 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: Thyroid Neoplasms, Thyroid Cancer, Papillary, Thyroidectomy
Papillary thyroid cancer is the most common endocrine malignancy, and due to its favorable prognosis, the extent of surgery has been a matter of debate. About 10% of these tumors are located in the thyroid isthmus, with no specific management in current guidelines. In the last decades, isthmusectomy has been proposed as a therapeutic option for isthmic papillary thyroid carcinoma, although there is no consensus on its management. We present two cases of patients from our institution with solitary isthmic papillary thyroid carcinoma without clinical macroscopic extrathyroidal extension or clinical-radiological lymph node involvement who were treated with isthmusectomy without prophylactic lymph node dissection. Neither of them had any postoperative complications. Both had an intermediate risk of recurrence due to aggressive variants. None of them had signs of recurrence during follow-up. We intend to show that isthmusectomy seems to be an effective and safe surgical alternative in selected patients through these cases.
|
Main messages
|
Thyroid cancer is the most common endocrine malignancy, and its incidence has been rising in the last decades [1]. More than 90% of these tumors are papillary thyroid carcinomas, which usually have a favorable prognosis.
The management of papillary thyroid cancer has shifted to an individualized approach [2], and the initial treatment and extent of surgery have been a matter of debate. The latest evidence [3],[4],[5],[6] supports partial thyroidectomy for well-selected intrathyroidal tumors up to 4 cm without clinical nodal involvement. This recommendation is based on the lack of significant survival and recurrence benefit for total thyroidectomy while benefiting from fewer complications related to the surgical treatment.
Nearly 10% of papillary thyroid carcinomas originate in the isthmus [7],[8],[9], with no specific management recommendations other than the usual partial thyroidectomy or total thyroidectomy approaches [2],[10]. During the last decades, isthmusectomy has arisen as an attractive surgical alternative for these patients [7],[8],[11],[12],[13],[14],[15],[16].
We present two cases of isthmic micropapillary thyroid cancer without clinical macroscopic extrathyroidal extension or clinical-radiological lymph node involvement. Both were treated with isthmusectomy without prophylactic lymph node dissection in our institution. Neither of them had postoperative complications or structural disease at the follow-up. We aim to share our experience treating isthmic papillary thyroid cancer patients with isthmusectomy to show that it is an effective and safe option in well-selected patients.
Both patients gave written permission to publish their cases through informed consent.
The first case is a 45-year-old woman without thyroid cancer risk factors, with a history of anterior cervical volume increase. Physical examination showed a 1 cm, mobile, painless, low-anterior cervical nodule with no clinical lymphadenopathy. She had normal thyroid function, and neck ultrasound found a well-defined 0.9 cm solid hypoechogenic isthmic nodule with microcalcifications. Fine-needle aspiration was performed due to non-specific local symptoms, suspicious ultrasound characteristics, and patient preference. This test informed that the nodule was suspicious for papillary thyroid cancer (Bethesda V).
Pre-operative ultrasound showed no extrathyroidal extension and no lymphadenopathy. Therefore, an isthmusectomy was performed without complications, including no dysphonia, immediate postoperative hypocalcemia, or calcium supplementation requirement. The biopsy confirmed a unifocal 0.9 cm hobnail papillary thyroid carcinoma without extrathyroidal extension, vascular invasion, solid areas, necrosis, mitosis, or lymph node involvement.
According to the American Joint Committee on Cancer Staging Manual (AJCC) 8th edition, the patient was classified as pT1aN0Mx. According to the American Thyroid Association (ATA) 2015 guidelines, the initial risk of recurrence was intermediate.
After 30 months of follow-up, the patient maintained the thyroid-stimulating hormone within normal range without levothyroxine supplementation need, no ultrasound evidence of regional recurrence, undetectable anti-thyroglobulin antibodies, and serum thyroglobulin of 6.0 ng/mL.
The second case is a 45-year-old asymptomatic man without thyroid cancer risk factors. A neck ultrasound was performed in the setting of a pre-operative study for bariatric surgery, finding an irregular 0.83 cm hypoechoic isthmic nodule with microcalcifications. The biochemical pre-operative study yielded normal thyroid function and results compatible with primary hyperparathyroidism. Physical examination showed a 1 cm mobile, painless left-anterior nodule without clinical lymphadenopathies.
Tc99m-sestamibi parathyroid scintigraphy with SPECT/CT scan revealed a hyperfunctioning right upper parathyroid gland. Due to surgical indication for primary hyperparathyroidism, fine-needle aspiration of the thyroid nodule was performed, which informed a lesion suspicious for papillary thyroid cancer (Bethesda V). Pre-operative ultrasound found an intrathyroidal nodule without lymphadenopathies.
An isthmusectomy and right upper parathyroid resection were performed without incidents. Intraoperatively, parathyroid hormone decreased more than 50% and normalized its value, and the patient developed no hypocalcemia or dysphonia. The biopsy confirmed a parathyroid adenoma and a unifocal 0.6 cm of a tall-cell variant of papillary thyroid carcinoma, with minimal extrathyroidal extension to perithyroidal adipose tissue without vascular invasion, necrosis, mitosis, or lymph node involvement.
According to the AJCC 8th edition, the patient was classified as pT1aN0Mx, and the risk of recurrence was intermediate, based on the ATA 2015 guidelines [2].
After 12 months of follow-up, the patient maintained a thyroid-stimulating hormone within normal limits without levothyroxine supplementation, no ultrasound evidence of regional recurrence, undetectable anti-thyroglobulin antibodies, and serum thyroglobulin 14.4 ng/mL, with parathyroid hormone and calcemic values within normal range.
Table 1. Clinical characteristics of the patients
Management of papillary thyroid cancer must be adapted to individual risk of recurrence. In well-selected patients, partial thyroidectomy achieves good disease control, with a very low associated morbidity [2],[3],[4],[5],[6]. When necessary, completion thyroidectomy does not impair the prognosis or increase permanent complications [17].
We present two patients with solitary isthmic micropapillary thyroid cancer without clinical macroscopic extrathyroidal extension or clinical-radiological lymph node involvement, treated with isthmusectomy and without postoperative complications. Both patients were classified with an intermediate risk of recurrence [2],[10]: the first was a hobnail variant, and the second was a tall cell variant with minimal extrathyroidal extension. None of them had signs of structural disease at follow-up. Their clinical characteristics are summarized in Table 1.
Partial thyroidectomy usually consists of lobectomy plus isthmusectomy. However, in the subgroup of patients with papillary thyroid carcinoma limited to the isthmus, isthmusectomy alone has been considered as an attractive surgical alternative [7],[8],[11],[12],[13],[14],[15],[16] – aiming to reduce associated surgical morbidity. Although it has been reported that near 10% of papillary thyroid cancers are located in the isthmus [7],[8],[9], in Nixon et al. series, only 1% of 1810 patients with papillary thyroid cancer had an isolated and intrathyroidal lesion in the isthmus without nodal involvement; therefore, these patients could be candidates for isthmusectomy [8]. Tuttle et al. endorse isthmusectomy as a suitable treatment for papillary thyroid cancer confined to the isthmus, proposing a clinical framework to help select low-risk patients [13]. Although both of our cases were papillary thyroid carcinomas smaller than 1 cm, isthmusectomy can still be an appropriate surgical option for larger tumors when they are intrathyroidal and with no evidence of lymph node involvement [13]. This latter aspect underpins the importance of a reliable pre-operative ultrasound.
Evidence for isthmusectomy is scant and contradictory. Some studies show an increased number of multifocal disease, lymph node involvement, and extrathyroidal extension of isthmic papillary thyroid cancer [9],[19],[20],[21],[22],[23]. Wang et al. suggest that total thyroidectomy with prophylactic central dissection is a better surgical option than isthmusectomy, due to the frequent involvement of central lymph nodes (pN1 38-71%), especially in those younger than 38 years and tumors larger than 0.6 cm [23]. However, in the absence of clinical-radiological nodal involvement, multiple studies have demonstrated that prophylactic central lymph node dissection detects clinically non-significant disease without a benefit in recurrence decrease [6],[24],[25] but exposes patients to a higher risk of complications in both total thyroidectomy and partial thyroidectomy [25].
Isthmusectomy achieves adequate disease control in well-selected patients, with disease-specific survival rates of 100% and long-time disease-free survival rates of nearly 95%, similar to total thyroidectomy and lobectomy approaches [7],[8],[11],[12],[13],[14],[15],[16].
As a surgical procedure, isthmusectomy does not expose the tracheoesophageal grooves and is associated with fewer postoperative complications than total thyroidectomy and lobectomy, which expose the patient to the risk of developing hypoparathyroidism and dysphonia [8],[11],[12],[14],[15],[21]. Seo et al. found no postoperative complications in the isthmusectomy group, except for one case of transient hypoparathyroidism (9% of all isthmusectomies) [15]. It is important to note that in Seo et al. study, prophylactic central lymph node dissection was performed in about 90% of the patients undergoing isthmusectomy, so the number of complications associated with isolated isthmusectomy could be even lower, with reported rates as low as 0% [7],[8],[14]. Additionally, recent evidence has shown that partial thyroidectomy (including cases with isthmusectomy) is associated with a better quality of life than total thyroidectomy in patients with low-risk papillary thyroid cancer, even if completion thyroidectomy is needed [26].
One of our cases had minimal extrathyroidal extension, which is the main indication for early completion thyroidectomy in most series. However, growing evidence shows that this feature is not associated with recurrence and mortality, suggesting that its presence alone should not be considered an indication for completion thyroidectomy [3],[10],[27],[28],[29].
Both of our cases had aggressive variants of papillary thyroid cancer and intermediate risk of recurrence according to the ATA 2015 guidelines. Although the tall cell variant in micropapillary thyroid carcinoma is associated with a more aggressive presentation, it has no impact on disease-specific survival [27]; therefore, this was not considered as an indication for completion in our patient. For example, in Park et al. series, 16% of the patients had tall cell variant papillary thyroid cancer, with no differences in survival and recurrence compared to the rest of the patients [14]. Even though there is no specific evidence of the prognostic impact of the hobnail variant in micropapillary thyroid carcinoma, it shares some genetic and molecular mechanisms with the tall cell variant, such as a mutation in the BRAF gene. Considering that there is no benefit of radioiodine ablation in micropapillary thyroid carcinomas with mutated BRAF gene [2], it could be argued that the hobnail variant of a micropapillary thyroid carcinoma should not worsen prognosis if completion thyroidectomy is not performed.
The need for levothyroxine supplementation is lower through a partial thyroidectomy than a complete thyroidectomy [6]. Furthermore, the isthmusectomy approach requires even less postoperative hypothyroidism because of the minimum resection of thyroid tissue [7]. Levothyroxine is required in 9.1% of patients undergoing this isthmusectomy compared to 42.5% and 100% of those undergoing partial thyroidectomy and total thyroidectomy, respectively [15].
Cervical ultrasound is the mainstay in the follow-up of patients with papillary thyroid cancer treated with partial thyroidectomy [30]. A serum thyroglobulin cut-off value and its trend over time have been proposed to assess recurrence in these patients. However, the latest evidence shows that neither a specific serum thyroglobulin threshold nor its trend over time is related to structural recurrence [6],[30],[31]. Patients undergoing isthmusectomy may have higher serum Thyroglobulin concentrations than those undergoing partial thyroidectomy because they preserve more thyroid tissue [7]. And thus, it is likely that these patients may not achieve an excellent biochemical response according to the ATA 2015 guidelines. However, this should not be of concern if the ultrasound shows no evidence of structural recurrence.
Despite being only two cases with a close follow-up, it is remarkable that these patients were managed by a multidisciplinary team, which carefully defines the intensity of treatment and follow-up according to their initial risk of recurrence and response to treatment.
We report two cases of patients with isthmic papillary thyroid carcinoma treated with isthmusectomy without prophylactic lymph node dissection with excellent surgical outcomes. The management of papillary thyroid cancer has shifted to an individualized approach, supporting partial thyroidectomy for well-selected patients. There is no specific management for papillary thyroid cancer located in the thyroid isthmus in international guidelines. In selected patients with intrathyroidal papillary thyroid carcinoma limited to the isthmus without clinical macroscopic extrathyroidal extension or clinical-radiological lymph node involvement, isthmusectomy seems to be an effective and safe surgical approach.
Contribution roles
RIOB-JMDR: Conceptualization, Methodology, Investigation, Resources, Writing – Original Draft Preparation, Writing – Review & Editing, Supervision, Project Administration. JALR-FDC: Conceptualization, Methodology, Investigation, Resources, Writing – Original Draft Preparation, Writing – Review & Editing.
Competing interests
None of the authors had any potential competing interests. Each author provided a signed ICMJE statement of interests.
Funding
There was no funding for this work.
Ethics
Ethical approval was not necessary given the nature of a case report article. Both patients gave written permission to publish their cases through informed consent.

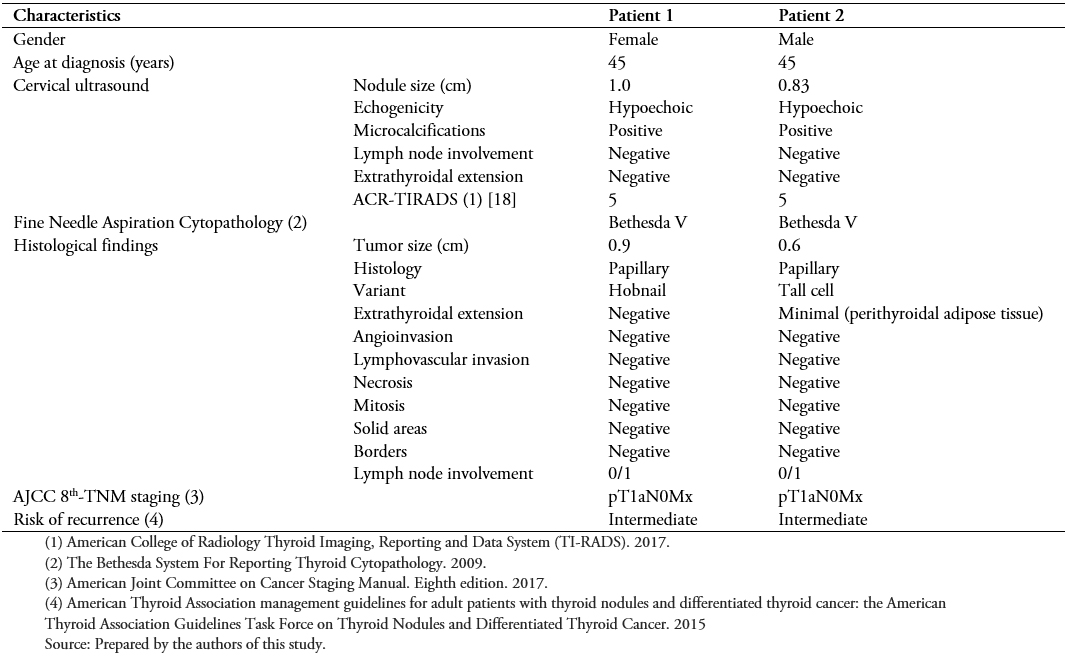 Table 1. Clinical characteristics of the patients
Table 1. Clinical characteristics of the patients

Papillary thyroid cancer is the most common endocrine malignancy, and due to its favorable prognosis, the extent of surgery has been a matter of debate. About 10% of these tumors are located in the thyroid isthmus, with no specific management in current guidelines. In the last decades, isthmusectomy has been proposed as a therapeutic option for isthmic papillary thyroid carcinoma, although there is no consensus on its management. We present two cases of patients from our institution with solitary isthmic papillary thyroid carcinoma without clinical macroscopic extrathyroidal extension or clinical-radiological lymph node involvement who were treated with isthmusectomy without prophylactic lymph node dissection. Neither of them had any postoperative complications. Both had an intermediate risk of recurrence due to aggressive variants. None of them had signs of recurrence during follow-up. We intend to show that isthmusectomy seems to be an effective and safe surgical alternative in selected patients through these cases.
 Autores:
Roberto Ignacio Olmos Borzone[1,4], Jorge Andrés López Ruiz-Esquide[2], Francisco Domínguez Covarrubias[3], José Miguel Domínguez Ruiz-Tagle[1,4]
Autores:
Roberto Ignacio Olmos Borzone[1,4], Jorge Andrés López Ruiz-Esquide[2], Francisco Domínguez Covarrubias[3], José Miguel Domínguez Ruiz-Tagle[1,4]

Citación: Olmos Borzone RI, López Ruiz-Esquide JA, Domínguez Covarrubias F, Domínguez Ruiz-Tagle JM. Isthmusectomy for well-differentiated thyroid carcinoma located to the isthmus: A report of two cases and review of the literature. Medwave 2021;21(10):e8493 doi: 10.5867/medwave.2021.10.8493
Fecha de envío: 4/4/2021
Fecha de aceptación: 17/10/2021
Fecha de publicación: 29/11/2021
Origen: No solicitado
Tipo de revisión: Con revisión externa por tres pares revisores, a doble ciego en primera ronda

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol. 2016 Nov;12(11):646-653. | CrossRef | PubMed |
Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol. 2016 Nov;12(11):646-653. | CrossRef | PubMed | Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016 Jan;26(1):1-133. | CrossRef | PubMed |
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016 Jan;26(1):1-133. | CrossRef | PubMed | Nixon IJ, Ganly I, Patel S, Palmer FL, Whitcher MM, Tuttle RM, et al. The impact of microscopic extrathyroid extension on outcome in patients with clinical T1 and T2 well-differentiated thyroid cancer. Surgery. 2011 Dec;150(6):1242-9. | CrossRef | PubMed |
Nixon IJ, Ganly I, Patel S, Palmer FL, Whitcher MM, Tuttle RM, et al. The impact of microscopic extrathyroid extension on outcome in patients with clinical T1 and T2 well-differentiated thyroid cancer. Surgery. 2011 Dec;150(6):1242-9. | CrossRef | PubMed | Vaisman F, Momesso D, Bulzico DA, Pessoa CH, da Cruz MD, Dias F, et al. Thyroid Lobectomy Is Associated with Excellent Clinical Outcomes in Properly Selected Differentiated Thyroid Cancer Patients with Primary Tumors Greater Than 1 cm. J Thyroid Res. 2013;2013:398194. | CrossRef | PubMed |
Vaisman F, Momesso D, Bulzico DA, Pessoa CH, da Cruz MD, Dias F, et al. Thyroid Lobectomy Is Associated with Excellent Clinical Outcomes in Properly Selected Differentiated Thyroid Cancer Patients with Primary Tumors Greater Than 1 cm. J Thyroid Res. 2013;2013:398194. | CrossRef | PubMed | Song E, Han M, Oh HS, Kim WW, Jeon MJ, Lee YM, et al. Lobectomy Is Feasible for 1-4 cm Papillary Thyroid Carcinomas: A 10-Year Propensity Score Matched-Pair Analysis on Recurrence. Thyroid. 2019 Jan;29(1):64-70. | CrossRef | PubMed |
Song E, Han M, Oh HS, Kim WW, Jeon MJ, Lee YM, et al. Lobectomy Is Feasible for 1-4 cm Papillary Thyroid Carcinomas: A 10-Year Propensity Score Matched-Pair Analysis on Recurrence. Thyroid. 2019 Jan;29(1):64-70. | CrossRef | PubMed | Olmos R, López J, Donoso F, Ruiz-Esquide M, Zegers T, Lustig N, et al. Manejo de nódulos tiroideos y cáncer de tiroides con lobectomía: experiencia de un equipo multidisciplinario. Rev Chil Endocrinol y Diabetes. 2020;13(3):118–24. | Link |
Olmos R, López J, Donoso F, Ruiz-Esquide M, Zegers T, Lustig N, et al. Manejo de nódulos tiroideos y cáncer de tiroides con lobectomía: experiencia de un equipo multidisciplinario. Rev Chil Endocrinol y Diabetes. 2020;13(3):118–24. | Link | Sugenoya A, Shingu K, Kobayashi S, Masuda H, Takahashi S, Shimizu T, et al. Surgical strategies for differentiated carcinoma of the thyroid isthmus. Head Neck. 1993 Mar-Apr;15(2):158-60. | CrossRef | PubMed |
Sugenoya A, Shingu K, Kobayashi S, Masuda H, Takahashi S, Shimizu T, et al. Surgical strategies for differentiated carcinoma of the thyroid isthmus. Head Neck. 1993 Mar-Apr;15(2):158-60. | CrossRef | PubMed | Nixon IJ, Palmer FL, Whitcher MM, Shaha AR, Shah JP, Patel SG, et al. Thyroid isthmusectomy for well-differentiated thyroid cancer. Ann Surg Oncol. 2011 Mar;18(3):767-70. | CrossRef | PubMed |
Nixon IJ, Palmer FL, Whitcher MM, Shaha AR, Shah JP, Patel SG, et al. Thyroid isthmusectomy for well-differentiated thyroid cancer. Ann Surg Oncol. 2011 Mar;18(3):767-70. | CrossRef | PubMed | Lee YS, Jeong JJ, Nam KH, Chung WY, Chang HS, Park CS. Papillary carcinoma located in the thyroid isthmus. World J Surg. 2010 Jan;34(1):36-9. | CrossRef | PubMed |
Lee YS, Jeong JJ, Nam KH, Chung WY, Chang HS, Park CS. Papillary carcinoma located in the thyroid isthmus. World J Surg. 2010 Jan;34(1):36-9. | CrossRef | PubMed | Tala H, Díaz R, Domínguez JM, Pineda P, Olmos R, Munizaga F, et al. Protocolo Clínico Cáncer Diferenciado de Tiroides Programa de Cáncer del Adulto 2020. Sociedad Chilena de Endocrinología y Diabetes. 2020. | Link |
Tala H, Díaz R, Domínguez JM, Pineda P, Olmos R, Munizaga F, et al. Protocolo Clínico Cáncer Diferenciado de Tiroides Programa de Cáncer del Adulto 2020. Sociedad Chilena de Endocrinología y Diabetes. 2020. | Link | Skilbeck C, Leslie A, Simo R. Thyroid isthmusectomy: a critical appraisal. J Laryngol Otol. 2007 Oct;121(10):986-9. | CrossRef | PubMed |
Skilbeck C, Leslie A, Simo R. Thyroid isthmusectomy: a critical appraisal. J Laryngol Otol. 2007 Oct;121(10):986-9. | CrossRef | PubMed | Huang H, Liu S-Y, Ni S, Zhang Z-M, Wang X-L, Xu Z-G. Treatment Outcome of Papillary Carcinoma Confined to the Thyroid Isthmus. J Cancer Ther. 2016 Nov;07(12):963–9. | CrossRef |
Huang H, Liu S-Y, Ni S, Zhang Z-M, Wang X-L, Xu Z-G. Treatment Outcome of Papillary Carcinoma Confined to the Thyroid Isthmus. J Cancer Ther. 2016 Nov;07(12):963–9. | CrossRef | Tuttle RM, Zhang L, Shaha A. A clinical framework to facilitate selection of patients with differentiated thyroid cancer for active surveillance or less aggressive initial surgical management. Expert Rev Endocrinol Metab. 2018 Mar;13(2):77-85. | CrossRef | PubMed |
Tuttle RM, Zhang L, Shaha A. A clinical framework to facilitate selection of patients with differentiated thyroid cancer for active surveillance or less aggressive initial surgical management. Expert Rev Endocrinol Metab. 2018 Mar;13(2):77-85. | CrossRef | PubMed | Park H, Harries V, McGill MR, Ganly I, Shah JP. Isthmusectomy in selected patients with well-differentiated thyroid carcinoma. Head Neck. 2020 Jan;42(1):43-49. | CrossRef | PubMed |
Park H, Harries V, McGill MR, Ganly I, Shah JP. Isthmusectomy in selected patients with well-differentiated thyroid carcinoma. Head Neck. 2020 Jan;42(1):43-49. | CrossRef | PubMed | Seo HW, Song CM, Ji YB, Jeong JH, Koo HR, Tae K. Surgical Outcomes and Efficacy of Isthmusectomy in Single Isthmic Papillary Thyroid Carcinoma: A Preliminary Retrospective Study. J Invest Surg. 2021 Oct;34(10):1129-1134. | CrossRef | PubMed |
Seo HW, Song CM, Ji YB, Jeong JH, Koo HR, Tae K. Surgical Outcomes and Efficacy of Isthmusectomy in Single Isthmic Papillary Thyroid Carcinoma: A Preliminary Retrospective Study. J Invest Surg. 2021 Oct;34(10):1129-1134. | CrossRef | PubMed | Gui Z, Wang Z, Xiang J, Sun W, He L, Dong W, et al. Comparison of Outcomes Following Thyroid Isthmusectomy, Unilateral Thyroid Lobectomy, and Total Thyroidectomy in Patients with Papillary Thyroid Microcarcinoma of the Thyroid Isthmus: A Retrospective Study at a Single Center. Med Sci Monit. 2020 Dec 22;26:e927407. | CrossRef | PubMed |
Gui Z, Wang Z, Xiang J, Sun W, He L, Dong W, et al. Comparison of Outcomes Following Thyroid Isthmusectomy, Unilateral Thyroid Lobectomy, and Total Thyroidectomy in Patients with Papillary Thyroid Microcarcinoma of the Thyroid Isthmus: A Retrospective Study at a Single Center. Med Sci Monit. 2020 Dec 22;26:e927407. | CrossRef | PubMed | Gulcelik MA, Dogan L, Akgul GG, Güven EH, Ersöz Gulcelik N. Completion Thyroidectomy: Safer than Thought. Oncol Res Treat. 2018;41(6):386-390. | CrossRef | PubMed |
Gulcelik MA, Dogan L, Akgul GG, Güven EH, Ersöz Gulcelik N. Completion Thyroidectomy: Safer than Thought. Oncol Res Treat. 2018;41(6):386-390. | CrossRef | PubMed | Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA,et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017 May;14(5):587-595. | CrossRef | PubMed |
Tessler FN, Middleton WD, Grant EG, Hoang JK, Berland LL, Teefey SA,et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol. 2017 May;14(5):587-595. | CrossRef | PubMed | Karatzas T, Charitoudis G, Vasileiadis D, Kapetanakis S, Vasileiadis I. Surgical treatment for dominant malignant nodules of the isthmus of the thyroid gland: A case control study. Int J Surg. 2015 Jun;18:64-8. | CrossRef | PubMed |
Karatzas T, Charitoudis G, Vasileiadis D, Kapetanakis S, Vasileiadis I. Surgical treatment for dominant malignant nodules of the isthmus of the thyroid gland: A case control study. Int J Surg. 2015 Jun;18:64-8. | CrossRef | PubMed | Song CM, Lee DW, Ji YB, Jeong JH, Park JH, Tae K. Frequency and pattern of central lymph node metastasis in papillary carcinoma of the thyroid isthmus. Head Neck. 2016 Apr;38 Suppl 1:E412-6. | CrossRef | PubMed |
Song CM, Lee DW, Ji YB, Jeong JH, Park JH, Tae K. Frequency and pattern of central lymph node metastasis in papillary carcinoma of the thyroid isthmus. Head Neck. 2016 Apr;38 Suppl 1:E412-6. | CrossRef | PubMed | Vasileiadis I, Boutzios G, Karalaki M, Misiakos E, Karatzas T. Papillary thyroid carcinoma of the isthmus: Total thyroidectomy or isthmusectomy? Am J Surg. 2018 Jul;216(1):135-139. | CrossRef | PubMed |
Vasileiadis I, Boutzios G, Karalaki M, Misiakos E, Karatzas T. Papillary thyroid carcinoma of the isthmus: Total thyroidectomy or isthmusectomy? Am J Surg. 2018 Jul;216(1):135-139. | CrossRef | PubMed | Liu H, Li Y, Xiang J. Papillary Carcinoma of Thyroid Nodule if Located in Isthmus Is Associated with Greater Disease Progression: a Systematic Review and Meta-analysis. Indian J Surg. 2020 May 12;82(6):1212–8. | CrossRef |
Liu H, Li Y, Xiang J. Papillary Carcinoma of Thyroid Nodule if Located in Isthmus Is Associated with Greater Disease Progression: a Systematic Review and Meta-analysis. Indian J Surg. 2020 May 12;82(6):1212–8. | CrossRef | Wang J, Sun H, Gao L, Xie L, Cai X. Evaluation of thyroid isthmusectomy as a potential treatment for papillary thyroid carcinoma limited to the isthmus: A clinical study of 73 patients. Head Neck. 2016 Apr;38 Suppl 1:E1510-4. | CrossRef | PubMed |
Wang J, Sun H, Gao L, Xie L, Cai X. Evaluation of thyroid isthmusectomy as a potential treatment for papillary thyroid carcinoma limited to the isthmus: A clinical study of 73 patients. Head Neck. 2016 Apr;38 Suppl 1:E1510-4. | CrossRef | PubMed | Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012 Nov;22(11):1144-52. | CrossRef | PubMed |
Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012 Nov;22(11):1144-52. | CrossRef | PubMed | Viola D, Materazzi G, Valerio L, Molinaro E, Agate L, Faviana P, et al. Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab. 2015 Apr;100(4):1316-24. | CrossRef | PubMed |
Viola D, Materazzi G, Valerio L, Molinaro E, Agate L, Faviana P, et al. Prophylactic central compartment lymph node dissection in papillary thyroid carcinoma: clinical implications derived from the first prospective randomized controlled single institution study. J Clin Endocrinol Metab. 2015 Apr;100(4):1316-24. | CrossRef | PubMed | Moon JH, Ryu CH, Cho SW, Choi JY, Chung EJ, Hah JH, et al. Effect of Initial Treatment Choice on 2-year Quality of Life in Patients with Low-risk Papillary Thyroid Microcarcinoma. J Clin Endocrinol Metab. 2021 Mar 8;106(3):724-735. | CrossRef | PubMed |
Moon JH, Ryu CH, Cho SW, Choi JY, Chung EJ, Hah JH, et al. Effect of Initial Treatment Choice on 2-year Quality of Life in Patients with Low-risk Papillary Thyroid Microcarcinoma. J Clin Endocrinol Metab. 2021 Mar 8;106(3):724-735. | CrossRef | PubMed | Kuo EJ, Goffredo P, Sosa JA, Roman SA. Aggressive variants of papillary thyroid microcarcinoma are associated with extrathyroidal spread and lymph-node metastases: a population-level analysis. Thyroid. 2013 Oct;23(10):1305-11. | CrossRef | PubMed |
Kuo EJ, Goffredo P, Sosa JA, Roman SA. Aggressive variants of papillary thyroid microcarcinoma are associated with extrathyroidal spread and lymph-node metastases: a population-level analysis. Thyroid. 2013 Oct;23(10):1305-11. | CrossRef | PubMed | Al-Qurayshi Z, Shama MA, Randolph GW, Kandil E. Minimal extrathyroidal extension does not affect survival of well-differentiated thyroid cancer. Endocr Relat Cancer. 2017 May;24(5):221-226. | CrossRef | PubMed |
Al-Qurayshi Z, Shama MA, Randolph GW, Kandil E. Minimal extrathyroidal extension does not affect survival of well-differentiated thyroid cancer. Endocr Relat Cancer. 2017 May;24(5):221-226. | CrossRef | PubMed | Diker-Cohen T, Hirsch D, Shimon I, Bachar G, Akirov A, Duskin-Bitan H, et al. Impact of Minimal Extra-Thyroid Extension in Differentiated Thyroid Cancer: Systematic Review and Meta-analysis. J Clin Endocrinol Metab. 2018 Mar 1. | CrossRef | PubMed |
Diker-Cohen T, Hirsch D, Shimon I, Bachar G, Akirov A, Duskin-Bitan H, et al. Impact of Minimal Extra-Thyroid Extension in Differentiated Thyroid Cancer: Systematic Review and Meta-analysis. J Clin Endocrinol Metab. 2018 Mar 1. | CrossRef | PubMed |