Key Words: BNP, acute dyspnea, Epistemonikos, GRADE
Abstract
INTRODUCTION
The performance of B-type natriuretic peptide to accurately diagnose dyspnea of cardiac origin has been widely proved. However, its impact in clinical practice is less clear.
METHODS
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
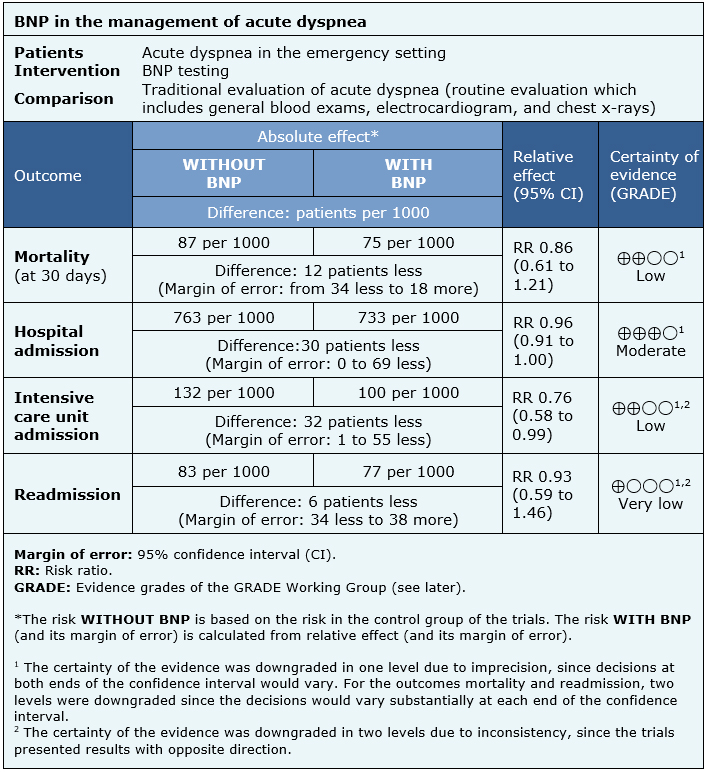
We identified two systematic reviews including five studies overall, of which all were randomized trials. We concluded the use of B-type natriuretic peptide for the management of acute dyspnea in the emergency setting probably leads to a small reduction in the need for hospitalization. Additionally, it may slightly reduce mortality and intensive care unit admission, but the certainty of the evidence is low.
Problem
BNP (brain natriuretic peptide or B-type natriuretic peptide) is a polypeptide, originally found in the brain, which is secreted by ventricular cardiomyocytes in response to the stretching of myocardial fibers due to an increased hydrostatic pressure. Therefore, its levels increase in heart failure, especially when there is a reduced left ventricular ejection fraction. Its function is to promote diuresis and natriuresis, and thus to lower blood pressure. Given its correlation with heart failure, it constitutes a diagnostic method in dyspnea of cardiac origin, with high sensitivity and specificity when used in conjunction with classic methods for the diagnosis of heart failure: symptoms, physical examination, chest radiography and electrocardiogram. However, it is not clear whether the addition of this test to the management of acute dyspnea leads to changes in the clinical decisions that will ultimately translate into benefits for these patients.
Methods
We searched in Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found two systematic reviews [1], [2], which included five primary studies [3], [4], [5], [6], [7], all corresponding to randomized controlled trials. |
|
What types of patients were included* |
All trials included patients that presented acute dyspnea in an emergency setting. The mean age ranged from 58 to 74 years across the different trials, with a small predominance of male participants. Three trials [3], [5], [6], reported that 17% to 40% of the patients included had past medical history of heart failure. Four trials [3], [4], [5], [6], reported that 24 to 45% of included patients had chronic obstructive pulmonary disease, and four trials [3], [4], [5], [6], reported past history of tobacco use in 28 to 50% of patients. |
|
What types of interventions were included* |
Three trials evaluated the use of BNP [4], [6], [7] and two trials measured Pro-BNP [3], [5]. All trials compared against routine evaluation, which included general blood exams, electrocardiogram and chest x-rays. |
|
What types of outcomes |
The trials evaluated multiple outcomes, which were grouped by the systematic reviews as follows:
The mean follow up time for the trials was 30 days, with a range from 30 to 60 days. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of findings
The information on the effects of BNP in the management of acute dyspnea in the emergency setting is based on five randomized trials [3], [4], [5], [6], [7] that included 2488 patients.
All trials reported hospital admissions (2488 patients), three trials evaluated mortality (at 30 days) (1524 patients) and intensive care unit admissions (1541 patients) [4], [5], [6] and two trials evaluated readmission (848 patients) [4], [5].
The summary of findings is as follows:
- The use of BNP in the management of dyspnea in the emergency setting may slightly reduce mortality at 30 days (low certainty of evidence).
- The use of BNP in the management of acute dyspnea in the emergency setting probably slightly reduces hospital admissions (moderate certainty of evidence).
- The use of BNP in the management of acute dyspnea in the emergency setting may slightly reduce intensive care unit admissions (low certainty of evidence).
- We are uncertain whether the use of BNP test in the management of acute dyspnea in the emergency setting has any impact on readmissions as the certainty of the evidence has been assessed as very low.
|
Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
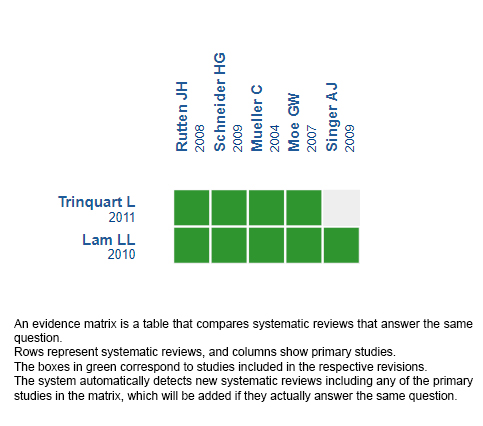
Follow the link to access the interactive version: B-type natriuretic peptide testing for managing acute dyspnea at emergency settings
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La exactitud diagnóstica del péptido natriurético cerebral (brain natriuretic peptide - BNP) para diferenciar el origen cardiogénico en pacientes con disnea aguda ha sido probada. Sin embargo, existe poca claridad en relación al impacto que tiene su incorporación en la práctica clínica.
MÉTODOS
Para responder esta pregunta utilizamos Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante búsquedas en múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, reanalizamos los datos de los estudios primarios, realizamos un metanálisis, preparamos tablas de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos dos revisiones sistemáticas que en conjunto incluyeron cinco estudios primarios, todos correspondientes a ensayos aleatorizados. Concluimos que la incorporación de BNP en el manejo de pacientes con disnea aguda probablemente disminuye levemente la necesidad de hospitalización. Además, podría disminuir levemente la mortalidad y hospitalizaciones en unidad de cuidados intensivos.
 Authors:
María Morales[1,2], Gabriel Rada[2,3,4]
Authors:
María Morales[1,2], Gabriel Rada[2,3,4]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Centro Evidencia UC
E-mail: radagabriel@epistemonikos.org
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Chile

Citation: Morales M, Rada G. B-type natriuretic peptide testing in the emergency setting for managing acute dyspnea. Medwave 2019;19(10):e7677 doi: 10.5867/medwave.2019.10.7677
Submission date: 30/11/2018
Acceptance date: 22/3/2019
Publication date: 8/11/2019
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Lam LL, Cameron PA, Schneider HG, Abramson MJ, Müller C, Krum H. Meta-analysis: Effect of B-Type Natriuretic Peptide Testing on Clinical Outcomes in Patients With Acute Dyspnea in the Emergency Setting. Ann Intern Med. 2010;153:728–735. | CrossRef |
- Trinquart, Ludovic et al. Natriuretic peptide testing in EDs for managing acute dyspnea: a meta-analysis. The American Journal of Emergency Medicine , Volume 29 , Issue 7 , 757 - 767.
- Moe GW, Howlett J, Januzzi JL, Zowall H. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007;115(24):3103-10.
- Mueller C, Scholer A, Laule-Kilian K, Martina B, Schindler C, Buser P, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 2004;350(7):647-54.
- Rutten JH, Steyerberg EW, Boomsma F, van Saase JL, Deckers JW, Hoogsteden HC, et al. N-terminal pro-brain natriuretic peptide testing in the emergency department: beneficial effects on hospitalization, costs, and outcome. Am Heart J 2008;156(1):71-7.
- Schneider HG, Lam L, Lokuge A, Krum H, Naughton MT, De Villiers Smit P, et al. B-type natriuretic peptide testing, clinical outcomes, and health services use in emergency department patients with dyspnea: a randomized trial. Ann Intern Med 2009;150(6):365-71.
- Singer AJ, Birkhahn RH, Guss D, Chandra A, Miller CD, Tiffany B, et al. Rapid Emergency Department Heart Failure Outpatients Trial (REDHOT II): a randomized controlled trial of the effect of serial B-type natriuretic peptide testing on patient management. Circ Heart Fail. 2009;2:287-93. | PubMed |
- Scuffham, P. A., Ball, J., Horowitz, J. D., Wong, C., Newton, P. J., Macdonald, P., McVeigh, J., Rischbieth, A., Emanuele, N., Carrington, M. J., Reid, C. M., Chan, Y. K., Stewart, S., WHICH? II Trial Investigators (2017). Standard vs. intensified management of heart failure to reduce healthcare costs: results of a multicentre, randomized controlled trial. European heart journal, 38(30), 2340-2348.
- Carpenter, C. R., Keim, S. M., Worster, A., Rosen, P., BEEM (Best Evidence in Emergency Medicine) (2011). Brain natriuretic peptide in the evaluation of emergency department dyspnea: is there a role?. The Journal of emergency medicine, 42(2), 197-205.
 Lam LL, Cameron PA, Schneider HG, Abramson MJ, Müller C, Krum H. Meta-analysis: Effect of B-Type Natriuretic Peptide Testing on Clinical Outcomes in Patients With Acute Dyspnea in the Emergency Setting. Ann Intern Med. 2010;153:728–735. | CrossRef |
Lam LL, Cameron PA, Schneider HG, Abramson MJ, Müller C, Krum H. Meta-analysis: Effect of B-Type Natriuretic Peptide Testing on Clinical Outcomes in Patients With Acute Dyspnea in the Emergency Setting. Ann Intern Med. 2010;153:728–735. | CrossRef | Trinquart, Ludovic et al. Natriuretic peptide testing in EDs for managing acute dyspnea: a meta-analysis. The American Journal of Emergency Medicine , Volume 29 , Issue 7 , 757 - 767.
Trinquart, Ludovic et al. Natriuretic peptide testing in EDs for managing acute dyspnea: a meta-analysis. The American Journal of Emergency Medicine , Volume 29 , Issue 7 , 757 - 767.  Moe GW, Howlett J, Januzzi JL, Zowall H. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007;115(24):3103-10.
Moe GW, Howlett J, Januzzi JL, Zowall H. N-terminal pro-B-type natriuretic peptide testing improves the management of patients with suspected acute heart failure: primary results of the Canadian prospective randomized multicenter IMPROVE-CHF study. Circulation 2007;115(24):3103-10.  Mueller C, Scholer A, Laule-Kilian K, Martina B, Schindler C, Buser P, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 2004;350(7):647-54.
Mueller C, Scholer A, Laule-Kilian K, Martina B, Schindler C, Buser P, et al. Use of B-type natriuretic peptide in the evaluation and management of acute dyspnea. N Engl J Med 2004;350(7):647-54.  Rutten JH, Steyerberg EW, Boomsma F, van Saase JL, Deckers JW, Hoogsteden HC, et al. N-terminal pro-brain natriuretic peptide testing in the emergency department: beneficial effects on hospitalization, costs, and outcome. Am Heart J 2008;156(1):71-7.
Rutten JH, Steyerberg EW, Boomsma F, van Saase JL, Deckers JW, Hoogsteden HC, et al. N-terminal pro-brain natriuretic peptide testing in the emergency department: beneficial effects on hospitalization, costs, and outcome. Am Heart J 2008;156(1):71-7.  Schneider HG, Lam L, Lokuge A, Krum H, Naughton MT, De Villiers Smit P, et al. B-type natriuretic peptide testing, clinical outcomes, and health services use in emergency department patients with dyspnea: a randomized trial. Ann Intern Med 2009;150(6):365-71.
Schneider HG, Lam L, Lokuge A, Krum H, Naughton MT, De Villiers Smit P, et al. B-type natriuretic peptide testing, clinical outcomes, and health services use in emergency department patients with dyspnea: a randomized trial. Ann Intern Med 2009;150(6):365-71.  Singer AJ, Birkhahn RH, Guss D, Chandra A, Miller CD, Tiffany B, et al. Rapid Emergency Department Heart Failure Outpatients Trial (REDHOT II): a randomized controlled trial of the effect of serial B-type natriuretic peptide testing on patient management. Circ Heart Fail. 2009;2:287-93. | PubMed |
Singer AJ, Birkhahn RH, Guss D, Chandra A, Miller CD, Tiffany B, et al. Rapid Emergency Department Heart Failure Outpatients Trial (REDHOT II): a randomized controlled trial of the effect of serial B-type natriuretic peptide testing on patient management. Circ Heart Fail. 2009;2:287-93. | PubMed | Scuffham, P. A., Ball, J., Horowitz, J. D., Wong, C., Newton, P. J., Macdonald, P., McVeigh, J., Rischbieth, A., Emanuele, N., Carrington, M. J., Reid, C. M., Chan, Y. K., Stewart, S., WHICH? II Trial Investigators (2017). Standard vs. intensified management of heart failure to reduce healthcare costs: results of a multicentre, randomized controlled trial. European heart journal, 38(30), 2340-2348.
Scuffham, P. A., Ball, J., Horowitz, J. D., Wong, C., Newton, P. J., Macdonald, P., McVeigh, J., Rischbieth, A., Emanuele, N., Carrington, M. J., Reid, C. M., Chan, Y. K., Stewart, S., WHICH? II Trial Investigators (2017). Standard vs. intensified management of heart failure to reduce healthcare costs: results of a multicentre, randomized controlled trial. European heart journal, 38(30), 2340-2348.  Carpenter, C. R., Keim, S. M., Worster, A., Rosen, P., BEEM (Best Evidence in Emergency Medicine) (2011). Brain natriuretic peptide in the evaluation of emergency department dyspnea: is there a role?. The Journal of emergency medicine, 42(2), 197-205.
Carpenter, C. R., Keim, S. M., Worster, A., Rosen, P., BEEM (Best Evidence in Emergency Medicine) (2011). Brain natriuretic peptide in the evaluation of emergency department dyspnea: is there a role?. The Journal of emergency medicine, 42(2), 197-205. Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








