Key Words: Hospitalization, child, adolescent, psychiatry, prognosis
Abstract
Introduction
Patients of the Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital (Valparaíso, Chile) exhibit different clinical and social characteristics compared to literature reports of other national centers, although published data are scarce.
Objectives
To describe the operation of the Unit, the socio-familial and clinical characteristics of its patients and analyze factors associated with their clinical evolution.
Methods
We performed a cross-sectional study to describe the patients hospitalized over a three-year period. Variables were registered in an anonymized database. Clinical evolution was evaluated over the year following hospital discharge.
Results
The Unit's model of care can be described as involving biomedical, psychodynamic, and ecological components. We included 98 patients, of which 70.4% were male, and the average age was 11.5 ± 2.3 years. 82.6% were of low socioeconomic status, and 35.7% did not attend school; 98.9% presented family dysfunction, and 91.8% of parents had a history of psychopathology. The most frequent reason for admission was the risk of harm to self or others. The most frequent discharge diagnoses were behav-ioral, depressive, and personality development disorders. The average length of stay was 41.8 ± 31.1 days. The most commonly used pharmacological agents were antipsychotics and mood stabilizers. Regarding clinical evolution in the first year post-discharge, 47% were evaluated as positive, 27% regular, and 26% unsatisfactory. The factor associated with an unsatisfactory clinical course was having had in-patient antidepressants. Re-admission during the first-year post-discharge was associated with comorbid substance use disorder. Treatment noncompliance was associated with a history of behavioral disorder at hospital dis-charge and having parents with a history of suicide or consummated suicide.
Conclusions
The patient profile is one of low socioeconomic status, severe psychopathology, maladaptive behavior, family dysfunction, and parental psychopathology. Substance use disorder is also associated with readmission.
|
Main messages
|
Introduction
In-hospital treatment is an important aspect in the care and management of children with severe psychiatric disorders, as evidenced by the recent increase in the annual rate of psychiatric hospitalizations in children and adolescents in developed countries[1]. This process is costly and not without complications[2],[3]. In any hospitalization, whether for psychiatric reasons or otherwise, up to 37% of youth may display some psychological sequelae, given the highly stressful situation for the child and family[4]. Further, hospitalization may even have traumatic consequences[5],[6].
During their time in hospital, children often suffer feelings of abandonment, and experience loneliness and guilt[5]. Regarding hospitalization for psychosocial reasons, such as suspected maltreatment and/or sexual abuse, the child's understanding of the problem is even more complex[7]. Admission to these units is therefore reserved for patients with severe psychiatric symptoms and are associated with complex psychosocial contexts (precarious support network, unprotected environments and/or severe maltreatment)[8],[9]. Thus, hospitalization should only occur where there is capacity to provide clinical stabilization and rapidly achieve a reduction in symptoms and risks[10].
Although there has been a significant increase in the availability of hospital beds for child psychiatry in Chile since the Ministry of Health implemented its Mental Health Plan in 2000[11], there is a significant lack of in-hospital resources for children, and the appropriate care model is currently under discussion[12]. Until 2007, there were seven beds exclusively destined for the hospitalization of children and adolescents in psychiatric care in Chile[13]. In 2014, ten short-stay units provided 125 beds, but there was an estimated shortage of at least 20 units[11]. Currently, there are 185 beds for children and adolescents requiring psychiatric care, 42% of which are in the Metropolitan Region and 21% in psychiatric hospitals[14].
Child and adolescent psychiatric hospitalization units and their therapeutic effectiveness have been described in many international studies[2]. However, results are limited primarily by the lack of standardized measures and difficulties inherent in performing randomized clinical trials in vulnerable populations[15]. In Latin America, studies on the subject are scarce. In Chile, characteristics of hospitalized populations and models of functioning have been described mainly for units that are not part of the public health network, which serves 74% of the population[16]. Internationally, research in this area is likewise scarce, and existing work is not recent. Adult psychiatric hospitalization in Chile has been extensively reported on, but to our knowledge, there are just three reports involving children and adolescents[9],[17],[18], two of which at the same unit[17],[18]. It therefore seems relevant to address this gap, especially in a public health and regional context.
The Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital, Valparaíso, Chile, designed for children and adolescents under 15 years of age, commenced operations in 2014 and has eight beds[19]. This article presents the sociodemographic, family, and clinical profile of patients at the Unit. Factors associated with clinical evolution are also analyzed.
Methods
Design and participants
A cross-sectional study was conducted to describe patients hospitalized at the Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital, from December 2014 to December 2017. Sampling was thus non-probabilistic. For patients who were hospitalized on more than one occasion, the first hospitalization was considered.
Data collection
This study was evaluated and approved by the Research Ethics Committee of the Valparaíso-San Antonio Health Service (approval number 051 2017). De-identified clinical and sociodemographic data were extracted from an anonymized database recorded by the clinical team. Informed consent was requested from parents to assess and extract data from the clinical record over the course of care. No interviews or direct assessment of the participants were carried out for the purpose of the present study.
Eligibility criteria correspond to those for admission to the Unit: Patients aged 15 years or less, with severe psychiatric pathology that, according to the criteria of the psychiatrist in charge, require hospitalization for diagnosis, psychosocial management and/or treatment. In addition, it was a requirement that patients exhibited stability from a medical-organic point of view. Patients that have violated the law are not admitted to the Unit as they have a separate specialized network for care.
Clinical features were evaluated according to the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders in its Fifth Version (DSM-5)[20]. The French Classification of Mental Disorders of Children and Adolescents (Item early psychosis - invasive developmental disorders) was used to study psychotic disharmony[21].
Clinical records of patients that received outpatient care at the Del Salvador Psychiatric Hospital were reviewed to determine progress at three months, six months, and one year following discharge. Progress was categorized as "good," "fair," or "unsatisfactory" according to the criteria used at the Unit. Good clinical evolution exemplified a response to treatment during hospitalization, and that response is maintained over the follow-up, exhibiting reduced or ameliorated symptoms that caused their admission. Fair clinical evolution is characterized by a reduction in some symptoms, which overall still affect their functionality, but not enough to require a new hospitalization. Unsatisfactory clinical evolution is exhibited by a relapse of symptoms that motivated hospitalization, such as suicidal behavior, dropping out of school, or other symptoms requiring readmission.
Data analysis
For descriptive statistics, proportions were used for qualitative variables and means with standard deviations for quantitative variables. Odds ratioswith their respective 95% confidence intervals were estimated to analyze factors associated with the clinical evolution. Data were analyzed using the Stata 15 statistical software (StataCorp, Texas, USA).
Results
The following is a description of the functioning of the Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital. Then, primary findings are reported according to the sociodemographic, family, and clinical characteristics of the patients, as well as to factors associated with clinical evolution.
Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital
This unit has a multilevel biopsychosocial model composed of:
- A biomedical model, led by child and adolescent psychiatrists, occupational therapists and nurses, in charge of diagnosing pathologies and caring for the different needs of patients.
- A psychodynamic model, led by child psychologists and child and adolescent psychiatrists, associated with the process of psychodiagnosis through projective techniques as well as individual and group interventions. The theoretical perspectives used emphasize Bowlby's attachment theory[22] and Winnicott's theory of dyadic relationships and psychic development[23].
- An ecological model developed by Urie Bronfenbrenner[24], which conceptualizes that the subject is a being that influences and is influenced by his or her environment, which is represented by a great interest in generating channels of communication between the different actors involved in the development of the child or adolescent: Coordination with schools, support programs, extended family, and outpatient therapists.
The phases of hospitalization include[19]:
- Comprehensive diagnosis.
- Clinical stabilization.
- Preparation for hospital discharge (pre-release).
- Follow-up.
Sociodemographic characteristics
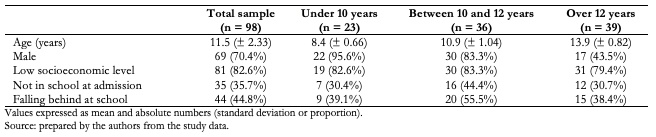
Ninety-eight patients were admitted over the study period, 70.4% of whom were men (n = 69). Ages ranged between 7 and 16 years, as, exceptionally, a 16-year-old patient with psychological functioning of a child, admitted to hospitalization in the adult units, was considered risky. The mean age was 11.5 years (standard deviation of 2.3 years). Children under 10 years of age constituted 23.47% (n = 23), 10-12 years old, 36.73% (n = 36), and over 12 years old, 39.8% (n = 39). A majority (82.6%; n = 81) were of a low socioeconomic level, corresponding to groups E and D of the Chilean socioeconomic classification model[21]. About a third (35.7%; n = 35) were outside of the school system; 22 of these cases were schooled again during hospitalization. Sociodemographic characteristics are presented in Table 1.
Table 1. Sociodemographic characteristics of the participants.
Family characteristics
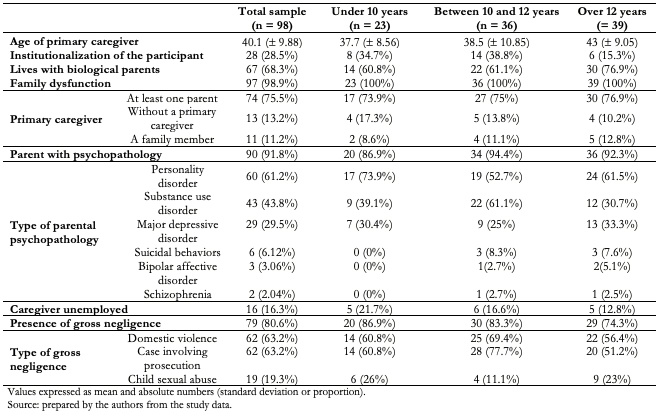
Almost all cases (n = 97) were classified as belonging to families with dysfunctional environments. The average age of the primary caregiver was 40.1 years (standard deviation of 9.88 years); 28.5% (n = 28) of children were institutionalized upon admission and, of these, 46.4% (n = 13) did not have a significant caregiver visiting them during hospitalization. 80.6% had a history of some type of serious negligence. 91.8% of parents presented a history of psychiatric pathology, where the most frequent was one of the personality disorders. Family characteristics are summarized in Table 2.
Table 2. Family characteristics of participants.
Reasons for admission, diagnosis at admission and discharge
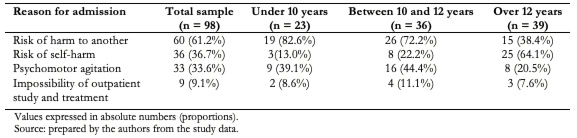
14.2% (n = 14) of patients were admitted involuntarily. The most frequent reason for hospitalization was risk of harm to others (61.2%). The distribution changed when stratified by age and/or sex. Regarding the diagnoses at admission, the three most frequent were conduct disorders (56.1%), intellectual disability (27.5%), and major depressive disorder (24.4%). The presence of symptoms from the suicide spectrum was observed in 41.8% (n = 41). Psychotic symptoms (either in isolation or in the context of a psychotic syndrome) were observed in 28.5% (n = 28) of cases, while antisocial behaviors were observed in 62.2% (n = 61). The reasons for admission are summarized in Table 3.
Table 3. Reasons for hospital admission of participants.
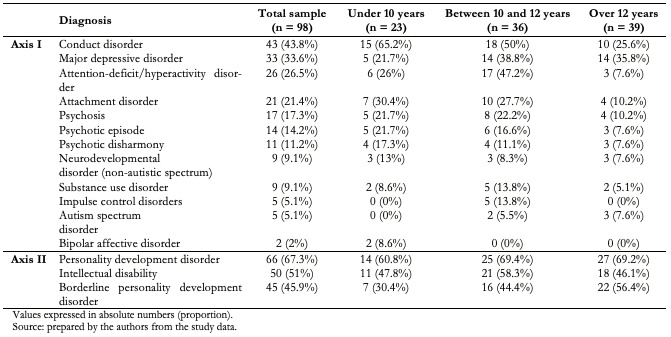
Following diagnostic study of each case, the most frequent discharge diagnoses in axis I were conduct disorders (43.8%) and major depressive disorder (33.6%), while in axis II the majority was personality development disorder of borderline structure (45.9%). Table 4 shows discharge diagnoses according to axis I and II.
Table 4. Participants' diagnosis at discharge.
Hospitalization process
The multidisciplinary team consists of child and adolescent psychiatrists, child and adolescent psychologists, social workers, occupational therapists, nurses, paramedical technicians, and assistants. In addition, there is a hospital school. The average length of hospital stay was 41.8 days (standard deviation of 31.1 days), ranging from 4 to 212 days and mode of 28 days. The management of each patient incorporated individual and family assessments, together with a complete social diagnosis. In most cases psychodiagnoses were performed with projective tests and psychometry, in addition to clinical interviews, according to clinical need (54% of cases). It should be noted that, during the hospitalization process, the average number of physical restraints was two times (standard deviation of 3.1 times) for the entire sample. Twelve patients (12.2%) received no visits during hospitalization.
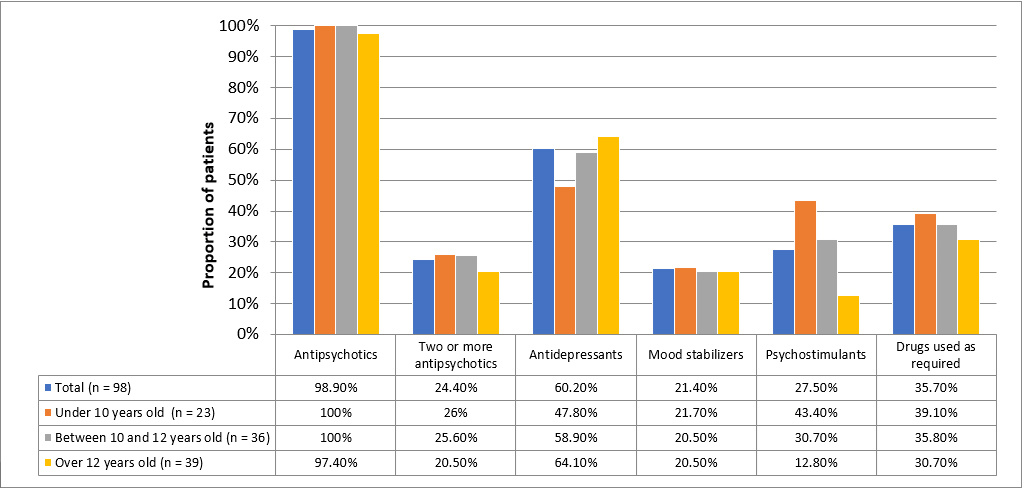
Regarding psychopharmacological treatment, antipsychotics, antidepressants, mood stabilizers, and psychostimulants were used primarily. Antipsychotics were the most widely used drugs, with 98.9% of patients using at least one antipsychotic as a basic pharmacological treatment and 24.4% using two or more. Second-generation antipsychotics were mainly used. Chlorpromazine was the only first-generation antipsychotic used, being indicated as use "when required" for containment or as a booster to a second-generation antipsychotic. The most commonly prescribed antipsychotic was quetiapine (n = 45), followed by risperidone (n = 31). Antidepressants were used in 59 patients, most of which were selective serotonin reuptake inhibitors. The most frequently used antidepressant was fluoxetine (n = 30), followed by sertraline (n = 11). Figure 1 summarizes the use of psychotropic drugs in the group studied.
Figure 1. Proportion of patients by type of psychopharmacological agent.
Clinical evolution
Ninety-two patients continued outpatient treatment at the Del Salvador Psychiatric Hospital following discharge; 47% (n = 43) met the criteria of a good evolution, 27% (n = 25) were classified as fair and 26% (n = 24) as unsatisfactory. Twenty-one patients (21.4%) were readmitted, some of whom were hospitalized at the adult’s unit as they were over 15 years old. Seven patients were readmitted during the first three months following discharge, all with a history of suicidal ideation and/or suicide attempt. In this group, one death by suicide occurred, six months after the initial hospitalization. Seven patients were readmitted between three months and one year of hospitalization; all were male and six presented antisocial behavior and/or were out of school.
The only factor significantly associated with an unsatisfactory clinical course was indication for an antidepressant during hospitalization (odds ratio: 4.72; 95% confidence interval: 1.3 to 16.1). Patients evidencing poor adherence to treatment, exhibited an odds ratio of 2.2 of having presented depressive symptoms (95% confidence interval: 1.2 to 3.5).
Patients who were readmitted less than three months post-discharge were at increased odds to have exhibited self-harm (odds ratio: 12; 95% confidence interval: 1.2 to 115.4) or substance use disorder on admission (odds ratio: 12; 95% confidence interval: 3.3 to 44.7). Patients readmitted between three and six months after discharge were at increased odds of having presented suicide on admission (odds ratio: 5.6; 95% confidence interval: 1.05 to 30.8) or a substance use disorder on admission (odds ratio 6.3; 95% confidence interval: 2 to 20). The only variable significantly associated with readmission six months to one year after discharge was substance use disorder on admission (odds ratio: 4.1; 95% confidence interval: 1.5 to 11).
Treatment withdrawal during outpatient follow-up associated with behavioral disorder at discharge (odds ratio 5.2; 95% confidence interval: 1.2 to 21.8) and parental history of attempted or committed suicide (odds ratio 7.4; 95% confidence interval: 1.2 to 2.45).
Discussion
In the present study we describe characteristics of the patients hospitalized in the Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital over a three-year period, analyzing factors associated with clinical evolution. The unit is organized according to a biopsychosocial approach that follows three models[19],[22],[23],[24], an eclectic and innovative perspective for this type of unit, observed in other centers in Latin America[25]. Most patients come from multi-problem families, of a low socioeconomic level, with a history of having suffered mistreatment and/or gross negligence and with parents that present some psychiatric pathology. Primary diagnoses were conduct disorder, major depressive disorder and development personality disorders, while substance use disorder was a factor consistently and significantly associated with hospital readmission. About half of the patients met criteria of good clinical evolution, while in one third the evolution was considered fair, and in one quarter unsatisfactory.
The first Chilean study in this area was published in 2007 by Pacheco and colleagues[17]. It was conducted in the Child Psychiatry Unit of a university psychiatric clinic, where the prevalent clinical profile was an average age of 15 years, the primary reason for hospitalization was suicide attempt, the predominant diagnosis in axis I was major depressive disorder, and the average hospital stay was 11 days. Later, the same research group published a case-control study conducted in the same unit[18], where it was found that among patients hospitalized for attempted suicide, the diagnosis of depression was more frequent.
In 2009, de la Barra and colleagues[9] described the characteristics of patients hospitalized in a Children's Psychiatric Hospitalization Service in a private general hospital, where they highlighted that the most frequent reason for admission was suicidal behavior, mood disorders as the most frequent pathology of axis I and an average hospitalization of 3.8 days. In the present study, the duration of hospitalizations on average was longer than described in national[9],[17] and international[26],[27],[28] literature. The need for longer hospitalizations may be explained by the high clinical complexity[29] and the social and family context[30], but also by administrative needs related to the patient's continuity outside hospital, e.g., admission to residences of the National Service for Minors, waiting for a legal resolution of proceedings in the family court, among others.
In our study, the greater frequency of men differs from that observed in local research[9],[17] and abroad[28],[31],[32], where a greater proportion of women predominates. Our findings are consistent with research in units for children under 12, where a higher proportion of men is common[2]. In the current work, clinical characteristics of patients varied with age, since in children under 12 years a male profile was observed more frequently, whereby reason for admission was predominantly risk of harm to others and/or psychomotor agitation. In children over 12 years, a predominantly female profile was evident, where the most common reason for admission was risk of self-harm and the most frequent diagnosis was major depressive disorder. A highly dysfunctional social and family environment was homogeneous across age groups. In this sense, the patients studied represent severe cases, both in psychiatric pathology and in psychosocial complexity, as highlighted by, for example, dropout from school. It is important to bear in mind that this unit is a tertiary referral center that attends to patients who are highly selected for their severity, with a history of multiple treatments and poor results to prior interventions.
The predominance of a profile of patients with symptomatology of the externalizing sphere, mainly behavioral, responds to the characteristics of the unit under study, since it is complex that children with this profile be managed in a pediatric ward of a general hospital. These patients require a large and safe physical space, and a nursing team trained in behavioral management, especially when pharmacological and/or physical containment is part of the picture. In addition, in patients living with multi-problem families, family and psychosocial interventions are of a primary necessity. Such patients in the Valparaíso region are therefore referred to this Short-stay Unit.
In this line, it has been stated that children with severe conduct disorders present a distorted and/or deficient personality structure[33], a statement that is consistent with the high proportion of development personality disorders found in this sample of patients. There are authors who assert that this diagnosis could not be made during adolescence, since the structure of the personality is still unstable and dynamic, therefore, the concept of "development" emphasizes a structure not consolidated in traits and permanent functioning and an identity not fully integrated[34],[35]. However, there are several studies that conclude that, despite the fact that the personality is developing, the diagnosis of development personality disorder is stable, even when made in early adolescence, between 12 and 14 years[36], which would also allow for the visualization of earlier and more effective long-term intervention in hospitalized patients[17],[32]. Indeed, some research proposes a systematic assessment of personality structure in high-risk populations such as hospitalized adolescents, as this would be useful in case of conceptualization and treatment planning[35].
As for the admission and discharge diagnoses, differences could be explained by the team that performs them, since the admission diagnosis is given by the professionals treating the patient on an outpatient basis, while the discharge diagnosis is performed by the unit's multidisciplinary team. Likewise, it can be explained by the complexity of the social and family context of each patient, which is associated with atypical clinical presentations that are difficult to diagnose. This would explain, for example, the decrease in conduct disorder between admission and discharge, since sometimes depressive or attachment clinical pictures may initially become present as disruptive behaviors that may be confused with conduct disorders. In short, during hospitalization the patient can be observed in depth and continuously, evaluating biological rhythms, episodes of crisis and agitation, as well as interaction with peers and adults.
The sample represents multi-problem families with dysfunction, including intrafamily conflictive relationships, family breakdown, mourning, mistreatment, abuse and/or negligence. However, we do not know the extent to which this dysfunction is a symptomatic expression of episodic stress for the family due to having a sick member, or if it is a structural condition. Either way, it has been recognized that family dysfunction worsens the patient's prognosis[37]. More than 90% of cases presented a parent with severe psychiatric pathology, which does not consider interventions in parental skills as a therapy. During the hospitalization of their children, parents are referred for treatment if necessary and coordination is made with the treatment teams at the primary or secondary level, but there is no a treatment Unit that integrally addresses the family's psychiatric pathology. It is worth noting that 13.2% did not have a significant primary caregiver, that is, they were children who had been abandoned by their direct relatives and who lived in residences of the National Service for Minors. During the hospitalization process, an affective adult reference person is always included in the intervention to accompany the patient, even if they did not live with him/her.
In terms of pharmacological treatment, the use of antipsychotics and antidepressants predominated; 98.9% were indicated at least one antipsychotic at discharge and 24.4% received two or more antipsychotics (without considering those indicated in case of emergency). The high frequency of use may be related to the ubiquitous functions, since they are used for treatment of psychosis, mania and psychomotor agitation, among others. Quetiapine was the most widely used antipsychotic, possibly because its use in low doses (non-antipsychotic) responds to the need for psychopharmacological treatment of some insomnia conditions[38].
A fundamental objective of hospital interventions is improving the functioning and psychosocial adaptation to daily life. In this sense, re-schooling is essential. Of 35 patients who were not in school at the time of admission, 22 were re-schooled during the hospitalization episode. However, re-schooling did not associate with good clinical evolution, as would have been expected.
About a third (26%) of the patients were classified as having unsatisfactory clinical evolution. The only factor significantly associated with this was indication for an antidepressant (odds ratio: 4.72; 95% confidence interval: 1.3 to 16.1). However, for those with additional depressive symptoms, odds of non-adherence to treatment was 2.2 (95% confidence interval: 1.2 to 3.5). This is consistent with existing literature[39].
Psychiatric hospital readmission is a frequent phenomenon in the child and adolescent population[40], especially if the families of the patients demonstrate high levels of dysfunction, as is the case here. We worked on the basis that readmissions prior to the year post-discharge could represent relapse, while readmissions after a year might correspond to independent episodes.
Readmissions during the first three months were significantly associated with higher odds of having been admitted with risk of self-harm and substance use disorder on admission. Both factors suggest patients with higher levels of impulsivity, weaker functioning, poorer coping strategies, and more risky behaviors. There is a degree of imprecision as evidenced by large confidence intervals. Readmission at three to six months associated with presence of suicidality and substance use disorder, consistent with the findings of other studies[40],[41]. It would be prudent to consider strict follow-up in patients with suicidality, as this appears to be a strong predictor of rehospitalization[40].
In patients readmitted between 6 months and 1 year, the impulsivity factor remains an element to be considered, since the only variable that remained significantly associated was having a substance use disorder (odds ratio: 4.1; 95% confidence interval: 1.5 to 11). It should be noted that the most frequent axis I pathology in parents was also a substance use disorder.
Within the limitations of this study, heterogeneity in diagnosis and recording clinical information is likely, and is inherent in retrospective data collection. This may have biased some results. We unfortunately could not report on the clinical evolution of patients whose follow-up was carried out in other centers. Due to the sample size, some associations may not emerge due to lack of power.
Conclusion
Child and adolescent psychiatric hospitalization is justified as an intervention when behavioral expression is maladaptive and psychopathology is severe, especially in highly complex socio-familial environments, as it is seen in the present work. Although restrictive, in these cases it could constitute an appropriate and timely therapeutic intervention for safe and effective management of acute clinical situations.
We propose, however, that child and adolescent psychiatric hospitalization units should be inserted in general hospitals and part of the community, as suggested in 2016 by the American Psychiatric Association (APA)[42] and, in 2019, by the Chilean Society of Child and Adolescent Psychiatry and Neurology (SOPNIA)[12]. Therefore, this study is not expected to be confused with validation of isolated and remote community psychiatric practice.
Notes
Authorship contributions
MJB, FL: conceptualization, methodology, formal analysis, investigation, resources, writing (original draft preparation), writing (review and editing), visualization, supervision, project administration. JS, MB, LAD: methodology, resources, writing (original draft preparation), writing (review and editing), visualization. MA: conceptualization, methodology, formal analysis, investigation, writing (original draft preparation), writing (review and editing), visualization, supervision.
Funding
The authors declare that there were no external sources of funding.
Competing interests
The authors have completed the ICMJE conflict of interest declaration form and declare that they have not received funding for the completion of this report; have had no financial relationships in the last three years with organizations that might have an interest in the published article; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the corresponding author or the editorial board of the Journal.
Ethics
This study was evaluated and approved by the Research Ethics Committee of the Valparaíso-San Antonio Health Service (approval number 051 2017).
From the editors
The original version of this article was submitted in Spanish. This is the English translation of the original article, lightly copyedited by the Journal.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introduction
Patients of the Short-stay Child and Adolescent Unit of the Del Salvador Psychiatric Hospital (Valparaíso, Chile) exhibit different clinical and social characteristics compared to literature reports of other national centers, although published data are scarce.
Objectives
To describe the operation of the Unit, the socio-familial and clinical characteristics of its patients and analyze factors associated with their clinical evolution.
Methods
We performed a cross-sectional study to describe the patients hospitalized over a three-year period. Variables were registered in an anonymized database. Clinical evolution was evaluated over the year following hospital discharge.
Results
The Unit's model of care can be described as involving biomedical, psychodynamic, and ecological components. We included 98 patients, of which 70.4% were male, and the average age was 11.5 ± 2.3 years. 82.6% were of low socioeconomic status, and 35.7% did not attend school; 98.9% presented family dysfunction, and 91.8% of parents had a history of psychopathology. The most frequent reason for admission was the risk of harm to self or others. The most frequent discharge diagnoses were behav-ioral, depressive, and personality development disorders. The average length of stay was 41.8 ± 31.1 days. The most commonly used pharmacological agents were antipsychotics and mood stabilizers. Regarding clinical evolution in the first year post-discharge, 47% were evaluated as positive, 27% regular, and 26% unsatisfactory. The factor associated with an unsatisfactory clinical course was having had in-patient antidepressants. Re-admission during the first-year post-discharge was associated with comorbid substance use disorder. Treatment noncompliance was associated with a history of behavioral disorder at hospital dis-charge and having parents with a history of suicide or consummated suicide.
Conclusions
The patient profile is one of low socioeconomic status, severe psychopathology, maladaptive behavior, family dysfunction, and parental psychopathology. Substance use disorder is also associated with readmission.
 Authors:
María José Barker[1], Fanny Leyton[1], Jana Stojanova[2], Marcelo Briceño[1], Luis Alberto Dueñas[1], Marcelo Arancibia[2]
Authors:
María José Barker[1], Fanny Leyton[1], Jana Stojanova[2], Marcelo Briceño[1], Luis Alberto Dueñas[1], Marcelo Arancibia[2]
Affiliation:
[1] Departamento de Pediatría, Cátedra de Psiquiatría Infanto-juvenil, Escuela de Medicina, Universidad de Valparaíso, Viña del Mar, Chile
[2] Centro Interdisciplinario de Estudios en Salud (CIESAL), Escuela de Medicina, Universidad de Valparaíso, Viña del Mar, Chile
E-mail: marcelo.arancibiame@uv.cl
Author address:
[1] Angamos 655
Edificio R2, Oficina 1107
Reñaca, Viña del Mar
Chile.

Citation: Barker M J, Leyton F, Stojanova J, Briceño M, Dueñas L A, Arancibia M. . Medwave 2020;20(2):e7853 doi: 10.5867/medwave.2020.02.7853
Submission date: 8/11/2019
Acceptance date: 18/2/2020
Publication date: 24/3/2020
Origin: Not commissioned.
Type of review: Externally peer-reviewed by three reviewers, double-blind.

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Van Horne B, Netherton E, Helton J, Fu M, Greeley C. The Scope and Trends of Pediatric Hospitalizations in Texas, 2004-2010. Hosp Pediatr. 2015 Jul;5(7):390-8. | CrossRef | PubMed |
- Green J, Jacobs B, Beecham J, Dunn G, Kroll L, Tobias C, Briskman J. Inpatient treatment in child and adolescent psychiatry--a prospective study of health gain and costs. J Child Psychol Psychiatry. 2007 Dec;48(12):1259-67. | CrossRef | PubMed |
- Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001 Jul 28;323(7306):191. | CrossRef | PubMed |
- Vessey JA. Children's psychological responses to hospitalization. Annu Rev Nurs Res. 2003;21:173-201. | PubMed |
- Hernández E, Rabadán J. La hospitalización: un paréntesis en la vida del niño. Atención educativa en población infantil hospitalizada. Perspect Educ. 2013;52(1):167–81. [Internte] | Link |
- Méndez X, Orgilés M, López-Roig S, Espada J. Atención psicológica en el cáncer infantil. Psicooncología. 2004;1(1):139–54. | CrossRef |
- Bella ME, Borgiattino V. [Demand for hospitalization due to psychosocial causes in a pediatric hospital]. Arch Argent Pediatr. 2016 Jun 1;114(3):252-7. | CrossRef | PubMed |
- Costello AJ, Dulcan MK, Kalas R. A checklist of hospitalization criteria for use with children. Hosp Community Psychiatry. 1991 Aug;42(8):823-8. | CrossRef | PubMed |
- de la Barra F, García R. Hospitalización psiquiátrica de niños y adolescentes II: experiencia clínica en un hospital general privado. Rev Chil Neuro-Psiquiatr. 2009;47(3):238–43. | CrossRef |
- Lamb CE. Alternatives to admission for children and adolescents: providing intensive mental healthcare services at home and in communities: what works? Curr Opin Psychiatry. 2009 Jul;22(4):345-50. | CrossRef | PubMed |
- Subsecretaría de Salud Pública. Plan de Salud Mental 2016-2020. Ministerio de Salud de Chile. 2015.
- Sociedad de Psiquiatría y Neurología de la Infancia y Adolescencia (SOPNIA). Comunicado Oficial. Declaración respecto Hospital Psiquiátrico Phillipe Pinel de Putaendo. Santiago; 2019.
- Pesce C. Hospitalización psiquiátrica infanto-juvenil en Chile: reflexión en torno a su implementación, diagnóstico del estado actual y proyecciones futuras. Rev Chil Psiquiatr Neurol Infanc Adolesc. 2014;25(1):27–36.
- Ministerios de Salud de Chile. Modelo de Gestión. Red Temática de Salud Mental en la Red General de Salud. Santiago; 2018. [Internet] | Link |
- de la Barra F, García R. Hospitalización psiquiátrica de niños y adolescentes I: revisión de la literatura. Rev Chil Neuro-Psiquiatr. 2009;47(3):228–37. | CrossRef |
- Minoletti A, Zaccaria A. Plan Nacional de Salud Mental en Chile: 10 años de experiencia. Rev Panam Salud Publica. 2005;18(4):346–58. [Internet] | Link |
- Pacheco P B, Lizana C P, Celhay S I, Pereira Q J. [Clinical characteristics of children and adolescent hospitalized in a university psychiatric clinic]. Rev Med Chil. 2007 Jun;135(6):751-8. | CrossRef | PubMed |
- Pacheco B, Lizana P, Celhay I. [Clinical differences between suicide and non suicide attempter hospitalized adolescents]. Rev Med Chil. 2010 Feb;138(2):160-7. | CrossRef | PubMed |
- Díaz J. Manual de Organización Unidad de Corta Estadía Infanto-juvenil Hospital Psiquiátrico del Salvador, Valparaíso; 2014.
- Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington; 2013. | CrossRef |
- Beraudi A, Asociación Franco-Argentina de Psiquiatría y Salud Mental. Clasificación Francesa de los Trastornos Mentales del Niño y del Adolescente. Buenos Aires: Polemos; 2004.
- Bowlby J. Attachment theory, separation anxiety and mourning.American Handbook of Psychiatry. 2nd Ed. New York. 1975.
- Winnicott D. Playing and reality. Tavistock Publications. 1st Ed. London. 1971.
- Bronfenbrenner U. The ecology of human development. Harvard University Press. Cambridge;1979.
- Márquez-Caraveo ME, Arroyo-García E, Granados-Rojas A, Ángeles-Llerenas A. [Children's Psychiatric Hospital Dr. Juan N. Navarro: 50 years of attention to the mental health of children and adolescents in Mexico]. Salud Publica Mex. 2017 Jul-Aug;59(4):477-484. | CrossRef | PubMed |
- Pfeiffer SI, Strzelecki SC. Inpatient psychiatric treatment of children and adolescents: a review of outcome studies. J Am Acad Child Adolesc Psychiatry. 1990 Nov;29(6):847-53. | CrossRef | PubMed |
- Bardach NS, Coker TR, Zima BT, Murphy JM, Knapp P, Richardson LP, Edwall G, Mangione-Smith R. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014 Apr;133(4):602-9. | CrossRef | PubMed |
- Duarte V, Zelaya L. Caracterización clínica y demográfica de la hospitalización psiquiátrica infanto-juvenil en un hospital general. Pediatr. 2019;46(2):90–6. | CrossRef |
- Masters GA, Baldessarini RJ, Öngür D, Centorrino F. Factors associated with length of psychiatric hospitalization. Compr Psychiatry. 2014 Apr;55(3):681-7. | CrossRef | PubMed |
- Gold J, Shera D, Clarkson B Jr. Private psychiatric hospitalization of children: predictors of length of stay. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):135-43. | CrossRef | PubMed |
- Hanssen-Bauer K, Heyerdahl S, Hatling T, Jensen G, Olstad PM, Stangeland T, et al. Admissions to acute adolescent psychiatric units: a prospective study of clinical severity and outcome. Int J Ment Health Syst. 2011 Jan 6;5(1):1. | CrossRef | PubMed |
- Pupo-González L, Nogueras-Reyes Y, de Prada-Justel ME, Labrada-Pupo D. Salud mental infanto juvenil, características de una problemática actual. Rev Electrónica Dr Zoilo E Mar Vidaurreta. 2018;43(6). [Internet] | Link |
- Kernberg P, Chazan S. Niños con desórdenes de conducta. Manual de psicoterapia. Santiago: Mediterráneo. 2018. 1;18–19.
- Bradley R, Zittel Conklin C, Westen D. The borderline personality diagnosis in adolescents: gender differences and subtypes. J Child Psychol Psychiatry. 2005 Sep;46(9):1006-19. | CrossRef | PubMed |
- Glenn CR, Klonsky ED. Reliability and validity of borderline personality disorder in hospitalized adolescents. J Can Acad Child Adolesc Psychiatry. 2013 Aug;22(3):206-11. | PubMed |
- Stepp SD, Pilkonis PA, Hipwell AE, Loeber R, Stouthamer-Loeber M. Stability of borderline personality disorder features in girls. J Pers Disord. 2010 Aug;24(4):460-72. | CrossRef | PubMed |
- Sourander A, Piha J. Three-year follow-up of child psychiatric inpatient treatment. Eur Child Adolesc Psychiatry. 1998 Sep;7(3):153-62. | CrossRef | PubMed |
- Saldaña SN, Keeshin BR, Wehry AM, Blom TJ, Sorter MT, DelBello MP, Strawn JR. Antipsychotic polypharmacy in children and adolescents at discharge from psychiatric hospitalization. Pharmacotherapy. 2014 Aug;34(8):836-44. | CrossRef | PubMed |
- Staton D. Achieving adolescent adherence to treatment of major depression. Adolesc Health Med Ther. 2010 Aug 4;1:73-85. | CrossRef | PubMed |
- Joyce VW, King CD, Nash CC, Lebois LAM, Ressler KJ, Buonopane RJ. Predicting Psychiatric Rehospitalization in Adolescents. Adm Policy Ment Health. 2019 Nov;46(6):807-820. | CrossRef | PubMed |
- Bobier C, Warwick M. Factors associated with readmission to adolescent psychiatric care. Aust N Z J Psychiatry. 2005 Jul;39(7):600-6. | CrossRef | PubMed |
- American Psychiatric Association. APA Official Actions. Position Statement on Psychiatric Hospitalization of Children and Adolescents. Washignton. 2016.
 Van Horne B, Netherton E, Helton J, Fu M, Greeley C. The Scope and Trends of Pediatric Hospitalizations in Texas, 2004-2010. Hosp Pediatr. 2015 Jul;5(7):390-8. | CrossRef | PubMed |
Van Horne B, Netherton E, Helton J, Fu M, Greeley C. The Scope and Trends of Pediatric Hospitalizations in Texas, 2004-2010. Hosp Pediatr. 2015 Jul;5(7):390-8. | CrossRef | PubMed | Green J, Jacobs B, Beecham J, Dunn G, Kroll L, Tobias C, Briskman J. Inpatient treatment in child and adolescent psychiatry--a prospective study of health gain and costs. J Child Psychol Psychiatry. 2007 Dec;48(12):1259-67. | CrossRef | PubMed |
Green J, Jacobs B, Beecham J, Dunn G, Kroll L, Tobias C, Briskman J. Inpatient treatment in child and adolescent psychiatry--a prospective study of health gain and costs. J Child Psychol Psychiatry. 2007 Dec;48(12):1259-67. | CrossRef | PubMed | Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001 Jul 28;323(7306):191. | CrossRef | PubMed |
Scott S, Knapp M, Henderson J, Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001 Jul 28;323(7306):191. | CrossRef | PubMed | Vessey JA. Children's psychological responses to hospitalization. Annu Rev Nurs Res. 2003;21:173-201. | PubMed |
Vessey JA. Children's psychological responses to hospitalization. Annu Rev Nurs Res. 2003;21:173-201. | PubMed | Hernández E, Rabadán J. La hospitalización: un paréntesis en la vida del niño. Atención educativa en población infantil hospitalizada. Perspect Educ. 2013;52(1):167–81. [Internte] | Link |
Hernández E, Rabadán J. La hospitalización: un paréntesis en la vida del niño. Atención educativa en población infantil hospitalizada. Perspect Educ. 2013;52(1):167–81. [Internte] | Link | Méndez X, Orgilés M, López-Roig S, Espada J. Atención psicológica en el cáncer infantil. Psicooncología. 2004;1(1):139–54. | CrossRef |
Méndez X, Orgilés M, López-Roig S, Espada J. Atención psicológica en el cáncer infantil. Psicooncología. 2004;1(1):139–54. | CrossRef | Bella ME, Borgiattino V. [Demand for hospitalization due to psychosocial causes in a pediatric hospital]. Arch Argent Pediatr. 2016 Jun 1;114(3):252-7. | CrossRef | PubMed |
Bella ME, Borgiattino V. [Demand for hospitalization due to psychosocial causes in a pediatric hospital]. Arch Argent Pediatr. 2016 Jun 1;114(3):252-7. | CrossRef | PubMed | Costello AJ, Dulcan MK, Kalas R. A checklist of hospitalization criteria for use with children. Hosp Community Psychiatry. 1991 Aug;42(8):823-8. | CrossRef | PubMed |
Costello AJ, Dulcan MK, Kalas R. A checklist of hospitalization criteria for use with children. Hosp Community Psychiatry. 1991 Aug;42(8):823-8. | CrossRef | PubMed | de la Barra F, García R. Hospitalización psiquiátrica de niños y adolescentes II: experiencia clínica en un hospital general privado. Rev Chil Neuro-Psiquiatr. 2009;47(3):238–43. | CrossRef |
de la Barra F, García R. Hospitalización psiquiátrica de niños y adolescentes II: experiencia clínica en un hospital general privado. Rev Chil Neuro-Psiquiatr. 2009;47(3):238–43. | CrossRef | Lamb CE. Alternatives to admission for children and adolescents: providing intensive mental healthcare services at home and in communities: what works? Curr Opin Psychiatry. 2009 Jul;22(4):345-50. | CrossRef | PubMed |
Lamb CE. Alternatives to admission for children and adolescents: providing intensive mental healthcare services at home and in communities: what works? Curr Opin Psychiatry. 2009 Jul;22(4):345-50. | CrossRef | PubMed | Subsecretaría de Salud Pública. Plan de Salud Mental 2016-2020. Ministerio de Salud de Chile. 2015.
Subsecretaría de Salud Pública. Plan de Salud Mental 2016-2020. Ministerio de Salud de Chile. 2015.  Sociedad de Psiquiatría y Neurología de la Infancia y Adolescencia (SOPNIA). Comunicado Oficial. Declaración respecto Hospital Psiquiátrico Phillipe Pinel de Putaendo. Santiago; 2019.
Sociedad de Psiquiatría y Neurología de la Infancia y Adolescencia (SOPNIA). Comunicado Oficial. Declaración respecto Hospital Psiquiátrico Phillipe Pinel de Putaendo. Santiago; 2019.  Pesce C. Hospitalización psiquiátrica infanto-juvenil en Chile: reflexión en torno a su implementación, diagnóstico del estado actual y proyecciones futuras. Rev Chil Psiquiatr Neurol Infanc Adolesc. 2014;25(1):27–36.
Pesce C. Hospitalización psiquiátrica infanto-juvenil en Chile: reflexión en torno a su implementación, diagnóstico del estado actual y proyecciones futuras. Rev Chil Psiquiatr Neurol Infanc Adolesc. 2014;25(1):27–36.  Ministerios de Salud de Chile. Modelo de Gestión. Red Temática de Salud Mental en la Red General de Salud. Santiago; 2018. [Internet] | Link |
Ministerios de Salud de Chile. Modelo de Gestión. Red Temática de Salud Mental en la Red General de Salud. Santiago; 2018. [Internet] | Link | de la Barra F, García R. Hospitalización psiquiátrica de niños y adolescentes I: revisión de la literatura. Rev Chil Neuro-Psiquiatr. 2009;47(3):228–37. | CrossRef |
de la Barra F, García R. Hospitalización psiquiátrica de niños y adolescentes I: revisión de la literatura. Rev Chil Neuro-Psiquiatr. 2009;47(3):228–37. | CrossRef | Minoletti A, Zaccaria A. Plan Nacional de Salud Mental en Chile: 10 años de experiencia. Rev Panam Salud Publica. 2005;18(4):346–58. [Internet] | Link |
Minoletti A, Zaccaria A. Plan Nacional de Salud Mental en Chile: 10 años de experiencia. Rev Panam Salud Publica. 2005;18(4):346–58. [Internet] | Link | Pacheco P B, Lizana C P, Celhay S I, Pereira Q J. [Clinical characteristics of children and adolescent hospitalized in a university psychiatric clinic]. Rev Med Chil. 2007 Jun;135(6):751-8. | CrossRef | PubMed |
Pacheco P B, Lizana C P, Celhay S I, Pereira Q J. [Clinical characteristics of children and adolescent hospitalized in a university psychiatric clinic]. Rev Med Chil. 2007 Jun;135(6):751-8. | CrossRef | PubMed | Pacheco B, Lizana P, Celhay I. [Clinical differences between suicide and non suicide attempter hospitalized adolescents]. Rev Med Chil. 2010 Feb;138(2):160-7. | CrossRef | PubMed |
Pacheco B, Lizana P, Celhay I. [Clinical differences between suicide and non suicide attempter hospitalized adolescents]. Rev Med Chil. 2010 Feb;138(2):160-7. | CrossRef | PubMed | Díaz J. Manual de Organización Unidad de Corta Estadía Infanto-juvenil Hospital Psiquiátrico del Salvador, Valparaíso; 2014.
Díaz J. Manual de Organización Unidad de Corta Estadía Infanto-juvenil Hospital Psiquiátrico del Salvador, Valparaíso; 2014.  Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington; 2013. | CrossRef |
Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington; 2013. | CrossRef | Beraudi A, Asociación Franco-Argentina de Psiquiatría y Salud Mental. Clasificación Francesa de los Trastornos Mentales del Niño y del Adolescente. Buenos Aires: Polemos; 2004.
Beraudi A, Asociación Franco-Argentina de Psiquiatría y Salud Mental. Clasificación Francesa de los Trastornos Mentales del Niño y del Adolescente. Buenos Aires: Polemos; 2004.  Bowlby J. Attachment theory, separation anxiety and mourning.American Handbook of Psychiatry. 2nd Ed. New York. 1975.
Bowlby J. Attachment theory, separation anxiety and mourning.American Handbook of Psychiatry. 2nd Ed. New York. 1975.  Winnicott D. Playing and reality. Tavistock Publications. 1st Ed. London. 1971.
Winnicott D. Playing and reality. Tavistock Publications. 1st Ed. London. 1971.  Bronfenbrenner U. The ecology of human development. Harvard University Press. Cambridge;1979.
Bronfenbrenner U. The ecology of human development. Harvard University Press. Cambridge;1979.  Márquez-Caraveo ME, Arroyo-García E, Granados-Rojas A, Ángeles-Llerenas A. [Children's Psychiatric Hospital Dr. Juan N. Navarro: 50 years of attention to the mental health of children and adolescents in Mexico]. Salud Publica Mex. 2017 Jul-Aug;59(4):477-484. | CrossRef | PubMed |
Márquez-Caraveo ME, Arroyo-García E, Granados-Rojas A, Ángeles-Llerenas A. [Children's Psychiatric Hospital Dr. Juan N. Navarro: 50 years of attention to the mental health of children and adolescents in Mexico]. Salud Publica Mex. 2017 Jul-Aug;59(4):477-484. | CrossRef | PubMed | Pfeiffer SI, Strzelecki SC. Inpatient psychiatric treatment of children and adolescents: a review of outcome studies. J Am Acad Child Adolesc Psychiatry. 1990 Nov;29(6):847-53. | CrossRef | PubMed |
Pfeiffer SI, Strzelecki SC. Inpatient psychiatric treatment of children and adolescents: a review of outcome studies. J Am Acad Child Adolesc Psychiatry. 1990 Nov;29(6):847-53. | CrossRef | PubMed | Bardach NS, Coker TR, Zima BT, Murphy JM, Knapp P, Richardson LP, Edwall G, Mangione-Smith R. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014 Apr;133(4):602-9. | CrossRef | PubMed |
Bardach NS, Coker TR, Zima BT, Murphy JM, Knapp P, Richardson LP, Edwall G, Mangione-Smith R. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014 Apr;133(4):602-9. | CrossRef | PubMed | Duarte V, Zelaya L. Caracterización clínica y demográfica de la hospitalización psiquiátrica infanto-juvenil en un hospital general. Pediatr. 2019;46(2):90–6. | CrossRef |
Duarte V, Zelaya L. Caracterización clínica y demográfica de la hospitalización psiquiátrica infanto-juvenil en un hospital general. Pediatr. 2019;46(2):90–6. | CrossRef | Masters GA, Baldessarini RJ, Öngür D, Centorrino F. Factors associated with length of psychiatric hospitalization. Compr Psychiatry. 2014 Apr;55(3):681-7. | CrossRef | PubMed |
Masters GA, Baldessarini RJ, Öngür D, Centorrino F. Factors associated with length of psychiatric hospitalization. Compr Psychiatry. 2014 Apr;55(3):681-7. | CrossRef | PubMed | Gold J, Shera D, Clarkson B Jr. Private psychiatric hospitalization of children: predictors of length of stay. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):135-43. | CrossRef | PubMed |
Gold J, Shera D, Clarkson B Jr. Private psychiatric hospitalization of children: predictors of length of stay. J Am Acad Child Adolesc Psychiatry. 1993 Jan;32(1):135-43. | CrossRef | PubMed | Hanssen-Bauer K, Heyerdahl S, Hatling T, Jensen G, Olstad PM, Stangeland T, et al. Admissions to acute adolescent psychiatric units: a prospective study of clinical severity and outcome. Int J Ment Health Syst. 2011 Jan 6;5(1):1. | CrossRef | PubMed |
Hanssen-Bauer K, Heyerdahl S, Hatling T, Jensen G, Olstad PM, Stangeland T, et al. Admissions to acute adolescent psychiatric units: a prospective study of clinical severity and outcome. Int J Ment Health Syst. 2011 Jan 6;5(1):1. | CrossRef | PubMed | Pupo-González L, Nogueras-Reyes Y, de Prada-Justel ME, Labrada-Pupo D. Salud mental infanto juvenil, características de una problemática actual. Rev Electrónica Dr Zoilo E Mar Vidaurreta. 2018;43(6). [Internet] | Link |
Pupo-González L, Nogueras-Reyes Y, de Prada-Justel ME, Labrada-Pupo D. Salud mental infanto juvenil, características de una problemática actual. Rev Electrónica Dr Zoilo E Mar Vidaurreta. 2018;43(6). [Internet] | Link | Kernberg P, Chazan S. Niños con desórdenes de conducta. Manual de psicoterapia. Santiago: Mediterráneo. 2018. 1;18–19.
Kernberg P, Chazan S. Niños con desórdenes de conducta. Manual de psicoterapia. Santiago: Mediterráneo. 2018. 1;18–19.  Bradley R, Zittel Conklin C, Westen D. The borderline personality diagnosis in adolescents: gender differences and subtypes. J Child Psychol Psychiatry. 2005 Sep;46(9):1006-19. | CrossRef | PubMed |
Bradley R, Zittel Conklin C, Westen D. The borderline personality diagnosis in adolescents: gender differences and subtypes. J Child Psychol Psychiatry. 2005 Sep;46(9):1006-19. | CrossRef | PubMed | Glenn CR, Klonsky ED. Reliability and validity of borderline personality disorder in hospitalized adolescents. J Can Acad Child Adolesc Psychiatry. 2013 Aug;22(3):206-11. | PubMed |
Glenn CR, Klonsky ED. Reliability and validity of borderline personality disorder in hospitalized adolescents. J Can Acad Child Adolesc Psychiatry. 2013 Aug;22(3):206-11. | PubMed | Stepp SD, Pilkonis PA, Hipwell AE, Loeber R, Stouthamer-Loeber M. Stability of borderline personality disorder features in girls. J Pers Disord. 2010 Aug;24(4):460-72. | CrossRef | PubMed |
Stepp SD, Pilkonis PA, Hipwell AE, Loeber R, Stouthamer-Loeber M. Stability of borderline personality disorder features in girls. J Pers Disord. 2010 Aug;24(4):460-72. | CrossRef | PubMed | Sourander A, Piha J. Three-year follow-up of child psychiatric inpatient treatment. Eur Child Adolesc Psychiatry. 1998 Sep;7(3):153-62. | CrossRef | PubMed |
Sourander A, Piha J. Three-year follow-up of child psychiatric inpatient treatment. Eur Child Adolesc Psychiatry. 1998 Sep;7(3):153-62. | CrossRef | PubMed | Saldaña SN, Keeshin BR, Wehry AM, Blom TJ, Sorter MT, DelBello MP, Strawn JR. Antipsychotic polypharmacy in children and adolescents at discharge from psychiatric hospitalization. Pharmacotherapy. 2014 Aug;34(8):836-44. | CrossRef | PubMed |
Saldaña SN, Keeshin BR, Wehry AM, Blom TJ, Sorter MT, DelBello MP, Strawn JR. Antipsychotic polypharmacy in children and adolescents at discharge from psychiatric hospitalization. Pharmacotherapy. 2014 Aug;34(8):836-44. | CrossRef | PubMed | Staton D. Achieving adolescent adherence to treatment of major depression. Adolesc Health Med Ther. 2010 Aug 4;1:73-85. | CrossRef | PubMed |
Staton D. Achieving adolescent adherence to treatment of major depression. Adolesc Health Med Ther. 2010 Aug 4;1:73-85. | CrossRef | PubMed | Joyce VW, King CD, Nash CC, Lebois LAM, Ressler KJ, Buonopane RJ. Predicting Psychiatric Rehospitalization in Adolescents. Adm Policy Ment Health. 2019 Nov;46(6):807-820. | CrossRef | PubMed |
Joyce VW, King CD, Nash CC, Lebois LAM, Ressler KJ, Buonopane RJ. Predicting Psychiatric Rehospitalization in Adolescents. Adm Policy Ment Health. 2019 Nov;46(6):807-820. | CrossRef | PubMed | Bobier C, Warwick M. Factors associated with readmission to adolescent psychiatric care. Aust N Z J Psychiatry. 2005 Jul;39(7):600-6. | CrossRef | PubMed |
Bobier C, Warwick M. Factors associated with readmission to adolescent psychiatric care. Aust N Z J Psychiatry. 2005 Jul;39(7):600-6. | CrossRef | PubMed | American Psychiatric Association. APA Official Actions. Position Statement on Psychiatric Hospitalization of Children and Adolescents. Washignton. 2016.
American Psychiatric Association. APA Official Actions. Position Statement on Psychiatric Hospitalization of Children and Adolescents. Washignton. 2016. Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








