Key Words: Vaccines, Reminder Systems, Primary health care, Epistemonikos, GRADE.
Abstract
INTRODUCTION
Different interventions have been proposed to improve influenza vaccine coverage. The use of reminders, through letters, phone calls, pamphlets or technological applications, among others, has stood out among the different alternatives to increase adherence to vaccination. However, its effectiveness is not clear. In this summary, the first of a series of evaluation of reminders will address the use of a reminder sent by mail.
METHODS
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the identified reviews, analyzed the data from the primary studies, performed a meta-analysis and prepared a summary table of the results using the GRADE method.
RESULTS AND CONCLUSIONS
We identified eight systematic reviews that included 35 primary studies, of which 32 correspond to randomized trials. We concluded that a reminder sent by mail, probably increase adherence to influenza vaccination in all age groups (adult population, over 60 an under 18).
Problem
Influenza is an acute respiratory disease caused by the influenza virus that can be prevented with a seasonal vaccine. Despite this, it remains an important cause of morbidity and mortality [1] since it is estimated that annual influenza epidemics cause 3-5 million serious cases and 290,000 to 650,000 deaths [2]. Additionally, these are associated to school and work absenteeism, generating substantial productivity losses [2].Various interventions have been proposed to increase the use of the influenza vaccine. Reminders can be provided through different communication channels: letters, phone calls, pamphlet or technological applications, among others. This article is part of a series evaluating the use of reminders and will focus particularly on sending, via traditional mail, a letter, postcard or brochure type reminder.
Methods
We search in Epistemonikos, the largest database of systematic health reviews, which is maintained through searches in multiple sources of information, including MEDLINE, EMBASE, Cochrane, among others. We extracted the data from the identified reviews and analyzed the data from the primary studies. With this information, we generate a structured summary called FRISBEE (Friendly Summaries of Body of Evidence using Epistemonikos), following a pre-established format, which includes key messages, a summary of the set of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of the studies when possible, a summary table of results with GRADE method and a section of other considerations for decision making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found eight systematic reviews [3], [4], [5], [6], [7], [8], [9], [10] which included 35 primary studies in 34 references [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44] of which, 32 are randomized trials reported in 31 references [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41]. Five trials were excluded [16], [18], [21], [33], [35] because they included co-interventions to increase influenza vaccination. Two trials were excluded [19], [24] because the intervention consisted of two or more letters as a reminder.In addition, observational studies [42], [43], [44] did not increase the certainty of existing evidence, nor did they provide additional relevant information. Finally, this table and the summary in general are based on 25 trialsreported in 24 references [11], [12], [13], [14], [15], [17], [20], [22], [23], [25], [26], [27], [28], [29], [30], [31], [32], [34], [36], [37], [38], [39], [40], [41]. |
|
What types of patients were included* |
The trials included a total of 589,144 participants of all ages, including children over six months to adults over 65 years. All included participants were targeted from population at risk, with the exception of two trials, targeted to the general population [23], and to the beneficiaries of a health insurance [28]. Five trials included children [19], [22], [24], [25], [41], 14 trials included older adults (over 60 years old) [11], [12], [13], [15], [17], [20], [27], [29], [32], [31], [34], [37], [38], [39] and the rest of the trials included population of any age. In general, the trials excluded participants who had already received the vaccine prior to the start of the trial, with egg allergy or participants living in nursing homes. |
|
What types of interventions were included* |
All trials evaluated the use of mail reminders in the form of postcard [11], [12], [13], [15], [20], [26], [27], [34], [36], letter [14], [17], [22], [23], [25], [28], [29], [31], [37], [38], [39], [40], [41] or pamphlet [30], [31]. All included trials compared against usual medical care. |
|
What types of outcomes |
The systematic reviews identified only evaluated adherence to treatment (influenza vaccination rate) The average follow-up of the trials was five months and 12 days (range from two weeks to 12 months). |
* Information about primary studies is not extracted directly from primary studies but from identified systematic reviews, unless otherwise stated.
Summary of findings
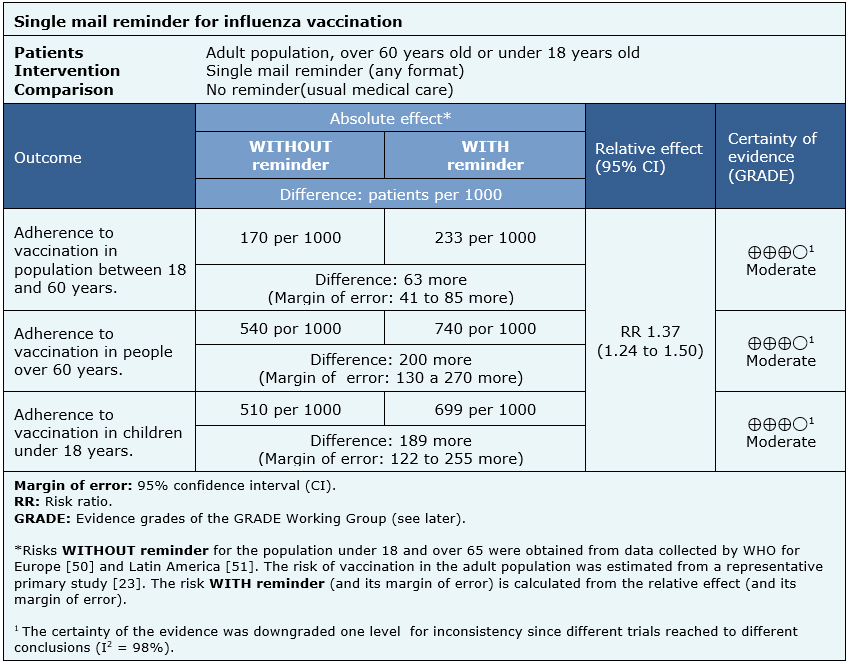
The information on the effects of a single mail reminder is based on 25 randomized trials that included 589,144 participants [11], [12], [13], [14], [15], [17], [20], [22], [23], [25], [26], [27], [28], [29], [30], [31], [32], [34], [36], [37], [38], [39], [40], [41].
All trials reported the outcome adherence to vaccination.
The summary of findings is as follows:
- A single mail reminder probably increases adherence to influenza vaccination in a population between 18 and 65 years.
- A single mail reminder probably increases adherence to influenza vaccination in people over 60.
- A single mail reminder probably increases adherence to influenza vaccination in a population under 18.
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
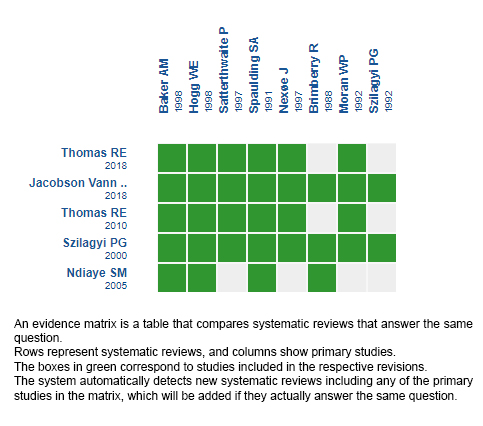
Follow the link to access the interactive version: Recordatorios mediante cartas paraaumentar la adherencia a la vacunación contra la influenza en población general
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
Distintas intervenciones han sido propuestas para reforzar el uso de la vacuna contra la influenza. El uso de recordatorios, ya sea a través de cartas, llamadas telefónicas, panfletos o aplicaciones tecnológicas, entre otras, ha destacado dentro de aquellas orientadas a incrementar la adherencia al tratamiento. Sin embargo, su efectividad no está clara. En este resumen, el primero de una serie de evaluación de recordatorios, se abordará el uso de un recordatorio enviado por correo.
MÉTODOS
Realizamos una búsqueda en Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante el cribado de múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, analizamos los datos de los estudios primarios, realizamos un meta-análisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos ocho revisiones sistemáticas que en conjunto incluyeron 35 estudios primarios, de los cuales, 32 corresponden a ensayos aleatorizados. Concluimos que un recordatorio enviado por correo probablemente aumenta la adherencia a vacunación contra influenza en todos los grupos etarios (población adulta, mayores de 60 años y menores de 18 años).
 Authors:
Nicole Silva[1,2], Camila Julio[1,2], Ángela Ortigoza[2,3]
Authors:
Nicole Silva[1,2], Camila Julio[1,2], Ángela Ortigoza[2,3]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Medicina Familiar, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: acortigoza@uc.com
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Chile

Citation: Silva N, Julio C, Ortigoza Á. Reminder sent by mail to increase adherence to influenza vaccination. Medwave 2019;19(12):e7746 doi: 10.5867/medwave.2019.12.7746
Submission date: 6/8/2019
Acceptance date: 19/12/2019
Publication date: 16/6/2020
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Organización Mundial de la Salud [Internet]. | Link |
- Organización Mundial de la Salud [Internet]. | Link |
- Aigbogun N.W. , Hawker J.I. , Stewart A. Interventions to increase influenza vaccination rates in children with high-risk conditions A systematic review. Vaccine. 2015 Dic; (33): 759–770.
- Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates (Review). Cochrane Database of Syst Rev. 2018, (1). | CrossRef |
- Jones Cooper SN, Walton-Moss B. Using reminder/recall systems to improve influenza immunization rates in children with asthma. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2013;27(5):327-33.
- Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, Rodewald LE. Effect of patient reminder/recall interventions on immunization rates: A review. JAMA. 2000;284(14):1820-7.
- Thomas RE, Russell ML, Lorenzetti DL. Systematic review of interventions to increase influenza vaccination rates of those 60 years and older. Vaccine. 2010;28(7):1684-701.
- Thomas RE, Lorenzetti DL. Interventions to increase influenza vaccination rates of those 60 years and older in the community. The Cochrane database of syst rev. 2018;5:CD005188.
- Ndiaye SM, Hopkins DP, Shefer AM, Hinman AR, Briss PA, Rodewald L, Willis B, Task Force on Community Preventive Services. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. American journal of preventive medicine. 2005;28(5 Suppl):248-79.
- Sarnoff R, Rundall T. Meta-analysis of effectiveness of interventions to increase influenza immunization rates among high-risk population groups. MCRR. 1998;55(4):432-56.
- Baker AM, McCarthy B, Gurley VF, Yood MU. Influenza immunization in a managed care organization. J Gen Intern Med. 1998;13(7):469-75.
- Barnas GP, McKinney WP. Postcard reminders and influenza vaccination. Geriatrics. 1989;37(2):195.
- Berg GD, Silverstein S, Thomas E, Korn AM. Cost and utilization avoidance with mail prompts: a randomized controlled trial. Am J Manag Care. 2008;14(11):748-54.
- Brimberry R. Vaccination of high-risk patients for influenza. A comparison of telephone and mail reminder methods. The Journal of family practice. 1988;26(4):397-400.
- Buchner DM, Larson EB, White RF. Influenza vaccination in community elderly. A controlled trial of postcard reminders. Geriatrics. 1987;35(8):755-60.
- Carter WB, Beach LR, Inui TS. The flu shot study: using multiattribute utility theory to design a vaccination intervention. Organizational behavior and human decision processes. 1986;38(3):378-91.
- Centers for Disease Control and Prevention (CDC). Increasing influenza vaccination rates for Medicare beneficiaries--Montana and Wyoming, 1994. MMWR. 1995;44(40):744-6.
- Clayton AE, McNutt LA, Homestead HL, Hartman TW, Senecal S. Public health in managed care: a randomized controlled trial of the effectiveness of postcard reminders. Am J Public Health. 1999;89(8):1235-7.
- Daley MF, Barrow J, Pearson K, Crane LA, Gao D, Stevenson JM, Berman S, Kempe A. Identification and recall of children with chronic medical conditions for influenza vaccination. Pediatrics. 2004;113(1 Pt 1): e26-33.
- Diaz Gravalos, GJ, Palmeiro, FG, Vazquez Fernandez, LA, Casado Gorriz, I, Fernandez Bernardez, MA, Sobrado Palomares, J. [Annual influenza vaccination. Causes of non-compliance among patients aged over 65 years]. Medifam - Revista de Medicina Familiar y Comunitaria. 1999;9(4):222-6.
- Dietrich AJ, Duhamel M. Improving geriatric preventive care through a patient-held checklist. Family medicine. 1989;21(3):195-8.
- Dombkowski KJ, Harrington LB, Dong S, Clark SJ. Seasonal influenza vaccination reminders for children with high-risk conditions: a registry-based randomized trial. American journal of preventive medicine. 2012;42(1):71-5.
- Hogg WE, Bass M, Calonge N, Crouch H, Satenstein G. Randomized controlled study of customized preventive medicine reminder letters in a community practice. Can Fam Physician 1998; 44:81-8.
- Kempe A, Daley MF, Barrow J, Allred N, Hester N, Beaty BL, Crane LA, Pearson K, Berman S. Implementation of universal influenza immunization recommendations for healthy young children: results of a randomized, controlled trial with registry-based recall. Pediatrics. 2005;115(1):146-54.
- Kemper KJ, Goldberg H. Do computer-generated reminder letters improve the rate of influenza immunization in an urban pediatric clinic? American journal of diseases of children (1960). 1993;147(7):717-8.
- Larson EB, Bergman J, Heidrich F, Alvin BL, Schneeweiss R. Do postcard reminders improve influenza compliance? A prospective trial of different postcard "cues". Medical care. 1982;20(6):639-48.
- Maglione MA, Stone EG, Shekelle PG. Mass mailings have little effect on utilization of influenza vaccine among Medicare beneficiaries. American Journal of Preventive Medicine. 2002;23(1):43-6.
- McCaul KD, Johnson RJ, Rothman AJ. The effects of framing and action instructions on whether older adults obtain flu shots. Health Psychol. 2002;21(6):624-8.
- Minor DS, Eubanks JT, Butler KR, Wofford MR, Penman AD, Replogle WH. Improving influenza vaccination rates by targeting individuals not seeking early seasonal vaccination. Am J Med 2010;123(11):1031-5.
- Moran WP, Nelson K, Wofford JL, Velez R, Case LD. Increasing influenza immunization among high-risk patients: education or financial incentive?. Am J Med. 1997;101(6):612-20.
- Moran WP, Nelson K, Wofford JL, Velez R. Computer-generated mailed reminders for influenza immunization: a clinical trial. J Gen Intern Med. 1992;7(5):535-7.
- Moran, WP, Wofford, JL, Velez, R. Assessment of influenza immunization of community elderly: illustrating the need for community level health information. Carolina Health Services Reviews. 1995; 3:21-29.
- Mullooly JP. Increasing influenza vaccination among high-risk elderly: a randomized controlled trial of a mail cue in an HMO setting. Am J Public Health. 1987;77(5):626-7.
- Nexøe J, Kragstrup J, Rønne T. Impact of postal invitations and user fee on influenza vaccination rates among the elderly. A randomized controlled trial in general practice. Scand J Prim Health Care. 1997;15(2):109-12.
- Nuttall D. The influence of health professionals on the uptake of the influenza immunization. Br J Community Nurs. 2003;8(9):391-6.
- Puech M, Ward J, Lajoie V. Postcard reminders from GPs for influenza vaccine: are they more effective than an ad hoc approach?. Aust N Z J Public Health 1998;22(2):254-6.
- Roca B, Herrero E, Resino E, Torres V, Penades M, Andreu C. Impact of education program on influenza vaccination rates in Spain. Am J Manag Care. 2012;18(12): e446-52.
- Satterthwaite P. A randomised intervention study to examine the effect on immunisation coverage of making influenza vaccine available at no cost. The New Zealand medical journal. 1997;110(1038):58-60.
- Smith DM, Zhou XH, Weinberger M, Smith F, McDonald RC. Mailed reminders for area-wide influenza immunization: a randomized controlled trial. J Am Geriatr Soc. 1999;47(1):1-5.
- Spaulding SA, Kugler JP. Influenza immunization: the impact of notifying patients of high-risk status. J Fam Pract. 1991;33(5):495-8.
- Szilagyi PG, Rodewald LE, Savageau J, Yoos L, Doane C. Improving influenza vaccination rates in children with asthma: a test of a computerized reminder system and an analysis of factors predicting vaccination compliance. Pediatrics. 1992;90(6):871-5.
- Larson EB, Olsen E, Cole W, Shortell S. The relationship of health beliefs and a postcard reminder to influenza vaccination. The Journal of family practice. 1979;8(6):1207-11.
- Moore ML, Parker AL. Influenza vaccine compliance among pediatric asthma patients: what is the better method of notification?. Pediatr Asthma Allergy Immunol. 2006; 19:200–4.
- Walter E, Sung J, Meine EK, Drucker RP. Clements DA. Lack of effectiveness of a letter reminder for annual influenza immunization of asthmatic children. Pediatr Infect Dis J. 1997; 16:1187–8.
- Community Preventive Services Task Force. Increasing appropriate vaccination: Client reminder and recall systems: Task Force finding and rationale statement. | Link |
- National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory Committee: standards for adult immunization practice. Public Health Reports 2014;129(2):115–23.
- American Academy of Pediatrics Committee on Infectious Diseases. Prevention of influenza: Recommendations for influenza immunization of children, 2008-2009. Pediatrics, 122(5), 1135- 1141.
- Norman D., Blyth C., Danchin M., Seale H., Barnes R., Moore H. Interventions to improve influenza vaccine coverage in children with medical comorbidities. PROSPERO 2019 CRD42019090623. | Link |
- Tim Chadborn, BSc MSc PhD. Childhood Influenza Immunisation Invitation Trial in Schools. International Clinical Trials Registry Platform NCT02883972. | Link |
 Aigbogun N.W. , Hawker J.I. , Stewart A. Interventions to increase influenza vaccination rates in children with high-risk conditions A systematic review. Vaccine. 2015 Dic; (33): 759–770.
Aigbogun N.W. , Hawker J.I. , Stewart A. Interventions to increase influenza vaccination rates in children with high-risk conditions A systematic review. Vaccine. 2015 Dic; (33): 759–770.  Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates (Review). Cochrane Database of Syst Rev. 2018, (1). | CrossRef |
Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates (Review). Cochrane Database of Syst Rev. 2018, (1). | CrossRef | Jones Cooper SN, Walton-Moss B. Using reminder/recall systems to improve influenza immunization rates in children with asthma. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2013;27(5):327-33.
Jones Cooper SN, Walton-Moss B. Using reminder/recall systems to improve influenza immunization rates in children with asthma. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2013;27(5):327-33.  Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, Rodewald LE. Effect of patient reminder/recall interventions on immunization rates: A review. JAMA. 2000;284(14):1820-7.
Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, Rodewald LE. Effect of patient reminder/recall interventions on immunization rates: A review. JAMA. 2000;284(14):1820-7.  Thomas RE, Russell ML, Lorenzetti DL. Systematic review of interventions to increase influenza vaccination rates of those 60 years and older. Vaccine. 2010;28(7):1684-701.
Thomas RE, Russell ML, Lorenzetti DL. Systematic review of interventions to increase influenza vaccination rates of those 60 years and older. Vaccine. 2010;28(7):1684-701.  Thomas RE, Lorenzetti DL. Interventions to increase influenza vaccination rates of those 60 years and older in the community. The Cochrane database of syst rev. 2018;5:CD005188.
Thomas RE, Lorenzetti DL. Interventions to increase influenza vaccination rates of those 60 years and older in the community. The Cochrane database of syst rev. 2018;5:CD005188.  Ndiaye SM, Hopkins DP, Shefer AM, Hinman AR, Briss PA, Rodewald L, Willis B, Task Force on Community Preventive Services. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. American journal of preventive medicine. 2005;28(5 Suppl):248-79.
Ndiaye SM, Hopkins DP, Shefer AM, Hinman AR, Briss PA, Rodewald L, Willis B, Task Force on Community Preventive Services. Interventions to improve influenza, pneumococcal polysaccharide, and hepatitis B vaccination coverage among high-risk adults: a systematic review. American journal of preventive medicine. 2005;28(5 Suppl):248-79.  Sarnoff R, Rundall T. Meta-analysis of effectiveness of interventions to increase influenza immunization rates among high-risk population groups. MCRR. 1998;55(4):432-56.
Sarnoff R, Rundall T. Meta-analysis of effectiveness of interventions to increase influenza immunization rates among high-risk population groups. MCRR. 1998;55(4):432-56.  Baker AM, McCarthy B, Gurley VF, Yood MU. Influenza immunization in a managed care organization. J Gen Intern Med. 1998;13(7):469-75.
Baker AM, McCarthy B, Gurley VF, Yood MU. Influenza immunization in a managed care organization. J Gen Intern Med. 1998;13(7):469-75.  Barnas GP, McKinney WP. Postcard reminders and influenza vaccination. Geriatrics. 1989;37(2):195.
Barnas GP, McKinney WP. Postcard reminders and influenza vaccination. Geriatrics. 1989;37(2):195.  Berg GD, Silverstein S, Thomas E, Korn AM. Cost and utilization avoidance with mail prompts: a randomized controlled trial. Am J Manag Care. 2008;14(11):748-54.
Berg GD, Silverstein S, Thomas E, Korn AM. Cost and utilization avoidance with mail prompts: a randomized controlled trial. Am J Manag Care. 2008;14(11):748-54.  Brimberry R. Vaccination of high-risk patients for influenza. A comparison of telephone and mail reminder methods. The Journal of family practice. 1988;26(4):397-400.
Brimberry R. Vaccination of high-risk patients for influenza. A comparison of telephone and mail reminder methods. The Journal of family practice. 1988;26(4):397-400.  Buchner DM, Larson EB, White RF. Influenza vaccination in community elderly. A controlled trial of postcard reminders. Geriatrics. 1987;35(8):755-60.
Buchner DM, Larson EB, White RF. Influenza vaccination in community elderly. A controlled trial of postcard reminders. Geriatrics. 1987;35(8):755-60.  Carter WB, Beach LR, Inui TS. The flu shot study: using multiattribute utility theory to design a vaccination intervention. Organizational behavior and human decision processes. 1986;38(3):378-91.
Carter WB, Beach LR, Inui TS. The flu shot study: using multiattribute utility theory to design a vaccination intervention. Organizational behavior and human decision processes. 1986;38(3):378-91.  Centers for Disease Control and Prevention (CDC). Increasing influenza vaccination rates for Medicare beneficiaries--Montana and Wyoming, 1994. MMWR. 1995;44(40):744-6.
Centers for Disease Control and Prevention (CDC). Increasing influenza vaccination rates for Medicare beneficiaries--Montana and Wyoming, 1994. MMWR. 1995;44(40):744-6.  Clayton AE, McNutt LA, Homestead HL, Hartman TW, Senecal S. Public health in managed care: a randomized controlled trial of the effectiveness of postcard reminders. Am J Public Health. 1999;89(8):1235-7.
Clayton AE, McNutt LA, Homestead HL, Hartman TW, Senecal S. Public health in managed care: a randomized controlled trial of the effectiveness of postcard reminders. Am J Public Health. 1999;89(8):1235-7.  Daley MF, Barrow J, Pearson K, Crane LA, Gao D, Stevenson JM, Berman S, Kempe A. Identification and recall of children with chronic medical conditions for influenza vaccination. Pediatrics. 2004;113(1 Pt 1): e26-33.
Daley MF, Barrow J, Pearson K, Crane LA, Gao D, Stevenson JM, Berman S, Kempe A. Identification and recall of children with chronic medical conditions for influenza vaccination. Pediatrics. 2004;113(1 Pt 1): e26-33.  Diaz Gravalos, GJ, Palmeiro, FG, Vazquez Fernandez, LA, Casado Gorriz, I, Fernandez Bernardez, MA, Sobrado Palomares, J. [Annual influenza vaccination. Causes of non-compliance among patients aged over 65 years]. Medifam - Revista de Medicina Familiar y Comunitaria. 1999;9(4):222-6.
Diaz Gravalos, GJ, Palmeiro, FG, Vazquez Fernandez, LA, Casado Gorriz, I, Fernandez Bernardez, MA, Sobrado Palomares, J. [Annual influenza vaccination. Causes of non-compliance among patients aged over 65 years]. Medifam - Revista de Medicina Familiar y Comunitaria. 1999;9(4):222-6.  Dietrich AJ, Duhamel M. Improving geriatric preventive care through a patient-held checklist. Family medicine. 1989;21(3):195-8.
Dietrich AJ, Duhamel M. Improving geriatric preventive care through a patient-held checklist. Family medicine. 1989;21(3):195-8.  Dombkowski KJ, Harrington LB, Dong S, Clark SJ. Seasonal influenza vaccination reminders for children with high-risk conditions: a registry-based randomized trial. American journal of preventive medicine. 2012;42(1):71-5.
Dombkowski KJ, Harrington LB, Dong S, Clark SJ. Seasonal influenza vaccination reminders for children with high-risk conditions: a registry-based randomized trial. American journal of preventive medicine. 2012;42(1):71-5.  Hogg WE, Bass M, Calonge N, Crouch H, Satenstein G. Randomized controlled study of customized preventive medicine reminder letters in a community practice. Can Fam Physician 1998; 44:81-8.
Hogg WE, Bass M, Calonge N, Crouch H, Satenstein G. Randomized controlled study of customized preventive medicine reminder letters in a community practice. Can Fam Physician 1998; 44:81-8.  Kempe A, Daley MF, Barrow J, Allred N, Hester N, Beaty BL, Crane LA, Pearson K, Berman S. Implementation of universal influenza immunization recommendations for healthy young children: results of a randomized, controlled trial with registry-based recall. Pediatrics. 2005;115(1):146-54.
Kempe A, Daley MF, Barrow J, Allred N, Hester N, Beaty BL, Crane LA, Pearson K, Berman S. Implementation of universal influenza immunization recommendations for healthy young children: results of a randomized, controlled trial with registry-based recall. Pediatrics. 2005;115(1):146-54.  Kemper KJ, Goldberg H. Do computer-generated reminder letters improve the rate of influenza immunization in an urban pediatric clinic? American journal of diseases of children (1960). 1993;147(7):717-8.
Kemper KJ, Goldberg H. Do computer-generated reminder letters improve the rate of influenza immunization in an urban pediatric clinic? American journal of diseases of children (1960). 1993;147(7):717-8.  Larson EB, Bergman J, Heidrich F, Alvin BL, Schneeweiss R. Do postcard reminders improve influenza compliance? A prospective trial of different postcard "cues". Medical care. 1982;20(6):639-48.
Larson EB, Bergman J, Heidrich F, Alvin BL, Schneeweiss R. Do postcard reminders improve influenza compliance? A prospective trial of different postcard "cues". Medical care. 1982;20(6):639-48.  Maglione MA, Stone EG, Shekelle PG. Mass mailings have little effect on utilization of influenza vaccine among Medicare beneficiaries. American Journal of Preventive Medicine. 2002;23(1):43-6.
Maglione MA, Stone EG, Shekelle PG. Mass mailings have little effect on utilization of influenza vaccine among Medicare beneficiaries. American Journal of Preventive Medicine. 2002;23(1):43-6.  McCaul KD, Johnson RJ, Rothman AJ. The effects of framing and action instructions on whether older adults obtain flu shots. Health Psychol. 2002;21(6):624-8.
McCaul KD, Johnson RJ, Rothman AJ. The effects of framing and action instructions on whether older adults obtain flu shots. Health Psychol. 2002;21(6):624-8.  Minor DS, Eubanks JT, Butler KR, Wofford MR, Penman AD, Replogle WH. Improving influenza vaccination rates by targeting individuals not seeking early seasonal vaccination. Am J Med 2010;123(11):1031-5.
Minor DS, Eubanks JT, Butler KR, Wofford MR, Penman AD, Replogle WH. Improving influenza vaccination rates by targeting individuals not seeking early seasonal vaccination. Am J Med 2010;123(11):1031-5.  Moran WP, Nelson K, Wofford JL, Velez R, Case LD. Increasing influenza immunization among high-risk patients: education or financial incentive?. Am J Med. 1997;101(6):612-20.
Moran WP, Nelson K, Wofford JL, Velez R, Case LD. Increasing influenza immunization among high-risk patients: education or financial incentive?. Am J Med. 1997;101(6):612-20.  Moran WP, Nelson K, Wofford JL, Velez R. Computer-generated mailed reminders for influenza immunization: a clinical trial. J Gen Intern Med. 1992;7(5):535-7.
Moran WP, Nelson K, Wofford JL, Velez R. Computer-generated mailed reminders for influenza immunization: a clinical trial. J Gen Intern Med. 1992;7(5):535-7.  Moran, WP, Wofford, JL, Velez, R. Assessment of influenza immunization of community elderly: illustrating the need for community level health information. Carolina Health Services Reviews. 1995; 3:21-29.
Moran, WP, Wofford, JL, Velez, R. Assessment of influenza immunization of community elderly: illustrating the need for community level health information. Carolina Health Services Reviews. 1995; 3:21-29.  Mullooly JP. Increasing influenza vaccination among high-risk elderly: a randomized controlled trial of a mail cue in an HMO setting. Am J Public Health. 1987;77(5):626-7.
Mullooly JP. Increasing influenza vaccination among high-risk elderly: a randomized controlled trial of a mail cue in an HMO setting. Am J Public Health. 1987;77(5):626-7.  Nexøe J, Kragstrup J, Rønne T. Impact of postal invitations and user fee on influenza vaccination rates among the elderly. A randomized controlled trial in general practice. Scand J Prim Health Care. 1997;15(2):109-12.
Nexøe J, Kragstrup J, Rønne T. Impact of postal invitations and user fee on influenza vaccination rates among the elderly. A randomized controlled trial in general practice. Scand J Prim Health Care. 1997;15(2):109-12.  Nuttall D. The influence of health professionals on the uptake of the influenza immunization. Br J Community Nurs. 2003;8(9):391-6.
Nuttall D. The influence of health professionals on the uptake of the influenza immunization. Br J Community Nurs. 2003;8(9):391-6.  Puech M, Ward J, Lajoie V. Postcard reminders from GPs for influenza vaccine: are they more effective than an ad hoc approach?. Aust N Z J Public Health 1998;22(2):254-6.
Puech M, Ward J, Lajoie V. Postcard reminders from GPs for influenza vaccine: are they more effective than an ad hoc approach?. Aust N Z J Public Health 1998;22(2):254-6.  Roca B, Herrero E, Resino E, Torres V, Penades M, Andreu C. Impact of education program on influenza vaccination rates in Spain. Am J Manag Care. 2012;18(12): e446-52.
Roca B, Herrero E, Resino E, Torres V, Penades M, Andreu C. Impact of education program on influenza vaccination rates in Spain. Am J Manag Care. 2012;18(12): e446-52.  Satterthwaite P. A randomised intervention study to examine the effect on immunisation coverage of making influenza vaccine available at no cost. The New Zealand medical journal. 1997;110(1038):58-60.
Satterthwaite P. A randomised intervention study to examine the effect on immunisation coverage of making influenza vaccine available at no cost. The New Zealand medical journal. 1997;110(1038):58-60.  Smith DM, Zhou XH, Weinberger M, Smith F, McDonald RC. Mailed reminders for area-wide influenza immunization: a randomized controlled trial. J Am Geriatr Soc. 1999;47(1):1-5.
Smith DM, Zhou XH, Weinberger M, Smith F, McDonald RC. Mailed reminders for area-wide influenza immunization: a randomized controlled trial. J Am Geriatr Soc. 1999;47(1):1-5.  Spaulding SA, Kugler JP. Influenza immunization: the impact of notifying patients of high-risk status. J Fam Pract. 1991;33(5):495-8.
Spaulding SA, Kugler JP. Influenza immunization: the impact of notifying patients of high-risk status. J Fam Pract. 1991;33(5):495-8.  Szilagyi PG, Rodewald LE, Savageau J, Yoos L, Doane C. Improving influenza vaccination rates in children with asthma: a test of a computerized reminder system and an analysis of factors predicting vaccination compliance. Pediatrics. 1992;90(6):871-5.
Szilagyi PG, Rodewald LE, Savageau J, Yoos L, Doane C. Improving influenza vaccination rates in children with asthma: a test of a computerized reminder system and an analysis of factors predicting vaccination compliance. Pediatrics. 1992;90(6):871-5.  Larson EB, Olsen E, Cole W, Shortell S. The relationship of health beliefs and a postcard reminder to influenza vaccination. The Journal of family practice. 1979;8(6):1207-11.
Larson EB, Olsen E, Cole W, Shortell S. The relationship of health beliefs and a postcard reminder to influenza vaccination. The Journal of family practice. 1979;8(6):1207-11.  Moore ML, Parker AL. Influenza vaccine compliance among pediatric asthma patients: what is the better method of notification?. Pediatr Asthma Allergy Immunol. 2006; 19:200–4.
Moore ML, Parker AL. Influenza vaccine compliance among pediatric asthma patients: what is the better method of notification?. Pediatr Asthma Allergy Immunol. 2006; 19:200–4.  Walter E, Sung J, Meine EK, Drucker RP. Clements DA. Lack of effectiveness of a letter reminder for annual influenza immunization of asthmatic children. Pediatr Infect Dis J. 1997; 16:1187–8.
Walter E, Sung J, Meine EK, Drucker RP. Clements DA. Lack of effectiveness of a letter reminder for annual influenza immunization of asthmatic children. Pediatr Infect Dis J. 1997; 16:1187–8.  Community Preventive Services Task Force. Increasing appropriate vaccination: Client reminder and recall systems: Task Force finding and rationale statement. | Link |
Community Preventive Services Task Force. Increasing appropriate vaccination: Client reminder and recall systems: Task Force finding and rationale statement. | Link | National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory Committee: standards for adult immunization practice. Public Health Reports 2014;129(2):115–23.
National Vaccine Advisory Committee. Recommendations from the National Vaccine Advisory Committee: standards for adult immunization practice. Public Health Reports 2014;129(2):115–23.  American Academy of Pediatrics Committee on Infectious Diseases. Prevention of influenza: Recommendations for influenza immunization of children, 2008-2009. Pediatrics, 122(5), 1135- 1141.
American Academy of Pediatrics Committee on Infectious Diseases. Prevention of influenza: Recommendations for influenza immunization of children, 2008-2009. Pediatrics, 122(5), 1135- 1141.  Norman D., Blyth C., Danchin M., Seale H., Barnes R., Moore H. Interventions to improve influenza vaccine coverage in children with medical comorbidities. PROSPERO 2019 CRD42019090623. | Link |
Norman D., Blyth C., Danchin M., Seale H., Barnes R., Moore H. Interventions to improve influenza vaccine coverage in children with medical comorbidities. PROSPERO 2019 CRD42019090623. | Link | Tim Chadborn, BSc MSc PhD. Childhood Influenza Immunisation Invitation Trial in Schools. International Clinical Trials Registry Platform NCT02883972. | Link |
Tim Chadborn, BSc MSc PhD. Childhood Influenza Immunisation Invitation Trial in Schools. International Clinical Trials Registry Platform NCT02883972. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








