 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: Behçet's disease, neurological involvement, vasculitis
Behçet's disease is a vasculitis that can cause inflammatory lesions in multiple organs or systems including the nervous system. Most cases worldwide have been reported along what is called the "Silk Route" from the Mediterranean region to Japan, so it is considered a rare disease in Latin American countries. The frequency of neurological involvement ranges from 5 to 13%. We present the case of a young adult woman with diagnostic criteria for Behçet's disease and manifestations of neurological disease, as well as a review of the literature.
Behçet's disease is a vasculitis that causes inflammatory injuries in multiple organs and systems like the skin, joints, gastrointestinal, renal, cardiopulmonary and/or neurological [1].
The larger number of cases on a global scale, has been informed along the so called “Silk Road” that goes from the Mediterranean region up to Japan. It typically appears in the third decade of life, affecting more men than women (1.4:1) with a higher incidence of serious systemic complications in young men [2]. In countries of America the incidence is much lower thus being catalogued as a rare disease [3]. The reported frequency of neurological injuries, ranges between 5 and 13 % and it has been admitted that these injuries increase mortality and morbidity of patients with Behçet´s disease [4],[5].
The diagnosis is based on the following criteria: repetitive oral ulcers generally painful (with a minimum of three relapses in one year), plus two or more of the following signs or symptoms: recurrent genital ulcers, ocular injuries as hypopyon, uveitis, retinal vasculitis, cutaneous injuries and positive pathergy test according to criteria proposed by the International Study Group in 1990 (Table 1) [6]. Recently, these criteria have been revised for presenting low sensibility and new international criteria have been established for Behçet´s disease by means of a ten-point score where a score over four gives the diagnosis. In this score neurological manifestations and vascular manifestations (arterial, venous thrombosis or phlebitis) are added to the previous criteria. Furthermore, if carried out, a positive pathergy test means an additional point [7] (Table 2).
The purpose of this article is to report a case of neuro-Behçet, to review the reported cases so far in Peru, and to identify their common characteristics.
Table 1. Criteria for the diagnosis of Behçet´s disease.
Table 2. Diagnostic score according to the New International Criteria for the Behçet´s disease.
The design of the present research is a retrospective cross-sectional case report. Informed consent for publication was requested and provided in accordance with international ethical standards. We carried out a search of medical literature regarding reported cases of Neuro-Behçet´s disease in Peru (MeSH: Symptom Complex Triple OR Adamantiades-Behcet Disease OR Behcet Triple Symptom Complex OR Old Silk Route Disease OR Behcet's Syndrome OR Behçet Disease AND Case Report [Publication Type] AND Neurologic Manifestations) in PubMed, Lilacs and Scielo. Six cases were identified in our country [7],[8],[9] with the criteria and the diagnostic score for Behçet´s disease.
The patient is a 20-year-old woman, from the Constitutional Province of the Callao, with European - Mediterranean descent from both parents and precedent painful ulcerative injuries in lingual mucous membranes, hard palate and lips during the previous three years with a progressive course and spontaneous remission. One year earlier she had an episode of blurry vision, during three or four days, which improved without treatment. Seven months earlier, an episode of previous uveitis in the right eye with spontaneous remission after two days. The following month she had a relapse in the left eye with the same characteristics (Figure 1). Four months earlier, she presented intermittent arthralgia of 8/10 intensity that diminished with analgesic and anti-inflammatory treatment. Two months earlier, the patient showed positional tremor in upper limbs with a duration of three days and spontaneous remission. One month earlier, she presented genital ulcers with spontaneous remission in two weeks without leaving a scar and with recurrence until diagnosis. During this time she refers constipation, which improves with lactulose.
Some weeks before, she went to the emergency department after a sudden vertical diplopia that was not spontaneously improving.
In the physical examination at admission: the patient had a fluent speech, anisocoria (R: 2.5 cm L: 3.5 cm), making it difficult to look down with the left eye, vertical nystagmus, central scotoma and upper eyelid ptosis in the right eye. The ocular fundus showed vitreitis, macular edema and foci of peripheral periphlebitis with right predominance. She also presented painful genital and perianal ulcers of slightly definite borders with a diameter of one to two centimeters (Figure 1).
Figure 1. Clinical signs of the patient.
Antiphospholipid antibodies, antinuclear antibodies, antineutrophil cytoplasm autoantibodies, rheumatoid factor, serum complement, and oligoclonal bands turned out negative (Table 3). Due to the mild protein C and S increase and low sedimentation rate, post infectious encephalopathy and/or rhombencephalitis was suspected. However, we found no indicators of any etiologic agent in the study of cerebrospinal fluid (Table 4).
Table 4. Cerebrospinal fluid characteristics.
The results of nuclear magnetic resonance (NMR) show hyperintense images in T2-FLAIR in medial region bilateral mesencephalic ranging left area and right hippocampus (figure 2). Visual evoked potentials demonstrated bilateral increased latencies with left predominance.
Figure 2. Images of RMN in considered T2-FLAIR.
We determined that the clinical picture corresponds to an inflammatory disease without infection evidence. The extra neurological symptoms and signs and the characteristic injuries of the central nervous system allowed to exclude other causes of inflammatory injuries as of lupus erythematosus, rheumatoid arthritis, herpes, HIV, syphilis, multiple sclerosis, post-infectious encephalopathy and viral rhombencephalitis.
The oral and genital ulcers with undefined etiology made us suspect Behçet´s disease, hence we requested the pathergy test [7] (Figure 3), which turned out to be negative. Nevertheless, in the biopsy sample of the rim of the ulcer, acute and chronic, superficial and deep inflammatory perivascular and interstitial infiltration were demonstrated, compatible with autoimmune disease (Figure 4).
Figure 4. Histological images of skin biopsies showing acute and chronic inflammatory infiltration.
Additionally, the hemogram presented leukocytosis (14,440 cells/mm3) with lymphocytes predominance. Hemoglobin in 9.1 g/dl with transferrin saturation of 7.75 %, ferritin 57 ng/ml and iron of 17.49 mcg/dl. The urine test with leukocytes over 100 per field, positive to Candida Albicans culture as the vaginal secretion test (Table 5).
Table 5. Hematology test and others.
After treating the infections and stabilizing the patient, treatment began with prednisone with a systemic dose of 0.5 mg to 1mg/kg/day that has continued up to today. She has also received treatment for two months with azathioprine with a dose between 1 to 2 mg/kg/day, during which, the patient presented meningoencephalitis of probable bacterial etiology, so we decided to withdraw this treatment. The patient later presents an evolution characterized by recurrent urinal infections, Cushing syndrome, osteopenia and osteoporosis as adverse reactions to the treatment with corticoids. As a consequence, she also present a decrease of visual acuity with right predominance.
Diagnosis according to criteria
The clinical picture of the patient met the major criterion (recurrent oral ulcers) and two of four additional criteria established by the International Study Group in 1990 (genital ulcers and previous uveitis as an ocular injury) [1] (Table 1). The patient also met the new international criteria, established in 2014, for Behçet´s disease, having presented eight of a maximum score of ten. These criteria add to the classic ones: skin injuries (aphthae) and neurological manifestations without vascular manifestations like arterial thrombosis or phlebitis [7] (Table 2).
Identified cases
The reports of Behçet´s disease in Peru are scarce. After the search, we could only identify six cases of Neuro - Behçet in the last 25 years which are described in Table 6.
The neurological compromise of Behçet´s disease can be classified as primary by direct affectation of the central or peripheral nervous system; and secondary to systemic complications of the disease or the treatment. Two primary affectations have been established: parenchymal and not parenchymal. Which rarely take place in the same individual [2], and its pathogenesis are probably different, although the most recognized finding is the perivascular lymphocytic infiltrate [10].
The parenchymal damage is characterized by an inflammation of small blood vessels in the parenchyma of the central nervous system. It affects most frequently male patients. Symptoms as ophthalmoparesis, cranial neuropathy, cerebellar damage or pyramidal dysfunction, can indicate affectation of the brain stem. Progressive forms of the disease characterized by subcortical dementia accompanied by ataxia; in addition to signs and symptoms indicative of cerebral hemispheres damage as hemiparesis, convulsion, dysphasia, cognitive dysfunction, psychosis and emotional lability have also been reported. Finally, the disease can also affect the spinal cord [10],[11].
The diagnosis of the Behçet´s disease rarely occurs in our population and it is usually not reported initially in patients with neurological compromise. Although there are reports of Behçet´s disease in Mongolia, Russia, Australia, New Zealand, Brazil, Mexico, Cuba, Argentina, Colombia and Chile, approximately in 200 patients [12], the reports of the Neuro-Behçet´s disease in Peru are scarce. Six cases were identified in the last 25 years, mostly with neurological symptomatology different from that of our patient, with the same proportion of men and women and ages ranging between 16 and 55 years, from urban areas of Lima, but with no specified European or Mediterranean descent (Table 6).
Our patient presented perianal and genital ulcers which are considered to be the most specific injuries of this disease [13]. She also presented uveitis that is seen in 25 to 75 % of patients mostly men. The patient also had a partial paralysis of III right cranial nerve (only eyelid ptosis) and left (pupil dilation), damage of the IV cranial nerve nucleus of the right side (slight medial deviation of the left eye with difficulty for directing the look down and lateral). This is similar to the case reported by Aydin et al. but this case only presented injury in the oculomotor nerve nucleus [14]. Hence, ocular signs can be the initial manifestations that generate main concern in the patient and/or doctor and lead the clinical suspicion to the definitive diagnosis even in absence of other more common clinical symptoms [15]. Despite that our patient fulfills the established diagnostic criteria for Behçet´s disease [1],[7] it presented a negative test of pathergy, which is specific but has low sensitivity, a fact that might increase the value of false negatives in the context of patients receiving any form of anti-inflammatory treatment [6],[7].
Neurological clinical manifestations in our patient appeared with a progressive course of approximately four years, similar period to that of published studies in Asia and Europe [12]. The neurological compromise of the present case was of parenchymal type; as in three published articles in Peru, with a total of six patients diagnosed with neuro-Behçet (Table 6). She did not show severe episodes at diagnosis and received opportune treatment; in contrast with the reported Peruvian case reported Hinostroza et al. [9], in which the diagnosis was late and neurological complications led the patient to deep coma. The neurological clinical manifestations of our patient were different from the reported cases by Barrios et al. [10], which included tonic-clonic convulsions, movement alterations, hemiparesis, Babinski (+) and migraine. Therefore, it is important to consider the neurological symptomatology of Behçet´s disease, especially in its varied clinical presentation, because the injuries might be irreversible and linked with a bad prognosis [16].
The treatment of the Behçet´s disease is based on the use of glucocorticoids in doses that change according to the severity of the presentation, generally, it starts with prednisone (1 mg/kg per day for one month, followed by withdrawal in a gradual form depending of the patient´s tolerance). In serious cases it is useful a treatment with corticoids pulses, as methylprednisolone 1 g, administered intravenously every 24 hours during one to five days [17]. In case of nervous compromise the treatment includes the use of azathioprine as a first line agent, alternatives include mycophenolate, methotrexate, and cyclophosphamide [18]. When there is an ocular compromise, the use of cyclosporine in combination with glucocorticoids is frequent [19] and in serious or resistant cases other immunosuppressants are used as azathioprine [20].
In our patient, the treatment was with corticoids and azathioprine, the result was a recovery of the neurological injuries without relapsing, but with recurrent urinary tract infections and development of Cushing syndrome as side effects of the corticoids. This favorable evolution is not seen in all patients, as it is in the Peruvian case presented by Visaga et al. [8], in which there was a late diagnosis and failure at the end of the treatment with corticoids. The absence of an answer to corticoids is associated with a bad prognosis and with a dependence status [21].
The most complex complication is the blindness caused by bilateral uveitis and scar tissue. Here the traditional use cyclosporine (5mg/kg) is indicated together with the treatment against the tumor necrosis factor alpha when resistance to immunosuppressants is identified [22]. Our patient presented a diagnosis of uveitis in the right eye seven months before diagnosis, a month after she had a recurrence in the left eye and this is the last reported episode.
In conclusion, in patients with neurological symptomatology and injuries, it is necessary to suspect the diagnosis of less frequent etiologies like Behçet´s disease, especially in young people even in populations where this diagnosis is not frequent. It is necessary to consider that the morbimortality of this disease increases when there is neurological damage [23]. Therefore, an early diagnosis is important since it allows an opportune treatment that avoids the development of severe complications and/or disabling sequelae.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The informed consent requested by Medwave has been signed by the patient; A copy of this was sent to the editorial board of the magazine.
Declaration of conflicts of interest
The authors have completed the ICMJE declaration of conflicts of interest form, and declare that they have not received funding for the report; Not having financial relationships with organizations that may have interests in the published article in the past three years; And not having other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Financing
The authors state that there were no external sources of funding.

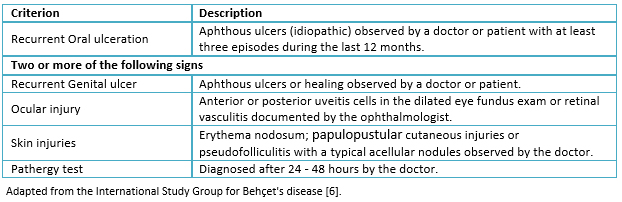 Table 1. Criteria for the diagnosis of Behçet´s disease.
Table 1. Criteria for the diagnosis of Behçet´s disease.

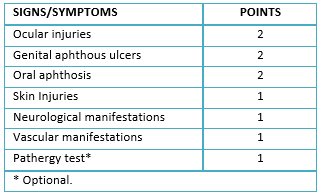 Table 2. Diagnostic score according to the New International Criteria for the Behçet´s disease.
Table 2. Diagnostic score according to the New International Criteria for the Behçet´s disease.

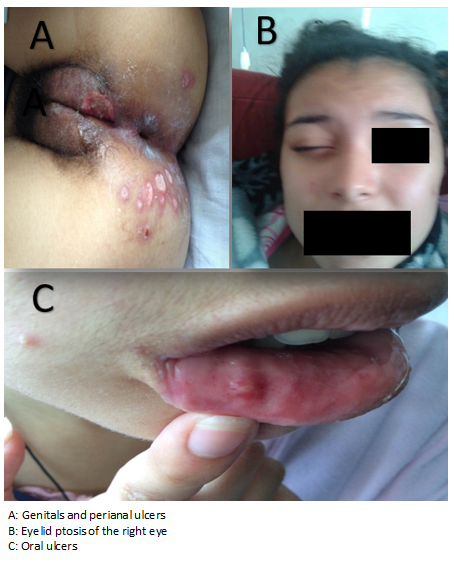 Figure 1. Clinical signs of the patient.
Figure 1. Clinical signs of the patient.

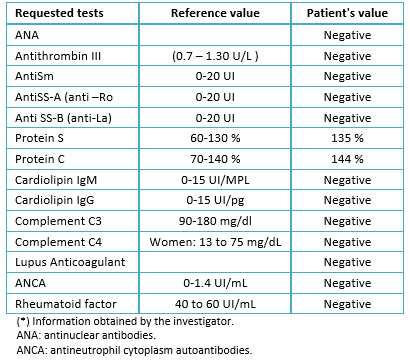 Table 3. Immune profiling.
Table 3. Immune profiling.

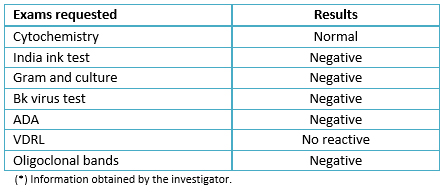 Table 4. Cerebrospinal fluid characteristics.
Table 4. Cerebrospinal fluid characteristics.

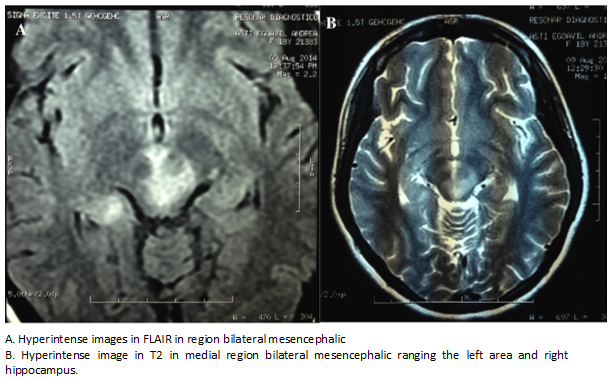 Figure 2. Images of RMN in considered T2-FLAIR.
Figure 2. Images of RMN in considered T2-FLAIR.

 Figure 3. Pathergy test.
Figure 3. Pathergy test.

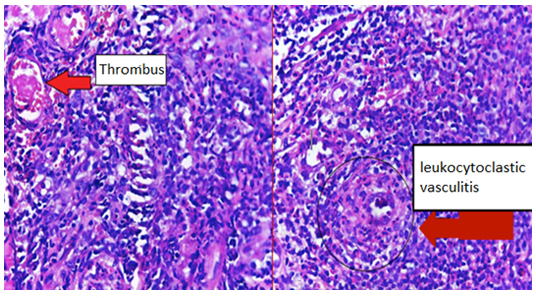 Figure 4. Histological images of skin biopsies showing acute and chronic inflammatory infiltration.
Figure 4. Histological images of skin biopsies showing acute and chronic inflammatory infiltration.

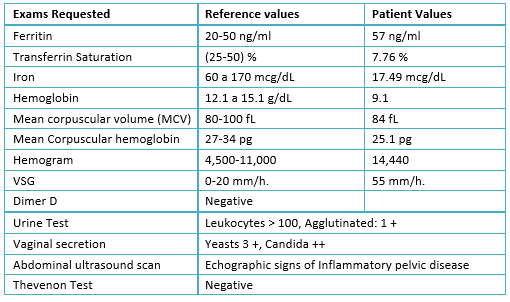 Table 5. Hematology test and others.
Table 5. Hematology test and others.

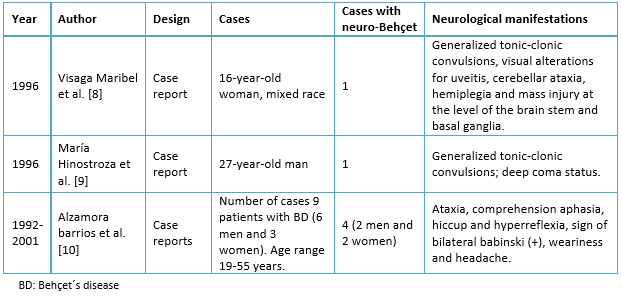 Table 6. Evidence table.
Table 6. Evidence table.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Behçet's disease is a vasculitis that can cause inflammatory lesions in multiple organs or systems including the nervous system. Most cases worldwide have been reported along what is called the "Silk Route" from the Mediterranean region to Japan, so it is considered a rare disease in Latin American countries. The frequency of neurological involvement ranges from 5 to 13%. We present the case of a young adult woman with diagnostic criteria for Behçet's disease and manifestations of neurological disease, as well as a review of the literature.
 Autores:
Roberto A. Molina[1,2,3], Andrely Huerta-Rosario[1,2,3], Carlos Alexander Alva Díaz[3,4,5], Koni Katerin Mejía Rojas[4,5], Nicanor Mori[4], Roberto Romero Sánchez[4,5]
Autores:
Roberto A. Molina[1,2,3], Andrely Huerta-Rosario[1,2,3], Carlos Alexander Alva Díaz[3,4,5], Koni Katerin Mejía Rojas[4,5], Nicanor Mori[4], Roberto Romero Sánchez[4,5]

Citación: Molina RA, Huerta-Rosario A, Alva Díaz CA, Mejía Rojas KK, Mori N, Romero Sánchez R. Neuro-Behçet's disease in Peru: a case report and literature review. Medwave 2017 Jun;17(5):e6978 doi: 10.5867/medwave.2017.05.6978
Fecha de envío: 2/2/2017
Fecha de aceptación: 3/6/2017
Fecha de publicación: 20/6/2017
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Ideguchi H, Suda A, Takeno M, Ueda A, Ohno S, Ishigatsubo Y. Behçet disease: evolution of clinical manifestations. Medicine (Baltimore). 2011 Mar;90(2):125-32. | CrossRef | PubMed |
Ideguchi H, Suda A, Takeno M, Ueda A, Ohno S, Ishigatsubo Y. Behçet disease: evolution of clinical manifestations. Medicine (Baltimore). 2011 Mar;90(2):125-32. | CrossRef | PubMed | Savey L, Resche-Rigon M, Wechsler B, Comarmond C, Piette JC, Cacoub P, et al. Ethnicity and association with disease manifestations and mortality in Behçet's disease. Orphanet J Rare Dis. 2014 Mar 27;9:42. | CrossRef | PubMed |
Savey L, Resche-Rigon M, Wechsler B, Comarmond C, Piette JC, Cacoub P, et al. Ethnicity and association with disease manifestations and mortality in Behçet's disease. Orphanet J Rare Dis. 2014 Mar 27;9:42. | CrossRef | PubMed | Castillo-González W, González--Argote J, Hernández-Estévez J. Enfermedad de Behçet. Revista Cubana de Reumatología. 2014;16(3):12. | Link |
Castillo-González W, González--Argote J, Hernández-Estévez J. Enfermedad de Behçet. Revista Cubana de Reumatología. 2014;16(3):12. | Link | Yoon DL, Kim YJ, Koo BS, Kim YG, Lee CK, Yoo B. Neuro-behçet's disease in South Korea: clinical characteristics and treatment response. Int J Rheum Dis. 2014 May;17(4):453-8. | CrossRef | PubMed |
Yoon DL, Kim YJ, Koo BS, Kim YG, Lee CK, Yoo B. Neuro-behçet's disease in South Korea: clinical characteristics and treatment response. Int J Rheum Dis. 2014 May;17(4):453-8. | CrossRef | PubMed | Zouboulis CC, Vaiopoulos G, Marcomichelakis N, Palimeris G, Markidou I, Thouas B, et al. Onset signs, clinical course, prognosis, treatment and outcome of adult patients with Adamantiades-Behçet's disease in Greece. Clin Exp Rheumatol. 2003 Jul-Aug;21(4 Suppl 30):S19-26. | PubMed |
Zouboulis CC, Vaiopoulos G, Marcomichelakis N, Palimeris G, Markidou I, Thouas B, et al. Onset signs, clinical course, prognosis, treatment and outcome of adult patients with Adamantiades-Behçet's disease in Greece. Clin Exp Rheumatol. 2003 Jul-Aug;21(4 Suppl 30):S19-26. | PubMed | Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990 May 5;335(8697):1078-80. | PubMed |
Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990 May 5;335(8697):1078-80. | PubMed | International Team for the Revision of the International Criteria for Behçet's Disease (ITR-ICBD). The International Criteria for Behçet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014 Mar;28(3):338-47. | CrossRef | PubMed |
International Team for the Revision of the International Criteria for Behçet's Disease (ITR-ICBD). The International Criteria for Behçet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014 Mar;28(3):338-47. | CrossRef | PubMed | Visaga M, Campos P, Bancalari E, Romero F, Hernandez H, Berrocal A, Trelles L, Calvo Armando, et al. Neurobehcet pediátrico. Presentación de un caso y revisión de la literatura. Rev Med Hered. 1996;7:178-181. | Link |
Visaga M, Campos P, Bancalari E, Romero F, Hernandez H, Berrocal A, Trelles L, Calvo Armando, et al. Neurobehcet pediátrico. Presentación de un caso y revisión de la literatura. Rev Med Hered. 1996;7:178-181. | Link | Alzamora B, Martínez F. Enfermedad de Behcet: estudio clínico y tratamiento en el Hospital Arzobispo Loayza. Rev Med Hered. 2001;12(2): 58-64. | Link |
Alzamora B, Martínez F. Enfermedad de Behcet: estudio clínico y tratamiento en el Hospital Arzobispo Loayza. Rev Med Hered. 2001;12(2): 58-64. | Link | International Team for the Revision of the International Criteria for Behçet's Disease (ITR-ICBD). The International Criteria for Behçet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014 Mar;28(3):338-47. | CrossRef | PubMed |
International Team for the Revision of the International Criteria for Behçet's Disease (ITR-ICBD). The International Criteria for Behçet's Disease (ICBD): a collaborative study of 27 countries on the sensitivity and specificity of the new criteria. J Eur Acad Dermatol Venereol. 2014 Mar;28(3):338-47. | CrossRef | PubMed | Cho SB, Cho S, Bang D. New insights in the clinical understanding of Behçet's disease. Yonsei Med J. 2012 Jan;53(1):35-42. | CrossRef | PubMed |
Cho SB, Cho S, Bang D. New insights in the clinical understanding of Behçet's disease. Yonsei Med J. 2012 Jan;53(1):35-42. | CrossRef | PubMed | Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu CS, et al. Diagnosis and management of Neuro-Behçet's disease: international consensus recommendations. J Neurol. 2014 Sep;261(9):1662-76. | CrossRef | PubMed |
Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu CS, et al. Diagnosis and management of Neuro-Behçet's disease: international consensus recommendations. J Neurol. 2014 Sep;261(9):1662-76. | CrossRef | PubMed | Aydin MD, Aydin N. A neuro-Behcet's lesion in oculomotor nerve nucleus. Acta Neurol Scand. 2003 Aug;108(2):139-41. | PubMed |
Aydin MD, Aydin N. A neuro-Behcet's lesion in oculomotor nerve nucleus. Acta Neurol Scand. 2003 Aug;108(2):139-41. | PubMed | Tugal-Tutkun I, Onal S, Ozyazgan Y, Soylu M, Akman M. Validity and agreement of uveitis experts in interpretation of ocular photographs for diagnosis of Behçet uveitis. Ocul Immunol Inflamm. 2014 Dec;22(6):461-8. | CrossRef | PubMed |
Tugal-Tutkun I, Onal S, Ozyazgan Y, Soylu M, Akman M. Validity and agreement of uveitis experts in interpretation of ocular photographs for diagnosis of Behçet uveitis. Ocul Immunol Inflamm. 2014 Dec;22(6):461-8. | CrossRef | PubMed | Siva A, Saip S. The spectrum of nervous system involvement in Behçet's syndrome and its differential diagnosis. J Neurol. 2009 Apr;256(4):513-29. | CrossRef | PubMed |
Siva A, Saip S. The spectrum of nervous system involvement in Behçet's syndrome and its differential diagnosis. J Neurol. 2009 Apr;256(4):513-29. | CrossRef | PubMed | Mat C, Yurdakul S, Uysal S, Gogus F, Ozyazgan Y, Uysal O, et al. A double-blind trial of depot corticosteroids in Behçet's syndrome. Rheumatology (Oxford). 2006 Mar;45(3):348-52. | PubMed |
Mat C, Yurdakul S, Uysal S, Gogus F, Ozyazgan Y, Uysal O, et al. A double-blind trial of depot corticosteroids in Behçet's syndrome. Rheumatology (Oxford). 2006 Mar;45(3):348-52. | PubMed | Saadoun D, Wechsler B, Terrada C, Hajage D, Le Thi Huong D, Resche-Rigon M, et al. Azathioprine in severe uveitis of Behçet's disease. Arthritis Care Res (Hoboken). 2010 Dec;62(12):1733-8. | CrossRef | PubMed |
Saadoun D, Wechsler B, Terrada C, Hajage D, Le Thi Huong D, Resche-Rigon M, et al. Azathioprine in severe uveitis of Behçet's disease. Arthritis Care Res (Hoboken). 2010 Dec;62(12):1733-8. | CrossRef | PubMed | Whitcup SM, Salvo EC Jr, Nussenblatt RB. Combined cyclosporine and corticosteroid therapy for sight-threatening uveitis in Behçet's disease. Am J Ophthalmol. 1994 Jul 15;118(1):39-45. | PubMed |
Whitcup SM, Salvo EC Jr, Nussenblatt RB. Combined cyclosporine and corticosteroid therapy for sight-threatening uveitis in Behçet's disease. Am J Ophthalmol. 1994 Jul 15;118(1):39-45. | PubMed | Kaklamani VG, Kaklamanis PG. Treatment of Behçet's disease--an update. Semin Arthritis Rheum. 2001 Apr;30(5):299-312. Erratum in: Semin Arthritis Rheum 2001 Aug;31(1):69. | PubMed |
Kaklamani VG, Kaklamanis PG. Treatment of Behçet's disease--an update. Semin Arthritis Rheum. 2001 Apr;30(5):299-312. Erratum in: Semin Arthritis Rheum 2001 Aug;31(1):69. | PubMed | Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu CS, et al. Diagnosis and management of Neuro-Behçet's disease: international consensus recommendations. J Neurol. 2014 Sep;261(9):1662-76. | CrossRef | PubMed |
Kalra S, Silman A, Akman-Demir G, Bohlega S, Borhani-Haghighi A, Constantinescu CS, et al. Diagnosis and management of Neuro-Behçet's disease: international consensus recommendations. J Neurol. 2014 Sep;261(9):1662-76. | CrossRef | PubMed |