 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: encephalopathy, hearing loss, microangiopathy, Susac syndrome, retinocochleocerebral vasculopathy, autoimmune endotheliopathy
Susac Syndrome is a rare entity, characterized by a triad of subacute encephalopathy, retinal artery occlusion and sensorineural hearing loss. It is more common in women and the age of onset fluctuates between 9-58 years of age. The pathogenesis is presented as microangiopathic changes at the cerebral, retinal and cochlear levels associated with an autoimmune mechanism. We present the case of a 31-year-old woman who started with a diffuse headache, puerile behavior, bradylalia and somnolence. As the disease progressed, she had auditory deficit and arterial obstruction of the right temporal retinal branch in retinal fluorescein angiography. Brain magnetic resonance showed rounded hyperintense lesions in the corpus callosum, periventricular region and cerebellum. This is the first reported case of Susac Syndrome in Peru, presented with the classic triad, which is an infrequent presentation. However, cases that show incomplete forms should be evaluated in a timely manner to initiate timely treatment and avoid irreversible consequences.
Susac syndrome is a rare disorder, initially described by John Susac in 1979, who reported two female cases with the classical triad of subacute encephalopathy, retinal artery occlusion and sensorineural hearing loss [1]. Susac syndrome is more common in women, with ratio of 3:1, the age of onset fluctuates between 9 and 58 years [2]. Currently, there have been reported 405 cases all over the world [3]; of which seven correspond to South America, five in Argentina [4], one in Brazil and one in Colombia [5].
It is little known about Susac syndrome pathogenesis [6]; however, microangiopathic damage within the brain, retina and cochlea, together with autoimmune mechanisms have been suggested. An inflammatory response has been documented in many cases, including non-specific antiendothelial cell antibodies and the favorable response to immunomodulatory therapy [7].
The encephalopathic manifestations are characterized by intense headache, sometimes with migraine type attacks. There are behavioral abnormalities such as aggressiveness, paranoia, apathy and depression; cognitive compromise can manifest with memory loss, confabulation, visuospatial dysfunction, decreased attention and concentration, disorientation and progressive compromise of consciousness leading to lethargy. Along this period, urinary incontinence and generalized seizures may occur in some cases [8]. Visual symptoms are reported as scotomas, photopsies, and decreased visual acuity mostly associated to compromise of central retina. Since, some patients may be asymptomatic, it is advisable to perform a fluorescein angiography that may show occlusion of retinal arteries distal to vessel bifurcations and hyperfluorescence of arterial walls [6]. The typical sensorineural hearing loss of this syndrome reveals the involvement of low and middle frequencies in audiometry, mainly caused by microinfarcts in the apical cochlea and may be the first and isolated symptom of the disease [9]. Hearing loss together with visual compromise are irreversible in most patients, and may have a rapidly progression [10].
Sagittal T2, FLAIR (Fluid attenuated inversion recovery) and T1 Brain MRI show microinfarcts of the central fibers of the corpus callosum with relative preservation of the peripheral fibers in. These findings have "snowballs" like appearance that become "holes" overtime. This particular sign is only described in Susac syndrome, and not in other autoimmune diseases such as vasculitis, multiple sclerosis or acute disseminated encephalomyelitis [11],[12]. In addition, microinfarcts can be found in the inner capsule, especially in the DWI sequence (Diffusion weighted Magnetic Resonance Imaging) that has the appearance of a "pearl necklace"; both findings are pathognomonic of Susac syndrome [9],[13].
Early diagnosis is essential to ensure immediate initiation of immunosuppressive therapy; at first, high-dose intravenous corticosteroids followed by oral corticosteroids combined with low doses of acetylsalicylic acid [14]. However, an immunosuppressant such as mycophenolate or azathioprine can be used as second line treatment of this entity [15]. We report the first case of Susac's syndrome in Peru manifesting the classical triad of this disorder.
A 31 year-old woman, suddenly complained abdominal pain, nausea, vomiting and diarrhea with self-limited course. A week later, the patient presented a moderate and diffuse headache followed by general malaise, apathy and hyporexia. Days prior to admission she had a childish like behavior with difficulty for recognizing their relatives, she was partially disoriented in time and place, slow for daily living activities, showed slurred speech, as well as drowsiness. She did not report any visual or auditory symptoms.
At physical examination at admission, she presented bradypsychia and sleepiness, non-fluent dysarthric language, she could understand and repeat words, but she was irritable. Muscular strength was preserved, with generalized hyperreflexia. She was severely ataxic with no possibility of walking. There was no neck rigidity neither other meningeal signs.
Routine hematimetry and biochemistry lab workup was normal. ANA, ANCAc and ANCAp antibodies were negative. The CSF (cerebrospinal fluid) analysis showed proteins 185 mg/dl, glucose 58 mg/dl; 7 cells, 98% lymphocytes, 2% polymorphonuclear, oligoclonal bands were negative. Two brain MRI images were performed two weeks apart between them, showing numerous small white matter hyperintensities in T2 and FLAIR protocols mostly located on the corpus callosum, cerebral hemispheres, peri and supraventricular, without edema, Figure 1(A and B). Other hyperintensities with similar patterns were also seen in the midbrain, middle cerebellar peduncles, and both cerebellar hemispheres. There was no evidence of contrast uptake.
Figure 1. Brain magnetic resonance FLAIR protocol.
A demyelinating disease with probable autoimmune etiology was initially proposed, and pulses of IV methylprednisolone 1 g/day were started for five days; followed by prednisone 1 mg/kg/day, with improvement observed by the fifth day of treatment. The patient was awake, fully oriented, fluent language, less negativist and irritable and able to walk with minimal support. However, on the tenth day of hospitalization, she complained hearing loss, dizziness and tinnitus with left side predominance, the audiometry showed sensorineural hearing loss of 40 dB in the right ear and 45 dB in the left, Figure 2.
Figure 2. Audiometry showing low and medium tone neurosensory hearing loss.
Considering the clinical features, neuroimaging and auditory compromise, the probable diagnosis of Susac's syndrome was considered. An ophthalmologic examination showed an obstruction of the temporal branch of the retinal artery of the right eye; this finding was corroborated in retinal fluorescein angiography, where multiple were disseminated arteriolar obstruction injuries were observed, Figure 3. Acetyl salicylic acid and mycophenolate were added to the treatment. At the time of medical discharge, the patient was alert, fully oriented, with fluent language, able to walk without support, was independent for daily-life activities and slight hearing improvement. At one-month follow-up she complained blurred vision without limiting her daily routine.
Figura 3. Retinal fluorescein angiography.
Susac syndrome is a very rare disorder, although cases have been reported in many regions of the world, most cases are from North America and Europe [15]; this is the first case reported in Peru. Just like this case, this entity occurs most often in young women, between 30 and 40 years of age [3],[5].
Most of Susac syndrome cases do not present the classic clinical triad; the few fully symptomatic cases reach only 13% [16]. The period between the first and third typical symptoms should be taken into account, as it may take up to 5 months to complete the triad [17]. In this case the clinical condition was completed approximately three months after the onset of symptoms; however, the triad could be previously documented by retinal fluorescein angiography, consistent with diagnostic criteria for definitive Susac syndrome. Susac syndrome diagnosis criteria were recently published by Ilka Kleffner et al. [18], in which definitive Susac syndrome is defined by clinical or paraclinical compromise involving the three targets (brain, retina and vestibulocochlear system) and probable Susac syndrome when there is an unequivocal clinical or paraclinical damage of two of the three involved targets (Table 1).
Table 1. Criteria for the diagnosis of Susac syndrome.
Few other disorders like Behcet's Disease, Marchiafava-Bignami's Disease or Cogan's Syndrome may occur with very similar clinical traits and share some components with Susac syndrome. [19],[20],[21] (Table 2) [11],[12],[19],[20],[21..
Table 2. Summary table of major differential diagnoses.
Encephalopathy is usually mild in most cases, however it may be subclinical or the dominant symptom and its severity does not correlate with the severity of initial neurological symptoms [16]. In this case, encephalopathy was the most prominent manifestation, and had a moderate degree of severity. The encephalopathic condition occurs in 60-70% of patients and may appear as deficits in various cognitive domains, usually presenting confusion or personality changes, mood disorders, and even psychotic symptoms; abulia may also be present and then progress to a stage where verbal and non-verbal communication is no longer possible [22]. Cognitive dysfunction is variable; some studies have mainly described psychomotor slowness and bradypsychia, while others indicated more specific symptoms in memory, attention and operating skills [23].
The patient had changes in behavior traits of aggressiveness, bradypsychia, apathy, decreased attention, poor concentration and cognitive impairment with memory loss, associated with persistent oppressive headache. Such symptoms not allow her to properly interact with her environment. Headache is currently considered a common symptom and is mainly relevant when of sudden onset with migraine or oppressive pattern [16].
The literature shows that the hearing loss is acute and can develop suddenly; even patients may wake up deaf in one ear and lose hearing on the other side in a short period of time (days to weeks) [24]. In this patient, hearing loss was not one of the initial symptoms; however, over the course of the disease, the auditory deficit first appeared in the left ear, where the deficit predominated and days later in the right side; these findings were corroborated in tonal and vocal audiometry, showing compromise of low and middle frequencies; which is consistent with other reported cases where hearing loss may be bilateral and asymmetric [18]. As part of the vestibulocochlear symptoms, tinnitus or vertigo may also be associated [25]; the patient presented fugitive tinnitus in the evolution, no evidence of nystagmus was reported despite having reported that she felt dizzy, so we cannot suggest the presence of peripheral vertigo [26].
The ophthalmologic examination in the Susac syndrome comprises fundoscopy, the fluorescein assessment (to determine the occlusion of the retinal arterial branches) and the optical coherence tomography in which damage of the inner layers of the retina is observed [27],[28]. These tests are useful for documenting retinal involvement independently of visual symptoms. In this case, fundoscopy revealed obstruction of the temporal branch of the retinal artery of the right eye confirmed by retinal fluorescein angiography. No retinal ischemic whitening, cotton patches, periarterial whitening, box segmentation or cherry red spotting were found that can also be found in the fundus [29]. Retinal artery obstruction is a common finding in Susac syndrome, as shown in a series of cases where it was reported in 100% of the patients included, most of whom remained asymptomatic for a long time [14]. Despite this, it should be emphasized that fundoscopy is less sensitive than fluorescein angiography to detect arterial occlusions [14].
The brain MRI of this case showed rounded FLAIR and T2 hyperintense lesions in in the corpus callosum, white matter, periventricular region and cerebellum. Similar findings have been described in other Susac syndrome reports where hyperintense, multifocal, and round lesions (snowball) are reported, and at least one of them is located in the corpus callosum, consistent with series of five cases in United States. In addition, corpus callosum atrophy can be associated with compensatory ventriculomegaly and in the diffusion of restriction areas [16],[30].
In approximately 45% of Susac syndrome cases, cerebrospinal fluid shows mild pleocytosis [16]; unspecific increased protein level as we found in this case, which was also described by Dorr et al. in a study where 67% of cases revealed lymphocytic pleocytosis and high protein content in the cerebrospinal fluid [17]; although the importance of this study is to rule out other possible etiologies [16].
There is no consensus in the treatment of Susac syndrome; but empirical treatment is administered based on the pathophysiological hypothesis of autoimmune inflammatory mechanisms. So, in the acute phase, high-dose corticosteroids intravenously is administered and, to prevent relapse, treatment with immunosuppressants was received by the reported patient [15].
This is the first case of Susac syndrome presented in Peru, with a clinical condition including the characteristic triad. Symptoms were objectified with imaging and functional auxiliary tests, so it is concluded that it is a defined Susac syndrome. It should be noted that cases presenting only an encephalopathy condition, hearing loss or visual disturbances should be considered in the differential diagnosis for this syndrome, and if further analyses confirm it, the early treatment may prevent irreversible consequences.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The informed consent requested by Medwave, has been signed by the patient; a copy of which was sent to the editorial board of the Journal.
Declaration of conflicts of interest
The authors have completed the ICMJE declaration of conflicts of interest form, and declare that they have not received funding for the report. They also declare not having financial relationships with organizations that might have interests in the published article in the past three years; and not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.

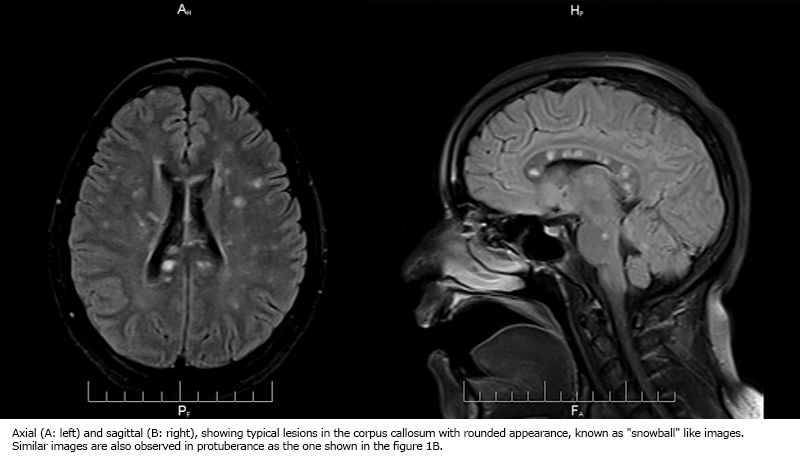 Figure 1. Brain magnetic resonance FLAIR protocol.
Figure 1. Brain magnetic resonance FLAIR protocol.

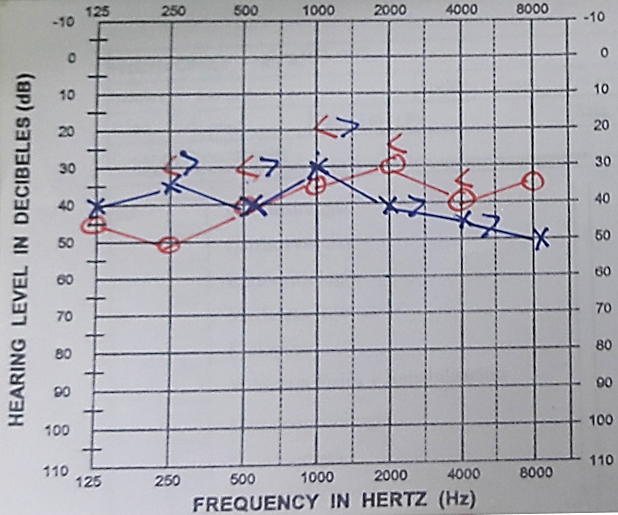 Figure 2. Audiometry showing low and medium tone neurosensory hearing loss.
Figure 2. Audiometry showing low and medium tone neurosensory hearing loss.

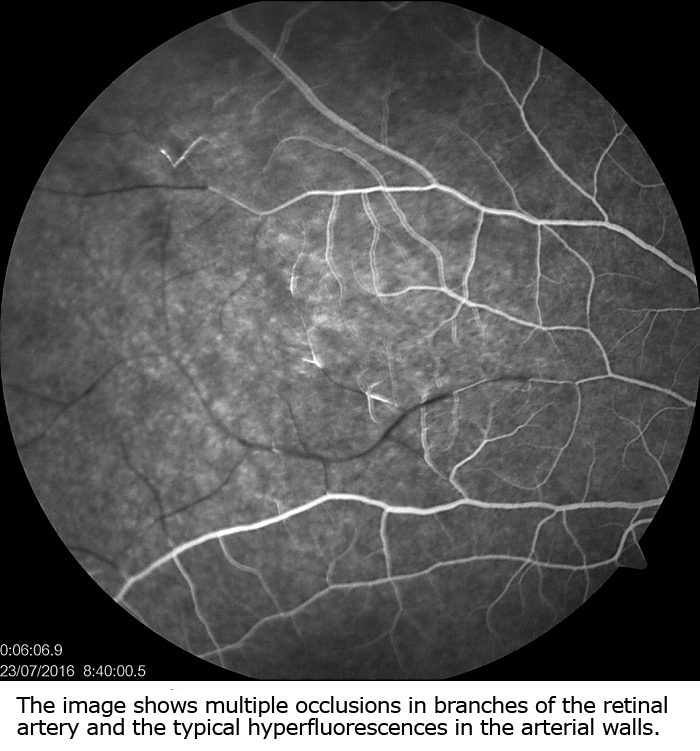 Figura 3. Retinal fluorescein angiography.
Figura 3. Retinal fluorescein angiography.

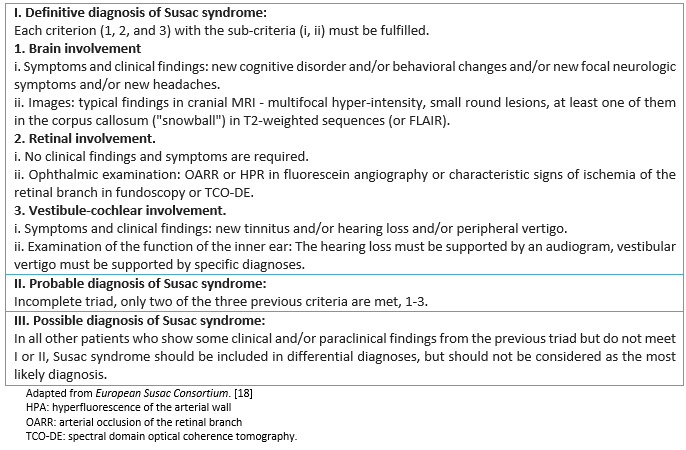 Table 1. Criteria for the diagnosis of Susac syndrome.
Table 1. Criteria for the diagnosis of Susac syndrome.

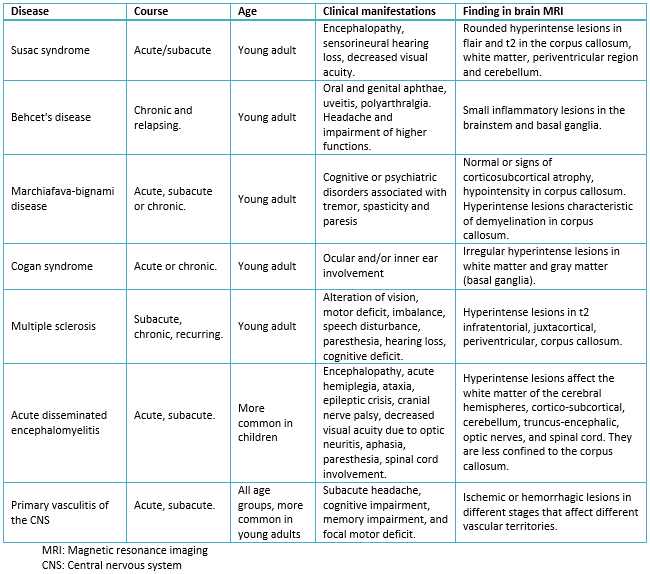 Table 2. Summary table of major differential diagnoses.
Table 2. Summary table of major differential diagnoses.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Susac Syndrome is a rare entity, characterized by a triad of subacute encephalopathy, retinal artery occlusion and sensorineural hearing loss. It is more common in women and the age of onset fluctuates between 9-58 years of age. The pathogenesis is presented as microangiopathic changes at the cerebral, retinal and cochlear levels associated with an autoimmune mechanism. We present the case of a 31-year-old woman who started with a diffuse headache, puerile behavior, bradylalia and somnolence. As the disease progressed, she had auditory deficit and arterial obstruction of the right temporal retinal branch in retinal fluorescein angiography. Brain magnetic resonance showed rounded hyperintense lesions in the corpus callosum, periventricular region and cerebellum. This is the first reported case of Susac Syndrome in Peru, presented with the classic triad, which is an infrequent presentation. However, cases that show incomplete forms should be evaluated in a timely manner to initiate timely treatment and avoid irreversible consequences.
 Autores:
Carolina Rivadeneira-Sotelo[1], María Meza Vega[1,2], Darwin Segura-Chávez[1], Sheila Castro-Suarez[1,3]
Autores:
Carolina Rivadeneira-Sotelo[1], María Meza Vega[1,2], Darwin Segura-Chávez[1], Sheila Castro-Suarez[1,3]

Citación: Rivadeneira-Sotelo C, Meza Vega M, Segura-Chávez D, Castro-Suarez S. Susac syndrome: the first case report in Peru. Medwave 2017 Ago;17(7):e7033 doi: 10.5867/medwave.2017.07.7033
Fecha de envío: 5/6/2017
Fecha de aceptación: 8/8/2017
Fecha de publicación: 30/8/2017
Origen: no solicitado
Tipo de revisión: con revisión por cuatro pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Susac JO, Hardman JM, Selhorst JB. Microangiopathy of the brain and retina. Neurology. 1979 Mar;29(3):313-6. | PubMed |
Susac JO, Hardman JM, Selhorst JB. Microangiopathy of the brain and retina. Neurology. 1979 Mar;29(3):313-6. | PubMed | van Winden M, Salu P. Branch retinal artery occlusion with visual field and multifocal erg in Susac syndrome: a case report. Doc Ophthalmol. 2010 Dec;121(3):223-9. | CrossRef | PubMed |
van Winden M, Salu P. Branch retinal artery occlusion with visual field and multifocal erg in Susac syndrome: a case report. Doc Ophthalmol. 2010 Dec;121(3):223-9. | CrossRef | PubMed | Deane KD, Tyler KN, Johnson DW, Tanabe JL, Oskarrson BE, Nitka EE, et al. Susac syndrome and pregnancy: disease management. J Clin Rheumatol. 2011 Mar;17(2):83-8. | CrossRef | PubMed |
Deane KD, Tyler KN, Johnson DW, Tanabe JL, Oskarrson BE, Nitka EE, et al. Susac syndrome and pregnancy: disease management. J Clin Rheumatol. 2011 Mar;17(2):83-8. | CrossRef | PubMed | Vodopivec I, Prasad S. Short Follow-up Bias Confounds Estimates of the "Typical" Clinical Course of Susac Syndrome. J Neuroophthalmol. 2017 Jun;37(2):149-153. | CrossRef | PubMed |
Vodopivec I, Prasad S. Short Follow-up Bias Confounds Estimates of the "Typical" Clinical Course of Susac Syndrome. J Neuroophthalmol. 2017 Jun;37(2):149-153. | CrossRef | PubMed | Cosacov R, Villarreal G. Síndrome de Susac y revisión de casos argentinos. Neurol Argent. 2016;8:122-5. | CrossRef |
Cosacov R, Villarreal G. Síndrome de Susac y revisión de casos argentinos. Neurol Argent. 2016;8:122-5. | CrossRef | Vodopivec I, Prasad S. Treatment of Susac Syndrome. Curr Treat Options Neurol. 2016 Jan;18(1):3. | CrossRef | PubMed |
Vodopivec I, Prasad S. Treatment of Susac Syndrome. Curr Treat Options Neurol. 2016 Jan;18(1):3. | CrossRef | PubMed | Jarius S, Kleffner I, Dörr JM, Sastre-Garriga J, Illes Z, Eggenberger E, et al. Clinical, paraclinical and serological findings in Susac syndrome: an international multicenter study. J Neuroinflammation. 2014 Mar 8;11:46. | CrossRef | PubMed |
Jarius S, Kleffner I, Dörr JM, Sastre-Garriga J, Illes Z, Eggenberger E, et al. Clinical, paraclinical and serological findings in Susac syndrome: an international multicenter study. J Neuroinflammation. 2014 Mar 8;11:46. | CrossRef | PubMed | Yurtsever B, Çabalar M, Kaya H, Tuğcu B, Yazıcı ZM, Yayla V. A Rare Cause of Hearing Loss: Susac Syndrome. J Int Adv Otol. 2015 Aug;11(2):167-9. | CrossRef | PubMed |
Yurtsever B, Çabalar M, Kaya H, Tuğcu B, Yazıcı ZM, Yayla V. A Rare Cause of Hearing Loss: Susac Syndrome. J Int Adv Otol. 2015 Aug;11(2):167-9. | CrossRef | PubMed | Nazari F, Azimi A, Abdi S. What is Susac syndrome? - A brief review of articles. Iran J Neurol. 2014 Oct 6;13(4):209-14. | PubMed |
Nazari F, Azimi A, Abdi S. What is Susac syndrome? - A brief review of articles. Iran J Neurol. 2014 Oct 6;13(4):209-14. | PubMed | Alper G. Acute disseminated encephalomyelitis. J Child Neurol. 2012 Nov;27(11):1408-25. | CrossRef | PubMed |
Alper G. Acute disseminated encephalomyelitis. J Child Neurol. 2012 Nov;27(11):1408-25. | CrossRef | PubMed | Dutra LA, de Souza AW, Grinberg-Dias G, Barsottini OG, Appenzeller S. Central nervous system vasculitis in adults: An update. Autoimmun Rev. 2017 Feb;16(2):123-131. | CrossRef | PubMed |
Dutra LA, de Souza AW, Grinberg-Dias G, Barsottini OG, Appenzeller S. Central nervous system vasculitis in adults: An update. Autoimmun Rev. 2017 Feb;16(2):123-131. | CrossRef | PubMed | van der Kooij SM, van Buchem MA, Overbeek OM, Dijkman G, Huizinga TW. Susac syndrome: a report of four cases and a review of the literature. Neth J Med. 2015 Jan;73(1):10-6. | PubMed |
van der Kooij SM, van Buchem MA, Overbeek OM, Dijkman G, Huizinga TW. Susac syndrome: a report of four cases and a review of the literature. Neth J Med. 2015 Jan;73(1):10-6. | PubMed | Rennebohm R, Susac JO, Egan RA, Daroff RB. Susac's Syndrome--update. J Neurol Sci. 2010 Dec 15;299(1-2):86-91. | CrossRef | PubMed |
Rennebohm R, Susac JO, Egan RA, Daroff RB. Susac's Syndrome--update. J Neurol Sci. 2010 Dec 15;299(1-2):86-91. | CrossRef | PubMed | Rennebohm RM, Egan RA, Susac JO. Treatment of Susac's Syndrome. Curr Treat Options Neurol. 2008 Jan;10(1):67-74. | PubMed |
Rennebohm RM, Egan RA, Susac JO. Treatment of Susac's Syndrome. Curr Treat Options Neurol. 2008 Jan;10(1):67-74. | PubMed | Dörr J, Krautwald S, Wildemann B, Jarius S, Ringelstein M, Duning T, et al. Characteristics of Susac syndrome: a review of all reported cases. Nat Rev Neurol. 2013 Jun;9(6):307-16. | CrossRef | PubMed |
Dörr J, Krautwald S, Wildemann B, Jarius S, Ringelstein M, Duning T, et al. Characteristics of Susac syndrome: a review of all reported cases. Nat Rev Neurol. 2013 Jun;9(6):307-16. | CrossRef | PubMed | Aubart-Cohen F, Klein I, Alexandra JF, Bodaghi B, Doan S, Fardeau C, et al. Long-term outcome in Susac syndrome. Medicine (Baltimore). 2007 Mar;86(2):93-102. | PubMed |
Aubart-Cohen F, Klein I, Alexandra JF, Bodaghi B, Doan S, Fardeau C, et al. Long-term outcome in Susac syndrome. Medicine (Baltimore). 2007 Mar;86(2):93-102. | PubMed | Kleffner I, Dörr J, Ringelstein M, Gross CC, Böckenfeld Y, Schwindt W, et al. Diagnostic criteria for Susac syndrome. J Neurol Neurosurg Psychiatry. 2016 Dec;87(12):1287-1295. | CrossRef | PubMed |
Kleffner I, Dörr J, Ringelstein M, Gross CC, Böckenfeld Y, Schwindt W, et al. Diagnostic criteria for Susac syndrome. J Neurol Neurosurg Psychiatry. 2016 Dec;87(12):1287-1295. | CrossRef | PubMed | López Bravo A, Parra Soto C, Bellosta Diago E, Cecilio Irazola Á, Santos-Lasaosa S. Neurological manifestations of Behçet's disease: Case report and literature review. Reumatol Clin. 2017 May 22. pii: S1699-258X(17)30100-6. | CrossRef | PubMed |
López Bravo A, Parra Soto C, Bellosta Diago E, Cecilio Irazola Á, Santos-Lasaosa S. Neurological manifestations of Behçet's disease: Case report and literature review. Reumatol Clin. 2017 May 22. pii: S1699-258X(17)30100-6. | CrossRef | PubMed | Rodríguez-Fernández S, Bravo-Doviso J, Ramos-Gómez LA, Martín-Delgado C, Ortiz-López R, Puente-Domínguez T. Enfermedad de Marchiafava-Bignami en Cuidados Intensivos. Med Intensiva. 2005;29(7):396-9. | Link |
Rodríguez-Fernández S, Bravo-Doviso J, Ramos-Gómez LA, Martín-Delgado C, Ortiz-López R, Puente-Domínguez T. Enfermedad de Marchiafava-Bignami en Cuidados Intensivos. Med Intensiva. 2005;29(7):396-9. | Link | Montesa S, Rodríguez-Muguruzab S, Viñac C, Olivé A. Síndrome de Cogan. Semin Fund Esp Reumatol. 2014;15(1):19-24. | CrossRef |
Montesa S, Rodríguez-Muguruzab S, Viñac C, Olivé A. Síndrome de Cogan. Semin Fund Esp Reumatol. 2014;15(1):19-24. | CrossRef | Pawate S, Agarwal A, Moses H, Sriram S. The spectrum of Susac's syndrome. Neurol Sci. 2009 Feb;30(1):59-64. | CrossRef | PubMed |
Pawate S, Agarwal A, Moses H, Sriram S. The spectrum of Susac's syndrome. Neurol Sci. 2009 Feb;30(1):59-64. | CrossRef | PubMed | Petty GW, Engel AG, Younge BR, Duffy J, Yanagihara T, Lucchinetti CF, et al. Retinocochleocerebral vasculopathy. Medicine (Baltimore). 1998 Jan;77(1):12-40. | PubMed |
Petty GW, Engel AG, Younge BR, Duffy J, Yanagihara T, Lucchinetti CF, et al. Retinocochleocerebral vasculopathy. Medicine (Baltimore). 1998 Jan;77(1):12-40. | PubMed | Roessler-Górecka M, Mendel T, Wiśniowska J, Seniów J. Neuropsychological characteristics of encephalopathy in Susac's Syndrome - Case report. Neurol Neurochir Pol. 2017 Mar - Apr;51(2):174-179. | CrossRef | PubMed |
Roessler-Górecka M, Mendel T, Wiśniowska J, Seniów J. Neuropsychological characteristics of encephalopathy in Susac's Syndrome - Case report. Neurol Neurochir Pol. 2017 Mar - Apr;51(2):174-179. | CrossRef | PubMed | Susac JO, Egan RA, Rennebohm RM, Lubow M. Susac's syndrome: 1975-2005 microangiopathy/autoimmune endotheliopathy. J Neurol Sci. 2007 Jun 15;257(1-2):270-2. | PubMed |
Susac JO, Egan RA, Rennebohm RM, Lubow M. Susac's syndrome: 1975-2005 microangiopathy/autoimmune endotheliopathy. J Neurol Sci. 2007 Jun 15;257(1-2):270-2. | PubMed | Robles-Cedeño R, Ramió-Torrentà L, Laguillo G, Gich J, Castellanos M. Long-term clinical and radiological evolution in one case of Susac's syndrome. Neurol Sci. 2012 Dec;33(6):1407-10. | CrossRef | PubMed |
Robles-Cedeño R, Ramió-Torrentà L, Laguillo G, Gich J, Castellanos M. Long-term clinical and radiological evolution in one case of Susac's syndrome. Neurol Sci. 2012 Dec;33(6):1407-10. | CrossRef | PubMed | Ringelstein M, Albrecht P, Kleffner I, Bühn B, Harmel J, Müller AK, et al. Retinal pathology in Susac syndrome detected by spectral-domain optical coherence tomography. Neurology. 2015 Aug 18;85(7):610-8. | CrossRef | PubMed |
Ringelstein M, Albrecht P, Kleffner I, Bühn B, Harmel J, Müller AK, et al. Retinal pathology in Susac syndrome detected by spectral-domain optical coherence tomography. Neurology. 2015 Aug 18;85(7):610-8. | CrossRef | PubMed | Egan RA, Hills WL, Susac JO. Gass plaques and fluorescein leakage in Susac Syndrome. J Neurol Sci. 2010 Dec 15;299(1-2):97-100. | CrossRef | PubMed |
Egan RA, Hills WL, Susac JO. Gass plaques and fluorescein leakage in Susac Syndrome. J Neurol Sci. 2010 Dec 15;299(1-2):97-100. | CrossRef | PubMed | Susac JO. Susac's syndrome: the triad of microangiopathy of the brain and retina with hearing loss in young women. Neurology. 1994 Apr;44(4):591-3. | PubMed |
Susac JO. Susac's syndrome: the triad of microangiopathy of the brain and retina with hearing loss in young women. Neurology. 1994 Apr;44(4):591-3. | PubMed |