 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: diaphragmatic hernia, cardiopulmonary arrest, laparoscopic surgery
A previously well 71-year-old woman presented to the Emergency Department with acute-onset left-sided chest pain. She was haemodynamically stable with unremarkable systemic examination. Her electrocardiogram and troponin were within normal limits and her chest radiograph showed a raised left hemi-diaphragm. Two hours after admission, this woman became acutely breathless, and suffered a pulseless electrical activity cardiac arrest. After cardiopulmonary resuscitation, there was a return of spontaneous circulation and regained consciousness. A repeat clinical assessment revealed a new left-sided dullness to percussion with contralateral percussive resonance on respiratory examination. CXR revealed a left pan-hemi-thoracic opacity whilst better definition using CT-pulmonary angiography (CTPA) indicated an acute tension gastrothorax secondary to a large left-sided diaphragmatic her-nia. Nasogastric (NG) tube insertion was used to decompress the stomach and the patient underwent uncomplicated emergency laparoscopic hernia reduction. She remained well at 1-year follow-up.
The aetiology of chest pain is vast and can include causes ranging from those that are cardiac such as acute myocardial infarction or pericarditis to those that are extra-cardiac, e.g. pulmonary embolism, costochondritis. Less commonly, chest pain may present as an indicator of intra-abdominal pathology, e.g. perforated peptic ulcer or pancreatitis [1]. After exclusion of common and less common causes of chest pain, acute gastrothorax should be considered within a differential diagnosis. Acute gastrothorax is post-traumatic in up to 15% of cases but can rarely occur due to diaphragmatic defects [2]. This can occur within adults and the paediatric population, which is often secondary to congenital diaphragmatic hernias within the latter group.
We present a case of an acute gastrothorax masquerading with a presenting complaint of chest pain and atypical radiological findings with near-fatal consequences.
A 71-year-old woman presented to the emergency department with a one-hour history of left-sided non-radiating chest pain. She was on oral anti-hypertensives: amlodipine and bendrofluazide but otherwise previously fit and well and was never a smoker. She was haemodynamically stable on arrival to the emergency department and systemic examination was unremarkable. Her electrocardiogram did not reveal any ischaemic changes. She was assessed for an acute coronary syndrome and her troponin was normal. Her chest X-ray revealed evidence of a markedly raised left hemi-diaphragm (Figure 1a).
Subsequently, two hours later she suddenly became acutely breathless and had a cardio-respiratory compromise with pulseless electrical activity cardiac arrest; thereafter three cycles of cardiopulmonary resuscitation for a non-shockable rhythm with return of spontaneous circulation. The patient was alert, conscious and had a patent airway with spontaneous but laboured breathing and adequate peripheral circulation.
The differential diagnosis included probable pulmonary embolism, acute coronary syndrome or tension-pneumothorax. Repeat 12-lead electrocardiogram was normal, arterial-blood-gas revealed uncompensated type-1 respiratory failure with normal base excess. While investigating for reversible causes for pulseless electrical activity-arrest, an urgent chest X-ray was performed for new clinical findings of relatively diminished vesicular breath sounds and dullness to percussion throughout the left lung field with good vesicular breath sounds and resonance to percussion over the right lung-field. This repeat chest X-ray revealed left hemi-thoracic opacification filling two-thirds of the chest (Figure 1b).
An urgent out-of-hours CT pulmonary angiogram was performed to exclude pulmonary-embolism and to radiologically investigate the new chest X-ray findings. The CT pulmonary angiogram revealed a large incarcerated left-sided diaphragmatic hernia containing distended stomach over the left hemi-thorax causing mediastinal shift and upward displacement of the lung parenchyma; strongly suggestive of acute tension gastrothorax (Figure 1c-d).
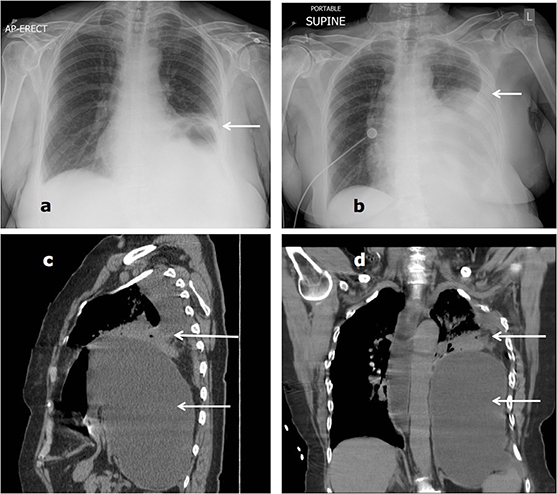
Figure 1. (a) Chest radiograph on admission highlighting raised left hemi-diaphragm, (b) chest radiograph after resuscitation showing a left hemi-thoracic opacification up to two-thirds of the chest with no features of acute pneumothorax, (c) sagittal view and (d) coronal view computed tomographic pulmonary angiogram (CTPA) showing left-sided gastrothorax and compression of left lung
An urgent nasogastric tube was inserted to prevent further lethal cardiorespiratory compromise. A repeat chest X-ray for positioning revealed worsening of the left hemi-thoracic opacity showing pan-hemi-thoracic opacification (Figure 2a). The nasogastric tube drained two and half litres of dark-brown aspirate with an acidic pH. Central-venous-access was secured and the patient successfully underwent an emergency laparoscopic herniorrhaphy of the incarcerated diaphragmatic hernia (Figure 3). Post-operative radiological findings on the intensive care unit (ICU) show resolution of the left hemi-thoracic defect (Figure 2b).
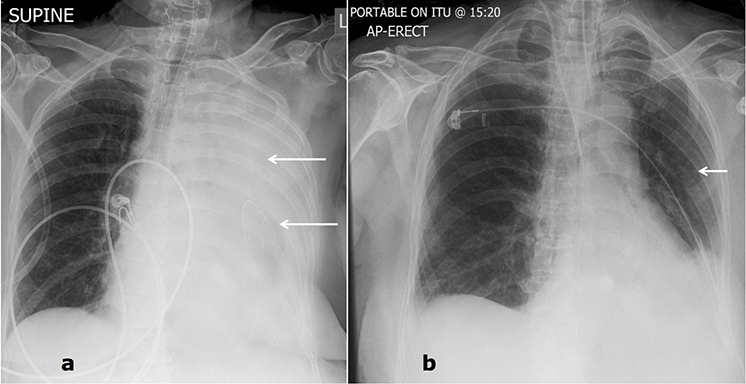
Figure 2: (a) Chest radiograph confirming nasogastric tube placement within the stomach in the left hemi-thorax with left pan-hemi-thoracic opacification, (b) Post-operative chest radiographic findings with normal lung fields.
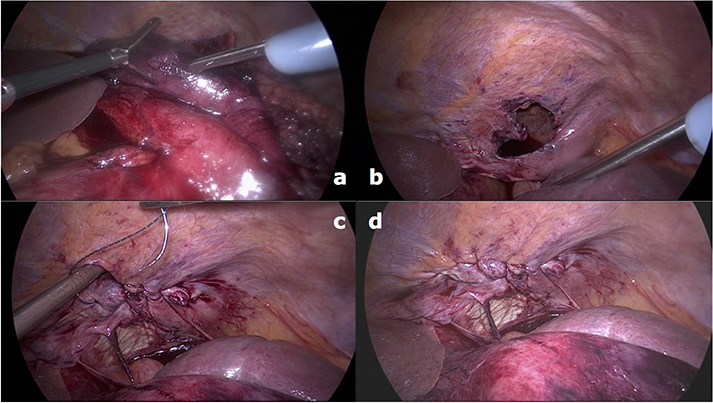
Figure 3: Intra-operative pictures of laparoscopic reduction of incarcerated diaphragmatic hernia as viewed from abdomen. (a) Herniated stomach into thorax, (b) apparent extent of diaphragmatic hernia after manipulation of stomach out of thorax, (c) suturing and (d) reduction of diaphragmatic hernia with stomach within the abdominal cavity.
The patient recovered well from the procedure with no complications and was discharged home within a fortnight after initial presentation. The patient remained stable when she was reviewed in the outpatient clinic 12 months later.
The aetiology of this patient’s gastrothorax is likely to be a diaphragmatic hernia. Diaphragmatic hernias may be congenital or acquired. The former option often presents in infancy with cardio-respiratory distress [3], which is sometimes associated with other abnormalities and genetic polymorphisms [4]. However, this patient is likely to have had an acquired diaphragmatic hernia. Many cases often follow blunt or penetrating trauma, including surgery, but with those cases that were non-traumatic are termed ‘spontaneous’. These often are causes by episodes involving raised intra-abdominal pressure including the Valsalva manoeuvre such as coughing, vomiting or even childbirth [5],[6].
We present a case of non-traumatic acute gastrothorax, which is one of few cases that presented with chest pain [7]. In contrast the case presented by Solé and colleagues (2013) demonstrated a similar clinical presentation of suspected acute coronary syndrome (ACS) but with widespread ST depression on electrocardiogram. Despite this, there was no hemi-thoracic neo-opacity on the chest radiograph as suggested by this study. Of the remaining cases of spontaneous gastrothoraces, both patients presented to the emergency department with respiratory distress and had known diaphragmatic hernias as suggested by previous history of hiatus hernia [8],[9]. The patient presented in our case notably did have a hiatus hernia. Both cases required decompression via endoscopy or a nasogastric tube and undefined corrective surgery [8],[9]. Traumatic gastrothorax was caused by vehicle collision by two cases [2],[10] and by playing party games 18 days prior to presentation [11]. Other traumatic cases implicated resuscitation [12] and esophagectomy and metastatic tumour recurrence [13] as causes of gastrothoraces.
An acute gastrothorax is a clinically rare but life-threatening condition often excluded in a differential diagnosis in the context of a patient presenting with chest pain. The clinical examination findings along with the cardiac arrest may allow the consideration of a tension pneumothorax as a possible diagnosis. Treatment of a tension pneumothorax at the bedside via needle decompression may result in disastrous consequences such as gastric perforation and acute lung injury [10]. Within the literature there are a number of clinical presentations of gastrothorax including breathlessness [12],[13],[14], lower back pain [13], cough [13], nausea [7] with investigative findings such as ischaemic electrocardiogram changes [7],[12].
Our case is unique in presentation as it is the second case to describe an acute presentation of a gastrothorax with chest pain [7]. Despite this, we describe a unique radiological finding of complete left hemi-thoracic radio-opacity which contrasts the vast majority of existing cases within the literature which describe radiolucent gastric bubbles within the left hemi-thorax [9],[11],[13],[14],[15].
Whilst clinical presentations may differ there is an overlying consensus that a gastrothorax requires urgent decompression via an nasogastric tube [7],[9],[11],[12],[13] at first presentation. An algorithm, which albeit is tailored for the paediatric population [16] suggests that further treatment should involve transthoracic needle decompression of the stomach if decompression is unsuccessful, with a view to surgery to correct the diaphragmatic defect [16]. Alternatives to the herniorrhaphy to the diaphragm with reduction of the diaphragmatic hernia include an open approach as compared to the laparoscopic approach that is likely to result in larger scar formation, prolonged post-operative pain and recovery [17]. Whilst there is a paucity of data specifically comparing techniques of surgical reduction of a gastrothorax, some data around the inguinal hernia repair suggest that laparoscopic technique carry a risk of intra-operative visceral injury, such as stomach and pericardium in this case [17]. Mesh repair, i.e. hernioplasty could potentially risk infection in an area in the thorax or abdomen but there is a lack of data to substantiate this extrapolation from inguinal studies [17].
Acute gastrothorax should be considered in all patients presenting with acute-onset left-sided chest pain especially with an unremarkable medical history and normal initial investigations. History taking should explore risk factors for a gastrothorax including recent activities increasing intra-abdominal pressure, traumatic injury, or known diaphragmatic or hiatus hernia. Furthermore, chest radiographic findings of a unilateral hemi-thoracic opacity may indeed represent fluid within the thorax, which may lie within the stomach as opposed to the pleural cavity. After initial stabilisation, urgent surgical intervention is required to reduce radiologically-confirmed acute tension gastrothorax causing mediastinal shift.
From the editor
This article was originally submitted in Spanish and English by the authors. The Journal has not copyedited the English version.
Ethical aspects
Informed consent requested by Medwave, was signed by the patient. A copy of this document was sent to the editorship of the Journal.
Conflicts of interests
The authors completed the ICMJE conflict of interest declaration form. They declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Funding
The authors declare that no external funding sources.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

A previously well 71-year-old woman presented to the Emergency Department with acute-onset left-sided chest pain. She was haemodynamically stable with unremarkable systemic examination. Her electrocardiogram and troponin were within normal limits and her chest radiograph showed a raised left hemi-diaphragm. Two hours after admission, this woman became acutely breathless, and suffered a pulseless electrical activity cardiac arrest. After cardiopulmonary resuscitation, there was a return of spontaneous circulation and regained consciousness. A repeat clinical assessment revealed a new left-sided dullness to percussion with contralateral percussive resonance on respiratory examination. CXR revealed a left pan-hemi-thoracic opacity whilst better definition using CT-pulmonary angiography (CTPA) indicated an acute tension gastrothorax secondary to a large left-sided diaphragmatic her-nia. Nasogastric (NG) tube insertion was used to decompress the stomach and the patient underwent uncomplicated emergency laparoscopic hernia reduction. She remained well at 1-year follow-up.
 Autores:
Deepwant Singh[1], Pieter Mackeith [2], Dipesh Pravin Gopal [3]
Autores:
Deepwant Singh[1], Pieter Mackeith [2], Dipesh Pravin Gopal [3]

Citación: Singh D , Mackeith P, Gopal DP. Acute non-traumatic gastrothorax: presentation of a case with chest pain and atypical radiologic findings. Medwave 2016 Mar;16(2):e6409 doi: 10.5867/medwave.2016.02.6409
Fecha de envío: 26/11/2015
Fecha de aceptación: 11/3/2016
Fecha de publicación: 23/3/2016
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Amsterdam EA, Kirk JD, Bluemke DA, Diercks D, Farkouh ME, Garvey JL, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010 Oct 26;122(17):1756-76. | CrossRef | PubMed |
Amsterdam EA, Kirk JD, Bluemke DA, Diercks D, Farkouh ME, Garvey JL, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010 Oct 26;122(17):1756-76. | CrossRef | PubMed | Nishijima D, Zehbtachi S, Austin RB. Acute posttraumatic tension gastrothorax mimicking acute tension pneumothorax. Am J Emerg Med. 2007 Jul;25(6):734.e5-6. | PubMed |
Nishijima D, Zehbtachi S, Austin RB. Acute posttraumatic tension gastrothorax mimicking acute tension pneumothorax. Am J Emerg Med. 2007 Jul;25(6):734.e5-6. | PubMed | Robinson PD, Fitzgerald DA. Congenital diaphragmatic hernia. Paediatr RespirRev. 2007 Dec;8(4):323-34; quiz 334-5. | PubMed |
Robinson PD, Fitzgerald DA. Congenital diaphragmatic hernia. Paediatr RespirRev. 2007 Dec;8(4):323-34; quiz 334-5. | PubMed | Wynn J, Yu L, Chung WK. Genetic causes of congenital diaphragmatic hernia. Semin Fetal Neonatal Med. 2014 Dec;19(6):324-30. | CrossRef | PubMed |
Wynn J, Yu L, Chung WK. Genetic causes of congenital diaphragmatic hernia. Semin Fetal Neonatal Med. 2014 Dec;19(6):324-30. | CrossRef | PubMed | Losanoff JE, Edelman DA, Salwen WA, Basson MD. Spontaneous rupture of the diaphragm: case report and comprehensive review of the world literature. J Thorac Cardiovasc Surg. 2010 Jun;139(6):e127-8. | CrossRef | PubMed |
Losanoff JE, Edelman DA, Salwen WA, Basson MD. Spontaneous rupture of the diaphragm: case report and comprehensive review of the world literature. J Thorac Cardiovasc Surg. 2010 Jun;139(6):e127-8. | CrossRef | PubMed | Ghidirim G, Mishin I, Condratsky E, Zastavnitsky G. Spontaneous diaphragmatic rupture: case report and literature review. Chirurgia (Bucur). 2013 Jan-Feb;108(1):99-101. | PubMed |
Ghidirim G, Mishin I, Condratsky E, Zastavnitsky G. Spontaneous diaphragmatic rupture: case report and literature review. Chirurgia (Bucur). 2013 Jan-Feb;108(1):99-101. | PubMed | Solé C, Rojas S, Vives JP, Sanz E. Tension gastrothorax mimicking acute coronary syndrome and causing cardiac arrest. Eur Heart J. 2014 Mar;35(12):794. | CrossRef | PubMed |
Solé C, Rojas S, Vives JP, Sanz E. Tension gastrothorax mimicking acute coronary syndrome and causing cardiac arrest. Eur Heart J. 2014 Mar;35(12):794. | CrossRef | PubMed | Gagg JW, Savva A. Tension gastrothorax: a rare cause of breathlessness. Emerg Med J. 2013 Jun;30(6):500. | CrossRef |
Gagg JW, Savva A. Tension gastrothorax: a rare cause of breathlessness. Emerg Med J. 2013 Jun;30(6):500. | CrossRef | de Jager CP, Trof RJ. Images in clinical medicine. Gastrothorax simulating acute tension pneumothorax. N Engl J Med. 2004 Aug 5;351(6):e5. | PubMed |
de Jager CP, Trof RJ. Images in clinical medicine. Gastrothorax simulating acute tension pneumothorax. N Engl J Med. 2004 Aug 5;351(6):e5. | PubMed | Bamgbade OA. Management of tension gastrothorax. Resuscitation. 2006 Aug;70(2):293-4. Epub 2006 Jul 10. | PubMed |
Bamgbade OA. Management of tension gastrothorax. Resuscitation. 2006 Aug;70(2):293-4. Epub 2006 Jul 10. | PubMed | How C, Tee A, Quah J. Delayed presentation of gastrothorax masquerading as pneumotho-rax. Prim Care Respir J. 2007 Feb;16(1):54–6. | PubMed |
How C, Tee A, Quah J. Delayed presentation of gastrothorax masquerading as pneumotho-rax. Prim Care Respir J. 2007 Feb;16(1):54–6. | PubMed | Dear C, Woodgate A, Ball J. Tension gastrothorax presenting with dramatic ECG changes. Anaesthesia. 2012 Nov;67(11):1280-1. | CrossRef | PubMed |
Dear C, Woodgate A, Ball J. Tension gastrothorax presenting with dramatic ECG changes. Anaesthesia. 2012 Nov;67(11):1280-1. | CrossRef | PubMed | McLaughlin K, Miller D, Currie GP. Iatrogenic gastrothorax mimicking a pneumothorax. QJM. 2009 Feb;102(2):149-50. | CrossRef | PubMed |
McLaughlin K, Miller D, Currie GP. Iatrogenic gastrothorax mimicking a pneumothorax. QJM. 2009 Feb;102(2):149-50. | CrossRef | PubMed | Pilate SA, De Clercq S. Tension pneumothorax and life saving diaphragmatic rupture: a case report and review of the literature. World J Emerg Surg. 2011 Aug 1;6:23. | CrossRef | PubMed |
Pilate SA, De Clercq S. Tension pneumothorax and life saving diaphragmatic rupture: a case report and review of the literature. World J Emerg Surg. 2011 Aug 1;6:23. | CrossRef | PubMed | Sharma R, Rosha D, Dash SK, Chand T. Tension Gastrothorax Complicating Third Trimester of Pregnancy: Suspicion is the Key. J Clin Imaging Sci. 2012;2:49. | CrossRef | PubMed |
Sharma R, Rosha D, Dash SK, Chand T. Tension Gastrothorax Complicating Third Trimester of Pregnancy: Suspicion is the Key. J Clin Imaging Sci. 2012;2:49. | CrossRef | PubMed | Ng J, Rex D, Sudhakaran N, Okoye B, Mukhtar Z. Tension gastrothorax in children: introduc-ing a management algorithm. J Pediatr Surg. 2013 Jul;48(7):1613-7. | CrossRef | PubMed |
Ng J, Rex D, Sudhakaran N, Okoye B, Mukhtar Z. Tension gastrothorax in children: introduc-ing a management algorithm. J Pediatr Surg. 2013 Jul;48(7):1613-7. | CrossRef | PubMed | Misiakos EP, Machairas A, Patapis P, Liakakos T. Laparoscopic ventral hernia repair: pros and cons compared with open hernia repair. JSLS. 2008 Apr-Jun;12(2):117-25. | PubMed |
Misiakos EP, Machairas A, Patapis P, Liakakos T. Laparoscopic ventral hernia repair: pros and cons compared with open hernia repair. JSLS. 2008 Apr-Jun;12(2):117-25. | PubMed |