Abstract
Sodium restriction has been recommended in chronic heart failure for decades. However, the evidence about the benefit of this measure is not clear, and it might even increase risks. Searching in Epistemonikos database, which is maintained by screening multiple databases, we identified three systematic reviews incorporating 13 studies addressing the question of this article, 10 were randomized trials. We extracted data, combined the evidence using meta-analysis and generated a summary of findings table following the GRADE approach. We concluded sodium restriction might increase mortality and the risk of hospital admission in chronic heart failure, but the certainty of the evidence is low.
Problem
High sodium intake increases morbidity and mortality, mainly in hypertensive people. Sodium restriction has also been recommended in chronic heart failure for decades, to diminish edema and to improve symptoms. However, it has been also postulated sodium restriction might increase the activity of renin-angiotensin and sympathetic systems through intravascular depletion, specially when combined with fluid restriction and diuretic therapy. Even though guidelines widely support this measure, existing evidence is controversial.
Methods
We used Epistemonikos database, which is maintained by screening multiple databases, to identify systematic reviews and their included primary studies. We extracted the information from the reviews, and with this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found three systematic reviews [1],[2],[3] incorporating 13 primary studies overall [4],[5],[6],[7],[8],[9],[10],[11],[12],[13],[14],[15],[16], including 10 randomized controlled trials [4],[5],[6],[7],[8],[9],[10],[11],[12],[13]. This table and the summary in general are based on the latter. |
|
What types of patients were included |
Ejection fraction was 22.5% in one trial [8], <35% in three trials [4],[5],[6], < 40% in one trial [13] and in five it was not reported [10],[12],[13],[14],[15]. NYHA functional class of included patients was the following: In three trials it was II at 30 days post-discharge [4],[5],[6]; in one trial 72.6% were class II and 11.7% class III [7]; in one trial 17% class II and 83% class III [9]; in one 48.1 % II, 51.9% III or IV [10]; in one 90% II and 10% III [11]; in one I-III [12]; in one 24% II, 74% III [13]; and in one it was not reported [8]. |
|
What types of interventions were included |
Three trials compared furosemide po + 120 mmol sodium per day versus furosemide po + 80 mmol sodium per day [4],[5],[6]. One trial compared providing general information versus providing information for a 2500 mg per day restriction [7]. Another trial compared a prescription of sodium 2000 mg per day versus 2000 mg per day + education by nutritionist [8]. One trial compared providing general information versus sodium restriction (2000-3000 mg/day and liquid 1.5 L + education) [9]. One trial compared provision of information + general care versus diet, education and sodium restriction 2000-3000mg per day [10]. One trial compared a restriction of 2300 versus 1500 mg per day [11]. One trial compared usual care versus diet, education and sodium restriction 2000-3000 mg per day [12]. Another trial compared provision of information about salt and fluid intake restriction versus fluid restriction 1500 cc per day and 5000 mg sodium per day restriction + nutritional support [13]. |
|
What types of outcomes |
The primary studies measured several outcomes, but the systematic reviews identified grouped them as follows:
|
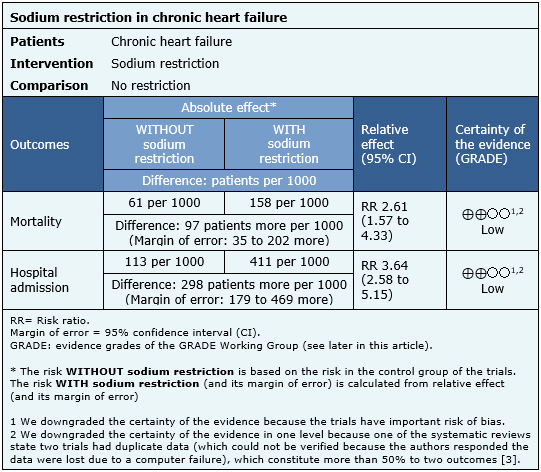
Summary of findings
The information about the effects of sodium restriction in chronic heart failure is based on only three trials including 775 patients for the outcome mortality and 578 for hospital admission [7],[8],[9]. The remaining trials were not incorporated in the meta-analysis of any of the reviews identified.
The summary of findings is the following:
- Sodium restriction might increase mortality in chronic heart failure, but the certainty of the evidence is low.
- Sodium restriction might increase the risk of hospital admission in chronic heart failure, but the certainty of the evidence is low.

Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
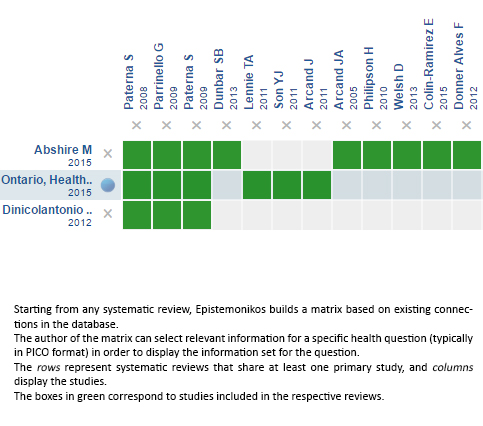
Follow the link to access the interactive version: Sodium restriction in chronic heart failure
Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

El alto consumo de sodio ha sido asociado a un aumento de morbilidad y mortalidad, en especial en pacientes con hipertensión. La restricción de sodio también ha sido recomendada en la insuficiencia cardiaca crónica desde hace décadas, ya que en teoría permitiría manejar el edema y controlar los síntomas. Sin embargo, también se ha planteado que la restricción de sodio podría aumentar la activación del sistema simpático y renina-angiotensina-aldosterona por medio de la depleción de volumen intravascular, especialmente en combinación con restricción de fluidos y terapia diurética. Si bien las guías clínicas apoyan ampliamente esta intervención, la evidencia al respecto es controvertida.
 Authors:
Victoria Castro-Gutiérrez[1,2], Gabriel Rada[2,3,4,5,6]
Authors:
Victoria Castro-Gutiérrez[1,2], Gabriel Rada[2,3,4,5,6]
Affiliation:
[1] Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[2] Proyecto Epistemonikos, Santiago, Chile
[3] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[4] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile
[5] GRADE working group
[6] The Cochrane Collaboration
E-mail: radagabriel@epistemonikos.org
Author address:
[1] Facultad de Medicina Pontificia Universidad Católica de Chile Lira 63 Santiago Centro Chile

Citation: Castro-Gutiérrez V, Rada G. Should sodium intake be restricted in chronic heart failure?. Medwave 2016;16(Suppl5):e6696 doi: 10.5867/medwave.2016.6696
Publication date: 5/12/2016

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Health Quality Ontario. Sodium restriction in heart failure: a rapid review. Toronto: Health Quality Ontario; 2015 February. 20 p | Link |
- DiNicolantonio JJ, Di Pasquale P, Taylor RS, Hackam DG. Low sodium versus normal sodium diets in systolic heart failure: systematic review and meta-analysis. Heart. 2013 Mar 12 | CrossRef | PubMed |
- Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, Andrews MJ, Dennison Himmelfarb C. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed |
- Paterna S, Parrinello G, Cannizzaro S, Fasullo S, Torres D, Sarullo FM, et al. Medium term effects of different dosage of diuretic, sodium, and fluid administration on neurohormonal and clinical outcome in patients with recently compensated heart failure. Am J Cardiol. 2009 Jan 1;103(1):93-102 | CrossRef | PubMed |
- Paterna S, Gaspare P, Fasullo S, Sarullo FM, Di Pasquale P. Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: is sodium an old enemy or a new friend? Clin Sci (Lond). 2008 Feb;114(3):221-30 | PubMed |
- Parrinello G, Di Pasquale P, Licata G, Torres D, Giammanco M, Fasullo S, et al. Long-term effects of dietary sodium intake on cytokines and neurohormonal activation in patients with recently compensated congestive heart failure. J Card Fail. 2009 Dec;15(10):864-73 | CrossRef | PubMed |
- Dunbar SB, Clark PC, Reilly CM, Gary RA, Smith A, McCarty F, et al. A trial of family partnership and education interventions in heart failure. J Card Fail. 2013 Dec;19(12):829-41 | CrossRef | PubMed |
- Arcand JA, Brazel S, Joliffe C, Choleva M, Berkoff F, Allard JP, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. Am Heart J. 2005 Oct;150(4):716 | PubMed |
- Philipson H, Ekman I, Swedberg K, Schaufelberger M. A pilot study of salt and water restriction in patients with chronic heart failure. Scand Cardiovasc J. 2010 Aug;44(4):209-14 | CrossRef | PubMed |
- Welsh D, Lennie TA, Marcinek R, Biddle MJ, Abshire D, Bentley B, et al. Low-sodium diet self-management intervention in heart failure: pilot study results. Eur J Cardiovasc Nurs. 2013 Feb;12(1):87-95 | CrossRef | PubMed |
- Colin-Ramirez E, McAlister FA, Zheng Y, Sharma S, Armstrong PW, Ezekowitz JA. The long-term effects of dietary sodium restriction on clinical outcomes in patients with heart failure. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure): a pilot study. Am Heart J. 2015 Feb;169(2):274-281.e1 | CrossRef | PubMed |
- Donner Alves F, Correa Souza G, Brunetto S, Schweigert Perry ID, Biolo A. Nutritional orientation, knowledge and quality of diet in heart failure: randomized clinical trial. Nutr Hosp. 2012 Mar-Apr;27(2):441-8 | CrossRef | PubMed |
- Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013 Nov;15(11):1304-10 | CrossRef | PubMed |
- Arcand J, Ivanov J, Sasson A, Floras V, Al-Hesayen A, Azevedo ER, et al. A high-sodium diet is associated with acute decompensated heart failure in ambulatory heart failure patients: a prospective follow-up study. Am J Clin Nutr. 2011 Feb;93(2):332-7 | CrossRef | PubMed |
- Lennie TA, Song EK, Wu JR, Chung ML, Dunbar SB, Pressler SJ, et al. Three gram sodium intake is associated with longer event-free survival only in patients with advanced heart failure. J Card Fail. 2011 Apr;17(4):325-30 | CrossRef | PubMed |
- Son YJ, Lee Y, Song EK. Adherence to a sodium-restricted diet is associated with lower symptom burden and longer cardiac event-free survival in patients with heart failure. J Clin Nurs. 2011 Nov;20(21-22):3029-38 | CrossRef | PubMed |
- McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al; ESC Committee for Practice Guidelines.. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847 | CrossRef |
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed |
- Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194 | CrossRef | PubMed |
- Maya Guglin, Low Sodium vs. Regular Diet in Patients Admitted for Heart Failure SALT, 2016 | Link |
- Stony Brook University. Dietary Sodium Intake and Outcomes in Heart Failure. clinicaltrials.gov. 2015 | Link |
- University of Michigan. Geriatric Out of Hospital Randomized Meal Trial in Heart Failure. clinicaltrials.gov. 2014
 Health Quality Ontario. Sodium restriction in heart failure: a rapid review. Toronto: Health Quality Ontario; 2015 February. 20 p | Link |
Health Quality Ontario. Sodium restriction in heart failure: a rapid review. Toronto: Health Quality Ontario; 2015 February. 20 p | Link | DiNicolantonio JJ, Di Pasquale P, Taylor RS, Hackam DG. Low sodium versus normal sodium diets in systolic heart failure: systematic review and meta-analysis. Heart. 2013 Mar 12 | CrossRef | PubMed |
DiNicolantonio JJ, Di Pasquale P, Taylor RS, Hackam DG. Low sodium versus normal sodium diets in systolic heart failure: systematic review and meta-analysis. Heart. 2013 Mar 12 | CrossRef | PubMed | Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, Andrews MJ, Dennison Himmelfarb C. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed |
Abshire M, Xu J, Baptiste D, Almansa JR, Xu J, Cummings A, Andrews MJ, Dennison Himmelfarb C. Nutritional Interventions in Heart Failure: A Systematic Review of the Literature. J Card Fail. 2015 Dec;21(12):989-99 | CrossRef | PubMed | Paterna S, Parrinello G, Cannizzaro S, Fasullo S, Torres D, Sarullo FM, et al. Medium term effects of different dosage of diuretic, sodium, and fluid administration on neurohormonal and clinical outcome in patients with recently compensated heart failure. Am J Cardiol. 2009 Jan 1;103(1):93-102 | CrossRef | PubMed |
Paterna S, Parrinello G, Cannizzaro S, Fasullo S, Torres D, Sarullo FM, et al. Medium term effects of different dosage of diuretic, sodium, and fluid administration on neurohormonal and clinical outcome in patients with recently compensated heart failure. Am J Cardiol. 2009 Jan 1;103(1):93-102 | CrossRef | PubMed | Paterna S, Gaspare P, Fasullo S, Sarullo FM, Di Pasquale P. Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: is sodium an old enemy or a new friend? Clin Sci (Lond). 2008 Feb;114(3):221-30 | PubMed |
Paterna S, Gaspare P, Fasullo S, Sarullo FM, Di Pasquale P. Normal-sodium diet compared with low-sodium diet in compensated congestive heart failure: is sodium an old enemy or a new friend? Clin Sci (Lond). 2008 Feb;114(3):221-30 | PubMed | Parrinello G, Di Pasquale P, Licata G, Torres D, Giammanco M, Fasullo S, et al. Long-term effects of dietary sodium intake on cytokines and neurohormonal activation in patients with recently compensated congestive heart failure. J Card Fail. 2009 Dec;15(10):864-73 | CrossRef | PubMed |
Parrinello G, Di Pasquale P, Licata G, Torres D, Giammanco M, Fasullo S, et al. Long-term effects of dietary sodium intake on cytokines and neurohormonal activation in patients with recently compensated congestive heart failure. J Card Fail. 2009 Dec;15(10):864-73 | CrossRef | PubMed | Dunbar SB, Clark PC, Reilly CM, Gary RA, Smith A, McCarty F, et al. A trial of family partnership and education interventions in heart failure. J Card Fail. 2013 Dec;19(12):829-41 | CrossRef | PubMed |
Dunbar SB, Clark PC, Reilly CM, Gary RA, Smith A, McCarty F, et al. A trial of family partnership and education interventions in heart failure. J Card Fail. 2013 Dec;19(12):829-41 | CrossRef | PubMed | Arcand JA, Brazel S, Joliffe C, Choleva M, Berkoff F, Allard JP, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. Am Heart J. 2005 Oct;150(4):716 | PubMed |
Arcand JA, Brazel S, Joliffe C, Choleva M, Berkoff F, Allard JP, et al. Education by a dietitian in patients with heart failure results in improved adherence with a sodium-restricted diet: a randomized trial. Am Heart J. 2005 Oct;150(4):716 | PubMed | Philipson H, Ekman I, Swedberg K, Schaufelberger M. A pilot study of salt and water restriction in patients with chronic heart failure. Scand Cardiovasc J. 2010 Aug;44(4):209-14 | CrossRef | PubMed |
Philipson H, Ekman I, Swedberg K, Schaufelberger M. A pilot study of salt and water restriction in patients with chronic heart failure. Scand Cardiovasc J. 2010 Aug;44(4):209-14 | CrossRef | PubMed | Welsh D, Lennie TA, Marcinek R, Biddle MJ, Abshire D, Bentley B, et al. Low-sodium diet self-management intervention in heart failure: pilot study results. Eur J Cardiovasc Nurs. 2013 Feb;12(1):87-95 | CrossRef | PubMed |
Welsh D, Lennie TA, Marcinek R, Biddle MJ, Abshire D, Bentley B, et al. Low-sodium diet self-management intervention in heart failure: pilot study results. Eur J Cardiovasc Nurs. 2013 Feb;12(1):87-95 | CrossRef | PubMed | Colin-Ramirez E, McAlister FA, Zheng Y, Sharma S, Armstrong PW, Ezekowitz JA. The long-term effects of dietary sodium restriction on clinical outcomes in patients with heart failure. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure): a pilot study. Am Heart J. 2015 Feb;169(2):274-281.e1 | CrossRef | PubMed |
Colin-Ramirez E, McAlister FA, Zheng Y, Sharma S, Armstrong PW, Ezekowitz JA. The long-term effects of dietary sodium restriction on clinical outcomes in patients with heart failure. The SODIUM-HF (Study of Dietary Intervention Under 100 mmol in Heart Failure): a pilot study. Am Heart J. 2015 Feb;169(2):274-281.e1 | CrossRef | PubMed | Donner Alves F, Correa Souza G, Brunetto S, Schweigert Perry ID, Biolo A. Nutritional orientation, knowledge and quality of diet in heart failure: randomized clinical trial. Nutr Hosp. 2012 Mar-Apr;27(2):441-8 | CrossRef | PubMed |
Donner Alves F, Correa Souza G, Brunetto S, Schweigert Perry ID, Biolo A. Nutritional orientation, knowledge and quality of diet in heart failure: randomized clinical trial. Nutr Hosp. 2012 Mar-Apr;27(2):441-8 | CrossRef | PubMed | Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013 Nov;15(11):1304-10 | CrossRef | PubMed |
Philipson H, Ekman I, Forslund HB, Swedberg K, Schaufelberger M. Salt and fluid restriction is effective in patients with chronic heart failure. Eur J Heart Fail. 2013 Nov;15(11):1304-10 | CrossRef | PubMed | Arcand J, Ivanov J, Sasson A, Floras V, Al-Hesayen A, Azevedo ER, et al. A high-sodium diet is associated with acute decompensated heart failure in ambulatory heart failure patients: a prospective follow-up study. Am J Clin Nutr. 2011 Feb;93(2):332-7 | CrossRef | PubMed |
Arcand J, Ivanov J, Sasson A, Floras V, Al-Hesayen A, Azevedo ER, et al. A high-sodium diet is associated with acute decompensated heart failure in ambulatory heart failure patients: a prospective follow-up study. Am J Clin Nutr. 2011 Feb;93(2):332-7 | CrossRef | PubMed | Lennie TA, Song EK, Wu JR, Chung ML, Dunbar SB, Pressler SJ, et al. Three gram sodium intake is associated with longer event-free survival only in patients with advanced heart failure. J Card Fail. 2011 Apr;17(4):325-30 | CrossRef | PubMed |
Lennie TA, Song EK, Wu JR, Chung ML, Dunbar SB, Pressler SJ, et al. Three gram sodium intake is associated with longer event-free survival only in patients with advanced heart failure. J Card Fail. 2011 Apr;17(4):325-30 | CrossRef | PubMed | Son YJ, Lee Y, Song EK. Adherence to a sodium-restricted diet is associated with lower symptom burden and longer cardiac event-free survival in patients with heart failure. J Clin Nurs. 2011 Nov;20(21-22):3029-38 | CrossRef | PubMed |
Son YJ, Lee Y, Song EK. Adherence to a sodium-restricted diet is associated with lower symptom burden and longer cardiac event-free survival in patients with heart failure. J Clin Nurs. 2011 Nov;20(21-22):3029-38 | CrossRef | PubMed | McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al; ESC Committee for Practice Guidelines.. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847 | CrossRef |
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al; ESC Committee for Practice Guidelines.. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847 | CrossRef | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed |
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed | Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194 | CrossRef | PubMed |
Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194 | CrossRef | PubMed | Stony Brook University. Dietary Sodium Intake and Outcomes in Heart Failure. clinicaltrials.gov. 2015 | Link |
Stony Brook University. Dietary Sodium Intake and Outcomes in Heart Failure. clinicaltrials.gov. 2015 | Link | University of Michigan. Geriatric Out of Hospital Randomized Meal Trial in Heart Failure. clinicaltrials.gov. 2014
University of Michigan. Geriatric Out of Hospital Randomized Meal Trial in Heart Failure. clinicaltrials.gov. 2014 Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








