 Para Descargar PDF debe Abrir sesión.
Para Descargar PDF debe Abrir sesión.
Palabras clave: bundle branch block, tachycardia, systolic heart failure, prognostic
A proper characterization of frequency-dependent bundle branch blocks can provide useful prognostic information in some clinical situations. Often, this physiological event may be due to an extensive damage of infrahisian system, which poses a high risk of developing advanced atrioventricular block requiring pacemaker implantation. We describe the case of a 62 year-old man with chronic ischemic heart disease who exhibited alternating tachycardia-dependent bundle branch block during stress test. We discuss the main prognostic implications of this unusual event in the context of systolic dysfunction.
Aberrant conduction (aberrancy) consists on the transient occurrence of a ventricular conduction disorder in the absence of previous bundle branch block (BBB), pre-excitation or drug effect. Physiologically, aberrant conduction occurs primarily by rate-dependent block [1].
Conduction velocity through specific myocardium depends on maximum slope and peak amplitude of phase 0; variables that are closely related with transmembrane potential before stimulation. If a cell of His-bundle or infrahisian tissue receives a premature stimulus during phase 3, then the transmembrane potential will be less negative, there will be fewer fast sodium channels available for activation and the slope of phase 0 will decrease, resulting in slower conduction during next activation. This physiological event is called phase 3 or tachycardia-dependent bundle branch block (BBB) [1]. From a morphological point of view, this phenomenon mainly adopts left bundle branch block pattern (LBBB) [2]. From an epidemiological point of view, the tachycardia-dependent bundle branch block is rarely observed in daily practice, with a prevalence of less than 0.5% during ECG exercise testing [3],[4],[5].
As permanent bundle branch block represents a marker of advanced coronary artery disease, it is easy to understand that prognosis in tachycardia-dependent bundle branch block will be worse in this heart disease, with an increased risk of hard events such as all-cause mortality, nonfatal myocardial infarction, need for percutaneous intervention or coronary bypass surgery, development of ventricular tachyarrhythmias and permanent bundle branch block [6]. In turn, this entity may manifest an extensive damage of infrahisian system at high risk of progression to advanced atrioventricular block and need for pacemaker implantation [6],[7],[8],[9],[10],[11].
We describe the case of a 62-years old man with chronic ischemic heart disease who exhibited alternating tachycardia-dependent bundle branch block during EKG stress test, discussing main prognostic implications of this unusual event in the context of systolic dysfunction.
A 62-year-old hypertensive man with chronic ischemic heart failure was controlled on an outpatient basis in the Multidisciplinary Heart Failure Unit, receiving optimal doses of carvedilol, furosemide, spironolactone, enalapril, aspirin and atorvastatin. The results of Doppler echocardiography were: left ventricular systolic diameter: 54 mm; septal thickness: 7 mm; left atrial area: 22 cm2; left ventricle ejection fraction: 30% (ellipsoid method); apical akinesia and septal dyskinesia with hypocontractility in the rest of left ventricle, mild mitral and tricuspid regurgitations. The patient was referred to EKG stress test to define the functional class of symptoms.
Exercise protocol
A progressive effort on a cycle ergometer (Astrand protocol) under surface 12-lead EKG and blood pressure monitoring during exercise and recovery until normalizing blood pressure and heart rate was performed. Written informed consent was provided before the test. At baseline the patient had a normal nutritional status and was eupneic. Heart auscultation: 65 bpm regular rate, normal sounds, apical murmur II/VI (Levine) with minimal axillary irradiation. Lung fields were clear and the rest of the examination was normal. Baseline EKG showed sinus rhythm and incomplete right bundle branch block (RBBB). Figure 1 shows ventricular conduction pattern at rest. Surface EKG tracing obtained before exercise (panel A) showed: 65 bpm sinus rhythm, PR interval = 190 ms, QRS duration = 110 ms, anterior scar, incomplete right bundle branch block (grade 1), signs of septoapical dyskinesia (black arrow), normal corrected QT interval. Panel (B) illustrates the pattern of conduction through His-Purkinje system, showing partially delayed conduction in right His bundle branch (yellow). Impulse conduction through left His bundle branch is shown in green.
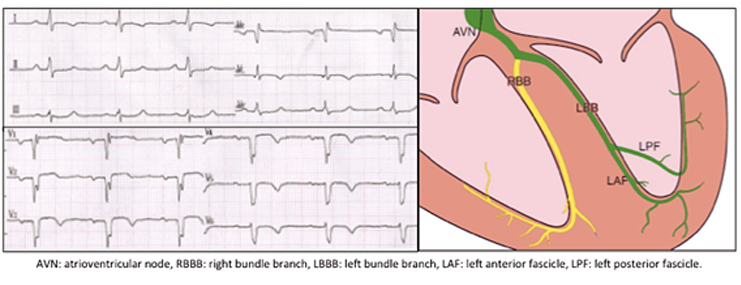
Figure 1. Ventricular conduction at baseline
The patient reached a maximum load of 600 kgmts during exercise (6.14 mets, NYHA functional class: IIA), referring tired legs and limiting dyspnea. Table 1 summarizes clinical and EKG data during stress test. During fifth minute of exercise (heart rate: 115 bpm) a complete left bundle branch block followed by varying degrees of delay in conduction through both His bundles was recorded (Figure 2).
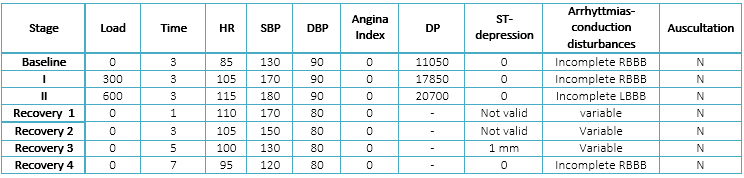
Table 1. Clinical and EKG data obtained during stress test and recovery (at baseline, during Astrand protocol and until seven minutes of recovery)
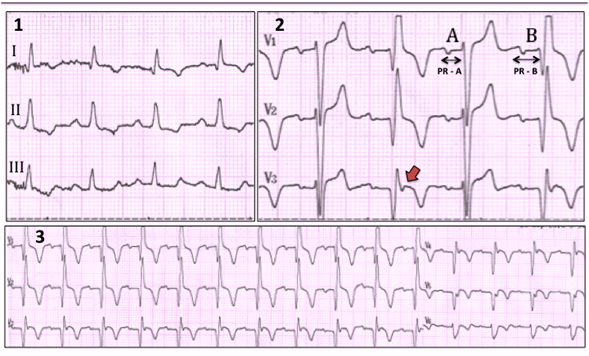
Figure 2. Ventricular conduction during recovery (first minute)
Figure 2 shows ventricular conduction during first minute of recovery. Conduction through right bundle branch was variable; slightly delayed with QR or Qr morphology (Part 1 of the diagram), adopting 2:1 sequence (Part 2 of diagram) or even severely delayed with complete and permanent right bundle branch block (Part 3 of diagram). In 2A right bundle branch conducted and in 2B it was delayed (2: 1 block in right bundle branch). PR interval in B (PR-B = 245 ms) was longer than in A (PR-A = 190 ms) since conduction was produced only through left bundle branch in B, always with first-degree block (see Figure 1). Reverse septal activation in A and B determined that large anterior non-activated myocardium would manifest as QR or qR morphology and signs of dyskinesia (red arrow).
The sequence of ventricular conduction during EKG stress test is summarized in Figure 3. Note that baseline ventricular conduction at a heart rate of 100 bpm was restored during recovery; reappearing with a longer cycle length which appeared in acceleration (360 ms vs. 315 ms, see Table 1). This situation is called "linking phenomenon" [11] and has been attributed to persistent concealed transeptal conduction during deceleration [12].
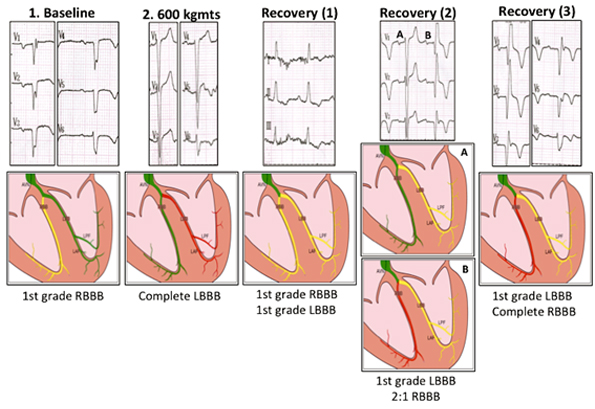
Figure 3. Evolution of ventricular conduction during EKG stress test
At the beginning of the exercise, delay of conduction through His left bundle branch was discrete (first degree), constant through right bundle branch (yellow) and constantly normal through left branch (green). During next stage (600 kmts), under the influence of circulating catecholamines, conduction through right bundle branch improved (green) and resulted in complete left bundle branch block morphology (left bundle branch in red). The delay observed in conduction through right bundle branch was variable in first minute of recovery; sometimes discrete (PE 1: right branch in yellow), sometimes in 2: 1 - Mobitz II sequence (PE 2 A: right bundle branch in green, PE 2 B: right bundle branch in red) and sometimes was complete and permanent (PE 3). So, severely altered conduction through both His bundles at different moments of EKG stress test (red) suggested an extensive damage of His-Purkinje system unmasked during exercise (see text).
Chronotropic response was adequate to treatment with beta-blockers. A Duke score of +5 conferred a moderate risk of major cardiovascular events in next 2 years.
Serial EKG records are required to diagnose a tachycardia-dependent bundle branch block, accurately detecting the exact moment when bundle branch block pattern appears, and then assuming that QRS complex is widened at some time immediately prior. Furthermore, the definition of conduction from the atria to ventricles requires all beats were preceded by similar P wave and PR interval to previous rhythm. These steps are essential for diagnosis.
Tachycardia-dependent bundle branch block is the most frequently observed paroxysmal aberrant conduction. Their clinical manifestations are highly variable, ranging from isolated fascicular block to complete atrioventricular block [13]. Bilateral His-Purkinje system disease can be manifested by alternant bundle branch block, an entity that includes bundle branch block pattern intermittently recorded in an isolated tracing or, as in this case, coexisting simultaneously in the same EKG [14],[15],[16],[17],[18],[19],[20],[21].
This phenomenon is often found in patients with advanced ischemic heart disease, extensive scar and/or bilateral degenerative fibrosis of ventricular conduction system at multiple levels [22],[23]. The more common alternating bundle branch block morphology is complete left bundle branch block alternating with normal ventricular conduction. Less commonly, complete right bundle branch block alternating with normal or incomplete right bundle branch block conduction is observed. The documented case of bilateral beat-to-beat bundle branch block alternation is an extremely unusual phenomenon.
Since first description published by Braun et al. in 1951 [17], literature has referred almost exclusively to reports of isolated cases exhibiting alternating bundle branch block [8],[10],[14],[18],[19],[20]. Wu et al. described nine cases of alternating bundle branch block evaluated by electrophysiological atrial pacing and hisian recordings [21]. Alternating bundle branch block occurrence was mostly associated with incomplete block in a bundle branch and sudden complete block in the other. While pathological specimens were not available, authors suggested that clinical course of alternating bundle branch block was mainly related to the severity of underlying heart disease and not to next development of advanced atrioventricular block.
It is clear that alternating bundle branch block phenomenon is a consequence of an extensive damage of infrahisian conduction system with potential high risk of progression to advanced atrioventricular block, both during myocardial infarction [22],[23] and stable chronic coronary disease [24],[25]. In our case, in wich alternating bundle branch block pattern was accompanied by a variable delay in atrioventricular conduction at baseline, progression to complete AV block is imminent [10],[24]. However, pacemaker implant in this clinical setting is still an indication based on anecdotal evidences, mostly reported during past decades. Current experts recommendations suggest to proceed with pacemaker implantation as soon as alternating bundle branch block is documented, even in the absence of previous syncope (class I recommendation, level of evidence C) [26].
In the few clinical cases with coronary artery disease and severe systolic dysfunction that develop alternating bundle branch block requiring pacemaker implantation it becomes very important to closely monitor clinical, electrocardiographic and functional outcomes after right ventricle stimulation and timely indicate the upgrade to biventricular pacing [26]. Otherwise, maintaining right ventricle endocardium stimulation could induce a worsening of symptoms and progressive deterioration of contractile function associated with interventricular and left ventricular dissynchrony [27].
In a small, placebo-controlled prospective trial Kanoupakis et al. examined the electrophysiological impacts of carvedilol treatment in 31 individuals with chronic systolic dysfunction (left ventricular ejection fraction: 26 + 8% in control group vs. 28 + 7% in carvedilol group) [33]. Researchers found that carvedilol prolonged the ventricular refractory period without significant changes in physiological parameters of repolarization as corrected QT interval or monophasic records in 90% of repolarization. Furthermore, changes in refractoriness were strongly correlated with left ventricular ejection fraction, suggesting that patients with better systolic function respond with greater physiological changes. However, this study only included patients with non-ischemic dilated cardiomyopathy who underwent a short period of carvedilol treatment. So, its findings cannot be extrapolated to our case. Even if these results were confirmed more widely, it is unlikely to have practical importance on usual drug therapy of chronic systolic dysfunction. Meanwhile, even in subjects with severe systolic dysfunction developing alternating bundle branch block, positive benefits of non-cardioselective β-blockers in terms of mortality, symptomatic improvement, ejection fraction and development of ventricular tachyarrhythmias widely exceed the risk of accelerated progression to advanced atrioventricular block [34],[35].
Bilateral alternating tachycardia-dependent bundle branch block is an exceptional finding. Its presentation in chronic coronary disease is a sign of extensive damage in ventricular conduction system at high risk of serious events including progression to advanced atrioventricular block requiring pacemaker implantation. Sometimes it also requires biventricular pacing. In individuals with permanent bundle branch block at baseline, EKG stress test may unmask an exacerbation of these changes in the form of tachycardia-dependent aberrant conduction alternating different morphologies, a situation that takes immediate prognostic and therapeutic relevance.
From the editor
This article was originally submitted in Spanish and was translated into English by the authors. The Journal has not copyedited this version.
Ethical aspects
The Editorial Board of Medwave considered the data included in this report do not disclose patient's identity, thus written informed consent was unnecessary.
Acknowledgements
The authors wish to thank Dr. José Carlos Pachón Mateos (PhD) for his valuable contributions to the review of ECG tracings.
Declaration of conflicts of interest
The authors completed the conflict of interests declaration form from the ICMJE and declared not having any conflict of interests with the matter dealt herein. Forms can be requested from the responsible author or the editors.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

A proper characterization of frequency-dependent bundle branch blocks can provide useful prognostic information in some clinical situations. Often, this physiological event may be due to an extensive damage of infrahisian system, which poses a high risk of developing advanced atrioventricular block requiring pacemaker implantation. We describe the case of a 62 year-old man with chronic ischemic heart disease who exhibited alternating tachycardia-dependent bundle branch block during stress test. We discuss the main prognostic implications of this unusual event in the context of systolic dysfunction.
 Autores:
Federico Ferrando-Castagnetto[1], Alejandro Vidal[1], Roberto Ricca-Mallada[1], Romina Nogara[1], Pablo Marichal[1], Fabián Martínez[1]
Autores:
Federico Ferrando-Castagnetto[1], Alejandro Vidal[1], Roberto Ricca-Mallada[1], Romina Nogara[1], Pablo Marichal[1], Fabián Martínez[1]

Citación: Ferrando-Castagnetto F, Vidal A, Ricca-Mallada R, Nogara R, Marichal P, Martínez F. Tachycardia-dependent bilateral bundle branch block in ischemic heart disease with systolic dysfunction: case report and review of prognostic implications. Medwave 2015 Oct;15(9):e6285 doi: 10.5867/medwave.2015.09.6285
Fecha de envío: 20/7/2015
Fecha de aceptación: 6/10/2015
Fecha de publicación: 16/10/2015
Origen: no solicitado
Tipo de revisión: con revisión por dos pares revisores externos, a doble ciego

Nos complace que usted tenga interés en comentar uno de nuestros artículos. Su comentario será publicado inmediatamente. No obstante, Medwave se reserva el derecho a eliminarlo posteriormente si la dirección editorial considera que su comentario es: ofensivo en algún sentido, irrelevante, trivial, contiene errores de lenguaje, contiene arengas políticas, obedece a fines comerciales, contiene datos de alguna persona en particular, o sugiere cambios en el manejo de pacientes que no hayan sido publicados previamente en alguna revista con revisión por pares.
Aún no hay comentarios en este artículo.
Para comentar debe iniciar sesión
 Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
Medwave publica las vistas HTML y descargas PDF por artículo, junto con otras métricas de redes sociales.
 Issa Z, Miller JM, Zipes DP. Intraventricular conduction abnormalities. In: Clinical arrhytmology and electrophysiologiy: a COMPANION to Braunwald`s heart disease. 1st ed. Phildadelfia, PA: Elsevier;2009: 143-46.
Issa Z, Miller JM, Zipes DP. Intraventricular conduction abnormalities. In: Clinical arrhytmology and electrophysiologiy: a COMPANION to Braunwald`s heart disease. 1st ed. Phildadelfia, PA: Elsevier;2009: 143-46.  Chilson DA, Zipes DP, Heger JJ, Browne KF, Prystowsky EN. Functional bundle branch block: discordant response of right and left bundle branches to changes in heart rate. Am J Cardiol. 1984 Aug 1;54(3):313-6. | PubMed |
Chilson DA, Zipes DP, Heger JJ, Browne KF, Prystowsky EN. Functional bundle branch block: discordant response of right and left bundle branches to changes in heart rate. Am J Cardiol. 1984 Aug 1;54(3):313-6. | PubMed | Aoki T, Nishikawa H, Motoyasu M, Shimizu Y, Ono N, Unno M, Kakuta Y, Konishi T, Nakano T. [Exercise-induced left bundle branch block in treadmill exercise test: clinical significance and prognosis]. Kokyu To Junkan. 1992 Aug;40(8):797-804. | PubMed |
Aoki T, Nishikawa H, Motoyasu M, Shimizu Y, Ono N, Unno M, Kakuta Y, Konishi T, Nakano T. [Exercise-induced left bundle branch block in treadmill exercise test: clinical significance and prognosis]. Kokyu To Junkan. 1992 Aug;40(8):797-804. | PubMed | Bounhoure JP, Donzeau JP, Doazan JP, Queyreau JM, Galinier M, Estrabaud M, et al. [Complete bundle branch block during exercise test. Clinical and coronary angiographic data]. Arch Mal Coeur Vaiss. 1991 Feb;84(2):167-71. | PubMed |
Bounhoure JP, Donzeau JP, Doazan JP, Queyreau JM, Galinier M, Estrabaud M, et al. [Complete bundle branch block during exercise test. Clinical and coronary angiographic data]. Arch Mal Coeur Vaiss. 1991 Feb;84(2):167-71. | PubMed | Stein R, Ho M, Oliveira CM, Ribeiro JP, Lata K, Abella J, et al. Exercise-induced left bundle branch block: prevalence and prognosis. Arq Bras Cardiol. 2011 Jul;97(1):26-32. | PubMed |
Stein R, Ho M, Oliveira CM, Ribeiro JP, Lata K, Abella J, et al. Exercise-induced left bundle branch block: prevalence and prognosis. Arq Bras Cardiol. 2011 Jul;97(1):26-32. | PubMed | Grady TA, Chiu AC, Snader CE, Marwick TH, Thomas JD, Pashkow FJ, et al. Prognostic significance of exercise-induced left bundle-branch block. JAMA. 1998 Jan 14;279(2):153-6. | PubMed |
Grady TA, Chiu AC, Snader CE, Marwick TH, Thomas JD, Pashkow FJ, et al. Prognostic significance of exercise-induced left bundle-branch block. JAMA. 1998 Jan 14;279(2):153-6. | PubMed | Candell Riera J, Oller Martínez G, Vega J, Gordillo E, Ferreira I, Peña C, et al. [Exercise-induced left bundle-branch block in patients with coronary artery disease versus patients with normal coronary arteries]. Rev Esp Cardiol. 2002 May;55(5):474-80. | PubMed |
Candell Riera J, Oller Martínez G, Vega J, Gordillo E, Ferreira I, Peña C, et al. [Exercise-induced left bundle-branch block in patients with coronary artery disease versus patients with normal coronary arteries]. Rev Esp Cardiol. 2002 May;55(5):474-80. | PubMed | Mitręga K, Lenarczyk R, Pruszkowska P, Kalarus Z, Sredniawa B. Alternating left and right bundle branch block. Kardiol Pol. 2014;72(10):987. | CrossRef | PubMed |
Mitręga K, Lenarczyk R, Pruszkowska P, Kalarus Z, Sredniawa B. Alternating left and right bundle branch block. Kardiol Pol. 2014;72(10):987. | CrossRef | PubMed | Wu D, Denes P, Dhingra RC, Amat-y-Leon F, Wyndham CR, Chuquimia R, Rosen KM. Electrophysiological and clinical observations in patients with alternating bundle branch block. Circulation 1976;3:456-464. | PubMed |
Wu D, Denes P, Dhingra RC, Amat-y-Leon F, Wyndham CR, Chuquimia R, Rosen KM. Electrophysiological and clinical observations in patients with alternating bundle branch block. Circulation 1976;3:456-464. | PubMed | Massumi R. Alternating bundle branch block together with alternation of PR intervals: advanced Mobitz II atrioventricular block. Rev Cardiovasc Med. 2010 Winter;11(1):44-52. | PubMed |
Massumi R. Alternating bundle branch block together with alternation of PR intervals: advanced Mobitz II atrioventricular block. Rev Cardiovasc Med. 2010 Winter;11(1):44-52. | PubMed | Rosenbaum MB, Elizari MV, Lázzari JO, Halpern MS, Nau GJ. Bilateral bundle branch block: its recognition and significance. Cardiovasc Clin.
1971;2(3):151-79. | PubMed |
Rosenbaum MB, Elizari MV, Lázzari JO, Halpern MS, Nau GJ. Bilateral bundle branch block: its recognition and significance. Cardiovasc Clin.
1971;2(3):151-79. | PubMed | Maury P, Duparc A, Hébrard A, Mondoly P, Rollin A, Delay M. Reverse left septal activation during intermittent left bundle-branch block: indirect proof for concealed retrograde left bundle-branch activation. J Electrocardiol. 2009 Nov-Dec;42(6):671-3. | CrossRef | PubMed |
Maury P, Duparc A, Hébrard A, Mondoly P, Rollin A, Delay M. Reverse left septal activation during intermittent left bundle-branch block: indirect proof for concealed retrograde left bundle-branch activation. J Electrocardiol. 2009 Nov-Dec;42(6):671-3. | CrossRef | PubMed | Josephson ME: Intraventricular conduction disturbances. In: Josephson ME (ed): Clinical Cardiac Electrophysiology, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2004:110-139.
Josephson ME: Intraventricular conduction disturbances. In: Josephson ME (ed): Clinical Cardiac Electrophysiology, 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2004:110-139.  Rosenbaum MB, Lepeschkin E. Bilateral bundle branch block. Am Heart J. 1955 Jul;50(1):38-61. | PubMed |
Rosenbaum MB, Lepeschkin E. Bilateral bundle branch block. Am Heart J. 1955 Jul;50(1):38-61. | PubMed | Lepeschkin E. The electrocardiographic diagnosis of bilateral bundle branch block in relation to heart block. Prog Cardiovasc Dis. 1964 Mar;6:445-71. | PubMed |
Lepeschkin E. The electrocardiographic diagnosis of bilateral bundle branch block in relation to heart block. Prog Cardiovasc Dis. 1964 Mar;6:445-71. | PubMed | Lenegre J. Etiology and pathology of bilateral bundle branch block in relation to complete heart block. Prog Cardiovasc Dis 1964;6: 409. | PubMed |
Lenegre J. Etiology and pathology of bilateral bundle branch block in relation to complete heart block. Prog Cardiovasc Dis 1964;6: 409. | PubMed | Braun SE, Rabinovich NP. [Alternating bundle branch block in hypertension]. Ter Arkh. 1951 Sep-Oct;23(5):68-72. | PubMed |
Braun SE, Rabinovich NP. [Alternating bundle branch block in hypertension]. Ter Arkh. 1951 Sep-Oct;23(5):68-72. | PubMed | Wagenaar LJ, van Gelder IC, van Veldhuisen DJ. Alternating bundle branch block. Neth Heart J. 2002 May;10(5):250-251. | PubMed |
Wagenaar LJ, van Gelder IC, van Veldhuisen DJ. Alternating bundle branch block. Neth Heart J. 2002 May;10(5):250-251. | PubMed | Ho RT, Stopper M, Koka AR. Alternating bundle branch block. Pacing Clin Electrophysiol. 2012 Feb;35(2):223-6. | CrossRef | PubMed |
Ho RT, Stopper M, Koka AR. Alternating bundle branch block. Pacing Clin Electrophysiol. 2012 Feb;35(2):223-6. | CrossRef | PubMed | Fazzini PF, Marchi F, Pucci P. [Prognostic significance of the intraventricular blocks during acute myocardial infarction (author's transl)]. G Ital Cardiol. 1975;5(4):526-35. | PubMed |
Fazzini PF, Marchi F, Pucci P. [Prognostic significance of the intraventricular blocks during acute myocardial infarction (author's transl)]. G Ital Cardiol. 1975;5(4):526-35. | PubMed | Beck OA, Hochrein H. [Alternating and intermittent bilateral bundle-branch block in acute myocardial infarct with development of total atrioventricular block]. Z Kardiol. 1976 Mar;65(3):245-55. | PubMed |
Beck OA, Hochrein H. [Alternating and intermittent bilateral bundle-branch block in acute myocardial infarct with development of total atrioventricular block]. Z Kardiol. 1976 Mar;65(3):245-55. | PubMed | Ogura Y, Kato J, Ogawa Y, Shiokoshi T, Kitaoka T, Suzuki T, et al. A case of alternating bundle branch block in combination with intra-Hisian block. Int Heart J. 2005 Jul;46(4):737-44. | PubMed |
Ogura Y, Kato J, Ogawa Y, Shiokoshi T, Kitaoka T, Suzuki T, et al. A case of alternating bundle branch block in combination with intra-Hisian block. Int Heart J. 2005 Jul;46(4):737-44. | PubMed | Fisch C, Zipes DP, McHenry PL. Rate dependent aberrancy. Circulation. 1973 Oct;48(4):714-24. | PubMed |
Fisch C, Zipes DP, McHenry PL. Rate dependent aberrancy. Circulation. 1973 Oct;48(4):714-24. | PubMed | European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA), Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013 Aug;15(8):1070-118. | CrossRef | PubMed |
European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA), Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace. 2013 Aug;15(8):1070-118. | CrossRef | PubMed | Tops LF, Schalij MJ, Bax JJ. The effects of right ventricular apical pacing on ventricular function and dyssynchrony implications for therapy. J Am Coll Cardiol. 2009 Aug 25;54(9):764-76. | CrossRef | PubMed |
Tops LF, Schalij MJ, Bax JJ. The effects of right ventricular apical pacing on ventricular function and dyssynchrony implications for therapy. J Am Coll Cardiol. 2009 Aug 25;54(9):764-76. | CrossRef | PubMed | Jaillon P, Weissenburger J, Heckle J, Cheymol G. Effects of the beta-adrenergic blocking agents propranolol and timolol on canine cardiac refractory periods. Eur J Pharmacol. 1979 Oct 1;58(3):265-71. | PubMed |
Jaillon P, Weissenburger J, Heckle J, Cheymol G. Effects of the beta-adrenergic blocking agents propranolol and timolol on canine cardiac refractory periods. Eur J Pharmacol. 1979 Oct 1;58(3):265-71. | PubMed | Morady F, Kou WH, Nelson SD, de Buitleir M, Schmaltz S, Kadish AH, et al. Accentuated antagonism between beta-adrenergic and vagal effects
on ventricular refractoriness in humans. Circulation. 1988 Feb;77(2):289-97. | PubMed |
Morady F, Kou WH, Nelson SD, de Buitleir M, Schmaltz S, Kadish AH, et al. Accentuated antagonism between beta-adrenergic and vagal effects
on ventricular refractoriness in humans. Circulation. 1988 Feb;77(2):289-97. | PubMed | Euler DE, Scanlon PJ. Effect of propranolol on ventricular repolarization and refractoriness: role of beta-blockade versus direct membrane effects. Cardiovasc Drugs Ther. 1988 Mar;1(6):605-12. | PubMed |
Euler DE, Scanlon PJ. Effect of propranolol on ventricular repolarization and refractoriness: role of beta-blockade versus direct membrane effects. Cardiovasc Drugs Ther. 1988 Mar;1(6):605-12. | PubMed | Robinson C, Birkhead J, Crook B, Jennings K, Jewitt D. Clinical electrophysiological effects of atenolol--a new cardioselective beta-blocking agent. Br Heart J. 1978 Jan;40(1):14-21. | PubMed |
Robinson C, Birkhead J, Crook B, Jennings K, Jewitt D. Clinical electrophysiological effects of atenolol--a new cardioselective beta-blocking agent. Br Heart J. 1978 Jan;40(1):14-21. | PubMed | Naccarelli GV, Lukas MA. Carvedilol's antiarrhythmic properties: therapeutic implications in patients with left ventricular dysfunction. Clin Cardiol. 2005 Apr;28(4):165-73. | PubMed |
Naccarelli GV, Lukas MA. Carvedilol's antiarrhythmic properties: therapeutic implications in patients with left ventricular dysfunction. Clin Cardiol. 2005 Apr;28(4):165-73. | PubMed | Kanoupakis EM, Manios EG, Mavrakis HE, Kallergis EM, Lyrarakis GM, Koutalas EP, Vardas PE. Electrophysiological effects of carvedilol administration in patients with dilated cardiomyopathy. Cardiovasc Drugs Ther. 2008 Jun;22(3):169-76. | CrossRef | PubMed |
Kanoupakis EM, Manios EG, Mavrakis HE, Kallergis EM, Lyrarakis GM, Koutalas EP, Vardas PE. Electrophysiological effects of carvedilol administration in patients with dilated cardiomyopathy. Cardiovasc Drugs Ther. 2008 Jun;22(3):169-76. | CrossRef | PubMed | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):1810-52. | CrossRef | PubMed |
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):1810-52. | CrossRef | PubMed | Packer M, Fowler MB, Roecker EB, Coats AJ, Katus HA, Krum H, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002 Oct 22;106(17):2194-9. | PubMed |
Packer M, Fowler MB, Roecker EB, Coats AJ, Katus HA, Krum H, et al. Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study. Circulation. 2002 Oct 22;106(17):2194-9. | PubMed |