Key Words: gastritis, gastric mucosa, altitude, hypoxia
Abstract
Introduction
Chronic gastritis is one of the most common diseases in the population. Several factors influence its appearance; however, the effect of high altitude has not been studied thoroughly.
Objective
To determine the association between the altitude of the residential area and chronic gastritis in outpatients of Peru.
Methods
Observational, analytical, and cross-sectional study. Secondary data analysis was conducted. The dependent variable was chronic gastritis, obtained from patient references, and verified in the medical history according to the pathological history mentioned during medical consultation. The independent variable was the altitude of the residential areas (categorized into low altitude, intermediate altitude, high and very high), and the secondary co-variables were age, sex, and time living at altitude. Generalized linear models were used to estimate prevalence ratios using Poisson family and city as a cluster.
Results
Of the 4263 patients studied, 63% were female; the median age was 42 years. The overall prevalence of chronic gastritis was 12,9%. There was an association with chronic gastritis and altitude of residence at the intermediate and high levels, but not at the very high; with an adjusted prevalence ratio of 1.52 (95% confidence interval, 1.03 to 2.23); 2.01 (1.55 to 2.60) and 1.12 (0.84 to 1.48), respectively.
Conclusions
We found a significant association between chronic gastritis and intermediate and high altitude but not at very high, which could be explained by hypobaric hypoxia in altitude that could lead to gastric wall lesions and other socio-demographic variables.
|
Main messages
|
Introduction
Gastritis, in any form, is one of the most prevalent diseases in the world[1]. It is estimated that hundreds of millions worldwide suffer from the disease[1],[2]. As a consequence, gastritis and gastric diseases are two of the leading causes of morbidity in all populations. Their distribution is variable by various risk factors, such as alcohol consumption, tobacco, non-steroidal anti-inflammatories, some drugs, gastric irritants, radiation, caustics, Helicobacter pylori infection, and others[1],[2],[3].
In Peru, as in other countries of the region, chronic gastritis is one of the leading causes of medical consultation[3], Helicobacter pylori infection being one of its principal influencers, the rates of which are similar according to the health conditions of each reality[4],[5].
The prevalence of Helicobacter pylori infection is higher in the population residing at high altitude[5],[6]. Furthermore, gastrointestinal problems are a common condition in populations residing or visiting high altitudes[7],[8],[9]. These conditions range from mild alterations—acute mountain sickness, such as dyspepsia, nausea or vomiting[10], or conditions that decrease the functionality of the gastrointestinal system, mainly due to acute exposure to hypoxic conditions[8],[11])—to more serious conditions, such as episodes of gastric ulcers with digestive bleeding[12],[13], malignant lesions of the gastric mucosa[9], mesenteric infarctions and increased prevalence of acute abdomen due to intestinal volvulus[14]. The pathogenesis of these disorders, to date, has not been fully clarified; however, exposure to chronic hypobaric hypoxia[11],[15], polycythemia[16], increased production of hydrochloric acid by increased vagal stimulation, the Andean megacolon[11],[14], and others[17], are known to be involved.
All of these factors could exacerbate the risk of gastritis for high altitude residents. However, there are no comprehensive epidemiological studies in this field[11]. In Peru, despite having a large percentage of its population living at high altitudes, there are no studies that associate the prevalence of gastritis at different altitude levels. The purpose of this study is to determine the association between altitudinal zones of residence and chronic gastritis in outpatients in Peru.
Methods
Study design and setting
We conducted a cross-sectional study of secondary data analysis from January to June 2015 in 10 of 24 Peruvian departments: Lima, Loreto, Lambayeque, Piura, Huánuco, Cajamarca, Huancayo, Cusco, Puno, Cerro de Pasco. A representative sample was obtained from each department. Initially designed for another study, we worked with the variables previously collected in a dataset, the results of which were published[18].
Population and sample
The population was adult patients who went to different general medical offices in the cities comprised in this study. The sample was initially taken from this population, using a convenience non-probability sampling method. All patients who agreed to answer the questionnaire voluntarily were included. The questionnaire was validated in content by expert judgment, in the context of the primary publication[18]. All patients who completed the survey correctly were included, and those with incomplete data or who were not part of the final analysis were excluded. As it is a non-probability sampling, it is not possible to generalize the data reported here.
The initial population was 4455 patients; however, 168 patients (3.77%) did not answer the main research questions. The final population of the main study and this ancillary study was 4263 patients. Patients with complete study variables and whose referred diagnoses were first ascertained by a doctor during a medical consultation, were included in the dataset.
The clinical diagnosis of chronic gastritis (not endoscopic or histopathological) was considered as a dependent variable, which was obtained through the affirmative answer in the survey and verified in the medical history, as carried out by a doctor during a medical consultation.
The main independent variable was the altitude of residence (calculated according to the meters above mean sea level of the city where the patient declared having lived for over three months). Low altitude was categorized as less than 1500 meters above sea level, intermediate altitude as 1500 to 2500 meters above sea level, high altitude as 2500 to 3500 meters above sea level, and very high altitude as 3500 to 5800 meters above sea level. Age, sex, and years of living at said geographic altitude were also recorded.
Statistical analysis
For the description of the numerical variables, their normality was determined by graphical and analytical evaluation (observing skewness and kurtosis), and the results are expressed in means and standard deviations. If the assumption of normality is not fulfilled, the variables are reported as medians with interquartile ranges. Frequencies and percentages were used to describe the categorical variables. The analysis of the dependent variable between altitude and chronic gastritis was performed with the chi-square test. Subsequently, a bivariate analysis was generated, with the Mann-Whitney U test, to analyze the dependent variable versus age and years living at altitude, both with non-normal distribution. Furthermore, the chi-square test was used for the association between sex and the dependent variable.
The crude prevalence ratios and adjusted prevalence ratios were also determined, with their 95% confidence intervals. Consequently, the generalized linear models were used with the Poisson family and the log link function, using 'city' as a cluster. A confidence level of 95% was considered, and p-values of less than 0.05 were considered statistically significant. The data was processed in the Stata version 11.1 program (Stata Corp, Texas, USA).
Ethical aspects
The original investigation had the approval of the Ethics Committee of San Bartolomé National Hospital and Lambayeque Regional Hospital, which comply with the current regulations of the National Institute of Health of Peru. The original research group authorized the use of the database, respecting the confidentiality of the data. Only those patients who gave their consent for data collection were surveyed; the survey was anonymous.
Results
Of the 4263 participants included, the median age was 42 years with an interquartile range of 27 years. The female sex represented 63.05% (2688). 12.9% of participants were found to have a diagnosis of chronic gastritis. 26.13% of the patients lived in a low geographic altitude area, and 26.32% lived at a high altitude (Table 1).
Table 1. General characteristics of outpatients under study.
The median number of patient-years residing in their city was 20 years for patients with chronic gastritis (interquartile range, 0.5 to 38 years), which differed from the participants without chronic gastritis whose median was 18 years (interquartile range, 0.4 to 35 years), a statistically significant difference (p = 0.039).
In Graph 1, we observe that in a low-altitude zone, 7.7% have chronic gastritis; in an intermediate-altitude zone, 11.2% have chronic gastritis; in a zone of high altitude, 14.4% have chronic gastritis; and in a very high altitude zone, 7.9% have chronic gastritis.
In Table 2, we can see the crude and adjusted prevalence ratios. A positive association was found solely between high altitude and chronic gastritis in the simple regression analysis. In the multiple analysis adjusted for age, sex, and year of residence, an association was found with intermediate and high altitude.
Discussion
The study found that the prevalence of chronic gastritis in areas of intermediate and high altitude was higher than that found at sea level; this was not the case for the very high altitude area. Two cities located at this altitude, Puno and Juliaca, had a prevalence of chronic gastritis below that found in other cities located in the same altitudinal zone.
Among the reasons that could explain this inconsistency, the method used for the data collection could be considered since the selection of participants was not probabilistic and there may be bias for this reason. Other explanations may include the Helicobacter pylori infection rate—in which other socioeconomic, sanitary, and healthiness factors are involved that were not measured in the present study. Even so, it was observed that there was a higher report of chronic gastritis among patients in the intermediate and high altitude zones. This result agrees with what is found in the literature, in which it has been found that living at a higher altitude is associated with a higher Helicobacter pylori infection rate, which is the leading risk factor for chronic gastritis[19],[20].
Studies indicate that at high altitude, systemic hypoxia can cause a decrease in blood flow in the gastric mucosa, which could lead to ischemia and the subsequent destruction of its lining[15],[21]. A study by Galván Meza et al.[22]carried out in Peru, found that at 3280 meters above sea level, 33% of patients had a duodenal ulcer (33%) or a gastric ulcer (25%), simultaneously with chronic gastritis.
Other mechanisms in which altitude can injure the gastric mucosa is polycythemia. In high-altitude Tibetan inhabitants with altitude-induced polycythemia, pathological changes in the gastric mucosa suggestive of apoptosis were found[16]. Li et al.[23] found that the gastric mucosa of patients with polycythemia induced by altitude had a higher frequency of Helicobacter pylori infection.
It has been described that, in patients living at high altitudes in the Andes, there is a higher production of hydrochloric acid due to vagal stimulus caused by chronic hypoxia[24]. All these factors may be responsible for a higher reported prevalence of chronic gastritis in the intermediate and elevated altitudinal zones, as seen in other studies[25].
No association was found between chronic gastritis and age, similar to another study carried out in Latin America that found a high prevalence of Helicobacter pylori infection in Latinos, though not associated with age groups[4]. Helicobacter pylori infection is acquired mainly during childhood and is closely related to health and socioeconomic conditions[26], especially in developing countries where the main route of infection is fecal-oral. Younger generations have the same prevalence of Helicobacter pylori infection when they live in the same conditions of poor sanitation, as opposed to reports from developed countries, where better sanitation conditions result in younger patients with significantly less Helicobacter pylori infection than elderly patients[27],[28]. Because young people lived in improved sanitary conditions and were less exposed to infection by this bacteria, a decrease in the prevalence of this infection is seen in younger age groups.
These findings are consistent with the reported study in China[26] and Germany[27] were the prevalence of chronic gastritis was not associated with sex. Another study conducted in Peru found that the rates of Helicobacter pylori infection in men was 10% higher than that found in women, but this difference was not statistically significant[19]. Chronic gastritis affects both sexes equally and is more related to eating habits, drug consumption, environmental and genetic conditions.
The prevalence of chronic gastritis found in the different altitudinal zones was different from other studies. For example, in a study conducted in China[26], an overall prevalence of 26% of chronic gastritis was diagnosed through endoscopy. Another study from Germany[27] found a prevalence of 9% of chronic gastritis diagnosed through pepsinogen dosing in blood in a population older than 70 years. This inconsistency could we due to an underestimation of the prevalence of chronic gastritis in our population, whose values are closer to the study found in Germany—despite the difference in the risk factors present in each country—which is because many cases of chronic gastritis are not symptomatic[2]. Moreover, upper digestive endoscopy is done when a gastrointestinal illness is suspected, so many patients who said they had not been diagnosed with chronic gastritis are, in some cases, likely to have it but not been diagnosed because they did not present symptoms that make them seek medical care.
The study has limitations, mainly information bias, because the real frequency of this disease may be underestimated due to the absence of an endoscopy report. The primary variable was ascertained based on the report and confirmation of the diagnosis of chronic gastritis by the medical history, as long as a physician made the diagnosis during the consultation, which may lead to recall bias. However, various studies show that these measurement methods can be quite reliable in estimating the prevalence of chronic diseases. The study by Oksanen et al., for example, found that the self-report detection of a disease diagnosed by a doctor has a sensitivity and specificity greater than 78 and 93%, respectively, to detect the prevalence of chronic diseases[29]. Also, Haapanen et al. found an adequate kappa concordance index between the gold standard and the self-report of known chronic diseases[30]. Another limitation was selection bias because of non-probability sampling and Berkson's bias, which prevents extrapolating these results to the general population.
These results should serve to initiate prospective investigations designed to evaluate incidence rates and the risk of chronic gastritis in patients living at different altitudes. Therefore, they can serve as a baseline, so that future investigations can carry out case-control or cohort studies that can control these limitations, as ours was a retrospective study of secondary individual data.
Conclusion
For all the above, we found an association between the diagnosis of chronic gastritis and the patients' residential altitude, especially for intermediate and high altitude. No association was found among chronic gastritis, sex, or the age of patients.
Many other characteristics must be evaluated in further research. Populations will always have intrinsic differences by residential altitude due to their adaptation to decreased environmental oxygen, low level of overcrowding (at least compared to the large cities on the coast), diet, access to health care services, genetics and evolution (which also generates changes in the digestive system), among others.
Notes
Authorship contributions
All authors have made the following contributions: Important and substantive contributions to the concept or design of the work; or to the acquisition, analysis or interpretation of work data. Critical writing or revision of the manuscript, with important intellectual contributions. Final approval of the version to be published. All authors consent to assume responsibility for all aspects of the work in order to ensure that any questions about the accuracy or integrity of any part of the work are addressed and investigated accordingly.
Competing interests
The authors declare that they have no competing interests related to the content of this article.
Funding
The authors did not receive funding to complete this study.
Ethics committee
The primary research generated by the database was approved by the ethics committee of the Hospital Nacional San Bartolomé, with file number: 18346-14.
From the editors
The original version of this manuscript was submitted in Spanish. This English version was submitted by the authors and has been lightly copyedited by the Journal.

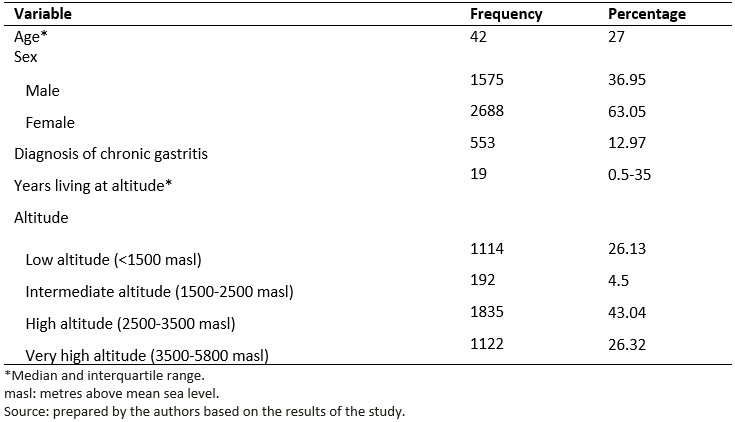 Table 1. General characteristics of outpatients under study.
Table 1. General characteristics of outpatients under study.

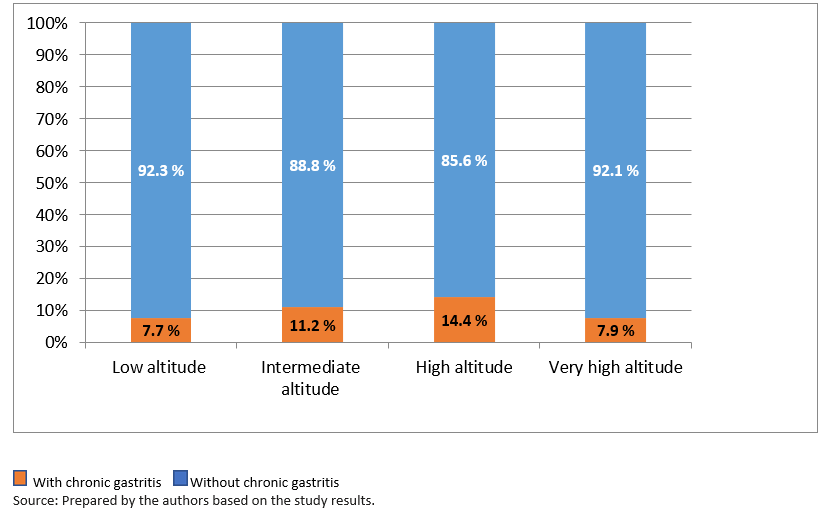 Graph 1. Distribution of the prevalence of chronic gastritis by different altitudinal zones of outpatients under study.
Graph 1. Distribution of the prevalence of chronic gastritis by different altitudinal zones of outpatients under study.

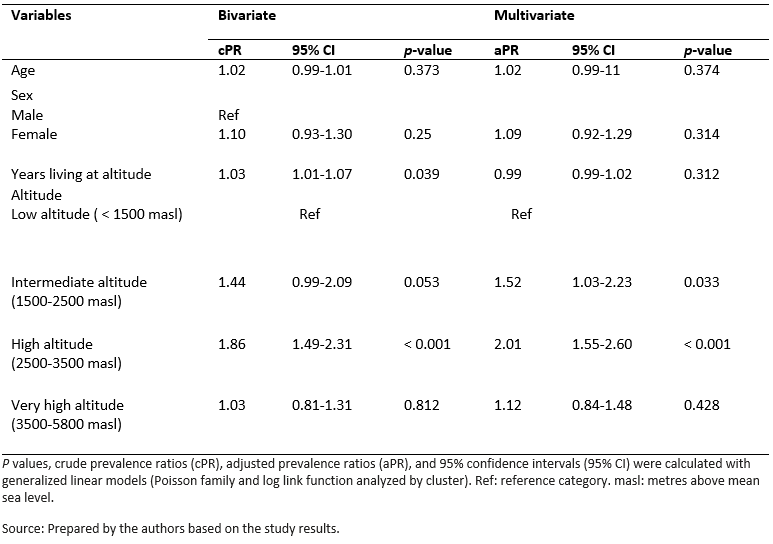 Table 2. Factors associated with chronic gastritis with crude and adjusted analyzes of outpatients in Peru.
Table 2. Factors associated with chronic gastritis with crude and adjusted analyzes of outpatients in Peru.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introducción
La gastritis crónica es unas de las enfermedades más comunes en la población y varía por regiones. Existen diversos factores que influyen en su aparición. Sin embargo, no se ha estudiado a profundidad el efecto de la altura.
Objetivos
Determinar la asociación entre la zona altitudinal de residencia y gastritis crónica en pacientes ambulatorios de Perú.
Métodos
Estudio transversal analítico. Se realizó a través del análisis secundario de datos. La variable dependiente fue gastritis crónica, tomada del reporte del paciente y verificado en la historia clínica, según antecedentes patológicos mencionados durante consulta médica. La variable independiente fue la zona altitudinal de residencia (divida en baja altitud, altitud intermedia, elevada y muy elevada). Las covariables secundarias fueron edad, sexo y tiempo viviendo en altura. Se realizaron modelos lineales generalizados para estimar razones de prevalencias, usando familia Poisson y ciudad como clúster.
Resultados
De los 4263 pacientes estudiados, 63% fue del sexo femenino; la mediana de la edad fue de 42 años. La prevalencia global de gastritis crónica fue 12,9%. Hubo asociación con gastritis crónica y altura de residencia a nivel intermedio, elevado, pero no con muy elevado, con una razón de prevalencia ajustada de 1,52 (intervalo de confianza 95%: 1,03 a 2,23); 2,01 (1,55 a 2,60) y 1,12 (0,84 a 1,48), respectivamente.
Conclusiones
Se encontró una asociación significativa entre gastritis crónica y altitud intermedia y elevada, pero no en muy elevada. Esto se explicaría por la hipoxia hipobárica en alturas, que podría conllevar lesiones en la pared gástrica, la adaptación de los peruanos a las alturas y por otras variables sociodemográficas.
 Authors:
Dante M. Quiñones-Laveriano[1], Jhony A. De La Cruz-Vargas[1], Sarah Quintana-Gomez[1], Virgilio E. Failoc-Rojas[2], José Lozano-Gutiérrez[1], Christian R. Mejia[3]
Authors:
Dante M. Quiñones-Laveriano[1], Jhony A. De La Cruz-Vargas[1], Sarah Quintana-Gomez[1], Virgilio E. Failoc-Rojas[2], José Lozano-Gutiérrez[1], Christian R. Mejia[3]
Affiliation:
[1] Instituto de Investigación en Ciencias Biomédicas, Universidad Ricardo Palma. Lima, Perú
[2] Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Universidad San Ignacio de Loyola. Lima, Perú
[3] Universidad Continental. Lima, Perú
E-mail: dante.quinones@urp.edu.pe
Author address:
[1] Jirón Junín # 881 Dep. C - 103 Lima, Perú Código postal: 15086

Citation: Quiñones-Laveriano DM, De La Cruz-Vargas JA, Quintana-Gomez S, Failoc-Rojas VE, Lozano-Gutiérrez J, Mejia CR. The altitude of residential areas and clinical diagnosis of chronic gastritis in ambulatory patients of Peru: A cross-sectional analytic study. Medwave 2020;20(6):e7972 doi: 10.5867/medwave.2020.06.7972
Submission date: 20/11/2019
Acceptance date: 21/6/2020
Publication date: 23/7/2020
Origin: Not commissioned
Type of review: Externally peer-reviewed by three reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Sipponen P, Maaroos HI. Chronic gastritis. Scand J Gastroenterol. 2015 Jun;50(6):657-67. | CrossRef | PubMed |
- Angós R. Gastritis. Med - Programa Form Médica Contin Acreditado. 2016 Feb;12(2):66–73. | CrossRef |
- Valdivia Roldán M. Gastritis y Gastropatías [Gastritis and gastropathies]. Rev Gastroenterol Peru. 2011 Jan-Mar;31(1):38-48. Spanish. | PubMed |
- Porras C, Nodora J, Sexton R, Ferreccio C, Jimenez S, Dominguez RL, et al. Epidemiology of Helicobacter pylori infection in six Latin American countries (SWOG Trial S0701). Cancer Causes Control. 2013 Feb;24(2):209-15. | CrossRef | PubMed |
- Ramírez-Ramos A, Gilman RH, Watanabe-Yamamoto J, Rosas-Aguirre A. Estudio de la epidemiología de la infección por el Helicobacter pylori en el Perú: 20 años después [Epidemiologic study of Helicobacter pylori infection in Perú]. Acta Gastroenterol Latinoam. 2004;34(2):69-78. Spanish. | PubMed |
- Sharma PK, Suri TM, Venigalla PM, Garg SK, Mohammad G, Das P, et al. Atrophic gastritis with high prevalence of Helicobacter pylori is a predominant feature in patients with dyspepsia in a high altitude area. Trop Gastroenterol. 2014 Oct-Dec;35(4):246-51. | CrossRef | PubMed |
- Carreño WD, García CP, Velásquez AMR, Dadán S. Trastornos gastrointestinales en pediatría asociados con la altura. Reporte de dos casos y revisión de la literatura [Pediatric gastrointestinal disorders at hight altitude. Report of two cases and review of literature.]. Acta Gastroenterol Latinoam. 2016 Mar;46(1):38-42. Spanish. | PubMed |
- Matu J, Deighton K, Ispoglou T, Duckworth L. The effect of moderate versus severe simulated altitude on appetite, gut hormones, energy intake and substrate oxidation in men. Appetite. 2017 Jun 1;113:284-292. | CrossRef | PubMed |
- Lahner E, Esposito G, Galli G, Annibale B. Atrophic gastritis and pre-malignant gastric lesions. Transl Gastrointest Cancer. 2015 Jun;4(4):272–81. | CrossRef |
- Sikri G, Bhattachar S. Acute mountain sickness and duration of pre-exposure to high altitude. Neuroreport. 2016 Sep 7;27(13):997. | CrossRef | PubMed |
- Anand AC, Sashindran VK, Mohan L. Gastrointestinal problems at high altitude. Trop Gastroenterol. 2006 Oct-Dec;27(4):147-53. | PubMed |
- Wu TY, Ding SQ, Liu JL, Jia JH, Dai RC, Zhu DC, et al. High-altitude gastrointestinal bleeding: an observation in Qinghai-Tibetan railroad construction workers on Mountain Tanggula. World J Gastroenterol. 2007 Feb 7;13(5):774-80. | CrossRef | PubMed |
- Berríos J, Sedano O, Calle E, Montero F, Manrique J, Hinostroza E. Hemorragia digestivea alta en los habitantes de las grandes alturas del Perú [Upper digestive hemorrhage in the inhabitants of high altitudes in Peru]. Rev Gastroenterol Peru. 1996 Jan-Apr;16(1):13-8. Spanish. | PubMed |
- Frisancho O. Dolicomegacolon Andino y vólvulos intestinales de altura [Dolichomegacolon of the Andes and intestinal volvulus due to altitude]. Rev Gastroenterol Peru. 2008 Jul-Sep;28(3):248-57. Spanish. | PubMed |
- Syam AF, Simadibrata M, Wanandi SI, Hernowo BS, Sadikin M, Rani AA. Gastric ulcers induced by systemic hypoxia. Acta Med Indones. 2011 Oct;43(4):243-8. | PubMed |
- Li K, Gesang L, He C. Mechanism of apoptosis involved in gastric mucosal lesions in Tibetans with high-altitude polycythemia. Exp Ther Med. 2017 Oct;14(4):3780-3787. | CrossRef | PubMed |
- Hamad N, Travis S. Gastrointestinal Function. In: High Altitude. Springer, New York, NY; 2014. p. 253–70. [On line] | Link |
- Mejia CR, Verastegui-Díaz A, Quiñones-Laveriano DM, Aranzabal-Alegría G,Failoc-Rojas VE. Actividad física y su asociación con enfermedades crónicas en ancianos de 11 ciudades del Perú [Physical activity and its association with chronic diseases in the elderly in 11 cities of Peru]. Gac Med Mex. 2017;153(4):480-485. Spanish. | CrossRef | PubMed |
- Ramírez Ramos A, Chinga Alayo E, Mendoza Requena D, Leey Casella J, Segovia Castro MC, Otoya C. Variacion de la prevalencia del H. pylori en le Perú período (1985-2002), en una población de nivel socioeconómico medio y alto [Changes in the prevalence of H. pylori in Perú; during the 1985-2002 period in medium and upper socio-economic strata]. Rev Gastroenterol Peru. 2003 Apr-Jun;23(2):92-8.Spanish. | PubMed |
- Soto G, Bautista CT, Roth DE, Gilman RH, Velapatiño B, Ogura M, et al; Gastrointestinal Physiology Working Group in Peru. Helicobacter pylori reinfection is common in Peruvian adults after antibiotic eradication therapy. J Infect Dis. 2003 Nov 1;188(9):1263-75. | CrossRef | PubMed |
- Li K, Gesang L, Dan Z, Gusang L, Dawa C, Nie Y. Transcriptome Reveals 1400-Fold Upregulation of APOA4-APOC3 and 1100-Fold Downregulation of GIF in the Patients with Polycythemia-Induced Gastric Injury. PLoS One. 2015 Oct 20;10(10):e0140534. | CrossRef | PubMed |
- Galvan Meza PJ, Escobar Orellana JC. Gastritis crónica confirmada por endoscopia digestiva alta: características clínicas y epidemiológicas en la altura (A 3280 msnm) - Hospital IV Essalud – Huancayo, 2008 [Tesis de grado]. Huancayo, Perú: Universidad Nacional del Centro del Perú; 2010. | Link |
- Li K, Gesang L, Dan Z, Dawa C, Gesang G, Ren D, et al. Endoscopic and histopathological features of Tibetans with high-altitude polycythemia. Int J Clin Exp Pathol. 2016;9(11):11631–11638.[On line] | Link |
- Berrios J. Algunas características del tracto gastrointestinal del habitante de las grandes alturas del Perú. Acta Andin. 1998;7(2):131–5.[On line] | Link |
- Pawar A, Sinha V, Sharma P, Sinha DK. High altitude area - A risk factor for gastric perforation? : A case series. Int J Surg Case Rep. 2018;53:429-432. | CrossRef | PubMed |
- Du Y, Bai Y, Xie P, Fang J, Wang X, Hou X, et al; Chinese Chronic Gastritis Research group. Chronic gastritis in China: a national multi-center survey. BMC Gastroenterol. 2014 Feb 7;14:21. | CrossRef | PubMed |
- Weck MN, Stegmaier C, Rothenbacher D, Brenner H. Epidemiology of chronic atrophic gastritis: population-based study among 9444 older adults from Germany. Aliment Pharmacol Ther. 2007 Sep 15;26(6):879-87. | CrossRef | PubMed |
- Nardone G, Rocco A, Compare D, De Colibus P, Autiero G, Pica L, et al. Is screening for and surveillance of atrophic gastritis advisable? Dig Dis. 2007;25(3):214-7. | CrossRef | PubMed |
- Oksanen T, Kivimäki M, Pentti J, Virtanen M, Klaukka T, Vahtera J. Self-report as an indicator of incident disease. Ann Epidemiol. 2010 Jul;20(7):547-54. | CrossRef | PubMed |
- Haapanen N, Miilunpalo S, Pasanen M, Oja P, Vuori I. Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol. 1997 Apr 15;145(8):762-9. | CrossRef | PubMed |
 Sipponen P, Maaroos HI. Chronic gastritis. Scand J Gastroenterol. 2015 Jun;50(6):657-67. | CrossRef | PubMed |
Sipponen P, Maaroos HI. Chronic gastritis. Scand J Gastroenterol. 2015 Jun;50(6):657-67. | CrossRef | PubMed | Angós R. Gastritis. Med - Programa Form Médica Contin Acreditado. 2016 Feb;12(2):66–73. | CrossRef |
Angós R. Gastritis. Med - Programa Form Médica Contin Acreditado. 2016 Feb;12(2):66–73. | CrossRef | Valdivia Roldán M. Gastritis y Gastropatías [Gastritis and gastropathies]. Rev Gastroenterol Peru. 2011 Jan-Mar;31(1):38-48. Spanish. | PubMed |
Valdivia Roldán M. Gastritis y Gastropatías [Gastritis and gastropathies]. Rev Gastroenterol Peru. 2011 Jan-Mar;31(1):38-48. Spanish. | PubMed | Porras C, Nodora J, Sexton R, Ferreccio C, Jimenez S, Dominguez RL, et al. Epidemiology of Helicobacter pylori infection in six Latin American countries (SWOG Trial S0701). Cancer Causes Control. 2013 Feb;24(2):209-15. | CrossRef | PubMed |
Porras C, Nodora J, Sexton R, Ferreccio C, Jimenez S, Dominguez RL, et al. Epidemiology of Helicobacter pylori infection in six Latin American countries (SWOG Trial S0701). Cancer Causes Control. 2013 Feb;24(2):209-15. | CrossRef | PubMed | Ramírez-Ramos A, Gilman RH, Watanabe-Yamamoto J, Rosas-Aguirre A. Estudio de la epidemiología de la infección por el Helicobacter pylori en el Perú: 20 años después [Epidemiologic study of Helicobacter pylori infection in Perú]. Acta Gastroenterol Latinoam. 2004;34(2):69-78. Spanish. | PubMed |
Ramírez-Ramos A, Gilman RH, Watanabe-Yamamoto J, Rosas-Aguirre A. Estudio de la epidemiología de la infección por el Helicobacter pylori en el Perú: 20 años después [Epidemiologic study of Helicobacter pylori infection in Perú]. Acta Gastroenterol Latinoam. 2004;34(2):69-78. Spanish. | PubMed | Sharma PK, Suri TM, Venigalla PM, Garg SK, Mohammad G, Das P, et al. Atrophic gastritis with high prevalence of Helicobacter pylori is a predominant feature in patients with dyspepsia in a high altitude area. Trop Gastroenterol. 2014 Oct-Dec;35(4):246-51. | CrossRef | PubMed |
Sharma PK, Suri TM, Venigalla PM, Garg SK, Mohammad G, Das P, et al. Atrophic gastritis with high prevalence of Helicobacter pylori is a predominant feature in patients with dyspepsia in a high altitude area. Trop Gastroenterol. 2014 Oct-Dec;35(4):246-51. | CrossRef | PubMed | Carreño WD, García CP, Velásquez AMR, Dadán S. Trastornos gastrointestinales en pediatría asociados con la altura. Reporte de dos casos y revisión de la literatura [Pediatric gastrointestinal disorders at hight altitude. Report of two cases and review of literature.]. Acta Gastroenterol Latinoam. 2016 Mar;46(1):38-42. Spanish. | PubMed |
Carreño WD, García CP, Velásquez AMR, Dadán S. Trastornos gastrointestinales en pediatría asociados con la altura. Reporte de dos casos y revisión de la literatura [Pediatric gastrointestinal disorders at hight altitude. Report of two cases and review of literature.]. Acta Gastroenterol Latinoam. 2016 Mar;46(1):38-42. Spanish. | PubMed | Matu J, Deighton K, Ispoglou T, Duckworth L. The effect of moderate versus severe simulated altitude on appetite, gut hormones, energy intake and substrate oxidation in men. Appetite. 2017 Jun 1;113:284-292. | CrossRef | PubMed |
Matu J, Deighton K, Ispoglou T, Duckworth L. The effect of moderate versus severe simulated altitude on appetite, gut hormones, energy intake and substrate oxidation in men. Appetite. 2017 Jun 1;113:284-292. | CrossRef | PubMed | Lahner E, Esposito G, Galli G, Annibale B. Atrophic gastritis and pre-malignant gastric lesions. Transl Gastrointest Cancer. 2015 Jun;4(4):272–81. | CrossRef |
Lahner E, Esposito G, Galli G, Annibale B. Atrophic gastritis and pre-malignant gastric lesions. Transl Gastrointest Cancer. 2015 Jun;4(4):272–81. | CrossRef | Sikri G, Bhattachar S. Acute mountain sickness and duration of pre-exposure to high altitude. Neuroreport. 2016 Sep 7;27(13):997. | CrossRef | PubMed |
Sikri G, Bhattachar S. Acute mountain sickness and duration of pre-exposure to high altitude. Neuroreport. 2016 Sep 7;27(13):997. | CrossRef | PubMed | Anand AC, Sashindran VK, Mohan L. Gastrointestinal problems at high altitude. Trop Gastroenterol. 2006 Oct-Dec;27(4):147-53. | PubMed |
Anand AC, Sashindran VK, Mohan L. Gastrointestinal problems at high altitude. Trop Gastroenterol. 2006 Oct-Dec;27(4):147-53. | PubMed | Wu TY, Ding SQ, Liu JL, Jia JH, Dai RC, Zhu DC, et al. High-altitude gastrointestinal bleeding: an observation in Qinghai-Tibetan railroad construction workers on Mountain Tanggula. World J Gastroenterol. 2007 Feb 7;13(5):774-80. | CrossRef | PubMed |
Wu TY, Ding SQ, Liu JL, Jia JH, Dai RC, Zhu DC, et al. High-altitude gastrointestinal bleeding: an observation in Qinghai-Tibetan railroad construction workers on Mountain Tanggula. World J Gastroenterol. 2007 Feb 7;13(5):774-80. | CrossRef | PubMed | Berríos J, Sedano O, Calle E, Montero F, Manrique J, Hinostroza E. Hemorragia digestivea alta en los habitantes de las grandes alturas del Perú [Upper digestive hemorrhage in the inhabitants of high altitudes in Peru]. Rev Gastroenterol Peru. 1996 Jan-Apr;16(1):13-8. Spanish. | PubMed |
Berríos J, Sedano O, Calle E, Montero F, Manrique J, Hinostroza E. Hemorragia digestivea alta en los habitantes de las grandes alturas del Perú [Upper digestive hemorrhage in the inhabitants of high altitudes in Peru]. Rev Gastroenterol Peru. 1996 Jan-Apr;16(1):13-8. Spanish. | PubMed | Frisancho O. Dolicomegacolon Andino y vólvulos intestinales de altura [Dolichomegacolon of the Andes and intestinal volvulus due to altitude]. Rev Gastroenterol Peru. 2008 Jul-Sep;28(3):248-57. Spanish. | PubMed |
Frisancho O. Dolicomegacolon Andino y vólvulos intestinales de altura [Dolichomegacolon of the Andes and intestinal volvulus due to altitude]. Rev Gastroenterol Peru. 2008 Jul-Sep;28(3):248-57. Spanish. | PubMed | Syam AF, Simadibrata M, Wanandi SI, Hernowo BS, Sadikin M, Rani AA. Gastric ulcers induced by systemic hypoxia. Acta Med Indones. 2011 Oct;43(4):243-8. | PubMed |
Syam AF, Simadibrata M, Wanandi SI, Hernowo BS, Sadikin M, Rani AA. Gastric ulcers induced by systemic hypoxia. Acta Med Indones. 2011 Oct;43(4):243-8. | PubMed | Li K, Gesang L, He C. Mechanism of apoptosis involved in gastric mucosal lesions in Tibetans with high-altitude polycythemia. Exp Ther Med. 2017 Oct;14(4):3780-3787. | CrossRef | PubMed |
Li K, Gesang L, He C. Mechanism of apoptosis involved in gastric mucosal lesions in Tibetans with high-altitude polycythemia. Exp Ther Med. 2017 Oct;14(4):3780-3787. | CrossRef | PubMed | Hamad N, Travis S. Gastrointestinal Function. In: High Altitude. Springer, New York, NY; 2014. p. 253–70. [On line] | Link |
Hamad N, Travis S. Gastrointestinal Function. In: High Altitude. Springer, New York, NY; 2014. p. 253–70. [On line] | Link | Mejia CR, Verastegui-Díaz A, Quiñones-Laveriano DM, Aranzabal-Alegría G,Failoc-Rojas VE. Actividad física y su asociación con enfermedades crónicas en ancianos de 11 ciudades del Perú [Physical activity and its association with chronic diseases in the elderly in 11 cities of Peru]. Gac Med Mex. 2017;153(4):480-485. Spanish. | CrossRef | PubMed |
Mejia CR, Verastegui-Díaz A, Quiñones-Laveriano DM, Aranzabal-Alegría G,Failoc-Rojas VE. Actividad física y su asociación con enfermedades crónicas en ancianos de 11 ciudades del Perú [Physical activity and its association with chronic diseases in the elderly in 11 cities of Peru]. Gac Med Mex. 2017;153(4):480-485. Spanish. | CrossRef | PubMed | Ramírez Ramos A, Chinga Alayo E, Mendoza Requena D, Leey Casella J, Segovia Castro MC, Otoya C. Variacion de la prevalencia del H. pylori en le Perú período (1985-2002), en una población de nivel socioeconómico medio y alto [Changes in the prevalence of H. pylori in Perú; during the 1985-2002 period in medium and upper socio-economic strata]. Rev Gastroenterol Peru. 2003 Apr-Jun;23(2):92-8.Spanish. | PubMed |
Ramírez Ramos A, Chinga Alayo E, Mendoza Requena D, Leey Casella J, Segovia Castro MC, Otoya C. Variacion de la prevalencia del H. pylori en le Perú período (1985-2002), en una población de nivel socioeconómico medio y alto [Changes in the prevalence of H. pylori in Perú; during the 1985-2002 period in medium and upper socio-economic strata]. Rev Gastroenterol Peru. 2003 Apr-Jun;23(2):92-8.Spanish. | PubMed | Soto G, Bautista CT, Roth DE, Gilman RH, Velapatiño B, Ogura M, et al; Gastrointestinal Physiology Working Group in Peru. Helicobacter pylori reinfection is common in Peruvian adults after antibiotic eradication therapy. J Infect Dis. 2003 Nov 1;188(9):1263-75. | CrossRef | PubMed |
Soto G, Bautista CT, Roth DE, Gilman RH, Velapatiño B, Ogura M, et al; Gastrointestinal Physiology Working Group in Peru. Helicobacter pylori reinfection is common in Peruvian adults after antibiotic eradication therapy. J Infect Dis. 2003 Nov 1;188(9):1263-75. | CrossRef | PubMed | Li K, Gesang L, Dan Z, Gusang L, Dawa C, Nie Y. Transcriptome Reveals 1400-Fold Upregulation of APOA4-APOC3 and 1100-Fold Downregulation of GIF in the Patients with Polycythemia-Induced Gastric Injury. PLoS One. 2015 Oct 20;10(10):e0140534. | CrossRef | PubMed |
Li K, Gesang L, Dan Z, Gusang L, Dawa C, Nie Y. Transcriptome Reveals 1400-Fold Upregulation of APOA4-APOC3 and 1100-Fold Downregulation of GIF in the Patients with Polycythemia-Induced Gastric Injury. PLoS One. 2015 Oct 20;10(10):e0140534. | CrossRef | PubMed | Galvan Meza PJ, Escobar Orellana JC. Gastritis crónica confirmada por endoscopia digestiva alta: características clínicas y epidemiológicas en la altura (A 3280 msnm) - Hospital IV Essalud – Huancayo, 2008 [Tesis de grado]. Huancayo, Perú: Universidad Nacional del Centro del Perú; 2010. | Link |
Galvan Meza PJ, Escobar Orellana JC. Gastritis crónica confirmada por endoscopia digestiva alta: características clínicas y epidemiológicas en la altura (A 3280 msnm) - Hospital IV Essalud – Huancayo, 2008 [Tesis de grado]. Huancayo, Perú: Universidad Nacional del Centro del Perú; 2010. | Link | Li K, Gesang L, Dan Z, Dawa C, Gesang G, Ren D, et al. Endoscopic and histopathological features of Tibetans with high-altitude polycythemia. Int J Clin Exp Pathol. 2016;9(11):11631–11638.[On line] | Link |
Li K, Gesang L, Dan Z, Dawa C, Gesang G, Ren D, et al. Endoscopic and histopathological features of Tibetans with high-altitude polycythemia. Int J Clin Exp Pathol. 2016;9(11):11631–11638.[On line] | Link | Berrios J. Algunas características del tracto gastrointestinal del habitante de las grandes alturas del Perú. Acta Andin. 1998;7(2):131–5.[On line] | Link |
Berrios J. Algunas características del tracto gastrointestinal del habitante de las grandes alturas del Perú. Acta Andin. 1998;7(2):131–5.[On line] | Link | Pawar A, Sinha V, Sharma P, Sinha DK. High altitude area - A risk factor for gastric perforation? : A case series. Int J Surg Case Rep. 2018;53:429-432. | CrossRef | PubMed |
Pawar A, Sinha V, Sharma P, Sinha DK. High altitude area - A risk factor for gastric perforation? : A case series. Int J Surg Case Rep. 2018;53:429-432. | CrossRef | PubMed | Du Y, Bai Y, Xie P, Fang J, Wang X, Hou X, et al; Chinese Chronic Gastritis Research group. Chronic gastritis in China: a national multi-center survey. BMC Gastroenterol. 2014 Feb 7;14:21. | CrossRef | PubMed |
Du Y, Bai Y, Xie P, Fang J, Wang X, Hou X, et al; Chinese Chronic Gastritis Research group. Chronic gastritis in China: a national multi-center survey. BMC Gastroenterol. 2014 Feb 7;14:21. | CrossRef | PubMed | Weck MN, Stegmaier C, Rothenbacher D, Brenner H. Epidemiology of chronic atrophic gastritis: population-based study among 9444 older adults from Germany. Aliment Pharmacol Ther. 2007 Sep 15;26(6):879-87. | CrossRef | PubMed |
Weck MN, Stegmaier C, Rothenbacher D, Brenner H. Epidemiology of chronic atrophic gastritis: population-based study among 9444 older adults from Germany. Aliment Pharmacol Ther. 2007 Sep 15;26(6):879-87. | CrossRef | PubMed | Nardone G, Rocco A, Compare D, De Colibus P, Autiero G, Pica L, et al. Is screening for and surveillance of atrophic gastritis advisable? Dig Dis. 2007;25(3):214-7. | CrossRef | PubMed |
Nardone G, Rocco A, Compare D, De Colibus P, Autiero G, Pica L, et al. Is screening for and surveillance of atrophic gastritis advisable? Dig Dis. 2007;25(3):214-7. | CrossRef | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








