Abstract
INTRODUCTION
Psoriatic arthritis is an inflammatory arthritis without a clear etiology. Biological therapy is key for its treatment, especially in more complex patients. There are several alternatives for biological treatment, but due to its high cost, it is important to evaluate their real effectiveness.
METHODS
To answer this question we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others. We extracted data from the systematic reviews, reanalyzed data of primary studies, conducted a meta-analysis and generated a summary of findings table using the GRADE approach.
RESULTS AND CONCLUSIONS
We identified 12 systematic reviews including three randomized trials overall. We concluded ustekinumab leads to clinical improvement in psoriatic arthritis, and probably is not associated to severe adverse effects.
Problem
Psoriatic arthritis is an inflammatory arthritis without a clear etiology. It is associated with psoriasis, and most are seronegative for rheumatoid factor. Currently, there are several treatment alternatives for this condition, many of them extrapolated from drugs proven in rheumatoid arthritis. The efficacy of new medications in psoriatic arthritis has been studied in greater depth recently, especially for patients resistant to initial treatment, either with non-steroidal anti-inflammatories, disease modifying drugs (e.g. methotrexate) or biological medication (e.g. TNF inhibitors). Among these new alternatives is ustekinumab, an IL-12 and IL-23 inhibitor.
Methods
To answer the question, we used Epistemonikos, the largest database of systematic reviews in health, which is maintained by screening multiple information sources, including MEDLINE, EMBASE, Cochrane, among others, to identify systematic reviews and their included primary studies. We extracted data from the identified reviews and reanalyzed data from primary studies included in those reviews. With this information, we generated a structured summary denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos) using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies when it is possible, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found twelve systematic reviews [1],[2],[3],[4],[5],[6],[7],[8],[9],[10],[11],[12], that include three primary studies, reported in six references [13],[14],[15],[16],[17],[18]. All of them are randomized controlled trials. This table and the summary in general are based on the latter. |
|
What types of patients were included* |
All of these trials included adult patients with clinical psoriatic arthritis diagnosis and active disease (three or more tender joints, plus C-reactive protein of 3 mg/L [13],[14] or 15 mg/L [15]) and inadequate response or poor tolerance to the use of non-steroidal anti-inflammatories or disease modifying drugs in addition to plaque psoriasis with active lesion or previous history of disease. One trial [13] excluded patients with previous anti-TNF use. On the other hand, the other two trials [14],[15] did include patients with inadequate response or poor tolerance to the use of biological therapies. |
|
What types of interventions were included* |
Two trials [13],[14] included subcutaneous ustekinumab 45 mg or 90 mg at baseline, then at week four, then every twelve weeks. One trial [15] did not report the dose or administration scheme. All trials compared against placebo. |
|
What types of outcomes |
The outcomes were pooled by the different systematic reviews as follows:
|
* The information about primary studies is extracted from the systematic reviews identified, unless otherwise specified.
Summary of Findings
The information on the effects of ustekinumab is based on three randomized trials that included 1073 patients overall [13],[14],[15]. Two trials reported ACR 20 , HAQ-DI, PASI-75 and DAS-28 [13],[14]. Three trials reported serious adverse events [13],[14],[15].
The summary of findings is the following:
- Ustekinumab improves ACR 20 in psoriatic arthritis. The certainty of the evidence is high.
- Ustekinumab improves PASI 75 in psoriatic arthritis. The certainty of the evidence is high.
- Ustekinumab probably leads to little or no difference in serious adverse events in psoriatic arthritis. The certainty of the evidence is moderate.
- Ustekinumab improves DAS-28 in psoriatic arthritis. The certainty of the evidence is high.
- Ustekinumab leads to an improvement of doubtful clinical relevance in HAQ-DI in psoriatic arthritis. The certainty of the evidence is high.
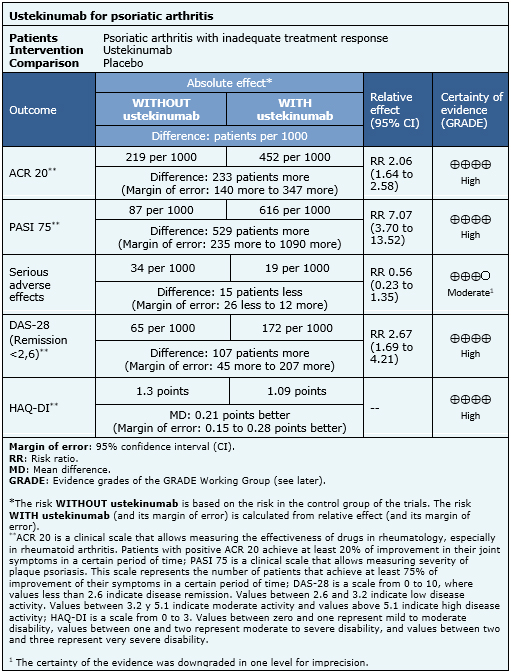
| Following the link to access the interactive version of this table (Interactive Summary of Findings – iSoF) |

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| Resource considerations |
|
| What would patients and their doctors think about this intervention |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
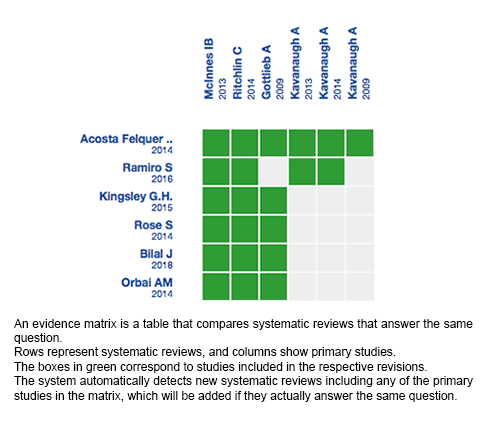
Follow the link to access the interactive version: Ustekinumab for psoriatic arthritis
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier.
After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
This article is part of the Epistemonikos Evidence Synthesis project. It is elaborated with a pre-established methodology, following rigorous methodological standards and internal peer review process. Each of these articles corresponds to a summary, denominated FRISBEE (Friendly Summary of Body of Evidence using Epistemonikos), whose main objective is to synthesize the body of evidence for a specific question, with a friendly format to clinical professionals. Its main resources are based on the evidence matrix of Epistemonikos and analysis of results using GRADE methodology. Further details of the methods for developing this FRISBEE are described here (http://dx.doi.org/10.5867/medwave.2014.06.5997)
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
Potential conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
La artritis psoriásica es una artritis inflamatoria sin una clara etiología, con el tratamiento biológico como un pilar fundamental en pacientes más complejos. Existen varias alternativas para tratamiento biológico, debido a su alto costo, es importante evaluar la real efectividad de estos para un buen tratamiento.
MÉTODOS
Para responder esta pregunta utilizamos Epistemonikos, la mayor base de datos de revisiones sistemáticas en salud a nivel mundial, la cual es mantenida mediante búsquedas en múltiples fuentes de información, incluyendo MEDLINE, EMBASE, Cochrane, entre otras. Extrajimos los datos desde las revisiones identificadas, reanalizamos los datos de los estudios primarios, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE.
RESULTADOS Y CONCLUSIONES
Identificamos 12 revisiones sistemáticas que en conjunto incluyen tres ensayos aleatorizados. Concluimos que el ustekinumab logra una mejoría clínica en pacientes con psoriasis, y probablemente no se asocia a efectos adversos graves.
 Authors:
Soledad Venegas-Iribarren[1,2], Romina Andino-Navarrete[2,3]
Authors:
Soledad Venegas-Iribarren[1,2], Romina Andino-Navarrete[2,3]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Dermatología, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
E-mail: rominaandino@gmail.com
Author address:
[1] Centro Evidencia UC Pontificia Universidad Católica de Chile Centro de Innovación UC Anacleto Angelini Avda.Vicuña Mackenna 4860 Macul Santiago Chile

Citation: Venegas-Iribarren S, Andino-Navarrete R. Is ustekinumab effective for psoriatic arthritis with insufficient response to initial treatment?. Medwave 2018 Mar-Abr;18(2):e7173 doi: 10.5867/medwave.2018.02.7173
Submission date: 23/11/2017
Acceptance date: 4/12/2017
Publication date: 8/3/2018
Origin: This article is a product of the Evidence Synthesis Project of Epistemonikos Fundation, in collaboration with Medwave for its publication.
Type of review: Non-blinded peer review by members of the methodological team of Epistemonikos Evidence Synthesis Project.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Acosta Felquer ML, Coates LC, Soriano ER, Ranza R, Espinoza LR, Helliwell PS, FitzGerald O, McHugh N, Roussou E, Mease PJ. Drug therapies for peripheral joint disease in psoriatic arthritis: a systematic review. J Rheumatol. 2014 Nov;41(11):2277-85. | CrossRef | PubMed |
- Bilal J, Riaz IB, Kamal MU, Elyan M, Sudano D, Khan MA. A Systematic Review and Meta-analysis of Efficacy and Safety of Novel Interleukin Inhibitors in the Management of Psoriatic Arthritis. J Clin Rheumatol. 2017 Sep 19. | CrossRef | PubMed |
- Boehncke WH, Alvarez Martinez D, Solomon JA, Gottlieb AB. Safety and efficacy of therapies for skin symptoms of psoriasis in patients with psoriatic arthritis: a systematic review. J Rheumatol. 2014 Nov;41(11):2301-5. | CrossRef | PubMed |
- Kingsley G.H., Scott D.L.. Assessing the effectiveness of synthetic and biologic disease-modifying antirheumatic drugs in psoriatic arthritis - A systematic review. Psoriasis: Targets and Therapy. 2015;5:71-81.
- Ramiro S, Smolen JS, Landewé R, van der Heijde D, Dougados M, Emery P, de Wit M, Cutolo M, Oliver S, Gossec L. Pharmacological treatment of psoriatic arthritis: a systematic literature review for the 2015 update of the EULAR recommendations for the management of psoriatic arthritis. Ann Rheum Dis. 2016 Mar;75(3):490-8. | CrossRef | PubMed |
- Rose S, Toloza S, Bautista-Molano W, Helliwell PS; GRAPPA Dactylitis Study Group. Comprehensive treatment of dactylitis in psoriatic arthritis. J Rheumatol. 2014 Nov;41(11):2295-300. | CrossRef | PubMed |
- Ungprasert P, Thongprayoon C, Davis JM 3rd. Indirect comparisons of the efficacy of subsequent biological agents in patients with psoriatic arthritis with an inadequate response to tumor necrosis factor inhibitors: a meta-analysis. Clin Rheumatol. 2016 Jul;35(7):1795-803. | CrossRef | PubMed |
- Ungprasert P, Thongprayoon C, Davis JM 3rd. Indirect comparisons of the efficacy of biological agents in patients with psoriatic arthritis with an inadequate response to traditional disease-modifying anti-rheumatic drugs or to non-steroidal anti-inflammatory drugs: A meta-analysis. Semin Arthritis Rheum. 2016 Feb;45(4):428-38. | CrossRef | PubMed |
- Wu Y, Chen J, Li YH, Ma GZ, Chen JZ, Gao XH, Chen HD. Treatment of psoriasis with interleukin-12/23 monoclonal antibody: a systematic review. Eur J Dermatol. 2012 Jan-Feb;22(1):72-82. | CrossRef | PubMed |
- Ustekinumab (Stelara) Injection [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2016 Nov. | PubMed | Link |
- Song GG, Lee YH. Relative efficacy and safety of apremilast, secukinumab, and ustekinumab for the treatment of psoriatic arthritis. Z Rheumatol. 2017 Aug 8. | CrossRef | PubMed |
- Orbai AM, Weitz J, Siegel EL, Siebert S, Savage LJ, Aydin SZ, Luime JJ, Elkayam O, Neerinckx B, Urbancek S, de Vlam K, Ritchlin CT; GRAPPA Enthesitis Working Group. Systematic review of treatment effectiveness and outcome measures for enthesitis in psoriatic arthritis. J Rheumatol. 2014 Nov;41(11):2290-4. | CrossRef | PubMed |
- McInnes IB, Kavanaugh A, Gottlieb AB, Puig L, Rahman P, Ritchlin C, Brodmerkel C, Li S, Wang Y, Mendelsohn AM, Doyle MK; PSUMMIT 1 Study Group. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013 Aug 31;382(9894):780-9. | CrossRef | PubMed |
- Ritchlin C, Rahman P, Kavanaugh A, McInnes IB, Puig L, Li S, Wang Y, Shen YK, Doyle MK, Mendelsohn AM, Gottlieb AB; PSUMMIT 2 Study Group. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014 Jun;73(6):990-9. | CrossRef | PubMed | PMC |
- Gottlieb A, Menter A, Mendelsohn A, Shen YK, Li S, Guzzo C, Fretzin S, Kunynetz R, Kavanaugh A. Ustekinumab, a human interleukin 12/23 monoclonal antibody, for psoriatic arthritis: randomised, double-blind, placebo-controlled, crossover trial. Lancet. 2009 Feb 21;373(9664):633-40. Erratum in: Lancet. 2009 Apr 18;373(9672):1340. Lancet. 2010 Nov 6;376(9752):1542. | CrossRef | PubMed |
- Kavanaugh A. The efficacy of ustekinumab on the articular and dermatologic manifestations of psoriatic arthritis. Curr Rheumatol Rep. 2009 Aug;11(4):233-4. | PubMed |
- Kavanaugh A, Ritchlin C, Rahman P, Puig L, Gottlieb AB, Li S, Wang Y, Noonan L, Brodmerkel C, Song M, Mendelsohn AM, McInnes IB; PSUMMIT-1 and 2 Study Groups. Ustekinumab, an anti-IL-12/23 p40 monoclonal antibody, inhibits radiographic progression in patients with active psoriatic arthritis: results of an integrated analysis of radiographic data from the phase 3, multicentre, randomised, double-blind, placebo-controlled PSUMMIT-1 and PSUMMIT-2 trials. Ann Rheum Dis. 2014 Jun;73(6):1000-6. | CrossRef | PubMed | PMC |
- Kavanaugh A, Puig L, Gottlieb AB. Efficacy and Safety of Ustekinumab in Patients with Active Psoriatic Arthritis: 2-Year Results from a Phase 3, Multicenter, Double-Blind, Placebo-Controlled Study. Arthritis Rheum. 2013;65(Supple 10):L10.
- American Academy of Dermatology Work Group, Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, Gordon KB, Gottlieb A, Koo JY, Lebwohl M, Leonardi CL, Lim HW, Van Voorhees AS, Beutner KR, Ryan C, Bhushan R. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. Guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions. J Am Acad Dermatol. 2011 Jul;65(1):137-74. | CrossRef | PubMed |
- Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, Finlay AY, Griffiths CE, Jackson K, McHugh NJ, McKenna KE, Reynolds NJ, Ormerod AD; (Chair of Guideline Group). British Association of Dermatologists' guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009 Nov;161(5):987-1019. | CrossRef | PubMed |
- Daudén E, Puig L, Ferrándiz C, Sánchez-Carazo JL, Hernanz-Hermosa JM; Spanish Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Consensus document on the evaluation and treatment of moderate-to-severe psoriasis: Psoriasis Group of the Spanish Academy of Dermatology and Venereology. J Eur Acad Dermatol Venereol. 2016 Mar;30 Suppl 2:1-18. | CrossRef | PubMed |
- Gossec L, Smolen JS, Ramiro S, de Wit M, Cutolo M, Dougados M, Emery P, Landewé R, Oliver S, Aletaha D, Betteridge N, Braun J, Burmester G, Cañete JD, Damjanov N, FitzGerald O, Haglund E, Helliwell P, Kvien TK, Lories R, Luger T, Maccarone M, Marzo-Ortega H, McGonagle D, McInnes IB, Olivieri I, Pavelka K, Schett G, Sieper J, van den Bosch F, Veale DJ, Wollenhaupt J, Zink A, van der Heijde D. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016 Mar;75(3):499-510. | CrossRef | PubMed |
 Acosta Felquer ML, Coates LC, Soriano ER, Ranza R, Espinoza LR, Helliwell PS, FitzGerald O, McHugh N, Roussou E, Mease PJ. Drug therapies for peripheral joint disease in psoriatic arthritis: a systematic review. J Rheumatol. 2014 Nov;41(11):2277-85. | CrossRef | PubMed |
Acosta Felquer ML, Coates LC, Soriano ER, Ranza R, Espinoza LR, Helliwell PS, FitzGerald O, McHugh N, Roussou E, Mease PJ. Drug therapies for peripheral joint disease in psoriatic arthritis: a systematic review. J Rheumatol. 2014 Nov;41(11):2277-85. | CrossRef | PubMed | Bilal J, Riaz IB, Kamal MU, Elyan M, Sudano D, Khan MA. A Systematic Review and Meta-analysis of Efficacy and Safety of Novel Interleukin Inhibitors in the Management of Psoriatic Arthritis. J Clin Rheumatol. 2017 Sep 19. | CrossRef | PubMed |
Bilal J, Riaz IB, Kamal MU, Elyan M, Sudano D, Khan MA. A Systematic Review and Meta-analysis of Efficacy and Safety of Novel Interleukin Inhibitors in the Management of Psoriatic Arthritis. J Clin Rheumatol. 2017 Sep 19. | CrossRef | PubMed | Boehncke WH, Alvarez Martinez D, Solomon JA, Gottlieb AB. Safety and efficacy of therapies for skin symptoms of psoriasis in patients with psoriatic arthritis: a systematic review. J Rheumatol. 2014 Nov;41(11):2301-5. | CrossRef | PubMed |
Boehncke WH, Alvarez Martinez D, Solomon JA, Gottlieb AB. Safety and efficacy of therapies for skin symptoms of psoriasis in patients with psoriatic arthritis: a systematic review. J Rheumatol. 2014 Nov;41(11):2301-5. | CrossRef | PubMed | Kingsley G.H., Scott D.L.. Assessing the effectiveness of synthetic and biologic disease-modifying antirheumatic drugs in psoriatic arthritis - A systematic review. Psoriasis: Targets and Therapy. 2015;5:71-81.
Kingsley G.H., Scott D.L.. Assessing the effectiveness of synthetic and biologic disease-modifying antirheumatic drugs in psoriatic arthritis - A systematic review. Psoriasis: Targets and Therapy. 2015;5:71-81.  Ramiro S, Smolen JS, Landewé R, van der Heijde D, Dougados M, Emery P, de Wit M, Cutolo M, Oliver S, Gossec L. Pharmacological treatment of psoriatic arthritis: a systematic literature review for the 2015 update of the EULAR recommendations for the management of psoriatic arthritis. Ann Rheum Dis. 2016 Mar;75(3):490-8. | CrossRef | PubMed |
Ramiro S, Smolen JS, Landewé R, van der Heijde D, Dougados M, Emery P, de Wit M, Cutolo M, Oliver S, Gossec L. Pharmacological treatment of psoriatic arthritis: a systematic literature review for the 2015 update of the EULAR recommendations for the management of psoriatic arthritis. Ann Rheum Dis. 2016 Mar;75(3):490-8. | CrossRef | PubMed | Rose S, Toloza S, Bautista-Molano W, Helliwell PS; GRAPPA Dactylitis Study Group. Comprehensive treatment of dactylitis in psoriatic arthritis. J Rheumatol. 2014 Nov;41(11):2295-300. | CrossRef | PubMed |
Rose S, Toloza S, Bautista-Molano W, Helliwell PS; GRAPPA Dactylitis Study Group. Comprehensive treatment of dactylitis in psoriatic arthritis. J Rheumatol. 2014 Nov;41(11):2295-300. | CrossRef | PubMed | Ungprasert P, Thongprayoon C, Davis JM 3rd. Indirect comparisons of the efficacy of subsequent biological agents in patients with psoriatic arthritis with an inadequate response to tumor necrosis factor inhibitors: a meta-analysis. Clin Rheumatol. 2016 Jul;35(7):1795-803. | CrossRef | PubMed |
Ungprasert P, Thongprayoon C, Davis JM 3rd. Indirect comparisons of the efficacy of subsequent biological agents in patients with psoriatic arthritis with an inadequate response to tumor necrosis factor inhibitors: a meta-analysis. Clin Rheumatol. 2016 Jul;35(7):1795-803. | CrossRef | PubMed | Ungprasert P, Thongprayoon C, Davis JM 3rd. Indirect comparisons of the efficacy of biological agents in patients with psoriatic arthritis with an inadequate response to traditional disease-modifying anti-rheumatic drugs or to non-steroidal anti-inflammatory drugs: A meta-analysis. Semin Arthritis Rheum. 2016 Feb;45(4):428-38. | CrossRef | PubMed |
Ungprasert P, Thongprayoon C, Davis JM 3rd. Indirect comparisons of the efficacy of biological agents in patients with psoriatic arthritis with an inadequate response to traditional disease-modifying anti-rheumatic drugs or to non-steroidal anti-inflammatory drugs: A meta-analysis. Semin Arthritis Rheum. 2016 Feb;45(4):428-38. | CrossRef | PubMed | Wu Y, Chen J, Li YH, Ma GZ, Chen JZ, Gao XH, Chen HD. Treatment of psoriasis with interleukin-12/23 monoclonal antibody: a systematic review. Eur J Dermatol. 2012 Jan-Feb;22(1):72-82. | CrossRef | PubMed |
Wu Y, Chen J, Li YH, Ma GZ, Chen JZ, Gao XH, Chen HD. Treatment of psoriasis with interleukin-12/23 monoclonal antibody: a systematic review. Eur J Dermatol. 2012 Jan-Feb;22(1):72-82. | CrossRef | PubMed | Ustekinumab (Stelara) Injection [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2016 Nov. | PubMed | Link |
Ustekinumab (Stelara) Injection [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2016 Nov. | PubMed | Link | Song GG, Lee YH. Relative efficacy and safety of apremilast, secukinumab, and
ustekinumab for the treatment of psoriatic arthritis. Z Rheumatol. 2017 Aug 8. | CrossRef | PubMed |
Song GG, Lee YH. Relative efficacy and safety of apremilast, secukinumab, and
ustekinumab for the treatment of psoriatic arthritis. Z Rheumatol. 2017 Aug 8. | CrossRef | PubMed | Orbai AM, Weitz J, Siegel EL, Siebert S, Savage LJ, Aydin SZ, Luime JJ, Elkayam O, Neerinckx B, Urbancek S, de Vlam K, Ritchlin CT; GRAPPA Enthesitis Working Group. Systematic review of treatment effectiveness and outcome measures for enthesitis in psoriatic arthritis. J Rheumatol. 2014 Nov;41(11):2290-4. | CrossRef | PubMed |
Orbai AM, Weitz J, Siegel EL, Siebert S, Savage LJ, Aydin SZ, Luime JJ, Elkayam O, Neerinckx B, Urbancek S, de Vlam K, Ritchlin CT; GRAPPA Enthesitis Working Group. Systematic review of treatment effectiveness and outcome measures for enthesitis in psoriatic arthritis. J Rheumatol. 2014 Nov;41(11):2290-4. | CrossRef | PubMed | McInnes IB, Kavanaugh A, Gottlieb AB, Puig L, Rahman P, Ritchlin C, Brodmerkel C, Li S, Wang Y, Mendelsohn AM, Doyle MK; PSUMMIT 1 Study Group. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013 Aug 31;382(9894):780-9. | CrossRef | PubMed |
McInnes IB, Kavanaugh A, Gottlieb AB, Puig L, Rahman P, Ritchlin C, Brodmerkel C, Li S, Wang Y, Mendelsohn AM, Doyle MK; PSUMMIT 1 Study Group. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet. 2013 Aug 31;382(9894):780-9. | CrossRef | PubMed | Ritchlin C, Rahman P, Kavanaugh A, McInnes IB, Puig L, Li S, Wang Y, Shen YK, Doyle MK, Mendelsohn AM, Gottlieb AB; PSUMMIT 2 Study Group. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014 Jun;73(6):990-9. | CrossRef | PubMed | PMC |
Ritchlin C, Rahman P, Kavanaugh A, McInnes IB, Puig L, Li S, Wang Y, Shen YK, Doyle MK, Mendelsohn AM, Gottlieb AB; PSUMMIT 2 Study Group. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis. 2014 Jun;73(6):990-9. | CrossRef | PubMed | PMC | Gottlieb A, Menter A, Mendelsohn A, Shen YK, Li S, Guzzo C, Fretzin S, Kunynetz R, Kavanaugh A. Ustekinumab, a human interleukin 12/23 monoclonal antibody, for psoriatic arthritis: randomised, double-blind, placebo-controlled, crossover trial. Lancet. 2009 Feb 21;373(9664):633-40. Erratum in: Lancet. 2009 Apr 18;373(9672):1340. Lancet. 2010 Nov 6;376(9752):1542. | CrossRef | PubMed |
Gottlieb A, Menter A, Mendelsohn A, Shen YK, Li S, Guzzo C, Fretzin S, Kunynetz R, Kavanaugh A. Ustekinumab, a human interleukin 12/23 monoclonal antibody, for psoriatic arthritis: randomised, double-blind, placebo-controlled, crossover trial. Lancet. 2009 Feb 21;373(9664):633-40. Erratum in: Lancet. 2009 Apr 18;373(9672):1340. Lancet. 2010 Nov 6;376(9752):1542. | CrossRef | PubMed | Kavanaugh A. The efficacy of ustekinumab on the articular and dermatologic manifestations of psoriatic arthritis. Curr Rheumatol Rep. 2009 Aug;11(4):233-4. | PubMed |
Kavanaugh A. The efficacy of ustekinumab on the articular and dermatologic manifestations of psoriatic arthritis. Curr Rheumatol Rep. 2009 Aug;11(4):233-4. | PubMed | Kavanaugh A, Ritchlin C, Rahman P, Puig L, Gottlieb AB, Li S, Wang Y, Noonan L, Brodmerkel C, Song M, Mendelsohn AM, McInnes IB; PSUMMIT-1 and 2 Study Groups. Ustekinumab, an anti-IL-12/23 p40 monoclonal antibody, inhibits radiographic progression in patients with active psoriatic arthritis: results of an integrated analysis of radiographic data from the phase 3, multicentre, randomised, double-blind, placebo-controlled PSUMMIT-1 and PSUMMIT-2 trials. Ann Rheum Dis.
2014 Jun;73(6):1000-6. | CrossRef | PubMed | PMC |
Kavanaugh A, Ritchlin C, Rahman P, Puig L, Gottlieb AB, Li S, Wang Y, Noonan L, Brodmerkel C, Song M, Mendelsohn AM, McInnes IB; PSUMMIT-1 and 2 Study Groups. Ustekinumab, an anti-IL-12/23 p40 monoclonal antibody, inhibits radiographic progression in patients with active psoriatic arthritis: results of an integrated analysis of radiographic data from the phase 3, multicentre, randomised, double-blind, placebo-controlled PSUMMIT-1 and PSUMMIT-2 trials. Ann Rheum Dis.
2014 Jun;73(6):1000-6. | CrossRef | PubMed | PMC | Kavanaugh A, Puig L, Gottlieb AB. Efficacy and Safety of Ustekinumab in Patients with Active Psoriatic Arthritis: 2-Year Results from a Phase 3, Multicenter, Double-Blind, Placebo-Controlled Study. Arthritis Rheum. 2013;65(Supple 10):L10.
Kavanaugh A, Puig L, Gottlieb AB. Efficacy and Safety of Ustekinumab in Patients with Active Psoriatic Arthritis: 2-Year Results from a Phase 3, Multicenter, Double-Blind, Placebo-Controlled Study. Arthritis Rheum. 2013;65(Supple 10):L10.  American Academy of Dermatology Work Group, Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, Gordon KB, Gottlieb A, Koo JY, Lebwohl M, Leonardi CL, Lim HW, Van Voorhees AS, Beutner KR, Ryan C, Bhushan R. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. Guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions. J Am Acad Dermatol. 2011 Jul;65(1):137-74. | CrossRef | PubMed |
American Academy of Dermatology Work Group, Menter A, Korman NJ, Elmets CA, Feldman SR, Gelfand JM, Gordon KB, Gottlieb A, Koo JY, Lebwohl M, Leonardi CL, Lim HW, Van Voorhees AS, Beutner KR, Ryan C, Bhushan R. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. Guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions. J Am Acad Dermatol. 2011 Jul;65(1):137-74. | CrossRef | PubMed | Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, Finlay AY, Griffiths CE, Jackson K, McHugh NJ, McKenna KE, Reynolds NJ, Ormerod AD; (Chair of Guideline Group). British Association of Dermatologists' guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009 Nov;161(5):987-1019. | CrossRef | PubMed |
Smith CH, Anstey AV, Barker JN, Burden AD, Chalmers RJ, Chandler DA, Finlay AY, Griffiths CE, Jackson K, McHugh NJ, McKenna KE, Reynolds NJ, Ormerod AD; (Chair of Guideline Group). British Association of Dermatologists' guidelines for biologic interventions for psoriasis 2009. Br J Dermatol. 2009 Nov;161(5):987-1019. | CrossRef | PubMed | Daudén E, Puig L, Ferrándiz C, Sánchez-Carazo JL, Hernanz-Hermosa JM; Spanish Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Consensus document on the evaluation and treatment of moderate-to-severe psoriasis: Psoriasis Group of the Spanish Academy of Dermatology and Venereology. J Eur Acad Dermatol Venereol. 2016 Mar;30 Suppl 2:1-18. | CrossRef | PubMed |
Daudén E, Puig L, Ferrándiz C, Sánchez-Carazo JL, Hernanz-Hermosa JM; Spanish Psoriasis Group of the Spanish Academy of Dermatology and Venereology. Consensus document on the evaluation and treatment of moderate-to-severe psoriasis: Psoriasis Group of the Spanish Academy of Dermatology and Venereology. J Eur Acad Dermatol Venereol. 2016 Mar;30 Suppl 2:1-18. | CrossRef | PubMed | Gossec L, Smolen JS, Ramiro S, de Wit M, Cutolo M, Dougados M, Emery P, Landewé R, Oliver S, Aletaha D, Betteridge N, Braun J, Burmester G, Cañete JD, Damjanov N, FitzGerald O, Haglund E, Helliwell P, Kvien TK, Lories R, Luger T, Maccarone M, Marzo-Ortega H, McGonagle D, McInnes IB, Olivieri I, Pavelka K, Schett G, Sieper J, van den Bosch F, Veale DJ, Wollenhaupt J, Zink A, van der Heijde D. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016 Mar;75(3):499-510. | CrossRef | PubMed |
Gossec L, Smolen JS, Ramiro S, de Wit M, Cutolo M, Dougados M, Emery P, Landewé R, Oliver S, Aletaha D, Betteridge N, Braun J, Burmester G, Cañete JD, Damjanov N, FitzGerald O, Haglund E, Helliwell P, Kvien TK, Lories R, Luger T, Maccarone M, Marzo-Ortega H, McGonagle D, McInnes IB, Olivieri I, Pavelka K, Schett G, Sieper J, van den Bosch F, Veale DJ, Wollenhaupt J, Zink A, van der Heijde D. European League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 update. Ann Rheum Dis. 2016 Mar;75(3):499-510. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








