Abstract
Oxygen therapy is used for the treatment of acute coronary syndrome without further discussion. However, the support of this practice in clinical research is scarce, and the real effects of this measure are not known. To answer this question, we searched in Epistemonikos database, which is maintained by screening multiple information sources. We identified five systematic reviews including 12 studies overall, five of which were randomized trials. We extracted data, conducted a meta-analysis and generated a summary of findings table using the GRADE approach. We concluded that using oxygen probably does not decrease pain, and might not make any difference in mortality during an acute coronary syndrome.
Problem
Oxygen therapy has a wide clinical use mainly in patients with cardiac and pulmonary disease. In this context, the use of oxygen in patients with an acute coronary syndrome is considered part of the usual treatment. This practice is supported by pathophysiology, as an increased arterial coronary oxygen concentration reduces myocardial hypoperfusion, the pain caused by this condition, and probably the associated morbimortality. However, other theories suggest that hyperoxia could lead to reduction in coronary flow and an increase in free radicals associated with oxygen, increasing the damage caused by the ischemia. However, the clinical effects of this intervention are not clear.
Methods
We used Epistemonikos database, which is maintained by screening multiple sources of information, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found five systematic reviews [1],[2],[3],[4],[5] including 12 primary studies reported in 20 references [6], [7],[8],[9],[10],[11],[12],[13],[14],[15],[16],[17],[18], [19],[20],[21],[22],[23],[24],[25]. Of these, five studies correspond to randomized controlled trials, reported in 13 references [11],[12],[13],[15],[16],[17],[18],[19],[20], [21],[23],[24],[25]. This table and the summary in general are based on the latter, since the observational studies did not increase the certainty of the existing evidence, nor did they provide relevant additional information. |
|
What types of patients were included |
Two trials included patients with confirmed acute myocardial infarction [23],[25] and three with suspected infarction [11],[12],[13]. Regarding the use of thrombolysis and angioplasty (PCI), two trials used PCI as first line therapy [11],[23]; another trial used PCI as first option in one of the centers while in the other thrombolysis was performed [12]; another trial mentions that it was conducted after the implementation of thrombolysis [25], but does not specify whether it was used as their primary intervention; one trial was conducted in pre-thrombolysis era [13]. The mean age was reported in three of the trials [11], [12],[13] ranging from 56 to 63 years. The same three trials report the average male proportion varied between 74% and 79%. The main reasons for exclusion reported by the trials were heart failure [13],[23],[25]; chronic obstructive pulmonary disease [12],[13]; other pulmonary conditions [13],[23], [25]; cyanosis [12],[25]; and complications of infarction [12],[23]. None of the five trials reported comorbidities of the patients included. |
|
What types of interventions were included |
All of the trials in this summary used facial oxygen mask for oxygen delivery as the intervention. Four of the trials used 100% oxygen [11],[12],[13],[25] but with different oxygen flow; two at 6 L/min [12],[13]; one at 8 L/min [11]; another at 4 L/min [25]. One trial used 45% oxygen with a flow between 3 and 6 L/min [23]. Three trials used ambient air as comparison [11],[23], [25]; one used oxygen to maintain arterial saturation between 93 and 96% [12]; another used oxygen at 21% with a 6 L/min flow [13]. The follow-up time considered by two of the trials [13], [25] was up to the patient's discharge. Another trial followed-up for 30 days [12], another for 10 days [23] and one trial for 6 months [11]. |
|
What types of outcomes |
Outcomes reported in the trials were grouped by the systematic reviews as follows:
|
Summary of findings
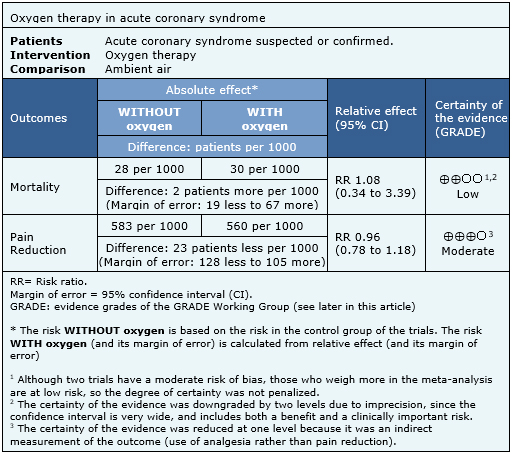
The information on the effects of oxygen on acute coronary syndrome is based on five randomized trials involving 1,123 patients. Four of the trials reported mortality [11],[12],[13],[23] and two trials (250 patients) reported pain estimated as analgesics requirement [13],[25]. The summary of findings is as follows:
- Oxygen therapy probably does not decrease pain during an acute coronary syndrome. The certainty of the evidence is moderate.
- Oxygen therapy might make no difference in mortality during an acute coronary syndrome. The certainty of the evidence is low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
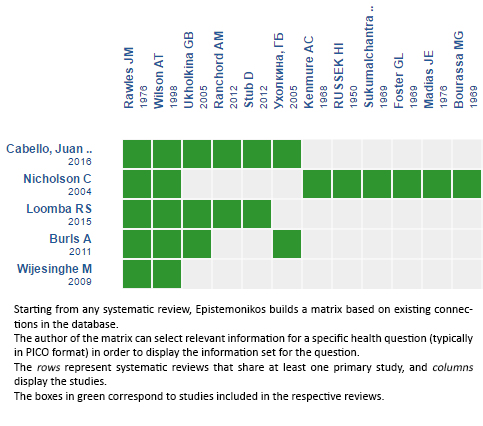
Follow the link to access the interactive version: Oxygen therapy for acute myocardial ischemia
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

La oxigenoterapia es utilizada para el tratamiento del síndrome coronario agudo sin mayor discusión. Sin embargo, el sustento de esta práctica en investigación clínica es escaso, desconociéndose los verdaderos efectos que trae su implementación. Para responder esta interrogante utilizamos la base de datos Epistemonikos, la cual es mantenida mediante búsquedas en múltiples fuentes de información, e identificamos cinco revisiones sistemáticas que en conjunto incluyen doce estudios, de los cuales cinco son estudios aleatorizados. Extrajimos los datos, realizamos un metanálisis y preparamos una tabla de resumen de los resultados utilizando el método GRADE. Concluimos que el uso de oxígeno probablemente no disminuye el dolor, y podría no hacer ninguna diferencia en la mortalidad durante un síndrome coronario agudo.
 Authors:
José Tomás Bennett-Laso[1,2], Tomás Kramer-Urrutia[1,2], Gabriel Rada[2,3,4,5,6]
Authors:
José Tomás Bennett-Laso[1,2], Tomás Kramer-Urrutia[1,2], Gabriel Rada[2,3,4,5,6]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
E-mail: radagabriel@epistemonikos.org
Author address:
[1] Facultad de Medicina Pontificia Universidad Católica de Chile Diagonal Paraguay 476 Santiago Centro Chile.

Citation: Bennett-Laso JT, Kramer-Urrutia T, Rada G. Should we administer oxygen during an acute coronary syndrome?. Medwave2017;17(Suppl1):e6892 doi: 10.5867/medwave.2017.6892
Submission date: 29/12/2016
Acceptance date: 30/12/2016
Publication date: 29/3/2017

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Burls A, Cabello JB, Emparanza JI, Bayliss S, Quinn T. Oxygen therapy for acute myocardial infarction: a systematic review and meta-analysis. Emerg Med J. 2011 Nov;28(11):917-23 | CrossRef | PubMed |
- Cabello JB, Burls A, Emparanza JI, Bayliss SE, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2016 Dec 19;12:CD007160 | PubMed |
- Loomba RS, Nijhawan K, Aggarwal S, Arora RR. Oxygen in the Setting of Acute Myocardial Infarction: Is It Really a Breath of Fresh Air? J Cardiovasc Pharmacol Ther. 2016 Mar;21(2):143-9 | CrossRef | PubMed |
- Nicholson C. A systematic review of the effectiveness of oxygen in reducing acute myocardial ischaemia. J Clin Nurs. 2004 Nov;13(8):996-1007 | PubMed |
- Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Weatherall M, Beasley R. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart. 2009 Mar;95(3):198-202 | CrossRef | PubMed |
- Bourassa MG, Campeau L, Bois MA, Rico O. The effects of inhalation of 100 percent oxygen on myocardial lactate metabolism in coronary heart disease. Am J Cardiol. 1969 Aug;24(2):172-7 | PubMed |
- Foster GL, Casten GG, Reeves TJ. The effects of oxygen breathing in patients with acute myocardial infarction. Cardiovasc Res. 1969 Apr;3(2):179-89 | PubMed |
- Ganz W, Donoso R, Marcus H, Swan HJ. Coronary hemodynamics and myocardial oxygen metabolism during oxygen breathing in patients with and without coronary artery disease. Circulation. 1972 Apr;45(4):763-8 | PubMed |
- Kenmure AC, Murdoch WR, Beattie AD, Marshall JC, Cameron AJ. Circulatory and metabolic effects of oxygen in myocardial infarction. Br Med J. 1968 Nov 9;4(5627):360-4 | PubMed |
- Madias JE, Madias NE, Hood WB Jr. Precordial ST-segment mapping. 2. Effects of oxygen inhalation on ischemic injury in patients with acute myocardial infarction. Circulation. 1976 Mar;53(3):411-7 | PubMed |
- Nehme Z, Stub D, Bernard S, Stephenson M, Bray JE, Cameron P, et al. Effect of supplemental oxygen exposure on myocardial injury in ST-elevation myocardial infarction. Heart. 2016 Mar;102(6):444-51 | CrossRef | PubMed |
- Ranchord AM, Argyle R, Beynon R, Perrin K, Sharma V, Weatherall M, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: a pilot randomized controlled trial. Am Heart J. 2012 Feb;163(2):168-75 | CrossRef | PubMed |
- Rawles JM, Kenmure AC. Controlled trial of oxygen in uncomplicated myocardial infarction. Br Med J. 1976 May 8;1(6018):1121-3 | PubMed |
- Russek HI, Regan FD, Naegele CF. One hundred percent oxygen in the treatment of acute myocardial infarction and severe angina pectoris. J Am Med Assoc. 1950 Sep 30;144(5):373-5 | PubMed |
- Smith K, Nehme Z, Stub D, Stephenson M, Bernard S. Air Versus Oxygen In myocarDial infarction (AVOID) study: trial methods and experience from initial randomisation. Australasian Journal of Paramedicine. 2012;10:24-24 | Link |
- Smith K, Bray J, Stub D, Stephenson M, Bernard S. Avoid methods and experience of initial randomisations. Academic Emergency Medicine. 2012;19:762-3 | Link |
- Stub D, Smith K, Bernard S, Bray JE, Stephenson M, Cameron P, et al. A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study). Am Heart J. 2012 Mar;163(3):339-345.e1 | CrossRef | PubMed |
- Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray J, et al. A randomised controlled trial of oxygen therapy in acute ST-segment elevation myocardial infarction: The Air Versus Oxygen in Myocardial Infarction (AVOID) study. Circulation. 2014;130(23):2111-2111 | Link |
- Stub D, Smith K, Bernard S. Air versus oxygen in ST-elevation myocardial infarction. 2015 | Link |
- Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, et al. Air Versus Oxygen in ST-Segment-Elevation Myocardial Infarction. Circulation. 2015 Jun 16;131(24):2143-50 | CrossRef | PubMed |
- Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray J, et al. Air versus oxygen in myocardial infarction (AVOID) trial sub-study: time-dependent effect of oxygen administration on myocardial injury. Heart, Lung and Circulation. 2015;24:S374 | Link |
- Sukumalchantra Y, Levy S, Danzig R, Rubins S, Alpern H, Swan HJ. Correcting arterial hypoxemia by oxygen therapy in patients with acute myocardial infarction. Effect on ventilation and hemodynamics. Am J Cardiol. 1969 Dec;24(6):838-52 | PubMed |
- Ukholkina GB, Kostianov I, Kuchkina NV, Grendo EP, Gofman IaB. [Effect of oxygenotherapy used in combination with reperfusion in patients with acute myocardial infarction]. Kardiologiia. 2005;45(5):59 | PubMed |
- Ukholkina GB, Kostyanov IJ, Kuchkina NV, Grindot EP, Gofman IaB. Oxygen therapy in combination with endovascular reperfusion during the first hours of acute myocardial infarction:clinical and laboratory findings. International Journal of Interventional Cardioangiology. 2005;9.
- Wilson AT, Channer KS. Hypoxaemia and supplemental oxygen therapy in the first 24 hours after myocardial infarction: the role of pulse oximetry. J R Coll Physicians Lond. 1997 Nov-Dec;31(6):657-61 | PubMed |
- O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):e362-425 | CrossRef | PubMed |
- Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al; ACC/AHA Task Force Members. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec 23;130(25):e344-426 | CrossRef | PubMed |
- Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al; Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016 Jan 14;37(3):267-315 | CrossRef | PubMed |
- Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012 Oct;33(20):2569-619 | CrossRef | PubMed |
- ACTRN12616000461493. All New Zealand Acute Coronary syndromes quality improvement (ANZACS-QI) registry trial to evaluate two oxygen protocols as part of usual care in patients presenting with a suspected acute coronary syndrome, 2016 | Link |
- ACTRN12609000466246. A randomized controlled trial comparing controlled oxygen therapy versus high flow oxygen therapy for acute myocardial infarctions in the pre-hospital setting | Link |
- Khoshnood A, Carlsson M, Akbarzadeh M, Bhiladvala P, Roijer A, Bodetoft S, et al. The Effects of Oxygen Therapy on Myocardial Salvage in ST Elevation Myocardial Infarction Treated with Acute Percutaneous Coronary Intervention: The Supplemental Oxygen in Catheterized Coronary Emergency Reperfusion (SOCCER) Study. Cardiology. 2015;132(1):16-21 | CrossRef | PubMed |
 Burls A, Cabello JB, Emparanza JI, Bayliss S, Quinn T. Oxygen therapy for acute myocardial infarction: a systematic review and meta-analysis. Emerg Med J. 2011 Nov;28(11):917-23 | CrossRef | PubMed |
Burls A, Cabello JB, Emparanza JI, Bayliss S, Quinn T. Oxygen therapy for acute myocardial infarction: a systematic review and meta-analysis. Emerg Med J. 2011 Nov;28(11):917-23 | CrossRef | PubMed | Cabello JB, Burls A, Emparanza JI, Bayliss SE, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2016 Dec 19;12:CD007160 | PubMed |
Cabello JB, Burls A, Emparanza JI, Bayliss SE, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2016 Dec 19;12:CD007160 | PubMed | Loomba RS, Nijhawan K, Aggarwal S, Arora RR. Oxygen in the Setting of Acute Myocardial Infarction: Is It Really a Breath of Fresh Air? J Cardiovasc Pharmacol Ther. 2016 Mar;21(2):143-9 | CrossRef | PubMed |
Loomba RS, Nijhawan K, Aggarwal S, Arora RR. Oxygen in the Setting of Acute Myocardial Infarction: Is It Really a Breath of Fresh Air? J Cardiovasc Pharmacol Ther. 2016 Mar;21(2):143-9 | CrossRef | PubMed | Nicholson C. A systematic review of the effectiveness of oxygen in reducing acute myocardial ischaemia. J Clin Nurs. 2004 Nov;13(8):996-1007 | PubMed |
Nicholson C. A systematic review of the effectiveness of oxygen in reducing acute myocardial ischaemia. J Clin Nurs. 2004 Nov;13(8):996-1007 | PubMed | Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Weatherall M, Beasley R. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart. 2009 Mar;95(3):198-202 | CrossRef | PubMed |
Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Weatherall M, Beasley R. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart. 2009 Mar;95(3):198-202 | CrossRef | PubMed | Bourassa MG, Campeau L, Bois MA, Rico O. The effects of inhalation of 100 percent oxygen on myocardial lactate metabolism in coronary heart disease. Am J Cardiol. 1969 Aug;24(2):172-7 | PubMed |
Bourassa MG, Campeau L, Bois MA, Rico O. The effects of inhalation of 100 percent oxygen on myocardial lactate metabolism in coronary heart disease. Am J Cardiol. 1969 Aug;24(2):172-7 | PubMed | Foster GL, Casten GG, Reeves TJ. The effects of oxygen breathing in patients with acute myocardial infarction. Cardiovasc Res. 1969 Apr;3(2):179-89 | PubMed |
Foster GL, Casten GG, Reeves TJ. The effects of oxygen breathing in patients with acute myocardial infarction. Cardiovasc Res. 1969 Apr;3(2):179-89 | PubMed | Ganz W, Donoso R, Marcus H, Swan HJ. Coronary hemodynamics and myocardial oxygen metabolism during oxygen breathing in patients with and without coronary artery disease. Circulation. 1972 Apr;45(4):763-8 | PubMed |
Ganz W, Donoso R, Marcus H, Swan HJ. Coronary hemodynamics and myocardial oxygen metabolism during oxygen breathing in patients with and without coronary artery disease. Circulation. 1972 Apr;45(4):763-8 | PubMed | Kenmure AC, Murdoch WR, Beattie AD, Marshall JC, Cameron AJ. Circulatory and metabolic effects of oxygen in myocardial infarction. Br Med J. 1968 Nov 9;4(5627):360-4 | PubMed |
Kenmure AC, Murdoch WR, Beattie AD, Marshall JC, Cameron AJ. Circulatory and metabolic effects of oxygen in myocardial infarction. Br Med J. 1968 Nov 9;4(5627):360-4 | PubMed | Madias JE, Madias NE, Hood WB Jr. Precordial ST-segment mapping. 2. Effects of oxygen inhalation on ischemic injury in patients with acute myocardial infarction. Circulation. 1976 Mar;53(3):411-7 | PubMed |
Madias JE, Madias NE, Hood WB Jr. Precordial ST-segment mapping. 2. Effects of oxygen inhalation on ischemic injury in patients with acute myocardial infarction. Circulation. 1976 Mar;53(3):411-7 | PubMed | Nehme Z, Stub D, Bernard S, Stephenson M, Bray JE, Cameron P, et al. Effect of supplemental oxygen exposure on myocardial injury in ST-elevation myocardial infarction. Heart. 2016 Mar;102(6):444-51 | CrossRef | PubMed |
Nehme Z, Stub D, Bernard S, Stephenson M, Bray JE, Cameron P, et al. Effect of supplemental oxygen exposure on myocardial injury in ST-elevation myocardial infarction. Heart. 2016 Mar;102(6):444-51 | CrossRef | PubMed | Ranchord AM, Argyle R, Beynon R, Perrin K, Sharma V, Weatherall M, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: a pilot randomized controlled trial. Am Heart J. 2012 Feb;163(2):168-75 | CrossRef | PubMed |
Ranchord AM, Argyle R, Beynon R, Perrin K, Sharma V, Weatherall M, et al. High-concentration versus titrated oxygen therapy in ST-elevation myocardial infarction: a pilot randomized controlled trial. Am Heart J. 2012 Feb;163(2):168-75 | CrossRef | PubMed | Rawles JM, Kenmure AC. Controlled trial of oxygen in uncomplicated myocardial infarction. Br Med J. 1976 May 8;1(6018):1121-3 | PubMed |
Rawles JM, Kenmure AC. Controlled trial of oxygen in uncomplicated myocardial infarction. Br Med J. 1976 May 8;1(6018):1121-3 | PubMed | Russek HI, Regan FD, Naegele CF. One hundred percent oxygen in the treatment of acute myocardial infarction and severe angina pectoris. J Am Med Assoc. 1950 Sep 30;144(5):373-5 | PubMed |
Russek HI, Regan FD, Naegele CF. One hundred percent oxygen in the treatment of acute myocardial infarction and severe angina pectoris. J Am Med Assoc. 1950 Sep 30;144(5):373-5 | PubMed | Smith K, Nehme Z, Stub D, Stephenson M, Bernard S. Air Versus Oxygen In myocarDial infarction (AVOID) study: trial methods and experience from initial randomisation. Australasian Journal of Paramedicine. 2012;10:24-24 | Link |
Smith K, Nehme Z, Stub D, Stephenson M, Bernard S. Air Versus Oxygen In myocarDial infarction (AVOID) study: trial methods and experience from initial randomisation. Australasian Journal of Paramedicine. 2012;10:24-24 | Link | Smith K, Bray J, Stub D, Stephenson M, Bernard S. Avoid methods and experience of initial randomisations. Academic Emergency Medicine. 2012;19:762-3 | Link |
Smith K, Bray J, Stub D, Stephenson M, Bernard S. Avoid methods and experience of initial randomisations. Academic Emergency Medicine. 2012;19:762-3 | Link | Stub D, Smith K, Bernard S, Bray JE, Stephenson M, Cameron P, et al. A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study). Am Heart J. 2012 Mar;163(3):339-345.e1 | CrossRef | PubMed |
Stub D, Smith K, Bernard S, Bray JE, Stephenson M, Cameron P, et al. A randomized controlled trial of oxygen therapy in acute myocardial infarction Air Verses Oxygen In myocarDial infarction study (AVOID Study). Am Heart J. 2012 Mar;163(3):339-345.e1 | CrossRef | PubMed | Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray J, et al. A randomised controlled trial of oxygen therapy in acute ST-segment elevation myocardial infarction: The Air Versus Oxygen in Myocardial Infarction (AVOID) study. Circulation. 2014;130(23):2111-2111 | Link |
Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray J, et al. A randomised controlled trial of oxygen therapy in acute ST-segment elevation myocardial infarction: The Air Versus Oxygen in Myocardial Infarction (AVOID) study. Circulation. 2014;130(23):2111-2111 | Link | Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, et al. Air Versus Oxygen in ST-Segment-Elevation Myocardial Infarction. Circulation. 2015 Jun 16;131(24):2143-50 | CrossRef | PubMed |
Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray JE, et al. Air Versus Oxygen in ST-Segment-Elevation Myocardial Infarction. Circulation. 2015 Jun 16;131(24):2143-50 | CrossRef | PubMed | Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray J, et al. Air versus oxygen in myocardial infarction (AVOID) trial sub-study: time-dependent effect of oxygen administration on myocardial injury. Heart, Lung and Circulation. 2015;24:S374 | Link |
Stub D, Smith K, Bernard S, Nehme Z, Stephenson M, Bray J, et al. Air versus oxygen in myocardial infarction (AVOID) trial sub-study: time-dependent effect of oxygen administration on myocardial injury. Heart, Lung and Circulation. 2015;24:S374 | Link | Sukumalchantra Y, Levy S, Danzig R, Rubins S, Alpern H, Swan HJ. Correcting arterial hypoxemia by oxygen therapy in patients with acute myocardial infarction. Effect on ventilation and hemodynamics. Am J Cardiol. 1969 Dec;24(6):838-52 | PubMed |
Sukumalchantra Y, Levy S, Danzig R, Rubins S, Alpern H, Swan HJ. Correcting arterial hypoxemia by oxygen therapy in patients with acute myocardial infarction. Effect on ventilation and hemodynamics. Am J Cardiol. 1969 Dec;24(6):838-52 | PubMed | Ukholkina GB, Kostianov I, Kuchkina NV, Grendo EP, Gofman IaB. [Effect of oxygenotherapy used in combination with reperfusion in patients with acute myocardial infarction]. Kardiologiia. 2005;45(5):59 | PubMed |
Ukholkina GB, Kostianov I, Kuchkina NV, Grendo EP, Gofman IaB. [Effect of oxygenotherapy used in combination with reperfusion in patients with acute myocardial infarction]. Kardiologiia. 2005;45(5):59 | PubMed | Ukholkina GB, Kostyanov IJ, Kuchkina NV, Grindot EP, Gofman IaB. Oxygen therapy in combination with endovascular reperfusion during the first hours of acute myocardial infarction:clinical and laboratory findings. International Journal of Interventional Cardioangiology. 2005;9.
Ukholkina GB, Kostyanov IJ, Kuchkina NV, Grindot EP, Gofman IaB. Oxygen therapy in combination with endovascular reperfusion during the first hours of acute myocardial infarction:clinical and laboratory findings. International Journal of Interventional Cardioangiology. 2005;9.  Wilson AT, Channer KS. Hypoxaemia and supplemental oxygen therapy in the first 24 hours after myocardial infarction: the role of pulse oximetry. J R Coll Physicians Lond. 1997 Nov-Dec;31(6):657-61 | PubMed |
Wilson AT, Channer KS. Hypoxaemia and supplemental oxygen therapy in the first 24 hours after myocardial infarction: the role of pulse oximetry. J R Coll Physicians Lond. 1997 Nov-Dec;31(6):657-61 | PubMed | O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):e362-425 | CrossRef | PubMed |
O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013 Jan 29;127(4):e362-425 | CrossRef | PubMed | Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al; ACC/AHA Task Force Members. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec 23;130(25):e344-426 | CrossRef | PubMed |
Amsterdam EA, Wenger NK, Brindis RG, Casey DE Jr, Ganiats TG, Holmes DR Jr, et al; ACC/AHA Task Force Members. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014 Dec 23;130(25):e344-426 | CrossRef | PubMed | Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al; Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016 Jan 14;37(3):267-315 | CrossRef | PubMed |
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, et al; Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016 Jan 14;37(3):267-315 | CrossRef | PubMed | Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012 Oct;33(20):2569-619 | CrossRef | PubMed |
Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012 Oct;33(20):2569-619 | CrossRef | PubMed | ACTRN12616000461493. All New Zealand Acute Coronary syndromes quality improvement (ANZACS-QI) registry trial to evaluate two oxygen protocols as part of usual care in patients presenting with a suspected acute coronary syndrome, 2016 | Link |
ACTRN12616000461493. All New Zealand Acute Coronary syndromes quality improvement (ANZACS-QI) registry trial to evaluate two oxygen protocols as part of usual care in patients presenting with a suspected acute coronary syndrome, 2016 | Link | ACTRN12609000466246. A randomized controlled trial comparing controlled oxygen therapy versus high flow oxygen therapy for acute myocardial infarctions in the pre-hospital setting | Link |
ACTRN12609000466246. A randomized controlled trial comparing controlled oxygen therapy versus high flow oxygen therapy for acute myocardial infarctions in the pre-hospital setting | Link | Khoshnood A, Carlsson M, Akbarzadeh M, Bhiladvala P, Roijer A, Bodetoft S, et al. The Effects of Oxygen Therapy on Myocardial Salvage in ST Elevation Myocardial Infarction Treated with Acute Percutaneous Coronary Intervention: The Supplemental Oxygen in Catheterized Coronary Emergency Reperfusion (SOCCER) Study. Cardiology. 2015;132(1):16-21 | CrossRef | PubMed |
Khoshnood A, Carlsson M, Akbarzadeh M, Bhiladvala P, Roijer A, Bodetoft S, et al. The Effects of Oxygen Therapy on Myocardial Salvage in ST Elevation Myocardial Infarction Treated with Acute Percutaneous Coronary Intervention: The Supplemental Oxygen in Catheterized Coronary Emergency Reperfusion (SOCCER) Study. Cardiology. 2015;132(1):16-21 | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








