 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: renal cell carcinoma, hemorrhage, perioperative care, pericardiocentesis
In the United States during the year 2015, approximately 61,560 patients are expected to be diagnosed with kidney cancer and 14,080 to die from the disease. We present the case of a patient with renal cell carcinoma who suffered severe perioperative bleeding and coagulopathy after emergency sternotomy. We also engage in relevant aspects of perioperative anesthesia care including the considerations and management of coagulopathy, liver failure and renal failure in the oncologic patient. The case is a 49-year-old man with vena cava tumor thrombus who underwent radiologic tumor embolization, left radical nephrectomy, and inferior vena cava (IVC) thrombectomy. Postoperatively, he developed sepsis, multiple organ failure, and a pericardial effusion requiring pericardiocentesis. During pericardiocentesis, he suffered an iatrogenic left entricular perforation, requiring an emergency sternotomy and left ventricular repair. Cancer patients are often challenging for surgical and anesthesia teams, emergency care requires an organized and comprehensive approach. The use of recombinant factor VIIa NovoSeven can help in managing severe postoperative bleeding after cardiothoracic surgery in oncologic patients, but further studies should be done to confirm this.
In the United States, cancers of the kidney and of the renal pelvis are the seventh and tenth leading causes of new cancer cases in men and women, respectively. They are also the tenth leading cause of cancer deaths in men, who are almost twice as likely as women to develop kidney cancer. In 2015, approximately 61,560 patients were expected to be diagnosed with kidney cancer, and 14,080 were projected to die from the disease. Most of these cases would be renal cell carcinomas. At diagnosis, about 64% of cases present with local-stage disease; for these patients, the 5- and 10-year survival rates are 72% and 62%, respectively [1],[2].
We present the case of a patient with invasive renal cell carcinoma who experienced a chain of adverse events leading to an emergency sternotomy, severe intra- and postoperative bleeding, and coagulopathy. We discuss how the anesthesia team developed and implemented a successful strategy for management of postoperative bleeding in this emergent case.
Written informed consent for the publication of this case was obtained.
A 49-year-old male presented to his primary care physician, with bilateral lower extremity swelling, abdominal swelling, abdominal pain, dizziness, fatigue, and shortness of breath. These symptoms had developed over the course of four months after he had been treated for an upper respiratory infection with antibiotics and oral corticosteroids. A review of systems was negative. A full cardiac workup was also negative. The patient had a history of depression, anemia, erectile dysfunction, and obstructive sleep apnea. He reported no tobacco, alcohol, or illicit drug abuse. He had no family history of blood diseases but had a maternal uncle and grandfather with lung cancer. He was referred to a local cardiologist. An abdominal computed tomography (CT) study revealed a left renal mass with a thrombus in the inferior vena cava (IVC). The patient was then referred to MD Anderson Cancer Center for expert evaluation and treatment. Imaging studies to stage the tumor were performed. Magnetic resonance imaging (MRI) of the abdomen showed evidence of a left renal mass (6.4 × 4.5 × 5.6 cm) whose appearance was compatible with renal cell carcinoma; the mass extended into the suprahepatic and intrahepatic inferior vena cava and involved the left renal vein. Magnetic resonance imaging also revealed a right renal vein thrombus. Computed tomography of the chest unveiled a filling defect in the right lower lobe posterior basal segmental pulmonary artery; this defect was suspected to be either a tumor embolus or a bland pulmonary embolus. There were also three pulmonary nodules, from 3- to 4-mm, those were indeterminate and could have represented either granuloma or metastasis. The results of bilateral Doppler ultrasonography of the lower extremities, magnetic resonance imaging of the brain, and a bone scan were negative. The patient was classified as stage 3 and the treatment plan was surgery.
Further assessment revealed elevated liver function tests and a decrease in the patient’s functional status, leading to a diagnosis of Budd-Chiari syndrome. Therefore, the initial plan to operate was delayed until his condition improved enough that he could tolerate surgery. The interventional radiology team performed a left renal embolization and obtained a left renal biopsy, which was inconclusive upon pathologic analysis. In the following days, the patient deteriorated slowly and developed renal failure, along with encephalopathy caused by uremia and liver failure.
A month later, upon improvement of his condition, the patient was discharged from the hospital and scheduled for follow-up. By one-month follow-up, the patient no longer had any symptoms, imaging results, or laboratory tests suggesting Budd-Chiari syndrome. Left radical nephrectomy and possible left adrenalectomy and right radical nephrectomy along with inferior vena cava (IVC) thrombectomy and reconstruction were planned for later that month. The left radical nephrectomy, left adrenalectomy and inferior vena cava thrombectomy and reconstruction were performed. During surgery, however, the entire tumor thrombus could not be cleared from the hepatic vein, right renal vein, and right adrenal vein, so the surgical team refrained from conducting the right radical nephrectomy. It was also found that the tumor thrombus extended into the spine and spinal foramen and could not be completely excised.
Pathological examination of the surgical specimen revealed clear cell type, Fuhrman nuclear grade 3 renal cell carcinoma, with tumor invading the renal vein wall at the renal vein resection margin; metastatic carcinoma in one of four lymph nodes; and a renal cell carcinoma thrombus with vessel wall invasion at the inferior vena cava margin, right renal vein margin, and posterior lumbar vein margin.
The patient’s condition was stable and he was discharged home 10 days after surgery. One week after discharge, the patient presented to the emergency room with chest pain and abdominal pain. He was hospitalized, and treatment for sepsis and acute renal failure was initiated. The patient was evaluated for a pulmonary embolism, which was not confirmed. In the following days, an echocardiogram revealed that the patient had a large pericardial effusion that did not cause any hemodynamic instability or symptoms. Additionally, he had severe hiccups, raising the risks associated with pericardiocentesis. The patient was then found to be in atrial fibrillation and treated with intravenous amiodarone. Further studies, including liver function tests (LFTs) revealed liver failure. An abdominal computed tomography scan showed intrahepatic fluid collection. A second echocardiogram still showed evidence of pericardial effusion, but in light of the patient’s recent complicated surgery, a pericardial window was ruled out. Therefore, the treating team decided to place a pericardial drain via fluoroscopically guided pericardiocentesis. Unfortunately, the patient started coughing vigorously and unexpectedly during the procedure. It was discovered that the left ventricle had been perforated during catheter advancement. The patient was transferred to the operating room for emergency sternotomy with the catheter still in the chest (Figure 1).

Figure 1. Patient is transferred to the operating room with the catheter still in the chest.
Preoperative aspartate transaminase level (AST) of 77 IU/l (reference, 15-46 IU/L), alanine transaminase level (ALT) of 366 IU/l (reference, 7-56 IU/l), total bilirubin of 2.1 mg/dl (reference, 0.2-1.3 mg/dl), albumin 3 g/dl (reference, 3.5-4.7 g/dl), and creatinine 7.63 mg/dl.
Laboratory tests at the start of surgery showed an activated partial thromboplastin time (aPTT) of 195.1 sec, (reference, 24.7-35.9), prothrombin time (PT) of 20 sec (reference, 12.7-15.0), international normalized ratio (INR) of 1.73 (reference, 0.9-1.20), hemoglobin level (Hb) of 9.3 g/dl, and platelet count of 305 k/μl.
The patient’s vital signs were as follows: blood pressure (BP): 130/80 mm Hg; heart rate (HR): 110 beats per minute; respiratory rate (RR): 20 respirations per minute; and temperature: 37˚C.
The anesthesia team evaluated the patient as having an American Society of Anesthesiologists (ASA) physical classification of 4E and Mallampati class 2. The anesthesia plan included general endotracheal anesthesia using rapid sequence induction with cricoid pressure after surgical skin preparation with the patient awake. The patient was monitored in accordance with ASA standards. Because the patient was at risk for cardiac arrest and unstable dysrhythmia, we placed transcutaneous pacing pads (Figure 2). The patient underwent rapid sequence induction of general anesthesia with 250 μg fentanyl titrated, 1 mg midazolam, 20 mg etomidate, and 100 mg succinylcholine. The patient’s trachea was smoothly intubated using direct laryngoscopy with a size 2 Miller laryngoscope blade and a grade 1 view of the vocal cords. Positive end tidal CO2 and bilateral equal breath sounds were observed.
Anesthesia was maintained with desflurane, cisatracurium, and sufentanil. The patient was also given a loading dose of 1g aminocaproic acid as an antifibrinolytic, followed by a 1 g/h infusion.

Figure 2. Patient with the catheter in the chest and patch for transcutaneous pacing pad in position.
During the surgery, the surgeons noted a non-clotting bloody pericardial effusion. The catheter was already out of the left ventricle, and the puncture site, which was oozing blood, was identified. The bleeding was controlled with a single 5-0 Prolene polypropylene with pledget suture. Blood oozing from other surfaces was seen, and the pericardium seemed to be covered in a thrombin-like material with a rough whitish surface (Figure 3).
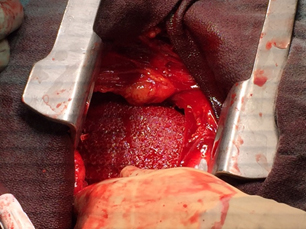
Figure 3. Left ventricle after repair with 5-0 Prolene suture.
After the incision was closed, the patient continued to lose blood: an estimated 3 L of blood was collected from the chest tubes over a period of 20 minutes. The anesthesia team managed bleeding and coagulopathy with standard blood products and fluids. The blood and blood products used were nine units of red blood cells, 12 units of fresh frozen plasma, 2 6-pack platelet units, and 2 10-units cryoprecipitate. Fluids administered included 500 ml 5% albumin. FloTrac/Vigileo (Edwards Lifesciences, Irvine, CA) minimally invasive hemodynamic monitoring was used for goal directed fluid therapy.
Because the bleeding had not stopped 20 minutes after closure of the incision, the surgeons considered reopening the incision and conducting further exploration, but they refrained from doing so, as the patient might not have tolerated a second procedure. The chest tubes continued to ooze blood, indicating a partial lack of response to the use of blood derivatives, so the anesthesia team decided to administer 10 mg NovoSeven recombinant factor VIIa (rFVIIa) (Novo Nordisk A/S, Bagsværd, Denmark). Ten minutes after administration of recombinant Factor VIIa, the blood loss was significantly reduced, with only an additional 200 ml collected over the next 30 minutes. The total estimated blood loss was 5.5 l. Vasopressin was also required during and after surgery for vasopressor support. The patient was stabilized in the operating room and then transferred to the intensive care unit. Transesophageal echocardiography performed in the operating room after surgery revealed minimal fluid surrounding the right atrium, but not collapsing it or any other vital structures.
Laboratory tests right at the end of surgery showed the following results: activated partial thromboplastin time (aPTT), 30 sec; prothrombin time (PT), 10 sec; international normalized ratio (INR), 0.68; hemoglobin (Hb), 9.5 g/dl; platelet count 184 k/μl, and fibrinogen, 433 mg/dl (reference, 202-450).
At the end of the procedure, samples of pericardial tissue were sent for pathologic analysis; the final report indicated acute fibrinous pericarditis. The patient was left with two chest tubes, a Blake drain from the previous surgery, and a Foley catheter. Postoperatively, the patient was managed in the intensive care unit for nine days, where he steadily improved, vasopressor support was discontinued, and he was weaned off mechanical ventilation and underwent intermittent hemodialysis. The patient showed no signs of coagulopathy. Having experienced no other complications, he was discharged to a long-term acute care facility 24 days after surgery, where management of his condition continued.
Treatment of cancer patients is often challenging for surgical and anesthesia teams. Both the natural course of the disease and adverse events related to medical care may have a significant impact on patient outcomes. The case presented here offers an opportunity to analyze a chain of adverse events in the management of a patient with complications of metastatic renal cell carcinoma, requiring consideration from both anesthetic and surgical points of view.
Renal cell carcinoma patients may develop a constellation of complications, as in the case presented here. Renal cell carcinoma can metastasize to the venous vessels; invasion of the IVC has been described in 4-15% of cases, of which 10-25% extend to the right atrium [3],[4]. Treatment for such cases includes radical nephrectomy and IVC thrombectomy [4],[5]. The choice of surgical strategy as well as the morbidity and mortality rates related to this procedure may be influenced by the level and volume of the tumor thrombus and the size of the tumor [5],[6],[7]. The 5-year survival rates of renal cell carcinoma patients undergoing radical nephrectomy and thrombectomy can drop from 60% to less than 20% if distant metastases are present [4],[8],[9]. Acute and chronic postoperative complications may include local or systemic infection, hemorrhage, deep vein thrombosis or pulmonary embolism, renal failure, the need for renal replacement therapy, myocardial infarction, and pneumothorax, among others [10].
Treatment for complications of radical nephrectomy and thrombectomy may present its own risks. Ventricular perforation, despite being a relatively rare complication of pericardiocentesis, is a catastrophic emergency that demands effective communication between surgical and anesthesia teams. The rate of ventricular perforation after image-guided pericardiocentesis has been reported to be around 1% and is influenced by the volume and location of the effusion, as well as its accessibility and the anatomical approach chosen [11],[12]. Right ventricle perforation is more common than left ventricle perforation, but the latter usually presents with more severe bleeding owing to the higher pressure in the left ventricle [13].
The relationship between cancer and coagulation disorders has been found in several studies. Malignancy induces a prothrombotic state that can increase tumor growth and dissemination. Tumor cells have the capacity of releasing procoagulants and inflammatory cytokines, which put the patient at a high risk of developing venous and arterial thrombosis. The clinical manifestations of cancer-related coagulation disorders range from asymptomatic to thrombosis of large vessels, or even severe bleeding caused by disseminated intravascular coagulation (DIC) [14],[15].
Postoperative bleeding after cardiothoracic surgery has been reported to occur in 5-11% of cases, and blood products are needed during as many as 80% of complex thoracic surgery cases. Postoperative bleeding can dramatically increase rates of morbidity and mortality and the lengths of hospital stays [16],[17],[18]. Traditionally, postoperative bleeding in cardiac surgery has been managed with blood products [16],[19].
More recently, recombinant Factor VIIa has been used off-label to aid hemostasis in challenging cases, [16],[17],[18],[19] such as this one, in which liver injury and sepsis aggravated coagulopathy [18],[20]. The mechanism of action of recombinant Factor VIIa involves binding to tissue factor (TF). Thrombin is generated from this process through the activation of Factor X (FX), and it will later activate platelets. At pharmacological doses recombinant Factor VIIa can also bind and activate Factor X on activated platelets. Factor X forms a complex with Factor Va, this will lead to a thrombin burst, and the production of a stable fibrin clot at the site of vessel injury [21],[22].
Sallah et al. published a series of 18 patients with cancer-related disseminated intravascular coagulation (DIC), for which recombinant Factor VIIa was used successfully after conventional therapy when blood products failed [23].
Patients undergoing cancer surgery face an increased risk of severe bleeding and coagulopathy during major surgical procedures. Multiple factors contribute to this increased risk, including tumor biology, the location of the tumor, the complexity of resection, previous oncological treatment, and comorbidities. Transfusion of blood products in oncologic surgery is used to improve delivery of oxygen and correct hemostasis disorders.
In cancer surgery, coagulation disorders can occur preoperatively, usually as a result of anticoagulant administration or cancer-related complications. However, they may also occur intra- and postoperatively, commonly due to hemodilution or consumption of coagulation factors, with the latter occurring in complications such as sepsis [20].
In this patient, vasopressor support was necessary, considering his hemodynamics in the presence of sepsis, surgical trauma, and liver failure. Endogenous vasopressin levels have been shown to be decreased in patients with septic shock, as well as those with end-stage liver failure [24],[25]. Additionally, desmopressin has also been used in the management of postoperative bleeding [19].
The anesthesia team must, therefore, be prepared for hemodynamic complications in cancer patients, and anticipate every possible scenario to provide timely treatment and to avoid adverse events. Anesthetic considerations must be continually assessed and re-assessed in patients undergoing emergency cardiothoracic cancer surgery: prior to induction, throughout the surgery, and postoperatively. Adequate intravenous and arterial lines must be secured before induction and the need for a central venous catheter should be assessed. Proper fluid management monitoring is especially critical for these patients; tools such as the FloTrac/Vigileo™ (Edwards Lifesciences, Irvine, CA, USA) are useful, keeping in mind that cardiac output monitoring in patients with sepsis or cirrhosis may be inaccurate [26],[27].
Blood products must be made available for immediate use, along with a rapid infuser to treat hypovolemic shock and re-establish proper hemodynamics [17],[28]. Hypothermia and acidosis management is also imperative, as both factors can aggravate coagulopathy [19],[29],[30]. Hypocalcemia may develop, especially in patients given large volumes of blood products; it should be identified and treated promptly, as it can further worsen coagulation capacity [29]. Preoxygenation should be followed by rapid sequence intubation using medications with an appropriate cardiovascular profile, as in any case of traumatic heart injury [31].
Treatment of cancer patients is often challenging for surgical and anesthesia teams. Both the natural course of the disease and adverse events related to medical care may have a significant impact on patient outcomes.
Implementing a comprehensive strategy is necessary for the treatment of a critically ill patient such as this one. The management of a cancer patient requiring emergency cardiothoracic surgery can be especially difficult in the presence of multi-organ failure and coagulopathy.
In this case, off-label use of recombinant Factor VIIa was an effective management for severe postoperative bleeding after emergency cardiothoracic surgery when traditional blood products were not enough. This should be analyzed carefully, as other factors may have influenced the patient’s improvement. Further studies should be made to evaluate its efficacy and safety in oncologic patients.
From the editor
The authors originally submitted this article in Spanish and English. The Journal has not copyedited the English version.
Ethical aspects
Informed consent requested by Medwave, has been signed by the patient and a copy was sent to the journal editorial board.
Conflicts of interest
The authors completed the ICMJE declaration of conflicts of interest and declare they have not received funding for the completion of the report; have no financial relationships with organizations that may have interests in the article published in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or editorial direction of the Journal.
Funding
The authors declare no external funding sources for this article.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

In the United States during the year 2015, approximately 61,560 patients are expected to be diagnosed with kidney cancer and 14,080 to die from the disease. We present the case of a patient with renal cell carcinoma who suffered severe perioperative bleeding and coagulopathy after emergency sternotomy. We also engage in relevant aspects of perioperative anesthesia care including the considerations and management of coagulopathy, liver failure and renal failure in the oncologic patient. The case is a 49-year-old man with vena cava tumor thrombus who underwent radiologic tumor embolization, left radical nephrectomy, and inferior vena cava (IVC) thrombectomy. Postoperatively, he developed sepsis, multiple organ failure, and a pericardial effusion requiring pericardiocentesis. During pericardiocentesis, he suffered an iatrogenic left entricular perforation, requiring an emergency sternotomy and left ventricular repair. Cancer patients are often challenging for surgical and anesthesia teams, emergency care requires an organized and comprehensive approach. The use of recombinant factor VIIa NovoSeven can help in managing severe postoperative bleeding after cardiothoracic surgery in oncologic patients, but further studies should be done to confirm this.
 Autores:
Javier Lasala[1], Miguel Alejandro Patino[1], Gabriel Mena[1], Shital Vachhani[1], Teresa Moon[1], Thao Bui[1], January Tsai[1]
Autores:
Javier Lasala[1], Miguel Alejandro Patino[1], Gabriel Mena[1], Shital Vachhani[1], Teresa Moon[1], Thao Bui[1], January Tsai[1]

Citación: Lasala J, Patino MA, Mena G, Vachhani S, Moon T, Bui T, et al. Severe perioperative bleeding in renal cell carcinoma after elective pericardiocentesis associated left ventricular puncture: case report . Medwave 2016 Jul;16(6):e6494 doi: 10.5867/medwave.2016.06.6494
Fecha de envío: 22/2/2016
Fecha de aceptación: 29/6/2016
Fecha de publicación: 12/7/2016
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015 Jan-Feb;65(1):5-29.
| CrossRef | PubMed |
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015 Jan-Feb;65(1):5-29.
| CrossRef | PubMed | Society AC: Cancer Facts & Figures 2015. Atlanta, Ga: American Cancer Society; 2015: 56.
Society AC: Cancer Facts & Figures 2015. Atlanta, Ga: American Cancer Society; 2015: 56.  Belgrano E, Trombetta C, Siracusano S, Carmignanib G, Martoranac G, Liguori G. Surgical management of renal cell carcinoma (RCC) with vena cava tumour thrombus. European Urology Supplements. 5(2006):610-618. | Link |
Belgrano E, Trombetta C, Siracusano S, Carmignanib G, Martoranac G, Liguori G. Surgical management of renal cell carcinoma (RCC) with vena cava tumour thrombus. European Urology Supplements. 5(2006):610-618. | Link | Bigot P, Fardoun T, Bernhard JC, Xylinas E, Berger J, Rouprêt M, et al. Neoadjuvant targeted molecular therapies in patients undergoing nephrectomy and inferior vena cava thrombectomy: is it useful? World J Urol. 2014 Feb;32(1):109-14. | CrossRef | PubMed |
Bigot P, Fardoun T, Bernhard JC, Xylinas E, Berger J, Rouprêt M, et al. Neoadjuvant targeted molecular therapies in patients undergoing nephrectomy and inferior vena cava thrombectomy: is it useful? World J Urol. 2014 Feb;32(1):109-14. | CrossRef | PubMed | Helfand BT, Smith ND, Kozlowski JM, Eskandari MK. Vena cava thrombectomy and primary repair after radical nephrectomy for renal cell carcinoma: single-center experience. Ann Vasc Surg. 2011 Jan;25(1):39-43. | CrossRef | PubMed |
Helfand BT, Smith ND, Kozlowski JM, Eskandari MK. Vena cava thrombectomy and primary repair after radical nephrectomy for renal cell carcinoma: single-center experience. Ann Vasc Surg. 2011 Jan;25(1):39-43. | CrossRef | PubMed | Zargar-Shoshtari K, Sharma P, Espiritu P, Kurian T, Pow-Sang JM, Mangar D, et al. Caval tumor thrombus volume influences outcomes in renal cell carcinoma with venous extension. Urol Oncol. 2015 Mar;33(3):112.e23-9. | CrossRef | PubMed |
Zargar-Shoshtari K, Sharma P, Espiritu P, Kurian T, Pow-Sang JM, Mangar D, et al. Caval tumor thrombus volume influences outcomes in renal cell carcinoma with venous extension. Urol Oncol. 2015 Mar;33(3):112.e23-9. | CrossRef | PubMed | Cost NG, Delacroix SE Jr, Sleeper JP, Smith PJ, Youssef RF, Chapin BF, et al. The impact of targeted molecular therapies on the level of renal cell carcinoma vena caval tumor thrombus. Eur Urol. 2011 Jun;59(6):912-8. | CrossRef | PubMed |
Cost NG, Delacroix SE Jr, Sleeper JP, Smith PJ, Youssef RF, Chapin BF, et al. The impact of targeted molecular therapies on the level of renal cell carcinoma vena caval tumor thrombus. Eur Urol. 2011 Jun;59(6):912-8. | CrossRef | PubMed | Klatte T, Pantuck AJ, Riggs SB, Kleid MD, Shuch B, Zomorodian N, et al. Prognostic factors for renal cell carcinoma with tumor thrombus extension. J Urol. 2007 Oct;178(4 Pt 1):1189-95. | PubMed |
Klatte T, Pantuck AJ, Riggs SB, Kleid MD, Shuch B, Zomorodian N, et al. Prognostic factors for renal cell carcinoma with tumor thrombus extension. J Urol. 2007 Oct;178(4 Pt 1):1189-95. | PubMed | Manassero F, Mogorovich A, Di Paola G, Valent F, Perrone V, Signori S, et al. Renal cell carcinoma with caval involvement: contemporary strategies of surgical treatment. Urol Oncol. 2011 Nov-Dec;29(6):745-50. | CrossRef | PubMed |
Manassero F, Mogorovich A, Di Paola G, Valent F, Perrone V, Signori S, et al. Renal cell carcinoma with caval involvement: contemporary strategies of surgical treatment. Urol Oncol. 2011 Nov-Dec;29(6):745-50. | CrossRef | PubMed | lute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int. 2004 Jul;94(1):33-41. | CrossRef | PubMed |
lute ML, Leibovich BC, Lohse CM, Cheville JC, Zincke H. The Mayo Clinic experience with surgical management, complications and outcome for patients with renal cell carcinoma and venous tumour thrombus. BJU Int. 2004 Jul;94(1):33-41. | CrossRef | PubMed | McIntyre WF, Jassal DS, Morris AL. Pericardial effusions: do they all require pericardiocentesis? Can J Cardiol. 2015 Jun;31(6):812-5. | CrossRef | PubMed |
McIntyre WF, Jassal DS, Morris AL. Pericardial effusions: do they all require pericardiocentesis? Can J Cardiol. 2015 Jun;31(6):812-5. | CrossRef | PubMed | Pourdjabbar A, Hibbert B, Hendry P, Labinaz M. Angio-Seal closure of an iatrogenic right ventricular perforation. Clin Res Cardiol. 2014 Jul;103(7):577-9. | CrossRef | PubMed |
Pourdjabbar A, Hibbert B, Hendry P, Labinaz M. Angio-Seal closure of an iatrogenic right ventricular perforation. Clin Res Cardiol. 2014 Jul;103(7):577-9. | CrossRef | PubMed | Loukas M, Walters A, Boon JM, Welch TP, Meiring JH, Abrahams PH. Pericardiocentesis: a clinical anatomy review. Clin Anat. 2012 Oct;25(7):872-81. | CrossRef | PubMed |
Loukas M, Walters A, Boon JM, Welch TP, Meiring JH, Abrahams PH. Pericardiocentesis: a clinical anatomy review. Clin Anat. 2012 Oct;25(7):872-81. | CrossRef | PubMed | Falanga A, Russo L, Milesi V. The coagulopathy of cancer. Curr Opin Hematol. 2014 Sep;21(5):423-9. | CrossRef | PubMed |
Falanga A, Russo L, Milesi V. The coagulopathy of cancer. Curr Opin Hematol. 2014 Sep;21(5):423-9. | CrossRef | PubMed | De Cicco M. The prothrombotic state in cancer: pathogenic mechanisms. Crit Rev Oncol Hematol. 2004 Jun;50(3):187-96. | PubMed |
De Cicco M. The prothrombotic state in cancer: pathogenic mechanisms. Crit Rev Oncol Hematol. 2004 Jun;50(3):187-96. | PubMed | Bishop CV, Renwick WE, Hogan C, Haeusler M, Tuckfield A, Tatoulis J. Recombinant activated factor VII: treating postoperative hemorrhage in cardiac surgery. Ann Thorac Surg. 2006 Mar;81(3):875-9. | PubMed |
Bishop CV, Renwick WE, Hogan C, Haeusler M, Tuckfield A, Tatoulis J. Recombinant activated factor VII: treating postoperative hemorrhage in cardiac surgery. Ann Thorac Surg. 2006 Mar;81(3):875-9. | PubMed | Warren O, Mandal K, Hadjianastassiou V, Knowlton L, Panesar S, John K, et al. Recombinant activated factor VII in cardiac surgery: a systematic review. Ann Thorac Surg. 2007 Feb;83(2):707-14. | PubMed |
Warren O, Mandal K, Hadjianastassiou V, Knowlton L, Panesar S, John K, et al. Recombinant activated factor VII in cardiac surgery: a systematic review. Ann Thorac Surg. 2007 Feb;83(2):707-14. | PubMed | Lau P, Ong V, Tan WT, Koh PL, Hartman M. Use of Activated Recombinant Factor VII in Severe Bleeding - Evidence for Efficacy and Safety in Trauma, Postpartum Hemorrhage, Cardiac Surgery, and Gastrointestinal Bleeding. Transfus Med Hemother. 2012 Apr;39(2):139-150. | PubMed |
Lau P, Ong V, Tan WT, Koh PL, Hartman M. Use of Activated Recombinant Factor VII in Severe Bleeding - Evidence for Efficacy and Safety in Trauma, Postpartum Hemorrhage, Cardiac Surgery, and Gastrointestinal Bleeding. Transfus Med Hemother. 2012 Apr;39(2):139-150. | PubMed | Elizalde M, Slobodskoy L, Diodato M, Chang J, Chedrawy EG. Use of recombinant factor VII in cardiac surgery. Recent Pat Cardiovasc Drug Discov. 2012 Dec;7(3):216-20. | PubMed |
Elizalde M, Slobodskoy L, Diodato M, Chang J, Chedrawy EG. Use of recombinant factor VII in cardiac surgery. Recent Pat Cardiovasc Drug Discov. 2012 Dec;7(3):216-20. | PubMed | Cata JP, Gottumukkala V. Blood transfusion practices in cancer surgery. Indian J Anaesth. 2014 Sep;58(5):637-42. | CrossRef | PubMed |
Cata JP, Gottumukkala V. Blood transfusion practices in cancer surgery. Indian J Anaesth. 2014 Sep;58(5):637-42. | CrossRef | PubMed | Franchini M, Manzato F, Salvagno GL, Lippi G. Potential role of recombinant activated factor VII for the treatment of severe bleeding associated with disseminated intravascular coagulation: a systematic review. Blood Coagul Fibrinolysis. 2007 Oct;18(7):589-93. | PubMed |
Franchini M, Manzato F, Salvagno GL, Lippi G. Potential role of recombinant activated factor VII for the treatment of severe bleeding associated with disseminated intravascular coagulation: a systematic review. Blood Coagul Fibrinolysis. 2007 Oct;18(7):589-93. | PubMed | Neufeld EJ, Négrier C, Arkhammar P, Benchikh el Fegoun S, Simonsen MD, Rosholm A, et al. Safety update on the use of recombinant activated factor VII in approved indications. Blood Rev. 2015 Jun;29 Suppl 1:S34-41. | CrossRef | PubMed |
Neufeld EJ, Négrier C, Arkhammar P, Benchikh el Fegoun S, Simonsen MD, Rosholm A, et al. Safety update on the use of recombinant activated factor VII in approved indications. Blood Rev. 2015 Jun;29 Suppl 1:S34-41. | CrossRef | PubMed | Sallah S, Husain A, Nguyen NP. Recombinant activated factor VII in patients with cancer and hemorrhagic disseminated intravascular coagulation. Blood Coagul Fibrinolysis. 2004 Oct;15(7):577-82. | PubMed |
Sallah S, Husain A, Nguyen NP. Recombinant activated factor VII in patients with cancer and hemorrhagic disseminated intravascular coagulation. Blood Coagul Fibrinolysis. 2004 Oct;15(7):577-82. | PubMed | Wagener G, Kovalevskaya G, Minhaz M, Mattis F, Emond JC, Landry DW. Vasopressin deficiency and vasodilatory state in end-stage liver disease. J Cardiothorac Vasc Anesth. 2011 Aug;25(4):665-70. | CrossRef | PubMed |
Wagener G, Kovalevskaya G, Minhaz M, Mattis F, Emond JC, Landry DW. Vasopressin deficiency and vasodilatory state in end-stage liver disease. J Cardiothorac Vasc Anesth. 2011 Aug;25(4):665-70. | CrossRef | PubMed | Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D. Circulating vasopressin levels in septic shock. Crit Care Med. 2003 Jun;31(6):1752-8. | PubMed |
Sharshar T, Blanchard A, Paillard M, Raphael JC, Gajdos P, Annane D. Circulating vasopressin levels in septic shock. Crit Care Med. 2003 Jun;31(6):1752-8. | PubMed | Marqué S, Gros A, Chimot L, Gacouin A, Lavoué S, Camus C, et al. Cardiac output monitoring in septic shock: evaluation of the third-generation Flotrac-Vigileo. J Clin Monit Comput. 2013 Jun;27(3):273-9. | CrossRef | PubMed |
Marqué S, Gros A, Chimot L, Gacouin A, Lavoué S, Camus C, et al. Cardiac output monitoring in septic shock: evaluation of the third-generation Flotrac-Vigileo. J Clin Monit Comput. 2013 Jun;27(3):273-9. | CrossRef | PubMed | Argueta E, Berdine G, Pena C, Nugent KM. FloTrac® monitoring system: what are its uses in critically ill medical patients? Am J Med Sci. 2015 Apr;349(4):352-6. | CrossRef | PubMed |
Argueta E, Berdine G, Pena C, Nugent KM. FloTrac® monitoring system: what are its uses in critically ill medical patients? Am J Med Sci. 2015 Apr;349(4):352-6. | CrossRef | PubMed | Stammers AH, Murdock JD, Klayman MH, Trowbridge C, Yen BR, Franklin D, et al. Utilization of rapid-infuser devices for massive blood loss. Perfusion. 2005 Mar;20(2):65-9. | PubMed |
Stammers AH, Murdock JD, Klayman MH, Trowbridge C, Yen BR, Franklin D, et al. Utilization of rapid-infuser devices for massive blood loss. Perfusion. 2005 Mar;20(2):65-9. | PubMed | De Robertis E, Kozek-Langenecker SA, Tufano R, Romano GM, Piazza O, Zito Marinosci G. Coagulopathy induced by acidosis, hypothermia and hypocalcaemia in severe bleeding. Minerva Anestesiol. 2015 Jan;81(1):65-75. | PubMed |
De Robertis E, Kozek-Langenecker SA, Tufano R, Romano GM, Piazza O, Zito Marinosci G. Coagulopathy induced by acidosis, hypothermia and hypocalcaemia in severe bleeding. Minerva Anestesiol. 2015 Jan;81(1):65-75. | PubMed | Martini WZ. Coagulopathy by hypothermia and acidosis: mechanisms of thrombin generation and fibrinogen availability. J Trauma. 2009 Jul;67(1):202-8 | CrossRef | PubMed |
Martini WZ. Coagulopathy by hypothermia and acidosis: mechanisms of thrombin generation and fibrinogen availability. J Trauma. 2009 Jul;67(1):202-8 | CrossRef | PubMed | Nussmeier N, Sarwar M, Searles B, Shore-Lessernon L, Stone M, Rossel I. Anesthesia for cardiac surgical procedures, in Miller R (editor): Miller's Anesthesia, Eighth ed. Philadelphia, PA: Saunders; 2015:2073-6.
Nussmeier N, Sarwar M, Searles B, Shore-Lessernon L, Stone M, Rossel I. Anesthesia for cardiac surgical procedures, in Miller R (editor): Miller's Anesthesia, Eighth ed. Philadelphia, PA: Saunders; 2015:2073-6.