 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: Balo’s concentric sclerosis, demyelination, tractography, magnetic resonance imaging, diffusion tensor imaging
Balo concentric sclerosis is an infrequent variant of a demyelinating disease related to multiple sclerosis, initially thought to have an acute presentation and a fatal outcome. Recent studies have reported non-fatal forms of Balo concentric sclerosis, focusing on the importance of early diagnosis using magnetic resonance imaging (MRI), along with spectroscopy and diffusion/perfusion sequences. Recently, we have been able to draw a three-dimensional image of a specific bundle of fibers by means of a diffusion tensor technique of the magnetic resonance imaging tractography (t-MRI). We report the case of a young woman presenting with acute and progressive focal neurological symptoms, including right body paresis, whose diagnosis was suggested by MRI and confirmed by pathology to be Balo concentric sclerosis. She was treated with boluses of methylprednisolone, achieving full neurological remission one year after admission. This is, to our knowledge, the first report describing the use of t-MRI for diagnosing BCS. We consider that t-MRI will allow, in a near future, early diagnosis of the disease, its prompt treatment, and establishing new classification criteria. This case confirms the existence of benign forms of Balo concentric sclerosis with a good response to steroid therapy, where functional recovery is possible.
In 1928, Joseph Balo described the “concentric periaxial sclerosis”, a variant of demyelinating diseases histologically characterized by multiple white matter lesions with a concentric demyelination and areas of focal necrosis, which is now known as Balo’s concentric sclerosis [1].
Initially, it was considered as a severe variant of multiple sclerosis [2],[3]. Nowadays they are accepted as related entities with substantial differences, such as the specific pattern of demyelination and the, in some cases, curable nature of Balo concentric sclerosis [4],[5]. There are less than 100 reported cases of Balo’s concentric sclerosis in the medical literature [2],[6].
Magnetic resonance imaging (MRI) is a procedure by which we can identify demyelinating lesions in the central nervous system, with already well defined diagnostic criteria (Table 1) [7]. Magnetic resonance imaging tractography (t-MRI) using diffusion tensor imaging, is the only non-invasive technique that allows in vivo dissection of white matter fibers. This technique constitutes and important complement to conventional MRI, since it allows for the study of projection, association and commissural fibers [8].
|
Table 1: Findings in skull magnetic resonance imaging for demyelinating lesions *
We present the case of a young woman with an acute neurological illness, in whom the brain magnetic resonance imaging adding t-MRI favored the early diagnosis of Balo concentric sclerosis previous to the biopsy. Likewise, we offer a discussion on the new clinical concepts and prognosis of the disease.
A 27-year-old woman with no previous disease, presents with a 2-day history of difficulty for fine movements and loss of strength in her right hand. Twenty-four hours later, while practicing sports, she suffered from loss of dorsiflexion strength in her lower right limb, along with clumsy, slow movements. She comes to the Emergency Department of Medica Sur Hospital, where a neurological assessment showed a muscle strength of 4/5 in her right limbs, with normal reflexes and no Babinski sign.
She was admitted and a magnetic resonance imaging was performed, showing a left capsulo-putaminal, ovoid lesion, which was hyperintense on T2, FLAIR and diffusion weighted images, and hypointense on T1. The lesion presented ring enhancement after the administration of gadolinium contrast (Figure 1). Magnetic resonance imaging spectroscopy and perfusion weighted imaging where not compatible with infectious or neoplastic disease [9].
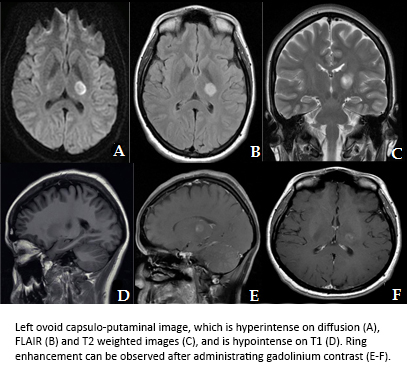
Figure 1. Brain magnetic resonance imaging (MRI).
We decided to perform t-MRI to complement the diagnosis, and we observed vertical changes in the corticospinal tract at the level of the lateral ventricles, due to the destruction of myelin sheaths. Multiple fibers were disrupted at the level of the left capsulo-putaminal ovoid lesion (Figure 2). A lumbar puncture was performed, which showed no cyto-chemical abnormalities, and was negative for tuberculosis, HIV, cryptococcus, herpes virus, and oligoclonal bands.
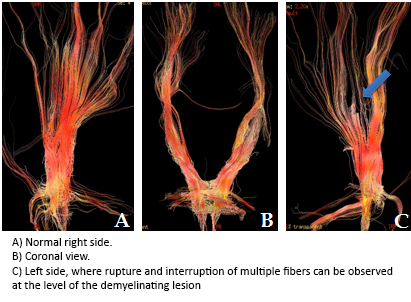
Figure 2. Diffusion tensor tractography with 3D reconstruction of the corticospinal tract.
At her third admission day finger extension was impossible in the right hand, and she also started presenting right central facial paresis. A brain biopsy for the lesion was performed because of this presentation, and the histopathological evaluation reported important demyelination with relative preservation of axons, mild perivascular lymphocyte infiltration with a few plasma cells, loss of astrocytes and phagocytosis of cellular debris and fragmented myelin. Atypical astrocytes with abnormal chromatin were focally observed, suggesting the presence of “Creutzfeldt astrocytes” (Figure 3).
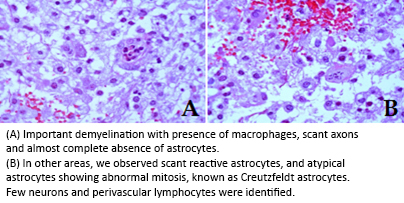
Figure 3. Histopathology.
Methylprednisolone bolus treatment was initiated at a charging dose of 30 mg/kg every 6 hours for two days, which caused an important recovery of function. She was discharged after 13 days from admission, in a good general condition and a score of 1 in the Rankin Outcome Scale. A follow-up visit after one year showed full clinical recovery and no further lesions on MRI.
Balo concentric sclerosis is a rare demyelinating disease that is more common between 20 and 50 years of age, and with a higher prevalence in Asian population [4]. It is characterized by focal concentric demyelination in the central nervous system, with a specific “onion skin” pattern [3],[6]. In the first reports of the disease the definitive diagnosis was made after the autopsy, and it was considered an acute and lethal entity [2]. Balo concentric sclerosis was initially thought to be a malignant variant of MS, similar to the Marburg variant [4]. At the same time, it was considered an early form of demyelination in which the lamellated lesions further evolved into a classic multiple sclerosis demyelinating plaque [4],[5]. With the help of magnetic resonance imaging in the daily practice, an early diagnosis of this disease has been achieved, after finding typical imaging patterns, which has allowed its classification as a separate and independent disease [2],[4],[10].
Microscopically, Balo concentric sclerosis presents with axonal changes similar to the ones observed during hypoxia, and some apoptotic changes have been demonstrated in the oligodendrocytes in the demyelinating layer [10]. At the border of these layers and also in the healthy tissue inside the lesion, increased expression of heat shock protein 70 (HSP-70) and hypoxia induced factor-alpha (HIF-1α) has been observed, and these molecules are known for their cytoprotective function in low oxygen conditions [10],[11]. This tissue pre-conditioning allows neurons to probably adapt to demyelinating lesions, which explains the existence of healthy tissue layers between the affected ones [11]. There is still no explanation to why the demyelinating axons have a similar histological appearance to hypoxic axons.
The clinical presentation of Balo concentric sclerosis is that of a subacute encephalopathy with focal neurological symptoms in young patients, including minor disturbances of cognition and behavior that can have a progressive evolution and even become fatal [6],[12]. Similar to the clinical evolution of our case, two recent reports of young patients with subacute disease, where the diagnosis of Balo concentric sclerosis was made by MRI, adequately responded to treatment with intravenous glucocorticoids [13],[14]. Unlike our report, where confirmation biopsy was performed, previously reported cases did not have histopathological analysis. Considering these differences in the clinical course of the disease it is possible to assume three different types of Balo concentric sclerosis: acute and self-limiting, relapsing-remitting variant, and rapidly progressive primary disease [5],[12].
Conventional tomography in Balo concentric sclerosis shows hypodense and homogeneous images on the site of the lesion, which initially suggests neoplastic or infectious processes [3]. Magnetic resonance imaging can identify demyelinating plaques, and, as in our case, a pattern of irregular concentric rings, which correspond to areas of demyelination interspersed with normal tissue, which is considered pathognomonic ("onion skin"). T2 weighted sequences show alternating patches of hyperintense demyelination with isointense unaffected areas, while T1 sequences show hypointense demyelinating rings, and the lesions present ring-enhancement after gadolinium administration [12],[15].
Magnetic resonance spectroscopy allows for the ruling out of brain tumors or abscesses. Metabolic abnormalities in Balo concentric sclerosis are similar to those seen in MS, including decreased N-acety-aspartate/creatinine ratio, increased choline/creatinine ratio, and peaks of lactate [16],[17]. There is also increased myo-inositol, while levels of N-acetyl-aspartate and choline are initially low and increase progressively as the disease remits [18]. Interestingly, in our case we did not observe this phenomenon. Being choline an important component of the myelin sheath, it is assumed that its elevation indicates demyelination [16],[17].
Advanced techniques of magnetic resonance imaging weighting are useful to support the diagnosis of Balo concentric sclerosis. The presence of hyperintensity on diffusion weighted imaging suggests cytotoxic edema and ischemia pattern, which may also occasionally be seen in MS. Unlike hyperintensity by ischemia, the image in Balo concentric sclerosis remains for a longer period of four to five weeks, in the cases reported [5],[12].
Diffusion sequenced images can show that demyelination follows a centrifugal pattern [12],[18]. One recent study analyzed the perfusion weighted pattern, in which a decreased perfusion from the center to the periphery was observed. The authors suggest that there is a deep venous vessel at the center of the lesion [19].
The use of t-MRI allows the visualization of white matter tracts in a multidimensional way, and assess their integrity [8],[20]. Undamaged and organized fascicles spread their water content unidirectionally, and this is detected by the computer for graphic reconstructions of the tracts, while regions with neuronal injury, axonal or demyelination present an alteration in the direction of diffusion of water, producing an abnormal image in t-IRM [19],[20]. In our case, the use of this technique revealed the disappearance of multiple myelin sheaths in the area of the injury, after observing intermittent interruption of corticospinal tract at the level of the internal capsule (Figure 2). This is one of the strongest points in our case presentation, since we were able to determine the location and size of the lesion using this technique, which was later confirmed by biopsy.
Previously, the definitive diagnosis was made during the autopsy. Today, with the new techniques of neuroimaging, early detection of the disease is possible, and it allows for stereotactic biopsy confirmation of the diagnosis, as was performed in our patient. However often the size or location of the biopsy is insufficient to visualize the characteristic alternating pattern part, when compared to that obtained with autopsy [12]. Use of Luxol Fast Blue (LFB), a specific staining for myelin in optical microscopy, shows dark blue bands in areas where the tissue is intact, while areas of demyelination are not stained, or stain pink if hematoxylin-eosin is also applied, because the existing hypercellularity in this tissue, where reactive astrocytosis, foamy macrophages, and perivascular lymphocytic infiltration can be seen [17],[18].
The presence of astrocytes with multiple enlarged fragmented nuclei and mitotic granular pattern, called Creutzfeldt astrocytes, is typical of demyelinating plaques of both Balo concentric sclerosis and multiple sclerosis [21]. By using the Bielschowsky silver stain, a relative preservation of axons in the lesion can be demonstrated [12]. Immunohistochemistry identifies perivascular lymphocytes as T cells positive for CD3 and CD8, and multiple macrophages and microglia positive to KiM1P [18]. In the case presented, we decided to perform a brain biopsy when in doubt, allowing for an accurate diagnosis, and complete clinical and imaging remission after a year of follow-up was achieved. In previously reported cases, the size of the lesions was not associated with clinical outcome [12].
Similar to what has been described in recent reports, our case is a nonfatal form of Balo concentric sclerosis, with a good response to early treatment with steroids. In this report, in addition to demonstrating the clinical, pathological and classical radiological findings, we include spectroscopy analysis of diffusion-weighted sequences and is one of the few published cases that reports a perfusion study.
We also believe, as an original contribution, the description and utility of the t-MRI for early diagnosis and treatment of this entity, as a technology that adds information to consider in the future different clinical forms of the Balo concentric sclerosis.
This is, to our knowledge, the first case of Balo concentric sclerosis in which a histopathological study correlates with the findings in the t-IRM. We also highlight the importance of early detection of the disease by this mean, and how it can assist in preventing a fatal outcome in a potentially curable entity.
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The images published in this article are owned by the hospital where they were obtained (Fundación Clínica Médica Sur) and were provided by the coauthors of the manuscript to enrich the description of the case and diagnostic techniques used.
Conflicts of interests
The authors completed the ICMJE conflict of interest declaration form translated into Spanish by Medwave. They declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Balo concentric sclerosis is an infrequent variant of a demyelinating disease related to multiple sclerosis, initially thought to have an acute presentation and a fatal outcome. Recent studies have reported non-fatal forms of Balo concentric sclerosis, focusing on the importance of early diagnosis using magnetic resonance imaging (MRI), along with spectroscopy and diffusion/perfusion sequences. Recently, we have been able to draw a three-dimensional image of a specific bundle of fibers by means of a diffusion tensor technique of the magnetic resonance imaging tractography (t-MRI). We report the case of a young woman presenting with acute and progressive focal neurological symptoms, including right body paresis, whose diagnosis was suggested by MRI and confirmed by pathology to be Balo concentric sclerosis. She was treated with boluses of methylprednisolone, achieving full neurological remission one year after admission. This is, to our knowledge, the first report describing the use of t-MRI for diagnosing BCS. We consider that t-MRI will allow, in a near future, early diagnosis of the disease, its prompt treatment, and establishing new classification criteria. This case confirms the existence of benign forms of Balo concentric sclerosis with a good response to steroid therapy, where functional recovery is possible.
 Autores:
Juan Alberto Nader Kawachi[1], María de la Luz Andrade Magdaleno[1], Carlos Andrés Peñaherrera[2], Yeni Fernández De Lara[3], María Isabel Lavenant Borja[4]
Autores:
Juan Alberto Nader Kawachi[1], María de la Luz Andrade Magdaleno[1], Carlos Andrés Peñaherrera[2], Yeni Fernández De Lara[3], María Isabel Lavenant Borja[4]

Citación: Nader Kawachi JA, Andrade Magdaleno ML, Peñaherrera CA, Fernández De Lara Y, Lavenant Borja MI. Early diagnosis of Balo's concentric sclerosis by diffusion tensor tractography: a case report and literature review. Medwave 2016 Mar;16(2):e6401 doi: 10.5867/medwave.2016.02.6402
Fecha de envío: 8/1/2016
Fecha de aceptación: 1/3/2016
Fecha de publicación: 14/3/2016
Origen: no solicitado
Tipo de revisión: con revisión por tres pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Karaarslan E, Altintas A, Senol U, Yeni N, Dincer A, Bayindir C, et al. Baló's concentric sclerosis: clinical and radiologic features of five cases. AJNR Am J Neuroradiol. 2001 Aug;22(7):1362-7. | PubMed |
Karaarslan E, Altintas A, Senol U, Yeni N, Dincer A, Bayindir C, et al. Baló's concentric sclerosis: clinical and radiologic features of five cases. AJNR Am J Neuroradiol. 2001 Aug;22(7):1362-7. | PubMed | Pelzers E, Van Goethem JW, van den Hauwe L, Degryse HR, Geens K, Parizel PM. Baló's concentric sclerosis. JBR-BTR. 2008 May-Jun;91(3):108-9. | PubMed |
Pelzers E, Van Goethem JW, van den Hauwe L, Degryse HR, Geens K, Parizel PM. Baló's concentric sclerosis. JBR-BTR. 2008 May-Jun;91(3):108-9. | PubMed | Andrade-Ramos MA, Núñez-Velasco S, Chiquete E, Espejo Plasencia I, Riestra-Castañeda R, Vargas-Sánchez A, et al. Esclerosis concéntrica de Baló: Reporte de caso y revisión de la literatura. Rev Mex Neuroci. 2011; 12(4):210–5. | Link |
Andrade-Ramos MA, Núñez-Velasco S, Chiquete E, Espejo Plasencia I, Riestra-Castañeda R, Vargas-Sánchez A, et al. Esclerosis concéntrica de Baló: Reporte de caso y revisión de la literatura. Rev Mex Neuroci. 2011; 12(4):210–5. | Link | Barun B, Adamec I, Habek M. Baló's concentric sclerosis in multiple sclerosis. Intern Med. 2012;51(15):2065-6. Epub 2012 Aug 1. | PubMed |
Barun B, Adamec I, Habek M. Baló's concentric sclerosis in multiple sclerosis. Intern Med. 2012;51(15):2065-6. Epub 2012 Aug 1. | PubMed | Hernández-Clares R, Di Capua D, Bartolomé M, de Las Heras V, Arroyo R. Balo's concentric sclerosis. Neurologia. 2011 Mar;26(2):125-7. | CrossRef | PubMed |
Hernández-Clares R, Di Capua D, Bartolomé M, de Las Heras V, Arroyo R. Balo's concentric sclerosis. Neurologia. 2011 Mar;26(2):125-7. | CrossRef | PubMed | Rovira A, Tintoré M, Alvarez-Cermeño JC, Izquierdo G, Prieto JM. [Recommendations for using and interpreting magnetic resonance imaging in multiple sclerosis]. Neurologia. 2010 May;25(4):248-65. | PubMed |
Rovira A, Tintoré M, Alvarez-Cermeño JC, Izquierdo G, Prieto JM. [Recommendations for using and interpreting magnetic resonance imaging in multiple sclerosis]. Neurologia. 2010 May;25(4):248-65. | PubMed | Recio Rodríguez M, Hernández Aceituno D, Hernández González LC, Martínez de Vega Fernández V, Carrascoso J. [3T tractography imaging: anatomy and clinical applications]. Radiologia. 2013 Jan-Feb;55(1):57-68. | CrossRef | PubMed |
Recio Rodríguez M, Hernández Aceituno D, Hernández González LC, Martínez de Vega Fernández V, Carrascoso J. [3T tractography imaging: anatomy and clinical applications]. Radiologia. 2013 Jan-Feb;55(1):57-68. | CrossRef | PubMed | Aguilar López R, Ibarra de la Torre A, Silva Morales F, Trujillo Ojeda HM. Abscesos cerebrales supra-e infratentoriales: resultados del tratamiento quirúrgico. Arch Neurocienc. 2006; 11(4):271-6. | Link |
Aguilar López R, Ibarra de la Torre A, Silva Morales F, Trujillo Ojeda HM. Abscesos cerebrales supra-e infratentoriales: resultados del tratamiento quirúrgico. Arch Neurocienc. 2006; 11(4):271-6. | Link | García Domínguez JM, Guzmán de Villoria Lebiedziejewski J. Catástrofes neurológicas por enfermedades desmielinizantes. Neurología. 2010;25(Supl 1):30-36. | Link |
García Domínguez JM, Guzmán de Villoria Lebiedziejewski J. Catástrofes neurológicas por enfermedades desmielinizantes. Neurología. 2010;25(Supl 1):30-36. | Link | Stadelmann C, Ludwin S, Tabira T, Guseo A, Lucchinetti CF, Leel-Ossy L, et al. Tissue preconditioning may explain concentric lesions in Baló's type of multiple sclerosis. Brain. 2005 May;128(Pt 5):979-87. | PubMed |
Stadelmann C, Ludwin S, Tabira T, Guseo A, Lucchinetti CF, Leel-Ossy L, et al. Tissue preconditioning may explain concentric lesions in Baló's type of multiple sclerosis. Brain. 2005 May;128(Pt 5):979-87. | PubMed | Darke M, Bahador FM, Miller DC, Litofsky NS, Ahsan H. Baló's concentric sclerosis: imaging findings and pathological correlation. J Radiol Case Rep. 2013 Jun 1;7(6):1-8.
| CrossRef | PubMed |
Darke M, Bahador FM, Miller DC, Litofsky NS, Ahsan H. Baló's concentric sclerosis: imaging findings and pathological correlation. J Radiol Case Rep. 2013 Jun 1;7(6):1-8.
| CrossRef | PubMed | Wengert O, Siebert E. Images in clinical medicine. Baló's concentric sclerosis. N Engl J Med. 2011 Aug 25;365(8):742. | CrossRef | PubMed |
Wengert O, Siebert E. Images in clinical medicine. Baló's concentric sclerosis. N Engl J Med. 2011 Aug 25;365(8):742. | CrossRef | PubMed | Grooters GS, Visser LH, Barkhof F, van der Knaap MS, van Asseldonk JT. Mystery case: Baló concentric sclerosis. Neurology. 2013 Feb 12;80(7):e71-2;discussion e72. | CrossRef | PubMed |
Grooters GS, Visser LH, Barkhof F, van der Knaap MS, van Asseldonk JT. Mystery case: Baló concentric sclerosis. Neurology. 2013 Feb 12;80(7):e71-2;discussion e72. | CrossRef | PubMed | Caracciolo JT, Murtagh RD, Rojiani AM, Murtagh FR. Pathognomonic MR imaging findings in Balo concentric sclerosis. AJNR Am J Neuroradiol. 2001 Feb;22(2):292-3. | PubMed |
Caracciolo JT, Murtagh RD, Rojiani AM, Murtagh FR. Pathognomonic MR imaging findings in Balo concentric sclerosis. AJNR Am J Neuroradiol. 2001 Feb;22(2):292-3. | PubMed | Chen CJ. Serial proton magnetic resonance spectroscopy in lesions of Balò concentric sclerosis. J Comput Assist Tomogr. 2001 Sep-Oct;25(5):713-8.
| PubMed |
Chen CJ. Serial proton magnetic resonance spectroscopy in lesions of Balò concentric sclerosis. J Comput Assist Tomogr. 2001 Sep-Oct;25(5):713-8.
| PubMed | Kim MO, Lee SA, Choi CG, Huh JR, Lee MC. Balo's concentric sclerosis: a clinical case study of brain MRI, biopsy, and proton magnetic resonance spectroscopic findings. J Neurol Neurosurg Psychiatry. 1997 Jun;62(6):655-8. | PubMed |
Kim MO, Lee SA, Choi CG, Huh JR, Lee MC. Balo's concentric sclerosis: a clinical case study of brain MRI, biopsy, and proton magnetic resonance spectroscopic findings. J Neurol Neurosurg Psychiatry. 1997 Jun;62(6):655-8. | PubMed | Lindquist S, Bodammer N, Kaufmann J, König F, Heinze HJ, Brück W, Sailer M. Histopathology and serial, multimodal magnetic resonance imaging in a multiple sclerosis variant. Mult Scler. 2007 May;13(4):471-82. | PubMed |
Lindquist S, Bodammer N, Kaufmann J, König F, Heinze HJ, Brück W, Sailer M. Histopathology and serial, multimodal magnetic resonance imaging in a multiple sclerosis variant. Mult Scler. 2007 May;13(4):471-82. | PubMed | Ripellino P, Stecco A, Leone MA, Cantello R. Basic and advanced imaging of a case of Balò's concentric sclerosis. BMJ Case Rep. 2013 Jan 25;2013. pii: bcr2012008413. | CrossRef | PubMed |
Ripellino P, Stecco A, Leone MA, Cantello R. Basic and advanced imaging of a case of Balò's concentric sclerosis. BMJ Case Rep. 2013 Jan 25;2013. pii: bcr2012008413. | CrossRef | PubMed | Little DM, Holloway RG. Diffusion tensor imaging: scientific advance, clinical tool, or just a pretty picture? Neurology. 2007 Jan 2;68(1):9-10. | PubMed |
Little DM, Holloway RG. Diffusion tensor imaging: scientific advance, clinical tool, or just a pretty picture? Neurology. 2007 Jan 2;68(1):9-10. | PubMed |