Key Words: Radiosurgery, brain oligometastases, lung cancer, Epistemonikos, GRADE.
Abstract
INTRODUCTION
Brain metastases are a common problem in oncology patients, especially in lung cancer. The usual treatment for cerebral oligometastases is whole brain radiation therapy. Given the persistent poor prognosis of this disease, other therapeutic alternatives such as stereotactic radiosurgery have been considered. However, there is no clarity regarding the effectiveness of its addition.
METHODS
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified 17 systematic reviews including seven studies overall, of which four were randomized trials. All trials assessed patients with brain oligometastases, but none of them included exclusively lung cancer population. We concluded that it is not possible to clearly establish whether radiosurgery decreases neurological functionality, cognitive impairment, mortality or serious adverse effects, as the certainty of the existing evidence has been assessed as very low.
Problem
Brain oligometastases are a common problem in oncology patients. It is usually defined by a limited number of metastases (less than five), placing it as an intermediate state between localized and metastatic cancer. This stage is associated with better prognosis, since it is possible to administer local treatment in addition to the systemic treatment of the disease. Within the histological origins we can find breast, kidney and colon cancer, among others, being the most frequent lung cancer.
The usual local treatment for cerebral oligometastases is the use of corticoids or whole brain radiotherapy and it is estimated that survival could vary between two and six months [1]. Given the persistent poor prognosis of this disease, other therapeutic alternatives such as stereotactic radiosurgery has been proposed, which allows the administration of higher doses of radiation in a localized area and may be more effective in the ablation of brain metastases. However, its indication is controversial, as it is not clear how effective can be its addition to systemic treatment or whole brain radiotherapy.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We identified 17 systematic reviews [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], including seven studies overall reported in eight references [19], [20], [21], [22], [23], [24], [25], [26], of which four were randomized trials reported in five references [19], [20], [21], [22], [26]. The table and summary are based on the randomized trials, as the observational studies did not increase the level of certainty of the evidence, nor added any additional relevant information. |
|
What types of patients were included* |
All trials included patients with a diagnosis of cerebral oligometastases, regardless of their primary histology. Only two trials reported the number of patients with primary lung cancer: in one trial it was 64% [19] and in another 44% [20]. Three trials included patients with one to three brain metastases [19], [21], [22], and one trial with two to four brain metastases [20]. Three trials excluded patients with a functionality below 70 points on the Karnofsky scale [19], [20], [21]. |
|
What types of interventions were included* |
All trials evaluated the addition of stereotactic radiosurgery to whole brain radiotherapy in comparison with whole brain radiotherapy alone. Regarding the doses used in the intervention, one trial reported that stereotactic radiosurgery was administered with doses between 14 to 20 Gy (average 14.6 Gy) [21]; one applied 20 Gy [22], another a 16 Gy dose [20], and one trial did not report the dose administered [19]. Only one trial specified the type of radiosurgery (Gamma knife) [22]. Regarding the comparison, three trials administered 30 Gy for the whole brain radiotherapy in 10 sessions [20], [21], [22]. One trial administered 37.5 Gy with a daily dose of 2.5 Gy [19]. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
The average follow-up of the trials was not reported. However, outcomes had a follow-up with a range between 3 to 18 months [19], [20], [21], [22]. |
*Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
Summary of findings
Information on the effects of stereotactic radiosurgery on brain oligometastases in lung cancer is based on four randomized trials involving 596 patients <a data-dropdown="drop19" href="#">[19]</a>, <a data-dropdown="drop20" href="#">[20]</a>, <a data-dropdown="drop21" href="#">[21]</a>.
Two trials evaluated mortality (358 patients) <a data-dropdown="drop19" href="#">[19]</a>, <a data-dropdown="drop20" href="#">[20]</a>. One trial evaluated the outcome neurological functionality (42 patients) <a data-dropdown="drop21" href="#">[21]</a>. One trial evaluated the outcomes cognitive deterioration (154 patients) <a data-dropdown="drop19" href="#">[19]</a> and acute and late serious adverse effects (326 patients) <a data-dropdown="drop19" href="#">[19]</a>. None of the systematic reviews reported the outcome quality of life.
The summary of findings is as follows:
- We are uncertain whether the addition of stereotactic radiosurgery reduces mortality as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces the deterioration of neurological functionality as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces cognitive deterioration as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces late serious adverse effects as the certainty of the evidence has been assessed as very low.
- We are uncertain whether the addition of stereotactic radiosurgery reduces acute serious adverse effects as the certainty of the evidence has been assessed as very low.
- No studies were found that looked at quality of life.
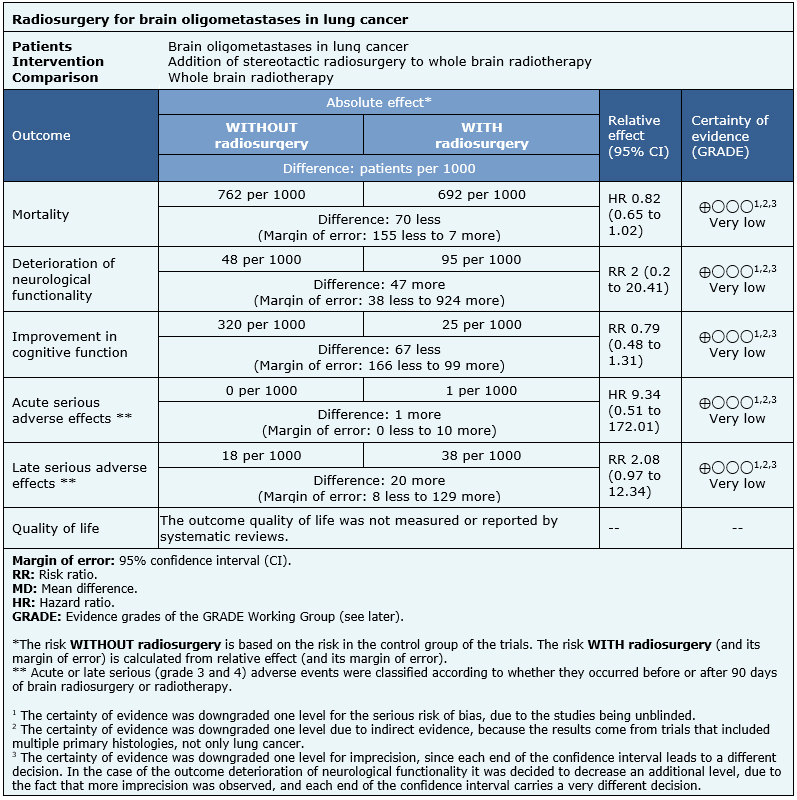
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
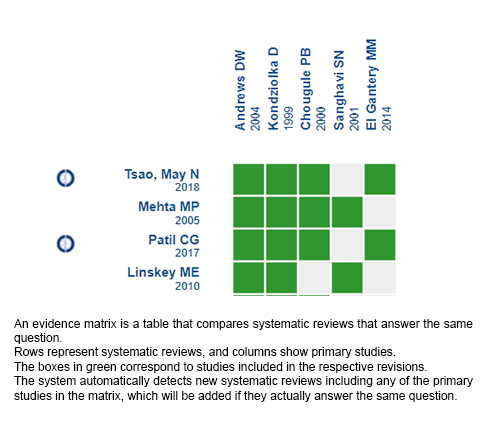
Follow the link to access the interactive version: Addition of radiosurgery to whole brain radiotherapy or systemic therapy for the treatment of brain oligometastases.
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.

INTRODUCCIÓN
Las metástasis cerebrales son un problema frecuente en el paciente oncológico, especialmente en el cáncer de pulmón. El tratamiento habitual para la oligometástasis cerebral es la radioterapia holo cerebral. Dado el persistente mal pronóstico de esta enfermedad, es que se han planteado otras alternativas terapéuticas como la radiocirugía. Sin embargo, no existe claridad respecto a la efectividad de su adición.
MÉTODOS
Realizamos una búsqueda en Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante el cribado de múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, analizamos los datos de los estudios primarios, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos 17 revisiones sistemáticas que en conjunto incluyeron siete estudios primarios, de los cuales, cuatro corresponden a ensayos aleatorizados. Todos los ensayos evaluaron a pacientes con metástasis cerebral, pero ninguno evaluó específicamente a población con cáncer de pulmón. Concluimos que no es posible establecer con claridad si la radiocirugía disminuye el deterioro de funcionalidad neurológica, deterioro cognitivo, mortalidad ni efectos adversos graves, debido a que la certeza de la evidencia existente ha sido evaluada como muy baja.
 Authors:
Gabriela Antúnez[1,2,3], Tomás Merino[2,3,4]
Authors:
Gabriela Antúnez[1,2,3], Tomás Merino[2,3,4]
Affiliation:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Chile
E-mail: tmerino@med.puc.cl

Citation: Antúnez G, Merino T. Radiosurgery for brain oligometastases in lung cancer . Medwave 2021;21(11):e8184 doi: 10.5867/medwave.2021.11.8184
Submission date: 31/1/2020
Acceptance date: 18/8/2020
Publication date: 23/12/2021
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Centro Evidencia UC in collaboration with the Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Villaruz LC, Kubicek GJ, Socinski MA. Management of non-small cell lung cancer with oligometastases. Curr Oncol Rep. 2012 Aug;14(4):333-41. | CrossRef | PubMed | PMC |
- Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, Liu M, Yuan Y. Whole Brain Radiation Therapy Plus Stereotactic Radiosurgery in the Treatment of BrainMetastases Leading to Improved Survival in Patients With Favorable Prognostic Factors. Front Oncol. 2019 Mar 29;9:205. | CrossRef | PubMed | PMC |
- Cohen-Inbar O, Sheehan JP. The role of stereotactic radiosurgery and whole brain radiation therapy as primary treatment in the treatment of patients with brain oligometastases - A systematic review. J Radiosurg SBRT. 2016;4(2):79-88. | PubMed | PMC |
- Mehta MP, Tsao MN, Whelan TJ, Morris DE, Hayman JA, Flickinger JC, Mills M, Rogers CL, Souhami L. The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 2005 Sep 1;63(1):37-46. | PubMed |
- Linskey ME, Andrews DW, Asher AL, Burri SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Kalkanis SN. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010 Jan;96(1):45-68. | CrossRef | PubMed | PMC |
- Tsao MN, Lloyd NS, Wong RK, Rakovitch E, Chow E, Laperriere N; Supportive Care Guidelines Group of Cancer Care Ontario's Program in Evidence-based Care. Radiotherapeutic management of brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2005 Jun;31(4):256-73. | PubMed |
- Stafinski T, Jhangri GS, Yan E, Menon D. Effectiveness of stereotactic radiosurgery alone or in combination with whole brain radiotherapy compared to conventional surgery and/or whole brain radiotherapy for the treatment of one or more brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2006 May;32(3):203-13. Epub 2006 Feb 10. | PubMed |
- Müller-Riemenschneider F, Bockelbrink A, Ernst I, Schwarzbach C, Vauth C, von der Schulenburg JM, Willich SN. Stereotactic radiosurgery for the treatment of brain metastases. Radiother Oncol. 2009 Apr;91(1):67-74. | CrossRef | PubMed |
- Scoccianti S, Ricardi U. Treatment of brain metastases: review of phase III randomized controlled trials. Radiother Oncol. 2012 Feb;102(2):168-79. | CrossRef | PubMed |
- Tsao M, Xu W, Sahgal A. A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer. 2012 May 1;118(9):2486-93. | CrossRef | PubMed |
- Patil CG, Pricola K, Sarmiento JM, Garg SK, Bryant A, Black KL. Whole brain radiation therapy (WBRT) alone versus WBRT and radiosurgery for the treatment of brain metastases. Cochrane Database Syst Rev. 2017 Sep 25;9:CD006121. | CrossRef | PubMed | PMC |
- Chao ST, De Salles A, Hayashi M, Levivier M, Ma L, Martinez R, Paddick I, Régis J, Ryu S, Slotman BJ, Sahgal A. Stereotactic Radiosurgery in the Management of Limited (1-4) Brain Metasteses: Systematic Review and International Stereotactic Radiosurgery Society Practice Guideline. Neurosurgery. 2018 Sep 1;83(3):345-353. | CrossRef | PubMed |
- Tsao MN, Xu W, Wong RK, Lloyd N, Laperriere N, Sahgal A, Rakovitch E, Chow E. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018 Jan 25;1:CD003869. | CrossRef | PubMed | PMC |
- Roos D. What is the randomised evidence for surgery and stereotactic radiosurgery for patients with solitary (or few) brain metastases? Int J Evid Based Healthc. 2011 Mar;9(1):61-6. | CrossRef | PubMed |
- Gupta T. Stereotactic radiosurgery for brain oligometastases: good for some, better for all? Ann Oncol. 2005 Nov;16(11):1749-54. Epub 2005 Aug 5. | PubMed |
- Schimmel WCM, Gehring K, Eekers DBP, Hanssens PEJ, Sitskoorn MM. Cognitive effects of stereotactic radiosurgery in adult patients with brain metastases: A systematic review. Adv Radiat Oncol. 2018 Jul 11;3(4):568-581. | CrossRef | PubMed | PMC |
- Goyal S, Silk AW, Tian S, Mehnert J, Danish S, Ranjan S, Kaufman HL. Clinical Management of Multiple Melanoma Brain Metastases: A Systematic Review. JAMA Oncol. 2015 Aug;1(5):668-76. | CrossRef | PubMed | PMC |
- Khan M, Lin J, Liao G, Li R, Wang B, Xie G, Zheng J, Yuan Y. Comparison of WBRT alone, SRS alone, and their combination in the treatment of one or more brain metastases: Review and meta-analysis. Tumour Biol. 2017 Jul;39(7):1010428317702903. | CrossRef | PubMed |
- Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004 May 22;363(9422):1665-72. | PubMed |
- Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys. 1999 Sep 1;45(2):427-34. | PubMed |
- El Gantery MM, Abd El Baky HM, El Hossieny HA, Mahmoud M, Youssef O. Management of brain metastases with stereotactic radiosurgery alone versus whole brain irradiation alone versus both. Radiat Oncol. 2014 May 20;9:116. | CrossRef | PubMed | PMC |
- Chougule, P.B et al. Randomized treatment of brain metastasis with gamma knife radiosurgery, whole brain radiotherapy or both. International Journal of Radiation Oncology • Biology • Physics, Volume 48, Issue 3, 114.
- Li B, Yu J, Suntharalingam M, Kennedy AS, Amin PP, Chen Z, Yin R, Guo S, Han T, Wang Y, Yu N, Song G, Wang L. Comparison of three treatment options for single brain metastasis from lung cancer. Int J Cancer. 2000 Feb 20;90(1):37-45. | PubMed |
- Auchter RM, Lamond JP, Alexander E, Buatti JM, Chappell R, Friedman WA, Kinsella TJ, Levin AB, Noyes WR, Schultz CJ, Loeffler JS, Mehta MP. A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastasis. Int J Radiat Oncol Biol Phys. 1996 Apr 1;35(1):27-35. | PubMed |
- Sanghavi SN, Miranpuri SS, Chappell R, Buatti JM, Sneed PK, Suh JH, Regine WF, Weltman E, King VJ, Goetsch SJ, Breneman JC, Sperduto PW, Scott C, Mabanta S, Mehta MP. Radiosurgery for patients with brain metastases: a multi-institutional analysis, stratified by the RTOG recursive partitioning analysis method. Int J Radiat Oncol Biol Phys. 2001 Oct 1;51(2):426-34. | PubMed |
- Sperduto PW, Shanley R, Luo X, Andrews D, Werner-Wasik M, Valicenti R, Bahary JP, Souhami L, Won M, Mehta M. Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1-3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys. 2014 Nov 1;90(3):526-31. | CrossRef | PubMed | PMC |
- Tsao MN, Lloyd NS, Wong RK; Supportive Care Guidelines Group of Cancer Care Ontario's Program in Evidence-based Care. Clinical practice guideline on the optimal radiotherapeutic management of brain metastases. BMC Cancer. 2005 Apr 4;5:34. | PubMed | PMC |
- Georges Noël, Waisse Waissi, Adrien Paix, Yvan Pin. Stereotactic radiation therapy in brain metastasis from melanoma: a systematic review. PROSPERO 2017 CRD42017082477 | Link |
 Villaruz LC, Kubicek GJ, Socinski MA. Management of non-small cell lung cancer with oligometastases. Curr Oncol Rep. 2012 Aug;14(4):333-41. | CrossRef | PubMed | PMC |
Villaruz LC, Kubicek GJ, Socinski MA. Management of non-small cell lung cancer with oligometastases. Curr Oncol Rep. 2012 Aug;14(4):333-41. | CrossRef | PubMed | PMC | Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, Liu M, Yuan Y. Whole Brain Radiation Therapy Plus Stereotactic Radiosurgery in the Treatment of BrainMetastases Leading to Improved Survival in Patients With Favorable Prognostic Factors. Front Oncol. 2019 Mar 29;9:205. | CrossRef | PubMed | PMC |
Khan M, Lin J, Liao G, Tian Y, Liang Y, Li R, Liu M, Yuan Y. Whole Brain Radiation Therapy Plus Stereotactic Radiosurgery in the Treatment of BrainMetastases Leading to Improved Survival in Patients With Favorable Prognostic Factors. Front Oncol. 2019 Mar 29;9:205. | CrossRef | PubMed | PMC | Cohen-Inbar O, Sheehan JP. The role of stereotactic radiosurgery and whole brain radiation therapy as primary treatment in the treatment of patients with brain oligometastases - A systematic review. J Radiosurg SBRT. 2016;4(2):79-88. | PubMed | PMC |
Cohen-Inbar O, Sheehan JP. The role of stereotactic radiosurgery and whole brain radiation therapy as primary treatment in the treatment of patients with brain oligometastases - A systematic review. J Radiosurg SBRT. 2016;4(2):79-88. | PubMed | PMC | Mehta MP, Tsao MN, Whelan TJ, Morris DE, Hayman JA, Flickinger JC, Mills M, Rogers CL, Souhami L. The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 2005 Sep 1;63(1):37-46. | PubMed |
Mehta MP, Tsao MN, Whelan TJ, Morris DE, Hayman JA, Flickinger JC, Mills M, Rogers CL, Souhami L. The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys. 2005 Sep 1;63(1):37-46. | PubMed | Linskey ME, Andrews DW, Asher AL, Burri SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Kalkanis SN. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010 Jan;96(1):45-68. | CrossRef | PubMed | PMC |
Linskey ME, Andrews DW, Asher AL, Burri SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS, McDermott M, Mehta MP, Mikkelsen T, Olson JJ, Paleologos NA, Patchell RA, Ryken TC, Kalkanis SN. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010 Jan;96(1):45-68. | CrossRef | PubMed | PMC | Tsao MN, Lloyd NS, Wong RK, Rakovitch E, Chow E, Laperriere N; Supportive Care Guidelines Group of Cancer Care Ontario's Program in Evidence-based Care. Radiotherapeutic management of brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2005 Jun;31(4):256-73. | PubMed |
Tsao MN, Lloyd NS, Wong RK, Rakovitch E, Chow E, Laperriere N; Supportive Care Guidelines Group of Cancer Care Ontario's Program in Evidence-based Care. Radiotherapeutic management of brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2005 Jun;31(4):256-73. | PubMed | Stafinski T, Jhangri GS, Yan E, Menon D. Effectiveness of stereotactic radiosurgery alone or in combination with whole brain radiotherapy compared to conventional surgery and/or whole brain radiotherapy for the treatment of one or more brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2006 May;32(3):203-13. Epub 2006 Feb 10. | PubMed |
Stafinski T, Jhangri GS, Yan E, Menon D. Effectiveness of stereotactic radiosurgery alone or in combination with whole brain radiotherapy compared to conventional surgery and/or whole brain radiotherapy for the treatment of one or more brain metastases: a systematic review and meta-analysis. Cancer Treat Rev. 2006 May;32(3):203-13. Epub 2006 Feb 10. | PubMed | Müller-Riemenschneider F, Bockelbrink A, Ernst I, Schwarzbach C, Vauth C, von der Schulenburg JM, Willich SN. Stereotactic radiosurgery for the treatment of brain metastases. Radiother Oncol. 2009 Apr;91(1):67-74. | CrossRef | PubMed |
Müller-Riemenschneider F, Bockelbrink A, Ernst I, Schwarzbach C, Vauth C, von der Schulenburg JM, Willich SN. Stereotactic radiosurgery for the treatment of brain metastases. Radiother Oncol. 2009 Apr;91(1):67-74. | CrossRef | PubMed | Scoccianti S, Ricardi U. Treatment of brain metastases: review of phase III randomized controlled trials. Radiother Oncol. 2012 Feb;102(2):168-79. | CrossRef | PubMed |
Scoccianti S, Ricardi U. Treatment of brain metastases: review of phase III randomized controlled trials. Radiother Oncol. 2012 Feb;102(2):168-79. | CrossRef | PubMed | Tsao M, Xu W, Sahgal A. A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer. 2012 May 1;118(9):2486-93. | CrossRef | PubMed |
Tsao M, Xu W, Sahgal A. A meta-analysis evaluating stereotactic radiosurgery, whole-brain radiotherapy, or both for patients presenting with a limited number of brain metastases. Cancer. 2012 May 1;118(9):2486-93. | CrossRef | PubMed | Patil CG, Pricola K, Sarmiento JM, Garg SK, Bryant A, Black KL. Whole brain radiation therapy (WBRT) alone versus WBRT and radiosurgery for the treatment of brain metastases. Cochrane Database Syst Rev. 2017 Sep 25;9:CD006121. | CrossRef | PubMed | PMC |
Patil CG, Pricola K, Sarmiento JM, Garg SK, Bryant A, Black KL. Whole brain radiation therapy (WBRT) alone versus WBRT and radiosurgery for the treatment of brain metastases. Cochrane Database Syst Rev. 2017 Sep 25;9:CD006121. | CrossRef | PubMed | PMC | Chao ST, De Salles A, Hayashi M, Levivier M, Ma L, Martinez R, Paddick I, Régis J, Ryu S, Slotman BJ, Sahgal A. Stereotactic Radiosurgery in the Management of Limited (1-4) Brain Metasteses: Systematic Review and International Stereotactic Radiosurgery Society Practice Guideline. Neurosurgery. 2018 Sep 1;83(3):345-353. | CrossRef | PubMed |
Chao ST, De Salles A, Hayashi M, Levivier M, Ma L, Martinez R, Paddick I, Régis J, Ryu S, Slotman BJ, Sahgal A. Stereotactic Radiosurgery in the Management of Limited (1-4) Brain Metasteses: Systematic Review and International Stereotactic Radiosurgery Society Practice Guideline. Neurosurgery. 2018 Sep 1;83(3):345-353. | CrossRef | PubMed | Tsao MN, Xu W, Wong RK, Lloyd N, Laperriere N, Sahgal A, Rakovitch E, Chow E. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018 Jan 25;1:CD003869. | CrossRef | PubMed | PMC |
Tsao MN, Xu W, Wong RK, Lloyd N, Laperriere N, Sahgal A, Rakovitch E, Chow E. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018 Jan 25;1:CD003869. | CrossRef | PubMed | PMC | Roos D. What is the randomised evidence for surgery and stereotactic radiosurgery for patients with solitary (or few) brain metastases? Int J Evid Based Healthc. 2011 Mar;9(1):61-6. | CrossRef | PubMed |
Roos D. What is the randomised evidence for surgery and stereotactic radiosurgery for patients with solitary (or few) brain metastases? Int J Evid Based Healthc. 2011 Mar;9(1):61-6. | CrossRef | PubMed | Gupta T. Stereotactic radiosurgery for brain oligometastases: good for some, better for all? Ann Oncol. 2005 Nov;16(11):1749-54. Epub 2005 Aug 5. | PubMed |
Gupta T. Stereotactic radiosurgery for brain oligometastases: good for some, better for all? Ann Oncol. 2005 Nov;16(11):1749-54. Epub 2005 Aug 5. | PubMed | Schimmel WCM, Gehring K, Eekers DBP, Hanssens PEJ, Sitskoorn MM. Cognitive effects of stereotactic radiosurgery in adult patients with brain metastases: A systematic review. Adv Radiat Oncol. 2018 Jul 11;3(4):568-581. | CrossRef | PubMed | PMC |
Schimmel WCM, Gehring K, Eekers DBP, Hanssens PEJ, Sitskoorn MM. Cognitive effects of stereotactic radiosurgery in adult patients with brain metastases: A systematic review. Adv Radiat Oncol. 2018 Jul 11;3(4):568-581. | CrossRef | PubMed | PMC | Goyal S, Silk AW, Tian S, Mehnert J, Danish S, Ranjan S, Kaufman HL. Clinical Management of Multiple Melanoma Brain Metastases: A Systematic Review. JAMA Oncol. 2015 Aug;1(5):668-76. | CrossRef | PubMed | PMC |
Goyal S, Silk AW, Tian S, Mehnert J, Danish S, Ranjan S, Kaufman HL. Clinical Management of Multiple Melanoma Brain Metastases: A Systematic Review. JAMA Oncol. 2015 Aug;1(5):668-76. | CrossRef | PubMed | PMC | Khan M, Lin J, Liao G, Li R, Wang B, Xie G, Zheng J, Yuan Y. Comparison of WBRT alone, SRS alone, and their combination in the treatment of one or more brain metastases: Review and meta-analysis. Tumour Biol. 2017 Jul;39(7):1010428317702903. | CrossRef | PubMed |
Khan M, Lin J, Liao G, Li R, Wang B, Xie G, Zheng J, Yuan Y. Comparison of WBRT alone, SRS alone, and their combination in the treatment of one or more brain metastases: Review and meta-analysis. Tumour Biol. 2017 Jul;39(7):1010428317702903. | CrossRef | PubMed | Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004 May 22;363(9422):1665-72. | PubMed |
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet. 2004 May 22;363(9422):1665-72. | PubMed | Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys. 1999 Sep 1;45(2):427-34. | PubMed |
Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys. 1999 Sep 1;45(2):427-34. | PubMed | El Gantery MM, Abd El Baky HM, El Hossieny HA, Mahmoud M, Youssef O. Management of brain metastases with stereotactic radiosurgery alone versus whole brain irradiation alone versus both. Radiat Oncol. 2014 May 20;9:116. | CrossRef | PubMed | PMC |
El Gantery MM, Abd El Baky HM, El Hossieny HA, Mahmoud M, Youssef O. Management of brain metastases with stereotactic radiosurgery alone versus whole brain irradiation alone versus both. Radiat Oncol. 2014 May 20;9:116. | CrossRef | PubMed | PMC | Chougule, P.B et al. Randomized treatment of brain metastasis with gamma knife radiosurgery, whole brain radiotherapy or both. International Journal of Radiation Oncology • Biology • Physics, Volume 48, Issue 3, 114.
Chougule, P.B et al. Randomized treatment of brain metastasis with gamma knife radiosurgery, whole brain radiotherapy or both. International Journal of Radiation Oncology • Biology • Physics, Volume 48, Issue 3, 114.  Li B, Yu J, Suntharalingam M, Kennedy AS, Amin PP, Chen Z, Yin R, Guo S, Han T, Wang Y, Yu N, Song G, Wang L. Comparison of three treatment options for single brain metastasis from lung cancer. Int J Cancer. 2000 Feb 20;90(1):37-45. | PubMed |
Li B, Yu J, Suntharalingam M, Kennedy AS, Amin PP, Chen Z, Yin R, Guo S, Han T, Wang Y, Yu N, Song G, Wang L. Comparison of three treatment options for single brain metastasis from lung cancer. Int J Cancer. 2000 Feb 20;90(1):37-45. | PubMed | Auchter RM, Lamond JP, Alexander E, Buatti JM, Chappell R, Friedman WA, Kinsella TJ, Levin AB, Noyes WR, Schultz CJ, Loeffler JS, Mehta MP. A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastasis. Int J Radiat Oncol Biol Phys. 1996 Apr 1;35(1):27-35. | PubMed |
Auchter RM, Lamond JP, Alexander E, Buatti JM, Chappell R, Friedman WA, Kinsella TJ, Levin AB, Noyes WR, Schultz CJ, Loeffler JS, Mehta MP. A multiinstitutional outcome and prognostic factor analysis of radiosurgery for resectable single brain metastasis. Int J Radiat Oncol Biol Phys. 1996 Apr 1;35(1):27-35. | PubMed | Sanghavi SN, Miranpuri SS, Chappell R, Buatti JM, Sneed PK, Suh JH, Regine WF, Weltman E, King VJ, Goetsch SJ, Breneman JC, Sperduto PW, Scott C, Mabanta S, Mehta MP. Radiosurgery for patients with brain metastases: a multi-institutional analysis, stratified by the RTOG recursive partitioning analysis method. Int J Radiat Oncol Biol Phys. 2001 Oct 1;51(2):426-34. | PubMed |
Sanghavi SN, Miranpuri SS, Chappell R, Buatti JM, Sneed PK, Suh JH, Regine WF, Weltman E, King VJ, Goetsch SJ, Breneman JC, Sperduto PW, Scott C, Mabanta S, Mehta MP. Radiosurgery for patients with brain metastases: a multi-institutional analysis, stratified by the RTOG recursive partitioning analysis method. Int J Radiat Oncol Biol Phys. 2001 Oct 1;51(2):426-34. | PubMed | Sperduto PW, Shanley R, Luo X, Andrews D, Werner-Wasik M, Valicenti R, Bahary JP, Souhami L, Won M, Mehta M. Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1-3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys. 2014 Nov 1;90(3):526-31. | CrossRef | PubMed | PMC |
Sperduto PW, Shanley R, Luo X, Andrews D, Werner-Wasik M, Valicenti R, Bahary JP, Souhami L, Won M, Mehta M. Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1-3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys. 2014 Nov 1;90(3):526-31. | CrossRef | PubMed | PMC | Tsao MN, Lloyd NS, Wong RK; Supportive Care Guidelines Group of Cancer Care Ontario's Program in Evidence-based Care. Clinical practice guideline on the optimal radiotherapeutic management of brain metastases. BMC Cancer. 2005 Apr 4;5:34. | PubMed | PMC |
Tsao MN, Lloyd NS, Wong RK; Supportive Care Guidelines Group of Cancer Care Ontario's Program in Evidence-based Care. Clinical practice guideline on the optimal radiotherapeutic management of brain metastases. BMC Cancer. 2005 Apr 4;5:34. | PubMed | PMC | Georges Noël, Waisse Waissi, Adrien Paix, Yvan Pin. Stereotactic radiation therapy in brain metastasis from melanoma: a systematic review. PROSPERO 2017 CRD42017082477 | Link |
Georges Noël, Waisse Waissi, Adrien Paix, Yvan Pin. Stereotactic radiation therapy in brain metastasis from melanoma: a systematic review. PROSPERO 2017 CRD42017082477 | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis









