Abstract
INTRODUCTION
Bronchiolitis is an acute small airways inflammation mainly caused by a viral infection. It is frequent in children under two years of age, particularly under 12 months. The use of systemic corticosteroids has been proposed for bronchiolitis, especially for severely ill patients. However, its efficacy is still controversial.
METHODS
To answer this question we gathered information using Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data from primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified four systematic reviews, including 20 randomized trials overall. We concluded the use of systemic corticosteroids has no benefit for the treatment of bronchiolitis, even for patients with mechanical ventilation.
Problem
Bronchiolitis is an acute small airways inflammation mainly caused by a viral infection, being respiratory syncytial virus one of the most important etiologies. It is highly frequent in children under two years of age, particularly under 12 months, being an important cause of hospital admission in this age group. Given its antiinflammatory effects and its efficacy in other respiratory conditions like asthma, the use of systemic corticosteroids has been proposed for patients presenting with bronchiolitis, especially for those severely ill.
The present summary aims to review if systemic corticosteroids are useful as an alternative treatment for patients presenting with an episode of bronchiolitis.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
Four systematic reviews were identified [1],[2],[3],[4]. They included |
|
What types of patients were included* |
All trials included patients presenting with bronchiolitis. Regarding age, 18 trials included patients less than 24 months [5],[6], Four trials included patients with mechanical ventilation [6],[14],[15],[16]. Six trials did not report if they included patients with mechanical ventilation [7],[8],[10],[13],[18],[20]. |
|
What types of interventions were included* |
All trials compared systemic corticosteroids versus placebo. Nine trials used dexamethasone [6],[8],[10],[11],[12],[16],[19],[23],[24], one used prednisone [5], one used methylprednisolone [7], seven used prednisolone [9],[14],[15],[18],[20],[21],[22], one used either prednisolone or methylprednisolone [17], and one used an initial course of hydrocortisone followed by prednisone [13]. In eleven trials the corticosteroid was administered orally [5],[9],[10],[12],[14],[15],[18],[19],[20],[21],[22], in three it was intravenous [6],[8],[16], in four it was intramuscular [7],[11],[23],[24], in one it was either oral or intravenous [17], and in one it was initially intravenous and then oral [13]. In 11 trials, intervention lasted on average four days, with a range from two to ten days [5],[6],[7],[8],[9],[10],[11],[12],[14],[15], |
|
What types of outcomes |
Systematic reviews reported the following outcomes: length of stay in hospital, length of stay in intensive care unit, duration of invasive mechanical ventilation, death of patients with mechanical ventilation, clinical score and duration of symptoms. Follow up was seven days or less in six trials [8],[9],[10],[14],[21],[23], two to four weeks in eight trials [6],[7],[11],[12],[13],[16],[20],[24], two months in one trial [22], a year in one trial [17], two years in one trial [5], and five years in one trial [14]. |
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
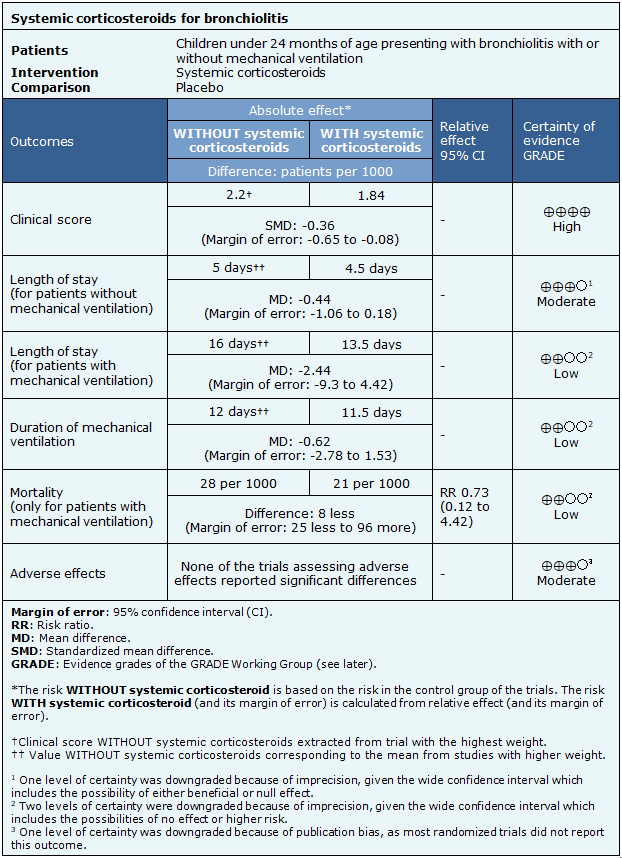
Summary of Findings
The information regarding the effects of systemic corticosteroids was based on ten randomized trials, including 580 patients [5],[6],[7],[8],[9],[10],[12],[13],[14],[15].Ten trials had no extractable data from the identified systematic reviews [4],[11],[17],[18],[19],[20],[21],[22],[23],[24].Three trials reported clinical score [7],[10],[12], five trials reported length of stay in hospital for patients without mechanical ventilation [6],[7],[9],[12],[13] and two reported length of stay for patients with mechanical ventilation [13],[15]. Three trials assessed the duration of mechanical ventilation [5],[13],[15] and three trials reported mortality in patients with mechanical ventilation [5],[13],[15]. Regarding adverse effects, four trials assessed them [8],[10],[13],[14]. The summary of findings is as follows:
- The use of systemic corticosteroids does not relevantly reduce clinical score for patients with bronchiolitis. The certainty of the evidence is high.
- The use of systemic corticosteroids probably does not reduce length of stay for patients without mechanical ventilation presenting with bronchiolitis. The certainty of the evidence is moderate.
- The use of systemic corticosteroids might result in little or no reduction in length of stay for patients with mechanical ventilation presenting with bronchiolitis. The certainty of the evidence is low.
- The use of systemic corticosteroids might result in little or no reduction of the duration of mechanical ventilation for patients presenting with bronchiolitis. The certainty of the evidence is low.
- The use of systemic corticosteroids might result in little or no reduction of mortality in patients with mechanical ventilation presenting with bronchiolitis. The certainty of the evidence is low.
- Probably, there are no significant adverse effects related to the use of systemic corticosteroids for bronchiolitis.
| Follow the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
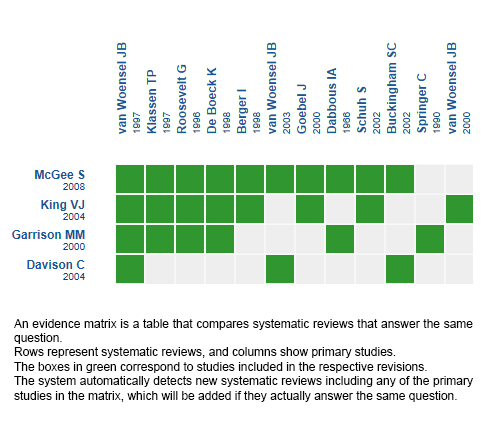
Follow the link to access the interactive version: Systemic corticosteroids for bronchiolitis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La bronquiolitis es una inflamación aguda de las vías aéreas pequeñas debida principalmente a una infección viral. Es una patología frecuente en menores de dos años y en especial en menores de 12 meses. Se ha propuesto el uso de corticoides sistémicos en bronquiolitis, en especial en pacientes de mayor severidad, siendo controversial su utilidad.
MÉTODOS
Para evaluarlo utilizamos Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud, la cual es mantenida mediante búsquedas en múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, reanalizamos los datos de los estudios primarios, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos cuatro revisiones sistemáticas que en conjunto incluyeron 20 ensayos aleatorizados. Concluimos que el uso de corticoides sistémicos no aporta ningún beneficio en el tratamiento de la bronquiolitis, aún en pacientes con ventilación mecánica.
 Authors:
Gonzalo Alarcón-Andrade[1,2], Lorena Cifuentes[2,3,4]
Authors:
Gonzalo Alarcón-Andrade[1,2], Lorena Cifuentes[2,3,4]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Pediatría, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Centro Evidencia UC, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: lorena.cifuentes@uc.cl
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Centro de Innovación UC Anacleto Angelini Avda.Vicuña Mackenna 4860 Macul Santiago Chile

Citation: Alarcón-Andrade G, Cifuentes L. Should systemic corticosteroids be used for bronchiolitis?. Medwave 2018 May-Jun;18(2):e7206 doi: 10.5867/medwave.2018.02.7206
Submission date: 24/11/2017
Acceptance date: 29/12/2017
Publication date: 7/5/2018
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Davison C, Ventre KM, Luchetti M, Randolph AG. Efficacy of interventions for bronchiolitis in critically ill infants: a systematic review and meta-analysis. Pediatr Crit Care Med. 2004 Sep;5(5):482-9. | PubMed | PMC |
- Garrison MM, Christakis DA, Harvey E, Cummings P, Davis RL. Systemic corticosteroids in infant bronchiolitis: A meta-analysis. Pediatrics. 2000 Apr;105(4):E44. | PubMed |
- King VJ, Viswanathan M, Bordley WC, Jackman AM, Sutton SF, Lohr KN, et al. Pharmacologic treatment of bronchiolitis in infants and children: a systematic review. Arch Pediatr Adolesc Med. 2004 Feb;158(2):127-37. | PubMed |
- McGee S, Hirschmann J. Use of corticosteroids in treating infectious diseases. Arch Intern Med. 2008 May 26;168(10):1034-46. | CrossRef | PubMed |
- Berger I, Argaman Z, Schwartz SB, Segal E, Kiderman A, Branski D, Kerem E. Efficacy of corticosteroids in acute bronchiolitis: short-term and long-term follow-up. Pediatr Pulmonol. 1998 Sep;26(3):162-6. | PubMed |
- Buckingham SC, Jafri HS, Bush AJ, Carubelli CM, Sheeran P, Hardy RD, Ottolini MG, Ramilo O, DeVincenzo JP. A randomized, double-blind, placebo-controlled trial of dexamethasone in severe respiratory syncytial virus (RSV) infection: effects on RSV quantity and clinical outcome. J Infect Dis. 2002 May 1;185(9):1222-8 | PubMed |
- Dabbous IA, Tkachyk JS, Stamm SJ. A double blind study on the effects of corticosteroids in the treatment of bronchiolitis. Pediatrics. 1966 Mar;37(3):477-84. | PubMed |
- De Boeck K, Van der Aa N, Van Lierde S, Corbeel L, Eeckels R. Respiratory syncytial virus bronchiolitis: a double-blind dexamethasone efficacy study. J Pediatr. 1997 Dec;131(6):919-21. | PubMed |
- Goebel J, Estrada B, Quinonez J, Nagji N, Sanford D, Boerth RC. Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr (Phila). 2000 Apr;39(4):213-20. | PubMed |
- Klassen TP, Sutcliffe T, Watters LK, Wells GA, Allen UD, Li MM. Dexamethasone in salbutamol-treated inpatients with acute bronchiolitis: a randomized, controlled trial. J Pediatr. 1997 Feb;130(2):191-6. | PubMed |
- Roosevelt G, Sheehan K, Grupp-Phelan J, Tanz RR, Listernick R. Dexamethasone in bronchiolitis: a randomised controlled trial. Lancet. 1996 Aug 3;348(9023):292-5. | PubMed |
- Schuh S, Coates AL, Binnie R, Allin T, Goia C, Corey M, Dick PT. Efficacy of oral dexamethasone in outpatients with acute bronchiolitis. J Pediatr. 2002 Jan;140(1):27-32. | PubMed |
- Springer C, Bar-Yishay E, Uwayyed K, Avital A, Vilozni D, Godfrey S. Corticosteroids do not affect the clinical or physiological status of infants with bronchiolitis. Pediatr Pulmonol. 1990;9(3):181-5. | PubMed |
- van Woensel JB, Wolfs TF, van Aalderen WM, Brand PL, Kimpen JL. Randomised double blind placebo controlled trial of prednisolone in children admitted to hospital with respiratory syncytial virus bronchiolitis. Thorax. 1997 Jul;52(7):634-7. | PubMed | PMC |
- van Woensel JB, Kimpen JL, Sprikkelman AB, Ouwehand A, van Aalderen WM. Long-term effects of prednisolone in the acute phase of bronchiolitis caused by respiratory syncytial virus. Pediatr Pulmonol. 2000 Aug;30(2):92-6 | PubMed |
- van Woensel JB, van Aalderen WM, de Weerd W, Jansen NJ, van Gestel JP, Markhorst DG, van Vught AJ, Bos AP, Kimpen JL. Dexamethasone for treatment of patients mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus. Thorax. 2003 May;58(5):383-7. | PubMed | PMC |
- Bülow SM, Nir M, Levin E, Friis B, Thomsen LL, Nielsen JE, Holm JC, Moller T, Bonde-Hansen ME, Nielsen HE. Prednisolone treatment of respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics. 1999 Dec;104(6):e77. | PubMed |
- Connolly JH, Field CM, Glasgow JF, Slattery CM, MacLynn DM. A double blind trial of prednisolone in epidemic bronchiolitis due to respiratory syncytial virus. Acta Paediatr Scand. 1969 Mar;58(2):116-20. | PubMed |
- Corneli HM, Zorc JJ, Mahajan P, Shaw KN, Holubkov R, Reeves SD, Ruddy RM, Malik B, Nelson KA, Bregstein JS, Brown KM, Denenberg MN, Lillis KA, Cimpello LB, Tsung JW, Borgialli DA, Baskin MN, Teshome G, Goldstein MA, Monroe D, Dean JM, Kuppermann N; Bronchiolitis Study Group of the Pediatric Emergency Care Applied Research Network (PECARN). A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med. 2007 Jul 26;357(4):331-9. Erratum in: N Engl J Med. 2008 Oct 30;359(18):1972. Majahan, Prashant [corrected to Mahajan, Prashant]. | PubMed |
- Csonka P, Kaila M, Laippala P, Iso-Mustajärvi M, Vesikari T, Ashorn P. Oral prednisolone in the acute management of children age 6 to 35 months with viral respiratory infection-induced lower airway disease: a randomized, placebo-controlled trial. J Pediatr. 2003 Dec;143(6):725-30. | PubMed |
- Daugbjerg P, Brenøe E, Forchhammer H, Frederiksen B, Glazowski MJ, Ibsen KK, Knabe N, Leth H, Marner B, Pedersen FK, et al. A comparison between nebulized terbutaline, nebulized corticosteroid and systemic corticosteroid for acute wheezing in children up to 18 months of age. Acta Paediatr. 1993 Jun-Jul;82(6-7):547-51. | PubMed |
- Jartti T, Lehtinen P, Vanto T, Hartiala J, Vuorinen T, Mäkelä MJ, Ruuskanen O. Evaluation of the efficacy of prednisolone in early wheezing induced by rhinovirus or respiratory syncytial virus. Pediatr Infect Dis J. 2006 Jun;25(6):482-8. | PubMed |
- Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses SW. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics. 1983 Jan;71(1):13-8. | PubMed |
- Teeratakulpisarn J, Limwattananon C, Tanupattarachai S, Limwattananon S, Teeratakulpisarn S, Kosalaraksa P. Efficacy of dexamethasone injection for acute bronchiolitis in hospitalized children: a randomized, double-blind, placebo-controlled trial. Pediatr Pulmonol. 2007 May;42(5):433-9. | PubMed |
- Rachelefsky G. Treating exacerbations of asthma in children: the role of systemic corticosteroids. Pediatrics. 2003 Aug;112(2):382-97. | PubMed |
- Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014 Nov;134(5):e1474-502. | CrossRef | PubMed |
- Ricci V, Delgado Nunes V, Murphy MS, Cunningham S; Guideline Development Group and Technical Team. Bronchiolitis in children: summary of NICE guidance. BMJ. 2015 Jun 2;350:h2305. | CrossRef | PubMed |
- Fernandes RM, Bialy LM, Vandermeer B, Tjosvold L, Plint AC, Patel H, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev. 2013 Jun 4;(6):CD004878. | CrossRef | PubMed |
- Hartling L, Fernandes RM, Bialy L, Milne A, Johnson D, Plint A, et al. Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis. BMJ. 2011 Apr 6;342:d1714. | CrossRef | PubMed |
- Barlas C, Kiper N, Göçmen A, Ozçelik U, Dilber E, Anadol D, et al. Racemic adrenaline and other treatment regimens in mild and moderate bronchiolitis. Cocuk Sagligi Ve Hastaliklari Dergisi 1998;41(2):155–66.
- Gómez-y-López RE, Hernández-Sierra JF, Torres-Ruvalcaba BA, Martínez-Puente E, del Carmen Martínez-Garcia M. [Comparative clinical study of dexamethasone vs. nebulized salbutamol in acute bronchiolitis]. Gac Med Mex. 2007 May-Jun;143(3):189-92. | PubMed |
- Kuyucu S, Unal S, Kuyucu N, Yilgor E. Additive effects of dexamethasone in nebulized salbutamol or L-epinephrine treated infants with acute bronchiolitis. Pediatr Int. 2004 Oct;46(5):539-44. | PubMed |
- Mesquita M, Castro-Rodríguez JA, Heinichen L, Fariña E, Iramain R. Single oral dose of dexamethasone in outpatients with bronchiolitis: a placebo controlled trial. Allergol Immunopathol (Madr). 2009 Mar-Apr;37(2):63-7. | PubMed |
- Plint AC, Johnson DW, Patel H, Wiebe N, Correll R, Brant R, Mitton C, Gouin S, Bhatt M, Joubert G, Black KJ, Turner T, Whitehouse S, Klassen TP; Pediatric Emergency Research Canada (PERC). Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med. 2009 May 14;360(20):2079-89. | CrossRef | PubMed |
- Zhang L, Ferruzzi E, Bonfanti T, Auler MI, D'avila NE, Faria CS, Costa MM. Long and short-term effect of prednisolone in hospitalized infants with acute bronchiolitis. J Paediatr Child Health. 2003 Sep-Oct;39(7):548-51. | PubMed |
- Lisa Hartlin, Terry Klassen, Dominic Allain, Ricardo Fernandes, Stephen Freedman, David Johnson, et al. Interventions for bronchiolitis in the acute care setting: a systematic review and network meta-analysis. PROSPERO 2016:CRD42016048625. | Link |
 Davison C, Ventre KM, Luchetti M, Randolph AG. Efficacy of interventions for bronchiolitis in critically ill infants: a systematic review and meta-analysis. Pediatr Crit Care Med. 2004 Sep;5(5):482-9. | PubMed | PMC |
Davison C, Ventre KM, Luchetti M, Randolph AG. Efficacy of interventions for bronchiolitis in critically ill infants: a systematic review and meta-analysis. Pediatr Crit Care Med. 2004 Sep;5(5):482-9. | PubMed | PMC | Garrison MM, Christakis DA, Harvey E, Cummings P, Davis RL. Systemic corticosteroids in infant bronchiolitis: A meta-analysis. Pediatrics. 2000 Apr;105(4):E44. | PubMed |
Garrison MM, Christakis DA, Harvey E, Cummings P, Davis RL. Systemic corticosteroids in infant bronchiolitis: A meta-analysis. Pediatrics. 2000 Apr;105(4):E44. | PubMed | King VJ, Viswanathan M, Bordley WC, Jackman AM, Sutton SF, Lohr KN, et al. Pharmacologic treatment of bronchiolitis in infants and children: a systematic review. Arch Pediatr Adolesc Med. 2004 Feb;158(2):127-37. | PubMed |
King VJ, Viswanathan M, Bordley WC, Jackman AM, Sutton SF, Lohr KN, et al. Pharmacologic treatment of bronchiolitis in infants and children: a systematic review. Arch Pediatr Adolesc Med. 2004 Feb;158(2):127-37. | PubMed | McGee S, Hirschmann J. Use of corticosteroids in treating infectious diseases. Arch Intern Med. 2008 May 26;168(10):1034-46. | CrossRef | PubMed |
McGee S, Hirschmann J. Use of corticosteroids in treating infectious diseases. Arch Intern Med. 2008 May 26;168(10):1034-46. | CrossRef | PubMed | Berger I, Argaman Z, Schwartz SB, Segal E, Kiderman A, Branski D, Kerem E. Efficacy of corticosteroids in acute bronchiolitis: short-term and long-term follow-up. Pediatr Pulmonol. 1998 Sep;26(3):162-6. | PubMed |
Berger I, Argaman Z, Schwartz SB, Segal E, Kiderman A, Branski D, Kerem E. Efficacy of corticosteroids in acute bronchiolitis: short-term and long-term follow-up. Pediatr Pulmonol. 1998 Sep;26(3):162-6. | PubMed | Buckingham SC, Jafri HS, Bush AJ, Carubelli CM, Sheeran P, Hardy RD, Ottolini MG, Ramilo O, DeVincenzo JP. A randomized, double-blind, placebo-controlled trial of dexamethasone in severe respiratory syncytial virus (RSV) infection: effects on RSV quantity and clinical outcome. J Infect Dis. 2002 May 1;185(9):1222-8 | PubMed |
Buckingham SC, Jafri HS, Bush AJ, Carubelli CM, Sheeran P, Hardy RD, Ottolini MG, Ramilo O, DeVincenzo JP. A randomized, double-blind, placebo-controlled trial of dexamethasone in severe respiratory syncytial virus (RSV) infection: effects on RSV quantity and clinical outcome. J Infect Dis. 2002 May 1;185(9):1222-8 | PubMed | Dabbous IA, Tkachyk JS, Stamm SJ. A double blind study on the effects of corticosteroids in the treatment of bronchiolitis. Pediatrics. 1966 Mar;37(3):477-84. | PubMed |
Dabbous IA, Tkachyk JS, Stamm SJ. A double blind study on the effects of corticosteroids in the treatment of bronchiolitis. Pediatrics. 1966 Mar;37(3):477-84. | PubMed | De Boeck K, Van der Aa N, Van Lierde S, Corbeel L, Eeckels R. Respiratory syncytial virus bronchiolitis: a double-blind dexamethasone efficacy study. J Pediatr. 1997 Dec;131(6):919-21. | PubMed |
De Boeck K, Van der Aa N, Van Lierde S, Corbeel L, Eeckels R. Respiratory syncytial virus bronchiolitis: a double-blind dexamethasone efficacy study. J Pediatr. 1997 Dec;131(6):919-21. | PubMed | Goebel J, Estrada B, Quinonez J, Nagji N, Sanford D, Boerth RC. Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr (Phila). 2000 Apr;39(4):213-20. | PubMed |
Goebel J, Estrada B, Quinonez J, Nagji N, Sanford D, Boerth RC. Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr (Phila). 2000 Apr;39(4):213-20. | PubMed | Klassen TP, Sutcliffe T, Watters LK, Wells GA, Allen UD, Li MM. Dexamethasone in salbutamol-treated inpatients with acute bronchiolitis: a randomized, controlled trial. J Pediatr. 1997 Feb;130(2):191-6. | PubMed |
Klassen TP, Sutcliffe T, Watters LK, Wells GA, Allen UD, Li MM. Dexamethasone in salbutamol-treated inpatients with acute bronchiolitis: a randomized, controlled trial. J Pediatr. 1997 Feb;130(2):191-6. | PubMed | Roosevelt G, Sheehan K, Grupp-Phelan J, Tanz RR, Listernick R. Dexamethasone in bronchiolitis: a randomised controlled trial. Lancet. 1996 Aug 3;348(9023):292-5. | PubMed |
Roosevelt G, Sheehan K, Grupp-Phelan J, Tanz RR, Listernick R. Dexamethasone in bronchiolitis: a randomised controlled trial. Lancet. 1996 Aug 3;348(9023):292-5. | PubMed | Schuh S, Coates AL, Binnie R, Allin T, Goia C, Corey M, Dick PT. Efficacy of oral dexamethasone in outpatients with acute bronchiolitis. J Pediatr. 2002 Jan;140(1):27-32.
| PubMed |
Schuh S, Coates AL, Binnie R, Allin T, Goia C, Corey M, Dick PT. Efficacy of oral dexamethasone in outpatients with acute bronchiolitis. J Pediatr. 2002 Jan;140(1):27-32.
| PubMed | Springer C, Bar-Yishay E, Uwayyed K, Avital A, Vilozni D, Godfrey S. Corticosteroids do not affect the clinical or physiological status of infants with bronchiolitis. Pediatr Pulmonol. 1990;9(3):181-5. | PubMed |
Springer C, Bar-Yishay E, Uwayyed K, Avital A, Vilozni D, Godfrey S. Corticosteroids do not affect the clinical or physiological status of infants with bronchiolitis. Pediatr Pulmonol. 1990;9(3):181-5. | PubMed | van Woensel JB, Wolfs TF, van Aalderen WM, Brand PL, Kimpen JL. Randomised double blind placebo controlled trial of prednisolone in children admitted to hospital with respiratory syncytial virus bronchiolitis. Thorax. 1997 Jul;52(7):634-7. | PubMed | PMC |
van Woensel JB, Wolfs TF, van Aalderen WM, Brand PL, Kimpen JL. Randomised double blind placebo controlled trial of prednisolone in children admitted to hospital with respiratory syncytial virus bronchiolitis. Thorax. 1997 Jul;52(7):634-7. | PubMed | PMC | van Woensel JB, Kimpen JL, Sprikkelman AB, Ouwehand A, van Aalderen WM. Long-term effects of prednisolone in the acute phase of bronchiolitis caused by respiratory syncytial virus. Pediatr Pulmonol. 2000 Aug;30(2):92-6 | PubMed |
van Woensel JB, Kimpen JL, Sprikkelman AB, Ouwehand A, van Aalderen WM. Long-term effects of prednisolone in the acute phase of bronchiolitis caused by respiratory syncytial virus. Pediatr Pulmonol. 2000 Aug;30(2):92-6 | PubMed | van Woensel JB, van Aalderen WM, de Weerd W, Jansen NJ, van Gestel JP, Markhorst DG, van Vught AJ, Bos AP, Kimpen JL. Dexamethasone for treatment of patients mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus. Thorax. 2003 May;58(5):383-7. | PubMed | PMC |
van Woensel JB, van Aalderen WM, de Weerd W, Jansen NJ, van Gestel JP, Markhorst DG, van Vught AJ, Bos AP, Kimpen JL. Dexamethasone for treatment of patients mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus. Thorax. 2003 May;58(5):383-7. | PubMed | PMC | Bülow SM, Nir M, Levin E, Friis B, Thomsen LL, Nielsen JE, Holm JC, Moller T, Bonde-Hansen ME, Nielsen HE. Prednisolone treatment of respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics. 1999 Dec;104(6):e77. | PubMed |
Bülow SM, Nir M, Levin E, Friis B, Thomsen LL, Nielsen JE, Holm JC, Moller T, Bonde-Hansen ME, Nielsen HE. Prednisolone treatment of respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics. 1999 Dec;104(6):e77. | PubMed | Connolly JH, Field CM, Glasgow JF, Slattery CM, MacLynn DM. A double blind trial of prednisolone in epidemic bronchiolitis due to respiratory syncytial virus. Acta Paediatr Scand. 1969 Mar;58(2):116-20. | PubMed |
Connolly JH, Field CM, Glasgow JF, Slattery CM, MacLynn DM. A double blind trial of prednisolone in epidemic bronchiolitis due to respiratory syncytial virus. Acta Paediatr Scand. 1969 Mar;58(2):116-20. | PubMed | Corneli HM, Zorc JJ, Mahajan P, Shaw KN, Holubkov R, Reeves SD, Ruddy RM, Malik B, Nelson KA, Bregstein JS, Brown KM, Denenberg MN, Lillis KA, Cimpello LB, Tsung JW, Borgialli DA, Baskin MN, Teshome G, Goldstein MA, Monroe D, Dean JM, Kuppermann N; Bronchiolitis Study Group of the Pediatric Emergency Care Applied Research Network (PECARN). A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med. 2007 Jul 26;357(4):331-9. Erratum in: N Engl J Med. 2008 Oct 30;359(18):1972. Majahan, Prashant [corrected to Mahajan, Prashant]. | PubMed |
Corneli HM, Zorc JJ, Mahajan P, Shaw KN, Holubkov R, Reeves SD, Ruddy RM, Malik B, Nelson KA, Bregstein JS, Brown KM, Denenberg MN, Lillis KA, Cimpello LB, Tsung JW, Borgialli DA, Baskin MN, Teshome G, Goldstein MA, Monroe D, Dean JM, Kuppermann N; Bronchiolitis Study Group of the Pediatric Emergency Care Applied Research Network (PECARN). A multicenter, randomized, controlled trial of dexamethasone for bronchiolitis. N Engl J Med. 2007 Jul 26;357(4):331-9. Erratum in: N Engl J Med. 2008 Oct 30;359(18):1972. Majahan, Prashant [corrected to Mahajan, Prashant]. | PubMed | Csonka P, Kaila M, Laippala P, Iso-Mustajärvi M, Vesikari T, Ashorn P. Oral prednisolone in the acute management of children age 6 to 35 months with viral respiratory infection-induced lower airway disease: a randomized, placebo-controlled trial. J Pediatr. 2003 Dec;143(6):725-30. | PubMed |
Csonka P, Kaila M, Laippala P, Iso-Mustajärvi M, Vesikari T, Ashorn P. Oral prednisolone in the acute management of children age 6 to 35 months with viral respiratory infection-induced lower airway disease: a randomized, placebo-controlled trial. J Pediatr. 2003 Dec;143(6):725-30. | PubMed | Daugbjerg P, Brenøe E, Forchhammer H, Frederiksen B, Glazowski MJ, Ibsen KK, Knabe N, Leth H, Marner B, Pedersen FK, et al. A comparison between nebulized terbutaline, nebulized corticosteroid and systemic corticosteroid for acute wheezing in children up to 18 months of age. Acta Paediatr. 1993 Jun-Jul;82(6-7):547-51. | PubMed |
Daugbjerg P, Brenøe E, Forchhammer H, Frederiksen B, Glazowski MJ, Ibsen KK, Knabe N, Leth H, Marner B, Pedersen FK, et al. A comparison between nebulized terbutaline, nebulized corticosteroid and systemic corticosteroid for acute wheezing in children up to 18 months of age. Acta Paediatr. 1993 Jun-Jul;82(6-7):547-51. | PubMed | Jartti T, Lehtinen P, Vanto T, Hartiala J, Vuorinen T, Mäkelä MJ, Ruuskanen O. Evaluation of the efficacy of prednisolone in early wheezing induced by rhinovirus or respiratory syncytial virus. Pediatr Infect Dis J. 2006 Jun;25(6):482-8.
| PubMed |
Jartti T, Lehtinen P, Vanto T, Hartiala J, Vuorinen T, Mäkelä MJ, Ruuskanen O. Evaluation of the efficacy of prednisolone in early wheezing induced by rhinovirus or respiratory syncytial virus. Pediatr Infect Dis J. 2006 Jun;25(6):482-8.
| PubMed | Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses SW. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics. 1983 Jan;71(1):13-8. | PubMed |
Tal A, Bavilski C, Yohai D, Bearman JE, Gorodischer R, Moses SW. Dexamethasone and salbutamol in the treatment of acute wheezing in infants. Pediatrics. 1983 Jan;71(1):13-8. | PubMed | Teeratakulpisarn J, Limwattananon C, Tanupattarachai S, Limwattananon S, Teeratakulpisarn S, Kosalaraksa P. Efficacy of dexamethasone injection for acute bronchiolitis in hospitalized children: a randomized, double-blind, placebo-controlled trial. Pediatr Pulmonol. 2007 May;42(5):433-9. | PubMed |
Teeratakulpisarn J, Limwattananon C, Tanupattarachai S, Limwattananon S, Teeratakulpisarn S, Kosalaraksa P. Efficacy of dexamethasone injection for acute bronchiolitis in hospitalized children: a randomized, double-blind, placebo-controlled trial. Pediatr Pulmonol. 2007 May;42(5):433-9. | PubMed | Rachelefsky G. Treating exacerbations of asthma in children: the role of systemic corticosteroids. Pediatrics. 2003 Aug;112(2):382-97. | PubMed |
Rachelefsky G. Treating exacerbations of asthma in children: the role of systemic corticosteroids. Pediatrics. 2003 Aug;112(2):382-97. | PubMed | Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014 Nov;134(5):e1474-502. | CrossRef | PubMed |
Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, Gadomski AM, et al. Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics. 2014 Nov;134(5):e1474-502. | CrossRef | PubMed | Ricci V, Delgado Nunes V, Murphy MS, Cunningham S; Guideline Development Group and Technical Team. Bronchiolitis in children: summary of NICE guidance. BMJ. 2015 Jun 2;350:h2305. | CrossRef | PubMed |
Ricci V, Delgado Nunes V, Murphy MS, Cunningham S; Guideline Development Group and Technical Team. Bronchiolitis in children: summary of NICE guidance. BMJ. 2015 Jun 2;350:h2305. | CrossRef | PubMed | Fernandes RM, Bialy LM, Vandermeer B, Tjosvold L, Plint AC, Patel H, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev. 2013 Jun 4;(6):CD004878. | CrossRef | PubMed |
Fernandes RM, Bialy LM, Vandermeer B, Tjosvold L, Plint AC, Patel H, et al. Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database Syst Rev. 2013 Jun 4;(6):CD004878. | CrossRef | PubMed | Hartling L, Fernandes RM, Bialy L, Milne A, Johnson D, Plint A, et al. Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis. BMJ. 2011 Apr 6;342:d1714. | CrossRef | PubMed |
Hartling L, Fernandes RM, Bialy L, Milne A, Johnson D, Plint A, et al. Steroids and bronchodilators for acute bronchiolitis in the first two years of life: systematic review and meta-analysis. BMJ. 2011 Apr 6;342:d1714. | CrossRef | PubMed | Barlas C, Kiper N, Göçmen A, Ozçelik U, Dilber E, Anadol D, et al. Racemic adrenaline and other treatment regimens in mild and moderate bronchiolitis. Cocuk Sagligi Ve Hastaliklari Dergisi 1998;41(2):155–66.
Barlas C, Kiper N, Göçmen A, Ozçelik U, Dilber E, Anadol D, et al. Racemic adrenaline and other treatment regimens in mild and moderate bronchiolitis. Cocuk Sagligi Ve Hastaliklari Dergisi 1998;41(2):155–66.  Gómez-y-López RE, Hernández-Sierra JF, Torres-Ruvalcaba BA, Martínez-Puente E, del Carmen Martínez-Garcia M. [Comparative clinical study of dexamethasone vs. nebulized salbutamol in acute bronchiolitis]. Gac Med Mex. 2007 May-Jun;143(3):189-92. | PubMed |
Gómez-y-López RE, Hernández-Sierra JF, Torres-Ruvalcaba BA, Martínez-Puente E, del Carmen Martínez-Garcia M. [Comparative clinical study of dexamethasone vs. nebulized salbutamol in acute bronchiolitis]. Gac Med Mex. 2007 May-Jun;143(3):189-92. | PubMed | Kuyucu S, Unal S, Kuyucu N, Yilgor E. Additive effects of dexamethasone in nebulized salbutamol or L-epinephrine treated infants with acute bronchiolitis. Pediatr Int. 2004 Oct;46(5):539-44. | PubMed |
Kuyucu S, Unal S, Kuyucu N, Yilgor E. Additive effects of dexamethasone in nebulized salbutamol or L-epinephrine treated infants with acute bronchiolitis. Pediatr Int. 2004 Oct;46(5):539-44. | PubMed | Mesquita M, Castro-Rodríguez JA, Heinichen L, Fariña E, Iramain R. Single oral dose of dexamethasone in outpatients with bronchiolitis: a placebo controlled trial. Allergol Immunopathol (Madr). 2009 Mar-Apr;37(2):63-7. | PubMed |
Mesquita M, Castro-Rodríguez JA, Heinichen L, Fariña E, Iramain R. Single oral dose of dexamethasone in outpatients with bronchiolitis: a placebo controlled trial. Allergol Immunopathol (Madr). 2009 Mar-Apr;37(2):63-7. | PubMed | Plint AC, Johnson DW, Patel H, Wiebe N, Correll R, Brant R, Mitton C, Gouin S, Bhatt M, Joubert G, Black KJ, Turner T, Whitehouse S, Klassen TP; Pediatric Emergency Research Canada (PERC). Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med. 2009 May 14;360(20):2079-89. | CrossRef | PubMed |
Plint AC, Johnson DW, Patel H, Wiebe N, Correll R, Brant R, Mitton C, Gouin S, Bhatt M, Joubert G, Black KJ, Turner T, Whitehouse S, Klassen TP; Pediatric Emergency Research Canada (PERC). Epinephrine and dexamethasone in children with bronchiolitis. N Engl J Med. 2009 May 14;360(20):2079-89. | CrossRef | PubMed | Zhang L, Ferruzzi E, Bonfanti T, Auler MI, D'avila NE, Faria CS, Costa MM. Long and short-term effect of prednisolone in hospitalized infants with acute bronchiolitis. J Paediatr Child Health. 2003 Sep-Oct;39(7):548-51. | PubMed |
Zhang L, Ferruzzi E, Bonfanti T, Auler MI, D'avila NE, Faria CS, Costa MM. Long and short-term effect of prednisolone in hospitalized infants with acute bronchiolitis. J Paediatr Child Health. 2003 Sep-Oct;39(7):548-51. | PubMed | Lisa Hartlin, Terry Klassen, Dominic Allain, Ricardo Fernandes, Stephen Freedman, David Johnson, et al. Interventions for bronchiolitis in the acute care setting: a systematic review and network meta-analysis. PROSPERO 2016:CRD42016048625. | Link |
Lisa Hartlin, Terry Klassen, Dominic Allain, Ricardo Fernandes, Stephen Freedman, David Johnson, et al. Interventions for bronchiolitis in the acute care setting: a systematic review and network meta-analysis. PROSPERO 2016:CRD42016048625. | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








