Abstract
This Living FRISBEE (Living FRIendly Summary of the Body of Evidence using Epistemonikos) is an update of the summary published in April 2015, based on a new systematic review published in May 2015.
About the update
The article updates the April 2015 Living FRISBEE (Living FRISBEE: Living FRIendly Summary of the Body of Evidence using Epistemonikos) (doi: 10.5867/medwave.2015.03.6129) by including one new systematic review appeared after publication of the original article [1].
The new evidence incorporated in this summary led to a downgrade in the certainty of the evidence from low to very low, and the corresponding changes on key messages and considerations for decision-making.
Problem
Digitalis have been in use for treatment of heart failure for more than two centuries. However, their effects on heart failure are controversial. On one hand they would improve symptoms and exercise tolerance. On the other hand they might increase mortality, especially when there is underlying ischemic heart disease, and they carry a high risk of adverse effects.
Methods
We used Epistemonikos database, which is maintained by screening more than 30 databases, to identify systematic reviews and their included primary studies. With this information we generated a structured summary using a pre-established format, which includes key messages, a summary of the body of evidence (presented as an evidence matrix in Epistemonikos), meta-analysis of the total of studies, a summary of findings table following the GRADE approach and a table of other considerations for decision-making.
|
Key messages
|
About the body of evidence for this question
|
What is the evidence. |
We found four systematic reviews [1],[2],[3],[4] including 13 randomized controlled trials that are reported in sixteen articles [5-20]. |
|
What types of patients were included |
All studies considered heart failure of any etiology, being the most frequent ischemic. All studies included patients in sinus rhythm. Only five studies included patients with reduced ejection fraction: < 45% [14],[15], < 40% [5] y and < 35% [17],[18]. One publication reported the outcomes of patients with preserved ejection fraction [20] from the largest trial (DIG). The average age was between 58 to 69 years in the different studies. |
|
What types of interventions were included |
All studies evaluated digoxin, eight using dose adjustments to reach a specific serum level [5],[9],[10],[14],[16-19]. All studies compared against placebo. |
|
What types of outcomes were measured |
Total mortality or heart failure mortality; hospitalization for any cause or for heart failure, emergency room visits, clinical deterioration, quality of life, walking test, neurohumoral markers and echocardiographic parameters. |
Summary of findings
The following information is based on 13 randomized trials that included 9022 patients. Only eight studies reported total mortality. One study reported hospitalization by any cause, four heart failure hospitalization and 12 reported clinical deterioration.
- There is uncertainty if digitalis decrease or increase mortality in chronic heart failure because the certainty of the evidence is very low.
- Digitalis in chronic heart failure might lead to a reduction in hospitalizations and clinical deterioration. The certainty of the evidence is low.
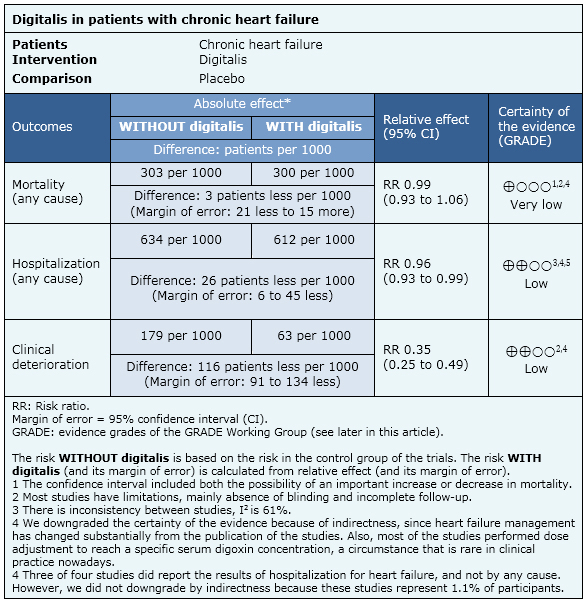
Digitalis for chronic heart failure
Other considerations for decision-making
|
To whom this evidence does and does not apply |
|
| About the outcomes included in this summary |
|
| Balance between benefits and risks, and certainty of the evidence |
|
| What would patients and their doctors think about this intervention |
|
| Resource considerations |
|
|
Differences between this summary and other sources |
|
| Could this evidence change in the future? |
|
How we conducted this summary
Using automated and collaborative means, we compiled all the relevant evidence for the question of interest and we present it as a matrix of evidence.
Follow the link to access the interactive version Digitalis for chronic heart failure

Notes
The upper portion of the matrix of evidence will display a warning of “new evidence” if new systematic reviews are published after the publication of this summary. Even though the project considers the periodical update of these summaries, users are invited to comment in Medwave or to contact the authors through email if they find new evidence and the summary should be updated earlier. After creating an account in Epistemonikos, users will be able to save the matrixes and to receive automated notifications any time new evidence potentially relevant for the question appears.
The details about the methods used to produce these summaries are described here http://dx.doi.org/10.5867/medwave.2014.06.5997.
Epistemonikos foundation is a non-for-profit organization aiming to bring information closer to health decision-makers with technology. Its main development is Epistemonikos database (www.epistemonikos.org).
These summaries follow a rigorous process of internal peer review.
Conflicts of interest
The authors do not have relevant interests to declare.

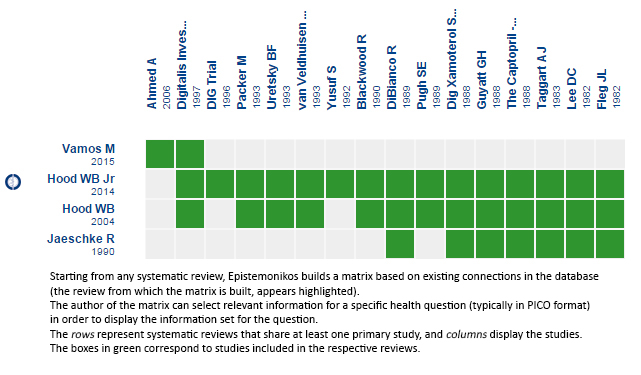 Matrix of evidence
Matrix of evidence
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Este resumen Epistemonikos (Living FRISBEE: Living FRIendly Summary of the Body of Evidence using Epistemonikos) es una actualización del resumen publicado en Abril de 2015, basado en una nueva revisión sistemática aparecida en mayo de 2015.
 Authors:
Carmen Rain[1], Gabriel Rada[1,2,3,4,5]
Authors:
Carmen Rain[1], Gabriel Rada[1,2,3,4,5]
Affiliation:
[1] Programa de Salud Basada en Evidencia, Facultad de Medicina, Pontificia Universidad Católica de Chile
[2] Departamento de Medicina Interna, Facultad de Medicina, Pontificia Universidad Católica de Chile
[3] GRADE working group
[4] The Cochrane Collaboration
[5] Fundación Epistemonikos
E-mail: radagabriel@epistemonikos.org

Citation: Rain C, Rada G. Is there a role for digitalis in chronic heart failure? –First update. Medwave 2015 Jun;15(suppl 1):e6148 doi: 10.5867/medwave.2015.6148
Publication date: 8/6/2015

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Vamos M, Erath JW, Hohnloser SH. Digoxin-associated mortality: a systematic review and meta-analysis of the literature. Eur Heart J. 2015 May 4. pii: ehv143. | PubMed | Link |
- Hood WB Jr, Dans AL, Guyatt GH, Jaeschke R, McMurray JJ. Digitalis for treatment of congestive heart failure in patients in sinus rhythm: a systematic review and meta-analysis. J Card Fail. 2004 Apr;10(2):155-64 | PubMed |
- Hood WB Jr, Dans AL, Guyatt GH, Jaeschke R, McMurray JJ. Digitalis for treatment of heart failure in patients in sinus rhythm. Cochrane Database Syst Rev. 2014 Apr 28;4:CD002901 | CrossRef | PubMed |
- Jaeschke R, Oxman AD, Guyatt GH. To what extent do congestive heart failure patients in sinus rhythm benefit from digoxin therapy? A systematic overview and meta-analysis. Am J Med. 1990 Mar;88(3):279-86. | PubMed | Link |
- Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. The Captopril-Digoxin Multicenter Research Group. JAMA. 1988 Jan 22-29;259(4):539-44. | PubMed |
- Blackwood R, Mayou RA, Garnham JC, Armstrong C, Bryant B. Exercise capacity and quality of life in the treatment of heart failure. Clin Pharmacol Ther. 1990 Sep;48(3):325-32. | PubMed |
- Pugh SE, White NJ, Aronson JK, Grahame-Smith DG, Bloomfield JG. Clinical, haemodynamic, and pharmacological effects of withdrawal and reintroduction of digoxin in patients with heart failure in sinus rhythm after long term treatment. Br Heart J. 1989 Jun;61(6):529-39. | PubMed |
- DiBianco R, Shabetai R, Kostuk W, Moran J, Schlant RC, Wright R. A comparison of oral milrinone, digoxin, and their combination in the treatment of patients with chronic heart failure. N Engl J Med. 1989 Mar 16;320(11):677-83. | PubMed |
- Guyatt GH, Sullivan MJ, Fallen EL, Tihal H, Rideout E, Halcrow S, Nogradi S, Townsend M, Taylor DW. A controlled trial of digoxin in congestive heart failure. Am J Cardiol. 1988 Feb 1;61(4):371-5. | PubMed |
- Taggart AJ, Johnston GD, McDevitt DG. Digoxin withdrawal after cardiac failure in patients with sinus rhythm. J Cardiovasc Pharmacol. 1983 Mar-Apr;5(2):229-34. | PubMed |
- Rationale, design, implementation, and baseline characteristics of patients in the DIG trial: a large, simple, long-term trial to evaluate the effect of digitalis on mortality in heart failure. Control Clin Trials. 1996 Feb;17(1):77-97. | PubMed |
- Double-blind placebo-controlled comparison of digoxin and xamoterol in chronic heart failure. The German and Austrian Xamoterol Study Group. Lancet. 1988 Mar 5;1(8584):489-93. | PubMed |
- Yusuf S, Garg R, Held P, Gorlin R. Need for a large randomized trial to evaluate the effects of digitalis on morbidity and mortality in congestive heart failure. Am J Cardiol. 1992 Jun 4;69(18):64G-70G. | PubMed |
- van Veldhuisen DJ, Man in 't Veld AJ, Dunselman PH, Lok DJ, Dohmen HJ, Poortermans JC, Withagen AJ, et al. Double-blind placebo-controlled study of ibopamine and digoxin in patients with mild to moderate heart failure: results of the Dutch Ibopamine Multicenter Trial (DIMT). J Am Coll Cardiol. 1993 Nov 15;22(6):1564-73. | PubMed |
- Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997 Feb 20;336(8):525-33. | PubMed |
- Lee DC, Johnson RA, Bingham JB, Leahy M, Dinsmore RE, Goroll AH, Newell JB, Strauss HW, Haber E. Heart failure in outpatients: a randomized trial of digoxin versus placebo. N Engl J Med. 1982 Mar 25;306(12):699-705. | PubMed |
- Uretsky BF, Young JB, Shahidi FE, Yellen LG, Harrison MC, Jolly MK. Randomized study assessing the effect of digoxin withdrawal in patients with mild to moderate chronic congestive heart failure: results of the PROVED trial. PROVED Investigative Group. J Am Coll Cardiol. 1993 Oct;22(4):955-62. | PubMed |
- Packer M, Gheorghiade M, Young JB, Costantini PJ, Adams KF, Cody RJ, Smith LK, Van Voorhees L, Gourley LA, Jolly MK. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting-enzyme inhibitors. RADIANCE Study. N Engl J Med. 1993 Jul 1;329(1):1-7. | PubMed |
- Fleg JL, Gottlieb SH, Lakatta EG. Is digoxin really important in treatment of compensated heart failure? A placebo-controlled crossover study in patients with sinus rhythm. Am J Med. 1982 Aug;73(2):244-50. | PubMed |
- Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. 2006 Aug 1;114(5):397-403. Epub 2006 Jul 24. | PubMed |
- Moe GW, Ezekowitz JA, O'Meara E, Lepage S, Howlett JG, Fremes S, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol. 2015 Jan;31(1):3-16. | PubMed |
- Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Katz SD, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WH, Teerlink JR, Walsh MN. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194. | CrossRef | PubMed |
- McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed |
- Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed |
- Fleg JL, Gottlieb SH, Lakatta EG. Is digoxin really important in treatment of compensated heart failure? A placebo-controlled crossover study in patients with sinus rhythm. Am J Med. 1982 Aug;73(2):244-50. | PubMed |
 Vamos M, Erath JW, Hohnloser SH. Digoxin-associated mortality: a systematic review and meta-analysis of the literature. Eur Heart J. 2015 May 4. pii: ehv143. | PubMed | Link |
Vamos M, Erath JW, Hohnloser SH. Digoxin-associated mortality: a systematic review and meta-analysis of the literature. Eur Heart J. 2015 May 4. pii: ehv143. | PubMed | Link | Hood WB Jr, Dans AL, Guyatt GH, Jaeschke R, McMurray JJ. Digitalis for treatment of congestive heart failure in patients in sinus rhythm: a systematic review and meta-analysis. J Card Fail. 2004 Apr;10(2):155-64 | PubMed |
Hood WB Jr, Dans AL, Guyatt GH, Jaeschke R, McMurray JJ. Digitalis for treatment of congestive heart failure in patients in sinus rhythm: a systematic review and meta-analysis. J Card Fail. 2004 Apr;10(2):155-64 | PubMed | Hood WB Jr, Dans AL, Guyatt GH, Jaeschke R, McMurray JJ. Digitalis for treatment of heart failure in patients in sinus rhythm. Cochrane Database Syst Rev. 2014 Apr 28;4:CD002901 | CrossRef | PubMed |
Hood WB Jr, Dans AL, Guyatt GH, Jaeschke R, McMurray JJ. Digitalis for treatment of heart failure in patients in sinus rhythm. Cochrane Database Syst Rev. 2014 Apr 28;4:CD002901 | CrossRef | PubMed | Jaeschke R, Oxman AD, Guyatt GH. To what extent do congestive heart failure patients in sinus rhythm benefit from digoxin therapy? A systematic overview and meta-analysis. Am J Med. 1990 Mar;88(3):279-86. | PubMed | Link |
Jaeschke R, Oxman AD, Guyatt GH. To what extent do congestive heart failure patients in sinus rhythm benefit from digoxin therapy? A systematic overview and meta-analysis. Am J Med. 1990 Mar;88(3):279-86. | PubMed | Link | Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. The Captopril-Digoxin Multicenter Research Group. JAMA. 1988 Jan 22-29;259(4):539-44. | PubMed |
Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. The Captopril-Digoxin Multicenter Research Group. JAMA. 1988 Jan 22-29;259(4):539-44. | PubMed | Blackwood R, Mayou RA, Garnham JC, Armstrong C, Bryant B. Exercise capacity and quality of life in the treatment of heart failure. Clin Pharmacol Ther. 1990 Sep;48(3):325-32. | PubMed |
Blackwood R, Mayou RA, Garnham JC, Armstrong C, Bryant B. Exercise capacity and quality of life in the treatment of heart failure. Clin Pharmacol Ther. 1990 Sep;48(3):325-32. | PubMed | Pugh SE, White NJ, Aronson JK, Grahame-Smith DG, Bloomfield JG. Clinical, haemodynamic, and pharmacological effects of withdrawal and reintroduction of digoxin in patients with heart failure in sinus rhythm after long term treatment. Br Heart J. 1989 Jun;61(6):529-39. | PubMed |
Pugh SE, White NJ, Aronson JK, Grahame-Smith DG, Bloomfield JG. Clinical, haemodynamic, and pharmacological effects of withdrawal and reintroduction of digoxin in patients with heart failure in sinus rhythm after long term treatment. Br Heart J. 1989 Jun;61(6):529-39. | PubMed | DiBianco R, Shabetai R, Kostuk W, Moran J, Schlant RC, Wright R. A comparison of oral milrinone, digoxin, and their combination in the treatment of patients with chronic heart failure. N Engl J Med. 1989 Mar 16;320(11):677-83. | PubMed |
DiBianco R, Shabetai R, Kostuk W, Moran J, Schlant RC, Wright R. A comparison of oral milrinone, digoxin, and their combination in the treatment of patients with chronic heart failure. N Engl J Med. 1989 Mar 16;320(11):677-83. | PubMed | Guyatt GH, Sullivan MJ, Fallen EL, Tihal H, Rideout E, Halcrow S, Nogradi S, Townsend M, Taylor DW. A controlled trial of digoxin in congestive heart failure. Am J Cardiol. 1988 Feb 1;61(4):371-5. | PubMed |
Guyatt GH, Sullivan MJ, Fallen EL, Tihal H, Rideout E, Halcrow S, Nogradi S, Townsend M, Taylor DW. A controlled trial of digoxin in congestive heart failure. Am J Cardiol. 1988 Feb 1;61(4):371-5. | PubMed | Taggart AJ, Johnston GD, McDevitt DG. Digoxin withdrawal after cardiac failure in patients with sinus rhythm. J Cardiovasc Pharmacol. 1983 Mar-Apr;5(2):229-34. | PubMed |
Taggart AJ, Johnston GD, McDevitt DG. Digoxin withdrawal after cardiac failure in patients with sinus rhythm. J Cardiovasc Pharmacol. 1983 Mar-Apr;5(2):229-34. | PubMed | Rationale, design, implementation, and baseline characteristics of patients in the DIG trial: a large, simple, long-term trial to evaluate the effect of digitalis on mortality in heart failure. Control Clin Trials. 1996 Feb;17(1):77-97. | PubMed |
Rationale, design, implementation, and baseline characteristics of patients in the DIG trial: a large, simple, long-term trial to evaluate the effect of digitalis on mortality in heart failure. Control Clin Trials. 1996 Feb;17(1):77-97. | PubMed | Double-blind placebo-controlled comparison of digoxin and xamoterol in chronic heart failure. The German and Austrian Xamoterol Study Group. Lancet. 1988 Mar 5;1(8584):489-93. | PubMed |
Double-blind placebo-controlled comparison of digoxin and xamoterol in chronic heart failure. The German and Austrian Xamoterol Study Group. Lancet. 1988 Mar 5;1(8584):489-93. | PubMed | Yusuf S, Garg R, Held P, Gorlin R. Need for a large randomized trial to evaluate the effects of digitalis on morbidity and mortality in congestive heart failure. Am J Cardiol. 1992 Jun 4;69(18):64G-70G. | PubMed |
Yusuf S, Garg R, Held P, Gorlin R. Need for a large randomized trial to evaluate the effects of digitalis on morbidity and mortality in congestive heart failure. Am J Cardiol. 1992 Jun 4;69(18):64G-70G. | PubMed | van Veldhuisen DJ, Man in 't Veld AJ, Dunselman PH, Lok DJ, Dohmen HJ, Poortermans JC, Withagen AJ, et al. Double-blind placebo-controlled study of ibopamine and digoxin in patients with mild to moderate heart failure: results of the Dutch Ibopamine Multicenter Trial (DIMT). J Am Coll Cardiol. 1993 Nov 15;22(6):1564-73. | PubMed |
van Veldhuisen DJ, Man in 't Veld AJ, Dunselman PH, Lok DJ, Dohmen HJ, Poortermans JC, Withagen AJ, et al. Double-blind placebo-controlled study of ibopamine and digoxin in patients with mild to moderate heart failure: results of the Dutch Ibopamine Multicenter Trial (DIMT). J Am Coll Cardiol. 1993 Nov 15;22(6):1564-73. | PubMed | Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997 Feb 20;336(8):525-33. | PubMed |
Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997 Feb 20;336(8):525-33. | PubMed | Lee DC, Johnson RA, Bingham JB, Leahy M, Dinsmore RE, Goroll AH, Newell JB, Strauss HW, Haber E. Heart failure in outpatients: a randomized trial of digoxin versus placebo. N Engl J Med. 1982 Mar 25;306(12):699-705. | PubMed |
Lee DC, Johnson RA, Bingham JB, Leahy M, Dinsmore RE, Goroll AH, Newell JB, Strauss HW, Haber E. Heart failure in outpatients: a randomized trial of digoxin versus placebo. N Engl J Med. 1982 Mar 25;306(12):699-705. | PubMed | Uretsky BF, Young JB, Shahidi FE, Yellen LG, Harrison MC, Jolly MK. Randomized study assessing the effect of digoxin withdrawal in patients with mild to moderate chronic congestive heart failure: results of the PROVED trial. PROVED Investigative Group. J Am Coll Cardiol. 1993 Oct;22(4):955-62. | PubMed |
Uretsky BF, Young JB, Shahidi FE, Yellen LG, Harrison MC, Jolly MK. Randomized study assessing the effect of digoxin withdrawal in patients with mild to moderate chronic congestive heart failure: results of the PROVED trial. PROVED Investigative Group. J Am Coll Cardiol. 1993 Oct;22(4):955-62. | PubMed | Packer M, Gheorghiade M, Young JB, Costantini PJ, Adams KF, Cody RJ, Smith LK, Van Voorhees L, Gourley LA, Jolly MK. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting-enzyme inhibitors. RADIANCE Study. N Engl J Med. 1993 Jul 1;329(1):1-7. | PubMed |
Packer M, Gheorghiade M, Young JB, Costantini PJ, Adams KF, Cody RJ, Smith LK, Van Voorhees L, Gourley LA, Jolly MK. Withdrawal of digoxin from patients with chronic heart failure treated with angiotensin-converting-enzyme inhibitors. RADIANCE Study. N Engl J Med. 1993 Jul 1;329(1):1-7. | PubMed | Fleg JL, Gottlieb SH, Lakatta EG. Is digoxin really important in treatment of compensated heart failure? A placebo-controlled crossover study in patients with sinus rhythm. Am J Med. 1982 Aug;73(2):244-50. | PubMed |
Fleg JL, Gottlieb SH, Lakatta EG. Is digoxin really important in treatment of compensated heart failure? A placebo-controlled crossover study in patients with sinus rhythm. Am J Med. 1982 Aug;73(2):244-50. | PubMed | Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. 2006 Aug 1;114(5):397-403. Epub 2006 Jul 24. | PubMed |
Ahmed A, Rich MW, Fleg JL, Zile MR, Young JB, Kitzman DW, et al. Effects of digoxin on morbidity and mortality in diastolic heart failure: the ancillary digitalis investigation group trial. Circulation. 2006 Aug 1;114(5):397-403. Epub 2006 Jul 24. | PubMed | Moe GW, Ezekowitz JA, O'Meara E, Lepage S, Howlett JG, Fremes S, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol. 2015 Jan;31(1):3-16. | PubMed |
Moe GW, Ezekowitz JA, O'Meara E, Lepage S, Howlett JG, Fremes S, et al. The 2014 Canadian Cardiovascular Society Heart Failure Management Guidelines Focus Update: anemia, biomarkers, and recent therapeutic trial implications. Can J Cardiol. 2015 Jan;31(1):3-16. | PubMed | Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Katz SD, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WH, Teerlink JR, Walsh MN. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194. | CrossRef | PubMed |
Heart Failure Society of America, Lindenfeld J, Albert NM, Boehmer JP, Collins SP, Ezekowitz JA, Givertz MM, Katz SD, Klapholz M, Moser DK, Rogers JG, Starling RC, Stevenson WG, Tang WH, Teerlink JR, Walsh MN. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010 Jun;16(6):e1-194. | CrossRef | PubMed | McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed |
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012 Jul;33(14):1787-847. | CrossRef | PubMed | Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed |
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013 Oct 15;128(16):e240-327 | CrossRef | PubMed | Fleg JL, Gottlieb SH, Lakatta EG. Is digoxin really important in treatment of compensated heart failure? A placebo-controlled crossover study in patients with sinus rhythm. Am J Med. 1982 Aug;73(2):244-50. | PubMed |
Fleg JL, Gottlieb SH, Lakatta EG. Is digoxin really important in treatment of compensated heart failure? A placebo-controlled crossover study in patients with sinus rhythm. Am J Med. 1982 Aug;73(2):244-50. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








