 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: anophthalmia, congenital heart disease, cor triatriatum, pulmonary hypertension, children
Clinical congenital anophthalmia is described as the uni- or bilateral absence of the eyeball that might occur in isolation or as part of a syndrome. It has a very low prevalence and its etiology is heterogeneous. Complex congenital cardiac malformations are also rare. The association of congenital anophthalmia and congenital heart disease is rarer still, and the etiology of those associations is not well understood yet. We report the case of a patient who had the very rare association of bilateral anophthalmia, multiple cardiac malformations and severe pulmonary hypertension.
Congenital clinical anophthalmia is described as the uni- or bilateral absence of the eyeball that can occur in isolation or as part of a syndrome. The prevalence of anophthalmia and microphthalmia is 3 and 14 per 100,000 births, respectively, while the combined prevalence might reach up to 30 cases per 100,000 births [1],[2],[3], and its etiology is heterogeneous. Although anophthalmia is clinically recognized, the biopsy can reveal residual ectoderm and, depending on the result, it can be classified as true anophthalmia, clinical anophthalmia or extreme microphthalmia. Some congenital heart diseases have a low prevalence and to see them together in a patient is very infrequent. The association of congenital malformations such as anophthalmia and complex heart disease has been rarely reported [1],[4],[5],[6],[7]. The etiology of such associations has not yet been fully elucidated. This is a case report of a patient who had the rare association of bilateral anophthalmia, multiple cardiac malformations and severe pulmonary arterial hypertension.
As policy of the research ethics committee of the hospital, the following report has informed consent signed by parents to submit and/or publish the data within the scientific context without showing the identity of the patient.
An 8-day-old female newborn delivered by normal spontaneous vaginal delivery after a full term pregnancy in a rural hospital was transferred and admitted in the Neonatal Intensive Care Unit. Her weight was 3.6 kg (p60), length 51 cm (p66), head circumference 35 cm (p66). The mother had a normal antenatal period and she reported no exposure to infections, alcohol, drugs or tobacco during pregnancy. Apgar scores were 5 and 7 at one and five minutes, respectively. The patient was the second born child of consanguineous parents (first cousins). The mother had a history of one miscarriage and a first female newborn that died minutes after the birth without a known cause.
On physical examination, the patient was hypoactive with a weak cry and in respiratory distress. The patient had dysmorphic facial features characterized by a narrow forehead, hypotelorism, small palpebral fissures, bilateral anophthalmia, depressed nasal bridge, anteverted nares and low seat ears. Other notable exam findings included right hand with preaxial polydactyly (bifid thumb), hirsutism and normal female external genitalia. Upon auscultation, a grade 4/6 systolic murmur was heard on the left superior sternal border. Patient had normal breath sounds with pulse oximetry of 85% despite supplemental oxygen by hood. After admission, patient had worsening respiratory distress that required assisted ventilation in synchronized intermittent mandatory ventilation mode.
Chest radiograph was done and read as moderate cardiomegaly and pulmonary infiltrates probably related to congenital pneumonia (Figure 1A). It did not show any vertebral malformation. Abdominal ultrasound showed polysplenia and renal ultrasound was normal. Neonatal metabolic screening (hypothyroidism, congenital adrenal hyperplasia, phenylketonuria, galactosemia) and STORCH (syphilis, toxoplasmosis, rubella, cytomegalovirus and herpesvirus) were negative. Karyotype was 46xx.
Head computed tomography scan did not show any cerebral abnormality. Computed tomography of the eyes and orbits was read as absence of eyeballs and presence of cystic remnants, threadlike optic nerve, hypoplasia of extrinsic ocular muscles and cryptophthalmos (Figures 1B and 1C). Electroencephalogram showed disorganized sleep pattern without epileptiform activity.
Transthoracic echocardiography was read as situs solitus, cor triatriatum sinister (left atrium divided by a septum into an anterior and a posterior chamber) with moderate gradient across the membrane, atrial septal defect caudal to the membrane, hemitruncus arteriosus and signs of moderate pulmonary hypertension (Figure 2).
Computed tomography angiography showed cor triatriatum sinister, a 4-milimeter atrial septal defect, partial anomalous pulmonary venous connection (cardiac and supracardiac), large patent ductus arteriosus, and left pulmonary artery originating from the ascending aorta (hemitruncus arteriosus). The origin of the left coronary artery was difficult to visualize (Figure 3).
Figure 3. Thoracic computed tomography.
Cardiac catheterization confirmed the large patent ductus arteriosus, cor triatriatum sinister and atrial septal defect. It also showed a Mori type II aortopulmonary window, and a partial anomalous pulmonary venous connection: left pulmonary veins were seen draining into the innominate vein by way of the vertical vein, while the right pulmonary veins were seen draining into the proximal chamber of the left atrium. Also noted were a juxta-ductal aortic coarctation, anomalous origin of the left coronary artery from the pulmonary trunk (ALCAPA or Bland-White-Garland Syndrome) (Figure 4), hypoplasia of the pulmonary arteries with Nakata index 110 mm2/m2 (normal value: 330 +/- 30 mm2/m2) [8] and severe pulmonary hypertension with negative vasoreactivity testing.
Figure 4. Cardiac catheterization.
At six months of age, tracheostomy and G-tube placement were done. Patient was transferred to the Pediatric Intensive Care Unit. During hospitalization, patient received various antibiotic treatments for recurrent pneumonias, most likely related to prolonged ventilation.
The patient did not have surgery because of the complexity of the congenital heart disease. Although the hospital arranged all the necessary paperwork to transfer the patient to a cardiology center, it was unsuccessful. Patient died after a cardiac arrest at seven months of age. Parents did not give authorization for an autopsy.
Anophthalmia can appear as an isolated physical feature but it may also be part of a variety of syndromes such as: Lenz, Fraser, Matthew-Wood syndrome (Spear syndrome or PDAC: pulmonary hypoplasia/agenesis, diaphragmatic hernia/eventration, anophthalmia/microphthalmia and cardiac defect), oculofaciocardiodental syndrome, anophthalmia-esophageal-genital syndrome and CHARGE (coloboma, heart defect, atresia choanae, retarded growth and development, genital abnormality, and ear abnormality) syndrome. These syndromes can be caused by genetic disorders that can be inherited in a dominant fashion (SOX2 mutations) or in a recessive fashion (CHX10 mutations). Anophthalmia may also be associated with infections during pregnancy, such as with cytomegalovirus infection [2],[3],[9],[10]. The association between anophthalmia, congenital heart disease and pulmonary hypertension is very rare and its etiology is not yet fully understood.
As in other countries of the region, the lack of technological resources makes diagnostic work-up in cases like these difficult and genetic counseling challenging. In this particular case, the history of consanguinity and previous miscarriage were highly suggestive of an inherited disease, making it likely for this couple to have a new descendant with similar features in the future.
Even with the diagnosis of pulmonary hypertension, vasodilators were not prescribed to this patient. There was a high risk of causing coronary steal if the pulmonary vascular resistances were diminished. Risk of provoking acute heart failure outweighed the benefits of administering the medication.
The spectrum of anophthalmia and congenital heart defects is wide and diverse. There are some established syndromes in which these phenotypes are associated. However, the congenital heart defects described in this patient have been previously reported only as separate entities and not as a part of a syndrome such as the one being described in this case report. The present case report adheres to the CARE guidelines for clinical case reports [11].
From the editor
The authors originally submitted this article in Spanish and English. The Journal has not copyedited the English version.
Ethical aspects
The father of the patient signed the informed consent requested by Medwave. A copy was sent to the Journal editorial board.
Conflicts of interest
The authors completed the ICMJE conflict of interest declaration form, translated to Spanish by Medwave, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare that there was no funding coming from external sources.

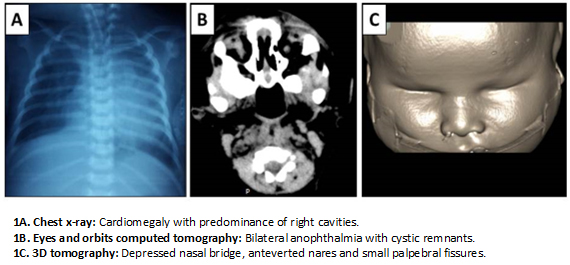 Figure 1. Imaging results.
Figure 1. Imaging results.

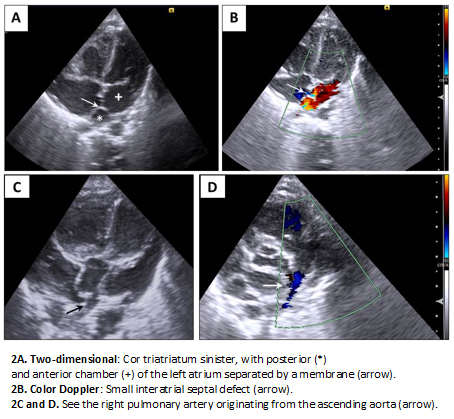 Figure 2. Echocardiography.
Figure 2. Echocardiography.

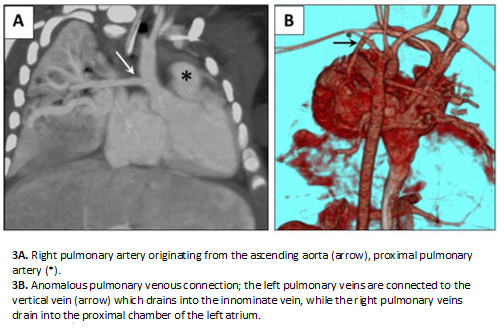 Figure 3. Thoracic computed tomography.
Figure 3. Thoracic computed tomography.

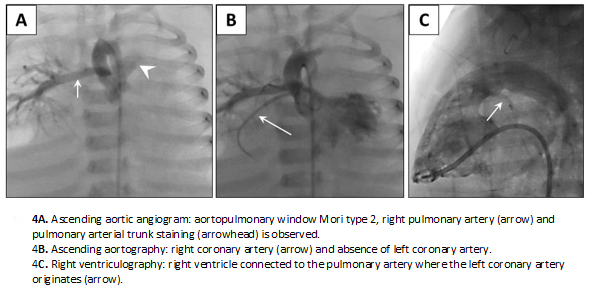 Figure 4. Cardiac catheterization.
Figure 4. Cardiac catheterization.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Clinical congenital anophthalmia is described as the uni- or bilateral absence of the eyeball that might occur in isolation or as part of a syndrome. It has a very low prevalence and its etiology is heterogeneous. Complex congenital cardiac malformations are also rare. The association of congenital anophthalmia and congenital heart disease is rarer still, and the etiology of those associations is not well understood yet. We report the case of a patient who had the very rare association of bilateral anophthalmia, multiple cardiac malformations and severe pulmonary hypertension.
 Autores:
Raúl Enrique Ríos-Méndez[1], Michell Marola Lozano Chinga[1]
Autores:
Raúl Enrique Ríos-Méndez[1], Michell Marola Lozano Chinga[1]

Citación: Ríos-Méndez RE, Lozano Chinga MM. Rare association of anophthalmia, complex congenital heart disease and pulmonary hypertension: case report. Medwave 2016 Oct;16(9):e6568 doi: 10.5867/medwave.2016.09.6568
Fecha de envío: 18/6/2016
Fecha de aceptación: 7/9/2016
Fecha de publicación: 7/10/2016
Origen: no solicitado
Tipo de revisión: con revisión por dos pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Morrison D, FitzPatrick D, Hanson I, Williamson K, van Heyningen V, Fleck B, et al. National study of microphthalmia, anophthalmia, and coloboma (MAC) in Scotland: investigation of genetic aetiology. J Med Genet. 2002 Jan;39(1):16-22. | PubMed |
Morrison D, FitzPatrick D, Hanson I, Williamson K, van Heyningen V, Fleck B, et al. National study of microphthalmia, anophthalmia, and coloboma (MAC) in Scotland: investigation of genetic aetiology. J Med Genet. 2002 Jan;39(1):16-22. | PubMed | Verma AS, Fitzpatrick DR. Anophthalmia and microphthalmia. Orphanet J Rare Dis. 2007 Nov 26;2:47. | PubMed |
Verma AS, Fitzpatrick DR. Anophthalmia and microphthalmia. Orphanet J Rare Dis. 2007 Nov 26;2:47. | PubMed | Bermejo Sánchez E, Ayala Garcés A, Félix Rodríguez V, Martín Bermejo M, Blanco García M, Egüés Jimeno J, et al. [Anophthalmia/micro-ophthalmia in syndromes: epidemiology study of newborns in Spain]. An Esp Pediatr. 1996 Sep;45(3):269-75. | PubMed |
Bermejo Sánchez E, Ayala Garcés A, Félix Rodríguez V, Martín Bermejo M, Blanco García M, Egüés Jimeno J, et al. [Anophthalmia/micro-ophthalmia in syndromes: epidemiology study of newborns in Spain]. An Esp Pediatr. 1996 Sep;45(3):269-75. | PubMed | Wang J, Steelman CK, Vincent R, Richburg D, Chang TS, Shehata BM. Two case reports of anophthalmia and congenital heart disease: Adding a new dimension to this association. Fetal Pediatr Pathol. 2010;29(5):291-8. | CrossRef | PubMed |
Wang J, Steelman CK, Vincent R, Richburg D, Chang TS, Shehata BM. Two case reports of anophthalmia and congenital heart disease: Adding a new dimension to this association. Fetal Pediatr Pathol. 2010;29(5):291-8. | CrossRef | PubMed | Pasutto F, Sticht H, Hammersen G, Gillessen-Kaesbach G, Fitzpatrick DR, Nürnberg G, et al. Mutations in STRA6 cause a broad spectrum of malformations including anophthalmia, congenital heart defects, diaphragmatic hernia, alveolar capillary dysplasia, lung hypoplasia, and mental retardation. Am J Hum Genet. 2007 Mar;80(3):550-60. | PubMed |
Pasutto F, Sticht H, Hammersen G, Gillessen-Kaesbach G, Fitzpatrick DR, Nürnberg G, et al. Mutations in STRA6 cause a broad spectrum of malformations including anophthalmia, congenital heart defects, diaphragmatic hernia, alveolar capillary dysplasia, lung hypoplasia, and mental retardation. Am J Hum Genet. 2007 Mar;80(3):550-60. | PubMed | Segel R, Levy-Lahad E, Pasutto F, Picard E, Rauch A, Alterescu G, et al. Pulmonary hypoplasia-diaphragmatic hernia-nophthalmia-cardiac defect (PDAC) syndrome due to STRA6 mutations--what are the minimal criteria? Am J Med Genet A. 2009 Nov;149A(11):2457-63. | CrossRef | PubMed |
Segel R, Levy-Lahad E, Pasutto F, Picard E, Rauch A, Alterescu G, et al. Pulmonary hypoplasia-diaphragmatic hernia-nophthalmia-cardiac defect (PDAC) syndrome due to STRA6 mutations--what are the minimal criteria? Am J Med Genet A. 2009 Nov;149A(11):2457-63. | CrossRef | PubMed | Herman TE, Siegel MJ. Anopthalmia/microphthlamia-esophageal atresia association with additional features imperforate anus, choanal atresia, cyanotic heart disease. J Perinatol. 2012 Oct;32(10):814-6. | CrossRef | PubMed |
Herman TE, Siegel MJ. Anopthalmia/microphthlamia-esophageal atresia association with additional features imperforate anus, choanal atresia, cyanotic heart disease. J Perinatol. 2012 Oct;32(10):814-6. | CrossRef | PubMed | Nakata S, Imai Y, Takanashi Y, Kurosawa H, Tezuka K, Nakazawa M, et al. A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J Thorac Cardiovasc Surg. 1984 Oct;88(4):610-9. | PubMed |
Nakata S, Imai Y, Takanashi Y, Kurosawa H, Tezuka K, Nakazawa M, et al. A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J Thorac Cardiovasc Surg. 1984 Oct;88(4):610-9. | PubMed | McCarthy RW, Frenkel LD, Kollarits CR, Keys MP. Clinical anophthalmia associated with congenital cytomegalovirus infection. Am J Ophthalmol. 1980 Oct;90(4):558-61. | PubMed |
McCarthy RW, Frenkel LD, Kollarits CR, Keys MP. Clinical anophthalmia associated with congenital cytomegalovirus infection. Am J Ophthalmol. 1980 Oct;90(4):558-61. | PubMed | Ragge NK, Subak-Sharpe ID, Collin JR. A practical guide to the management of anophthalmia and microphthalmia. Eye (Lond). 2007 Oct;21(10):1290-300.
| PubMed |
Ragge NK, Subak-Sharpe ID, Collin JR. A practical guide to the management of anophthalmia and microphthalmia. Eye (Lond). 2007 Oct;21(10):1290-300.
| PubMed |