was to be performed.
[…] “while I was in recovery, they told me that they had to perform the metabolic and the hearing screening on my baby, but they did not explain me what were those procedures about” […] M
[…] “When I asked what was that screening for, the nurse said that it was to verify if the baby could hear correctly, and that the procedure was not dangerous” […] G
The third was related to the lack of knowledge on the conditions in which the infant should come to the hearing screening. This was considered unfavorable because none of the informants were given information on the issue.
[…] “the diagnosis room is very small, the noise was normal, there were 3 or 4 nurses talking while doing the screenings. During the procedure, the babies become nervous because their ears are covered. The procedure lasts about 10 to 15 minutes if they are docile. They explain you how to manage the baby. If the baby becomes irritable, they let you relax, and then they call you back” […] E
The second category was Necessities. Seven sub-categories were identified; six were linked, one to the program, three with the screening procedure, and three with the treatment.
The first is concerned to the need of the hearing screening program in other hospitals and locations.
[…] “in the hospital where my child was born, they do not do the hearing screening. They told me to look for a place to have it because it was important for my baby” […] F
[…] “in Puebla, the private clinics do not perform the hearing screening. You have to go to the general hospital” […] C
[…] “in the hospital where my child was born, they do not offer the hearing screening; and this should be in all hospitals to prevent hearing problems in the infants” […] G
The related issues to hearing screening practice were: the necessity to widen the age of screening because of the indication which some received that the procedure should be performed in the 4th or 5th day after being born. Some interviewed commented that they were hospitalized for diverse causes, but that they did not receive the screening.
[…] “they did her the screening 5 days after she was born, not before leaving the hospital because they explained us it had to be that way” […] N
[…] “my son was in a contiguous room so they said they would come up and screen him, but nothing happened: he was 15 days but they did not perform him the screening” […] K
Another need was to have a better handling of the equipment while doing the screening.
[…] “they could not do her the screening in three occasions, the doctor said she moved a lot and was afraid to hurt her” […] C
[…] “they tried several times with different ear plugs but the baby did not respond; they said the ear was probably dirty or something and that we should return another day” […] J
The third is about the need of receiving a clear explanation about the results of the screening when this “fails.” In some mothers, this created some confusion and mistrust, abandoning the sequence of the program looking for someone who could give them a trustworthy explanation.
[…] “the screening is noisy, they said it up to three times, but never an explanation of why it was noisy” […] H
[…] “they could not do the screening in three occasions, so we left and saw a specialist who could check with detail the baby’s ears” […] C
The sub-categories related to the treatment were: the need to widen the language therapy service, and also increase it in frequency and duration.
[…] “in order to enter to therapy, they put my baby in a waiting list, they said because there are many children there, so we waited… the language therapy is necessary so it should be given with more frequency and duration… we spend more time going there than the therapy time itself” […] C
- The need of support for the development of language in the baby-kinders and pre-school centers was also expressed.
[…] “at school, they did not support her and let communication being with signals. The objective is that she speaks. Before we used to have some words but now only signals again” […] H
The prosthetic treatment was also regarded. They mentioned that there is a need to have economical support for all children to obtain their audition devices and cochlear implants, and that some are simply more fortunate than others.
[…] “they did not charge me for the cochlear implant, the Popular Insurance is covering all” […] A
[…] “they prescribed an audition device but I have not been able to buy it, and in the donation program, we were unlucky” […] D
The third category was Feelings, and it included three sub-categories involved with feelings towards the results of the screenings and diagnoses. The first was linked to the explanation of the screening results. It generated feelings of anguish, anxiety and desperation.
[…] “I felt very anguished for considering my daughter could be deaf. These persons suffer and can not speak and they cannot have a normal life” […] B
The second was linked to positive feelings in some interviewed when they were told about the advantages of the screening (confidence and security), but then negative feelings due to the explanation of the results.
[…] “I felt confidence, this screening really relieves you, it does not hurt, it is fast, and the results are almost immediate” […] J
[…] “They said that the device we have is probably malfunctioning. This little devices are not that reliable a nurse told me” […] E
The third sub-category is about the impact of a definitive diagnosis result, and it reflected negative feelings such as blame, pain, and lack of hope.
[…] “When they confirmed that my daughter did not hear, I felt vary bad, and I thought I was to have the blame” […] H
[…] “In that moment, the whole world collapsed on us because we had the hope that the problem could only be in only one side” […] C
The fourth category was Attitudes and it included two sub-categories, the first one reflecting the program in general (without agreement) and some interviewed considered it as good, but others considered that the medical personnel is insensible while giving the results.
[…] “the screening is good because it helps us know if our children are fine, you know, physically they look ok, but sometimes the ear comes with malformations, and you can not notice this. These programs are necessary” […] N
[…] “it is necessary that the personnel of the hearing screening program be more attentive and sensible while giving the results, because they should understand the difficult moments of the parents. Some mothers even go alone and need care and support from who we trust” […] H
The second sub-category reflects the results of the treatments in the final stage of the process. It was assessed as favorable in front of the results of the language development and the behavior changes in the children.
[…] “from the moment in which they put her the hearing device, she began to try to speak, before she only screamed, but now the devices help her a lot” […] C
[…] “with the use of the hearing devices, at first we did not notice changes; we saw him the same, but gradually, we started to notice the advances. We thought he was going to be as our aunts (deaf and mute)” […] A
Few studies have included the experience of the parents (indirect beneficiaries of programs like this) in an evaluation, which critically describe the programs and the practice of the hearing screening [25]. Fortunately, the vision of the parents has been considered as an epistemological contribution. It is also recognized that few are the assessing studies based on a qualitative-focused model [14]. Taking in consideration the obtained results in the present research, which was developed within the ontological, epistemological, and methodological criteria of the constructivist-respondent assessing model, we obtained a global view of the process of the program of neonatal hearing screening and early intervention, which corresponds to its holistic character. Methodologically, the categories, patterns, and interpretations were built upon the discourses of the interviews, which in turn were derived and refined hermeneutically and dialectically between the responsible researcher and the participants. The findings were credited as the result of the interaction between the evaluator and the evaluated object.
From the results of this program in 2012, it is known that the coverage was only 65% and the objective was 80% [4]; now, from the parental perspective, seven categories were identified which are related to the stage of hearing screening, and two of these are related with the partial knowledge mothers have about the screening, wrongly considering it a diagnostic study, and not knowing the conditions the infants should have. Three sub-categories of this stage were assessed as necessities, the limited age of the baby for the screening (only in the first week) and the problems related to the handling of the equipment, and the unclear explanations of the results. These situations provoked contrasted feelings because, while some participants had good results, others became confused and even abandoned the sequence of the program, delaying the diagnosis and treatments. These categories have been identified as findings in other studies on the results of hearing screening, like knowledge [26],[27], conditions of the infants to be prone for screening [17], and handling of the equipment for the screening and lack of clear explanations of the results [16]. In the diagnosis stage, only negative feelings that always accompany these cases were identified, reflects a need of more support from the health personnel [28]. The treatment stage is related with the necessities to acquire de hearing devices, and the low coverage of language therapy services in our country. The general opinion of the program was contradictory and depended on the obtained results [29].
The unfavorable results in the sub-categories of the screening stage can be influencing the low coverage of the program, the lack of knowledge, the failures in the practice, the confusion, and also the limited time to carry out the screenings, all these delay the process towards an early diagnosis and treatment, which was found to be unequal in terms of support opportunities; and considering also the difficulties to have an adequate language therapy service, all these provoke that children lose opportunities to receive proper treatments including cochlear implants just for being too old. The profiles of the interviewed told us about the territorial diversity in the practice of the hearing screening, while the chronological analysis of the children indicated that the age for diagnosis and treatment initiation has somewhat improved, but not enough to achieve the international standards in the universal neonatal hearing screening [30]. In fact, before these programs, children were first assessed at 3 or 4 years old [31],[32].
In the City of Mexico, in 2006, the detection of auditory incapacity, in relatively marginalized populations was at 2.8 years old in average, and the diagnosis was at 6.6 years old in average, but in highly marginalized populations this was at 5.4 and 10.4 years old respectively, reflecting the poor access to specialized services [33],[34]. So, addressing these situation is a proposal from public policies which will allow improvements to the Neonatal Hearing Screening Program; including in the areas of: diffusion, information for pregnant women, information for health personnel and general public, continuous training, support to the parents throughout all the screening stages, cases monitoring, continuous informing on the activities, financing alternatives for the diverse treatments, etcetera.
The qualitative evaluation of the parental perspective through the lens of the constructivist-respondent model showed a greater incidence of unfavorable categories in the screening and treatment stages - issues which can be addressed through public policies in order to benefit the neonates with audition problems and their families.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical considerations
Nevertheless this study was carried out using interviews which are considered as riskless according to the Health General Law regarding health research in Mexico - chapter I, article 17, informed consents were obtained from all participants, as well as approval from the screening and treatment personnel in agreement with the Ethics Commission – article 23. Also, and considering the articles 13 and 16, pseudonyms in terms of alphabet letters were used to guarantee the confidentiality of the participants.
Conflicts of interest
The authors completed the ICMJE conflict of interest declaration form, translated to Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Financing
This research was self-financed by the main researcher.

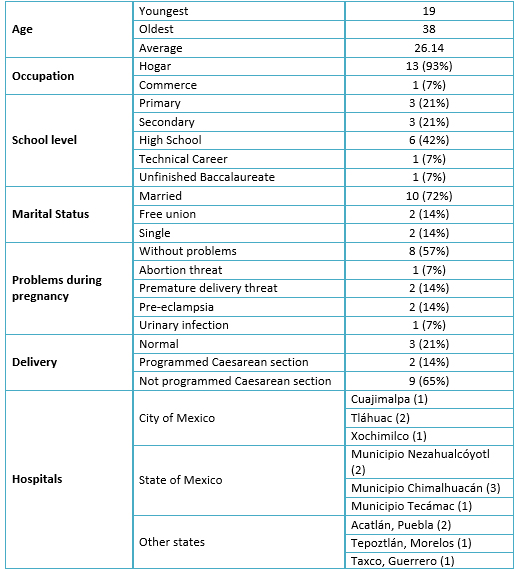 Table 1. General profile of the fourteen participants of the qualitative assessment related to the evaluating research on the process of the Program of Neonatal Hearing Screening.
Table 1. General profile of the fourteen participants of the qualitative assessment related to the evaluating research on the process of the Program of Neonatal Hearing Screening.

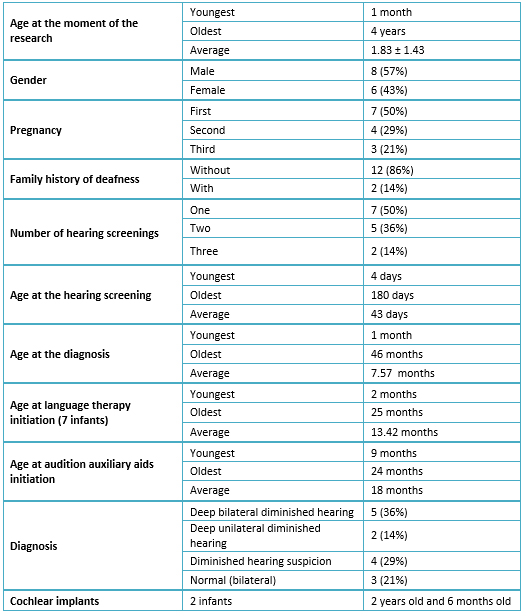 Table 2. General profile of the evolution if the infants participating in the process of the Program of Neonatal Hearing Screening.
Table 2. General profile of the evolution if the infants participating in the process of the Program of Neonatal Hearing Screening.

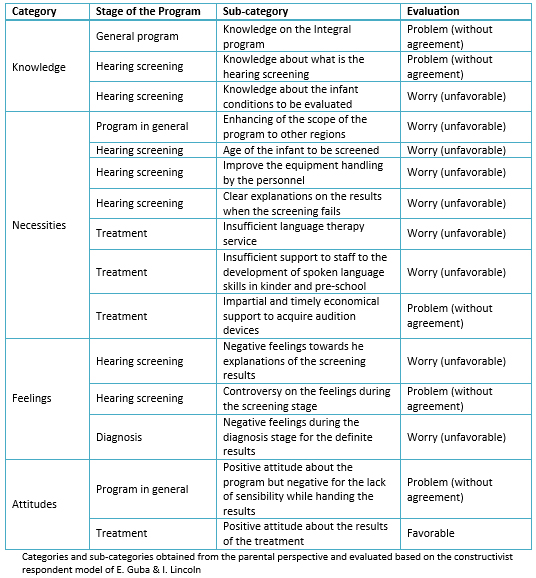 Table 3. Categories and sub-categories (aspects) about the process of the Neonatal Hearing Screening Program.
Table 3. Categories and sub-categories (aspects) about the process of the Neonatal Hearing Screening Program.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCTION
The Universal Newborn Hearing Screening Program in Mexico began in 2010. Its results, published in 2013 by the National Council for the Development and Inclusion of Persons with Disabilities (CONADIS), report low coverage and, currently, there is a dearth of information about its activities. This study describes the process of the program from the epistemological perspective of women whose children participated in the program, evaluating it under the sustenance of the constructivist-respondent model in search of aspects that could help explain its results.
METHODS
Descriptive study with a qualitative approach based on the constructivist–respondent paradigm. We elected the 14 women who participated in the study through trial and number until theoretical saturation. After signing an informed consent form and respecting the confidentiality and anonymity, these women underwent semi-structured interviews that were audio-recorded and transcribed as were conducted. The researchers separately analyzed and coded categories and conjointly summarized categories and subcategories. Validity and reliability were obtained through the credibility, transferability and triangulation.
RESULTS
From the speeches, we obtained the general profile of the interviewed, evolution of their children in the program process and four categories with 15 subcategories related to the reconstruction of the process: knowledge, needs, feelings and attitudes. One was evaluated as favorable, six without agreement and eight as unfavorable. The latter refer to our own context.
CONCLUSIONS
The epistemological perspective of the interviewed women showed aspects that could help explain the low coverage of the program. Attention from public policies could improve this feature. With the establishment of the program, children with deafness are diagnosed and treated at a lower age than before the program.
 Autores:
Maria del Consuelo Martínez Wbaldo[1], María de los Ángeles Torres Lagunas[2]
Autores:
Maria del Consuelo Martínez Wbaldo[1], María de los Ángeles Torres Lagunas[2]

Citación: Martínez Wbaldo MC, Torres Lagunas MA. Qualitative aspects of the process of Neonatal Hearing Screening Program in Mexico evaluated from the parental perspective. Medwave 2016 Dic;16(11):e6798 doi: 10.5867/medwave.2016.11.6798
Fecha de envío: 8/9/2016
Fecha de aceptación: 16/11/2016
Fecha de publicación: 12/12/2016
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Gerner de Garcia B, Gaffney C, Chacon S, Gaffney M. Overview of newborn hearing screening activities in Latin America. Rev Panam Salud Publica. 2011Mar;29(3):145-52. | PubMed |
Gerner de Garcia B, Gaffney C, Chacon S, Gaffney M. Overview of newborn hearing screening activities in Latin America. Rev Panam Salud Publica. 2011Mar;29(3):145-52. | PubMed | Programa DAE. ESPECÍFICO 2007-2012. Tamiz auditivo neonatal e intervención temprana, Secretaria de Salud, México; 2008. | Link |
Programa DAE. ESPECÍFICO 2007-2012. Tamiz auditivo neonatal e intervención temprana, Secretaria de Salud, México; 2008. | Link | Berruecos VP. Tamizaje auditivo neonatal e intervención temprana. Documento de Postura. Mexico, DF.: ANM; 2015. | Link |
Berruecos VP. Tamizaje auditivo neonatal e intervención temprana. Documento de Postura. Mexico, DF.: ANM; 2015. | Link | Sistema de Protección Social en Salud. Informe de resultados. México: DF: Secretaría de Salud; 2013. | Link |
Sistema de Protección Social en Salud. Informe de resultados. México: DF: Secretaría de Salud; 2013. | Link | Yee-Arellano HM, Leal-Garza F, Pauli-Müller K. Universal newborn hearing screening in Mexico: results of the first 2 years. Int J Pediatr Otorhinolaryngol. 2006 Nov;70(11):1863-70. | PubMed |
Yee-Arellano HM, Leal-Garza F, Pauli-Müller K. Universal newborn hearing screening in Mexico: results of the first 2 years. Int J Pediatr Otorhinolaryngol. 2006 Nov;70(11):1863-70. | PubMed | Bolaños M, Flores P, Martínez H. Detección temprana de hipoacusia en población infantil de Tlaxcala. Rev Mex AMCAOF. 2014;3(2):49-5. | Link |
Bolaños M, Flores P, Martínez H. Detección temprana de hipoacusia en población infantil de Tlaxcala. Rev Mex AMCAOF. 2014;3(2):49-5. | Link | Sandoval-García, Iglesias M, SilvaFJ. Frecuencia de hipoacusia neonatal en un hospital privado. Tamizauditivo. Rev Mex Pediatr. 2012;79(4):174-178. | Link |
Sandoval-García, Iglesias M, SilvaFJ. Frecuencia de hipoacusia neonatal en un hospital privado. Tamizauditivo. Rev Mex Pediatr. 2012;79(4):174-178. | Link | Ibar MG. Manual General de Evaluación. España: Octaedro; 2002.
Ibar MG. Manual General de Evaluación. España: Octaedro; 2002.  Cardozo M. La evaluación de las políticas públicas: problemas, metodologías, aportes y limitaciones. Revista de Administración Pública. 1993;(84):167-97. | Link |
Cardozo M. La evaluación de las políticas públicas: problemas, metodologías, aportes y limitaciones. Revista de Administración Pública. 1993;(84):167-97. | Link | Denman C. Haro J. Por los rincones. Antología de métodos cualitativos en investigación social. Religión y Sociedad. 2002; XIV(23). | Link |
Denman C. Haro J. Por los rincones. Antología de métodos cualitativos en investigación social. Religión y Sociedad. 2002; XIV(23). | Link | Guba EG, Lincoln YS. Fourth Generation Evaluation. Beverly Hills, California, EE.UU: Sage; 989:233-243.
Guba EG, Lincoln YS. Fourth Generation Evaluation. Beverly Hills, California, EE.UU: Sage; 989:233-243.  Young A, Tattersall H. Universal newborn hearing screening and early identification of deafness: parents' responses to knowing early and their expectations of child communication development. J Deaf Stud Deaf Educ. 2007 Spring;12(2):209-20. | PubMed |
Young A, Tattersall H. Universal newborn hearing screening and early identification of deafness: parents' responses to knowing early and their expectations of child communication development. J Deaf Stud Deaf Educ. 2007 Spring;12(2):209-20. | PubMed | Núñez-BatallaF, Antuña-León E,González-Trelles T,Carro-Fernández P. Validación del cuestionario de satisfacción de los padres con los programas de cribado auditivo neonatal en español Acta Otorrinolaringol Esp. 2009; 60(2):109-14. | CrossRef |
Núñez-BatallaF, Antuña-León E,González-Trelles T,Carro-Fernández P. Validación del cuestionario de satisfacción de los padres con los programas de cribado auditivo neonatal en español Acta Otorrinolaringol Esp. 2009; 60(2):109-14. | CrossRef | Fox R, Minchom S. Parental experiences of the newborn hearing screening programme in Wales: a postal questionnaire survey. Health Expect. 2008 Dec;11(4):376-83. | CrossRef | PubMed |
Fox R, Minchom S. Parental experiences of the newborn hearing screening programme in Wales: a postal questionnaire survey. Health Expect. 2008 Dec;11(4):376-83. | CrossRef | PubMed | Fitzpatrick E, Angus D, Durieux-Smith A, Graham ID, Coyle D. Parents' needs following identification of childhood hearing loss. Am J Audiol. 2008 Jun;17(1):38-49. | CrossRef | PubMed |
Fitzpatrick E, Angus D, Durieux-Smith A, Graham ID, Coyle D. Parents' needs following identification of childhood hearing loss. Am J Audiol. 2008 Jun;17(1):38-49. | CrossRef | PubMed | Bilsin E, Çuhadar D, Göv P. A review of the relationship between the needs ofmothers who have hearing impairment children and their state-trait anxiety levels. J Pediatr Nurs. 2015 Jan-Feb;30(1):254-61. | CrossRef | PubMed |
Bilsin E, Çuhadar D, Göv P. A review of the relationship between the needs ofmothers who have hearing impairment children and their state-trait anxiety levels. J Pediatr Nurs. 2015 Jan-Feb;30(1):254-61. | CrossRef | PubMed | Vohr BR, Letourneau KS, McDermott C. Maternal worry about neonatal hearing screening. J Perinatol. 2001 Jan-Feb;21(1):15-20. | PubMed |
Vohr BR, Letourneau KS, McDermott C. Maternal worry about neonatal hearing screening. J Perinatol. 2001 Jan-Feb;21(1):15-20. | PubMed | Gilbey P. Qualitative analysis of parents' experience with receiving the news of the detection of their child's hearing loss. Int J Pediatr Otorhinolaryngol. 2010 Mar;74(3):265-70. | CrossRef | PubMed |
Gilbey P. Qualitative analysis of parents' experience with receiving the news of the detection of their child's hearing loss. Int J Pediatr Otorhinolaryngol. 2010 Mar;74(3):265-70. | CrossRef | PubMed | Swanepoel D, Almec N. Maternal views on infant hearing loss and early intervention in a South African community. Int J Audiol. 2008;47 Suppl 1:S44-8. | CrossRef | PubMed |
Swanepoel D, Almec N. Maternal views on infant hearing loss and early intervention in a South African community. Int J Audiol. 2008;47 Suppl 1:S44-8. | CrossRef | PubMed | Alvarenga K F, Gadret JM, Araújo ES, Bevilacqua MC. Triagem auditiva neonatal: motivos da evasão das famílias no processo de detecção precoce. Ver Soc Bras Fonoaudiol. 2012;17(3):241-7. | Link |
Alvarenga K F, Gadret JM, Araújo ES, Bevilacqua MC. Triagem auditiva neonatal: motivos da evasão das famílias no processo de detecção precoce. Ver Soc Bras Fonoaudiol. 2012;17(3):241-7. | Link | Rodríguez G, Gil J, García E. Selección de informantes y recogida de datos. en: Metodología de la investigación cualitativa. Granada: Aljibe; 1999:135-147.
Rodríguez G, Gil J, García E. Selección de informantes y recogida de datos. en: Metodología de la investigación cualitativa. Granada: Aljibe; 1999:135-147.  Bertaux D. From the life-history approach to the transformation of sociological practice. Biography and Society: The life History approach in the social sciences. Beverly Hills, California: Sage; 1981.
Bertaux D. From the life-history approach to the transformation of sociological practice. Biography and Society: The life History approach in the social sciences. Beverly Hills, California: Sage; 1981.  King L, Appleton J. Fourth Generation Evaluation of Health Services: Exploring a Methodology That Offers Equal Voice to Consumer and Professional Stakeholders Qualitative Health Research 1999;(9): 698-710. | CrossRef |
King L, Appleton J. Fourth Generation Evaluation of Health Services: Exploring a Methodology That Offers Equal Voice to Consumer and Professional Stakeholders Qualitative Health Research 1999;(9): 698-710. | CrossRef | Hilú M, Zeigelboim BS. O conhecimento, a valorização da triagem auditiva neonatal e a intervenção precoce da perda auditiva. Ver Cefac. 2007;9(4):563-570. | Link |
Hilú M, Zeigelboim BS. O conhecimento, a valorização da triagem auditiva neonatal e a intervenção precoce da perda auditiva. Ver Cefac. 2007;9(4):563-570. | Link | Pacheco L, Tochetto T, Checalin M, Carvalho C. Information on neonatal hearing screening from pregnant women of different social classe / Triagem auditiva neonatal: informações de gestantes de diferentes classes sociais. Einstein. 2009;7(2):159-162. | Link |
Pacheco L, Tochetto T, Checalin M, Carvalho C. Information on neonatal hearing screening from pregnant women of different social classe / Triagem auditiva neonatal: informações de gestantes de diferentes classes sociais. Einstein. 2009;7(2):159-162. | Link | Tochetto TM, Petry T, GonçalvesMS, Silva ML, Pedroso FS. Sentimentos manifestados por mães frente à triagem auditiva neonatal. Revista CEFAC. 2008;10(4):566-571. | Link |
Tochetto TM, Petry T, GonçalvesMS, Silva ML, Pedroso FS. Sentimentos manifestados por mães frente à triagem auditiva neonatal. Revista CEFAC. 2008;10(4):566-571. | Link | Fitzpatrick E, Graham ID, Durieux-Smith A, Angus D, Coyle D. Parents' perspectives on the impact of the early diagnosis of childhood hearing loss. Int J Audiol. 2007 Feb;46(2):97-106. | PubMed |
Fitzpatrick E, Graham ID, Durieux-Smith A, Angus D, Coyle D. Parents' perspectives on the impact of the early diagnosis of childhood hearing loss. Int J Audiol. 2007 Feb;46(2):97-106. | PubMed | Alvo M. Délano, Paul H. Tamizaje universal de hipoacusia en el recién nacido Revista Hospital Clínico Universitario de Chile. 2010;21(2):170-6. | Link |
Alvo M. Délano, Paul H. Tamizaje universal de hipoacusia en el recién nacido Revista Hospital Clínico Universitario de Chile. 2010;21(2):170-6. | Link | Pittaluga E. Guía clínica: hipoacusia neurosensorial bilateral del prematuro. Gobierno de Chile, Ministerio de Salud; 2009. | Link |
Pittaluga E. Guía clínica: hipoacusia neurosensorial bilateral del prematuro. Gobierno de Chile, Ministerio de Salud; 2009. | Link | Molina AA, de la Peña RA, Cárdenas HJ. El reto de la inclusión y atención integral de niños, niñas y jóvenes con discapacidad en el Distrito Federal. Coedición: Gobierno del Distrito Federal / Fondo de las Naciones Unidas para la Infancia. UNICEF;2006. | Link |
Molina AA, de la Peña RA, Cárdenas HJ. El reto de la inclusión y atención integral de niños, niñas y jóvenes con discapacidad en el Distrito Federal. Coedición: Gobierno del Distrito Federal / Fondo de las Naciones Unidas para la Infancia. UNICEF;2006. | Link | Gerner de Garcia B, Gaffney C, Chacon S, Gaffney M. Overview of newborn hearing screening activities in Latin America. Rev Panam Salud Publica. 2011Mar;29(3):145-52. | PubMed |
Gerner de Garcia B, Gaffney C, Chacon S, Gaffney M. Overview of newborn hearing screening activities in Latin America. Rev Panam Salud Publica. 2011Mar;29(3):145-52. | PubMed |