Key Words: diabetes mellitus type 2, adolescent, young adult, prevalence, peru
Abstract
Introduction
Type 2 diabetes mellitus is a health problem in low and middle-income countries like Peru. There are few published reports on trends and surveillance of this disease in the young Peruvian population.
Objective
To describe the prevalence of type 2 diabetes mellitus in the population under 30 registered between 2005 and 2018 by the Ministry of Health of Peru.
Methods
A descriptive study was conducted from a secondary analysis of the national registries of type 2 diabetes (ICD 10: E11) in the population under 30 treated in the health facilities of the Ministry of Health of Peru between 2015 and 2018. Described by department and geographic region, the prevalence of diabetes was adjusted for age and sex.
Results
In the period between 2005 and 2018, the national prevalence of type 2 diabetes mellitus increased from 2.1 to 22.1 cases/100 000 population. Women had a higher prevalence. Geographic regions with the highest prevalence increase were the Coast from 3.8 to 35.3/100 000 population and the Rainforest from 1.1 to 22.1/100 000 population. In the same period, the departments with the highest prevalence increase were Cajamarca (1733.3%) and Puno (1704.2%). Furthermore, Tumbes, Ica, Lambayeque, Callao, Lima, Loreto, and Madre de Dios reported prevalence rates over the national average.
Conclusions
The prevalence of type 2 diabetes mellitus in the population under 30 and covered by the Peruvian Ministry of Health has increased more than ten times in the period between 2005 and 2018. The Coast and the cities with the highest population density had the highest prevalence. A greater focus to improve the strategies of risk factor control in the population under 30 is needed, including preventive actions on obesity and inadequate lifestyles, as well as a screening at a younger age for diabetes in the population at risk.
|
Key ideas
|
Introduction
Type 2 diabetes mellitus is a global health problem with a high burden of morbidity and mortality[1]. Although it is a noncommunicable chronic disease, it causes a deterioration in health-related quality of life, has economic costs for those living with the disease and increases expenses at health care centers[2]. Although type 2 diabetes mellitus has traditionally been considered a disease of the older adult population[3], several studies have reported an increase in the prevalence and incidence in other populations, including children, adolescents, and young adults[4],[5],[6], where the disease rates are even higher in these population groups than type 1 diabetes mellitus[6],[7].
The development of type 2 diabetes mellitus is strongly associated with genetic, social, environmental, and behavioral factors. For example, a sedentary lifestyle and unhealthy eating habits can lead to the development of preventable risk factors for the disease such as overweight, child obesity, and hypertension[8],[9],[10].
In several countries, epidemiologic surveillance systems do not continuously monitor noncommunicable diseases such as type 2 diabetes mellitus[5]. In Peru, it was not until 2014 that the Ministry of Health (MINSA) National Center for Disease Control and Prevention (CDC–Peru) implemented an epidemiologic surveillance system for type 2 diabetes mellitus[11].
MINSA facilities provide health services to the vast majority of Peru’s population. According to data collected in the National Population and Housing Census for 2017, of the population that received medical care at MINSA health facilities, 44.4% were covered by Peru´s Comprehensive Health Insurance (Seguro Integral de Salud, SIS), and 25.6% were uninsured[12] (in Peru, the uninsured can receive medical services at either MINSA or private health facilities). Other types of health insurance covered a third, smaller group receiving treatment at MINSA health facilities. Altogether, the patient groups receiving care at MINSA health facilities represent about 70% of the total population of Peru[12],[13], with the remainder covered by Social Security Health Insurance (EsSalud), the private sector, the Armed Forces, and the Police.
In Peru, type 2 diabetes mellitus affects about 7% of the general population[13], mainly adults over 30 years old, who often develop complications associated with the disease that increase mortality[14]. Recently, however, risk factors for developing diabetes have become more frequent in younger populations, and complications associated with the disease are occurring at earlier phases[15]. Cases of the disease in children, adolescents, and young adults have been reported by Peru’s type 2 diabetes mellitus surveillance system[10] and in some case report series[16]. Despite the increased incidence in younger people, the prevalence of type 2 diabetes mellitus in the population under 30 years old is still mostly unknown, because most studies only describe the prevalence of this disease in the older population (people over 25 or 30 years old)[17],[18],[19]. Therefore, this study aimed to describe the trend toward the development of type 2 diabetes mellitus in younger populations (under 30 years old) using data from MINSA health registries for the period 2015 to 2018.
Methods
Design
We carried out a descriptive, observational study analyzing type 2 diabetes mellitus in the population under 30 years old treated at MINSA health facilities during the period 2015 to 2018. We used secondary-source and free-access institutional data for this population group obtained from MINSA health registries.
Setting
The study included health data for the entire country, analyzing prevalence by Peru’s three geographic regions (Coast, Highlands, and Jungle) and 25 administrative departments.
Variables
The outcome variable was the prevalence rate for type 2 diabetes mellitus in the population under 30 years old treated at MINSA health facilities (i.e., for the purposes of this study, the population covered by EsSalud, or uninsured), based on the number of cases per year reported to MINSA medical registries for all years of the study period (2005 to 2018) by geographic region. Prevalence was analyzed by geographic region, as well as administrative department, and sex (when data for the latter two categories were included in the MINSA health records). All cases of type 2 diabetes mellitus diagnosed at age under 30 were included as registered in the 25 administrative regions of Peru.
The prevalence rate was calculated for each region, department and year, expressed for every 100 000 inhabitants. The population covered by Peru´s Comprehensive Health Insurance or uninsured was estimated for each year based on the National Household Survey of Peru (http://iinei.inei.gob.pe/microdatos/). Prevalence was adjusted for age and sex using the reference population estimated by the World Health Organization for 2000 to 2025, direct method[20].
Procedures
Data from national registries for type 2 (non-insulin dependent) diabetes mellitus (ICD-10 code E11) were requested through MINSA’s Platform for Access to Public Information (http://www.Ministerio de Salud.gob.pe/portada/transparencia/solicitud/frmFormulario.asp).
The database used in the study was designed and compiled by the General Office of Technologies of MINSA, which collects information on type 2 diabetes mellitus for sex, department, and age group variables obtained from registries of type 2 diabetes mellitus diagnosed at MINSA outpatient health facilities and Regional Health Directorates. The diagnoses are based on MINSA clinical practice guidelines for diagnosis, treatment, and control of type 2 diabetes mellitus[21].
Data analysis
Data management, preparation, and analysis were carried out using Microsoft Excel Software 2013 for Windows. The first phase of the study identified and compiled all type 2 diabetes mellitus cases reported by MINSA medical facilities. The case records included information on case frequency, geographic region, administrative department, and sex. No miscategorized records (from other regions) were found in the registries, so all 35 160 cases were included in the sample.
In the second stage of the study, prevalence rates were calculated by region and department for two sub-periods of the study (2005 to 2011 and 2012 to 2018) to determine percentage changes over time, as done in previous studies[22],[23]. Prevalence rates for these two periods were compared by sex (Figure 1) and geographic distribution (Figure 2), using the application QGIS v 2.10.1 (OSGeo, Beaverton, OR, USA). In Figure 2, the prevalence rate by department was divided into quintiles, following a similar methodology used in previous studies[14],[24].
Ethics
This study analyzed secondary, publicly available, de-identified data and thus did not require clinical study ethics approval.
Results
From 2005 to 2018, 35 160 cases of type 2 diabetes mellitus were reported for the population under 30 years old treated at MINSA health facilities. The number of reported cases per year increased from 530 in 2005 to 5154 in 2018. There were more cases in women than men, each year of the study, cases in women increased from 347 in 2005, to 3424 in 2018. The number of type 2 diabetes mellitus cases reported by MINSA health facilities for the under-30 age group increased in all three geographic regions from 2005 to 2018 (from 402 to 3611 cases in the Coast, 108 to 911 cases in the Highlands, and 20 to 632 cases in the Jungle).
Between 2005 and 2018, the prevalence rate increased more than tenfold (from 2.1 to 22.1 cases per 100 000 inhabitants). Prevalence was higher for women every year of the study, increasing from 5.3 cases/100 000 in 2005 to 58.0 cases/100 000 in 2018 (Figure 1).
The geographic region with the highest absolute increase in prevalence was the Coast (from 3.8 cases/100 000 to 35.3 cases/100 000), followed by the Jungle (from 1.1 cases/100 000 to 21.6 cases/100 000) (Figure 2). Coastal departments with the highest increase in prevalence were Tumbes (1594.0%) and Lambayeque (830.7%).
In the Jungle, the departments with the highest increase in prevalence were San Martin (1322.4%) and Loreto (990.2%). In the Highlands, the steepest increases were in Cajamarca (1733.3%) and Puno (1704.2%) (Table 1).
Departments with higher prevalence than the national average for 2018 (22.1/100 000), from highest to lowest, were Tumbes (80.4/100 000), Ica (59.1/100 000), Lambayeque (34.6/100 000), Callao (33.3/100 000), Lima (30.9/100 000), Loreto (26.4/100 000), and Madre de Dios (25.5/100 000) (Table 1 and Figure 3).
Discussion
The main findings of this study show a more than tenfold increase in the prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities from 2005 to 2018, with higher prevalence in women for each year of the study period. Geographic distribution of prevalence over the study period shows an increase in all regions and departments, with the Coast and the department of Lima reporting the highest prevalence increases.
This trend can be explained by various factors, including improvements in Peru’s disease registry systems at various primary health care facilities[25], and the increase in metabolic and chronic diseases in the infant and under-30 population in Peru[26]. These findings support those from previous studies that estimated a more than tenfold increase in the prevalence of type 2 diabetes mellitus over the past few decades[5]. This study highlights the epidemiologic transition that is taking place in middle-income countries like Peru[27]. Type 2 diabetes mellitus prevalence in these countries has reached the levels seen in some high-income countries with better surveillance systems for this disease, such as Canada, which reported a rate of 21 cases/100 000 in people under 20 years old in 2013[4], and the United States, which reported a rate of 24 cases/100 000 in the same age group in 2009[28].
Although obesity is one of the most important risk factors for type 2 diabetes mellitus, female sex, and polycystic ovary are also considered risk factors[8]. As has been reported previously, more women than men are treated at MINSA health care centers[29],[30], which could explain the higher type 2 diabetes mellitus prevalence found in this study for women versus men.
A higher prevalence of type 2 diabetes mellitus in the Coast may be explained by the higher population density of cities and better disease surveillance in this region. Another possible factor is the rate of internal migration to some departments in this region, particularly the most highly populated ones, such as Lima, which leads to increased urbanization and unhealthy behaviors and habits such as physical inactivity and consumption of a hypercaloric diet[26], both of which are more frequently reported in this region, especially at early stages of life[27], and are linked to various noncommunicable chronic diseases, including type 2 diabetes mellitus[27].
The number of studies on type 2 diabetes mellitus in patients under 30 years in Peru (nationally and by region) is insufficient, and the subject matter covered is limited to isolated case reports or case series[10],[16]. This study was designed to fill this gap by exploring and reporting epidemiologic information related to trends in prevalence in type 2 diabetes mellitus in the under-30 age group at the national, regional, and departmental level, by analyzing national data by year for more than ten years in the large proportion of the national population that attends MINSA health care centers.
Based on the findings of our study, we recommend implementation of health intervention policies focused on prevention and control activities to address the risk factors for diabetes mellitus, such as obesity in children and adolescents, because, at present, definitive diagnosis of this disease can be difficult due to its slow and asymptomatic onset[9],[31]. Early control is essential for limiting the micro- and macro-vascular lesions that may appear in type 2 diabetes mellitus patients over the long term[32],[33], and reducing the development of comorbidities and complications associated with the disease[34], which can lead to increased mortality in older patients[14].
This study has limitations. First, the data were obtained from a secondary database with potential problems in the quality of its sub-registries; however, the diagnoses of type 2 diabetes mellitus recorded in the registries are based on MINSA’s clinical practice guidelines for the disease, which reduces the potential for bias from false-positive cases. Second, screening for type 2 diabetes mellitus in Peru only includes people 18 years old or older[21], so cases in the population under these ages could have been undiagnosed. It is also possible that errors occurred in the recording and reporting of the registry information. Despite these potential limitations of the data source, we believe the under-reporting of type 2 diabetes mellitus cases in the MINSA registries is minimal due to the follow-up and internal review of cases in the health care networks of each department.
Furthermore, the sole source of the study data was MINSA health registries, so information on patients with type 2 diabetes mellitus who received medical care at other (non-MINSA) health facilities (e.g., those covered by EsSalud, the private sector, the Armed Forces, or the Police) was not included in the study. Therefore, the number of patients under 30 years old in Peru with type 2 diabetes mellitus may be greater than reported here. However, the vast majority of the population in Peru 18 to 30 years old are not covered by EsSalud or the other sources of insurance mentioned above; only a small percentage of this age group receives it through their employment (and coverage through parents expires at age 18). Therefore, most members of this age group are treated at MINSA health facilities so they would be included in this study.
The trend toward increased prevalence of type 2 diabetes mellitus in the population covered in our study can be partly explained by the progressive increase in the number of people covered by Peru's Comprehensive Health Insurance (SIS), which has grown at the national level from 19.4% in 2006 to 50.2 % in 2015[35]. Other possible factors in the increased case frequency in this age group are the preventive, promotional, and screening activities that have been carried out in patients 18 years old or older[21]; if so, prevalence rates in other (non-MINSA) health systems would also be affected.
Conclusions
In recent years, cases of type 2 diabetes mellitus in the population under 30 years old treated at health care centers of the Ministry of Health of Peru has increased. Increased prevalence was highest in the Coast region and departments with high population density. These results encourage us to develop strategies for the early detection of risk factors in the young Peruvian population, especially in geographic areas where high prevalence has been identified.
Notes
Roles and authorship contributions
MSCR and NAA: conceptualization, management of data, formal analysis, research, methodology, project management, supervision, presentation of data, development of the draft, writing (reviewing and editing). IMA and ABCE: conceptualization, management of data, research, development of the draft, writing (reviewing and editing). EARA and CJPV: research, project management, writing (reviewing and editing).
Competing interests
The authors have completed the ICMJE conflict of interest declaration form and declare that they have not received any funding to conduct this report, do not have financial relations with organizations that might have interests in the published article during the last three years, and do not have any other relationships or carry out other activities that could have an influence on the published article. The forms can be requested by contacting the corresponding author or the Journal Editorial Board.
Funding
The authors declare that there were no external sources of funding.
Ethics
This study analyzed secondary data obtained from publicly available information from the Ministry of Health of Peru and thus did not require approval by an institutional ethics committee.
From the editors
The original version of this article was submitted in Spanish. The translated version published in English has been copyedited by the Journal.

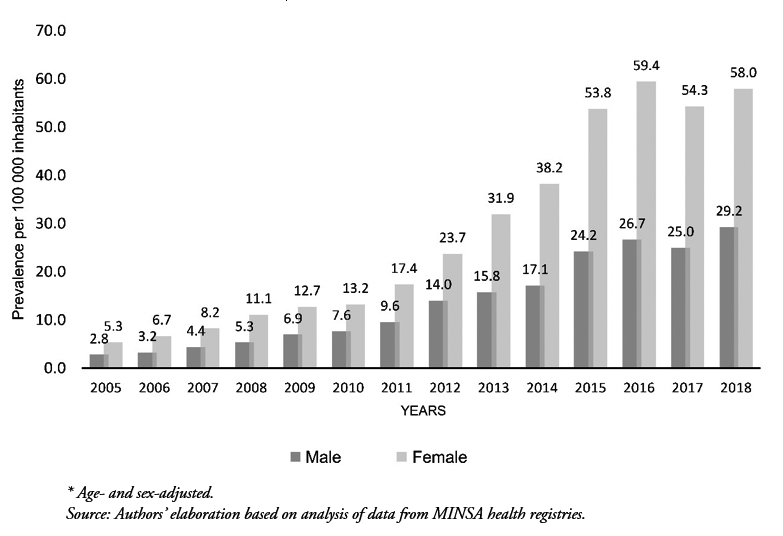 Figure 1. Prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by sex: 2005–2018. *
Figure 1. Prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by sex: 2005–2018. *

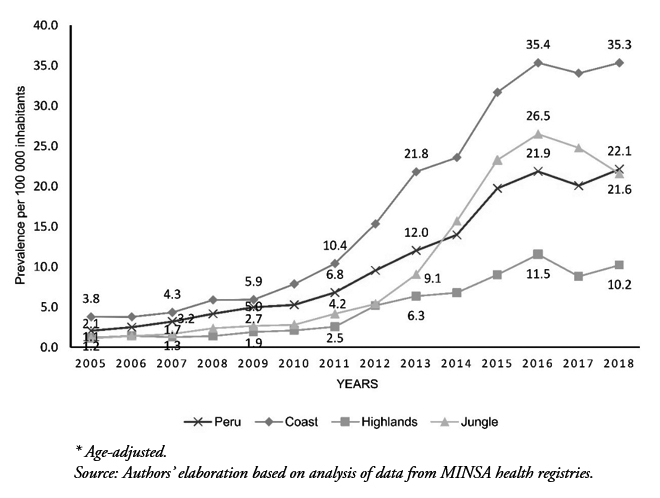 Figure 2. Prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by geographic region: 2005–2018.*
Figure 2. Prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by geographic region: 2005–2018.*

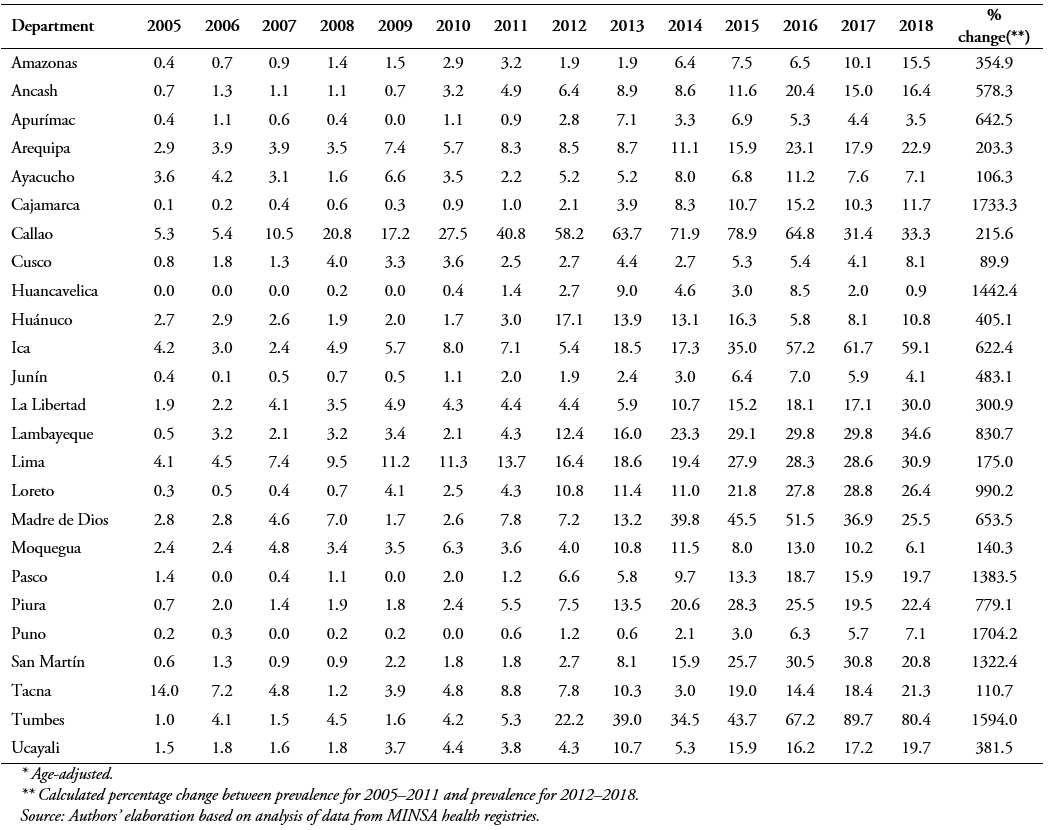 Table 1. Prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by department: 2005–2018.*
Table 1. Prevalence of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by department: 2005–2018.*

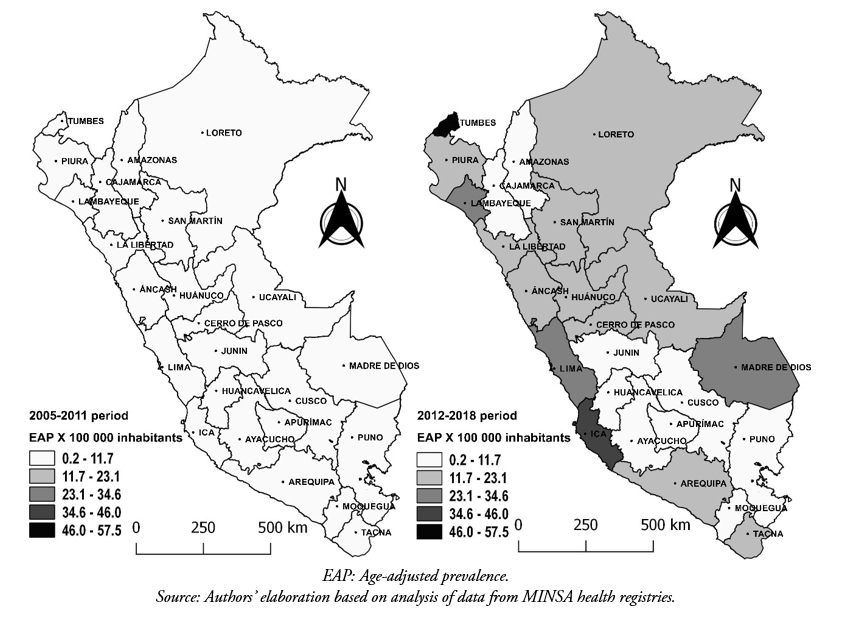 Figure 3. Distribution of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by department: 2005–2011 vs. 2012–2018.
Figure 3. Distribution of type 2 diabetes mellitus in the under-30 population treated at MINSA health facilities by department: 2005–2011 vs. 2012–2018.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introducción
La diabetes mellitus tipo 2 es un problema de salud en países de bajo y medianos ingresos como Perú. Existen escasos reportes publicados sobre el comportamiento de esta enfermedad en población peruana joven.
Objetivo
Describir la prevalencia de diabetes mellitus tipo 2 en la población menor de 30 años registrado en el Ministerio de Salud de Perú en el periodo 2005 a 2018.
Métodos
Se realizó un estudio observacional descriptivo. Se analizaron los registros nacionales de diabetes mellitus tipo 2 (código CIE 10: E11) en la población menor de 30 años, atendidos en establecimientos de salud del Ministerio de Salud de Perú entre los años 2005 y 2018. La prevalencia se reportó ajustada por edad y sexo, describiéndose por departamento y región geográfica.
Resultados
En el periodo 2005 a 2018, la prevalencia nacional de diabetes mellitus tipo 2 se incrementó de 2,1 a 22,1 casos por cada 100 000 habitantes; siendo el sexo femenino el de mayor prevalencia. Las regiones geográficas con mayor aumento de prevalencia fueron Costa de 3,8 a 35,3 por cada100 000 habitantes y Selva de 1,1 a 22,1 por cada 100 000 habitantes. Los departamentos con mayor incremento en la prevalencia fueron Cajamarca (1733,3%) y Puno (1704,2%); observándose departamentos como Tumbes, Ica, Lambayeque, Callao, Lima, Loreto y Madre de Dios con prevalencias mayores al promedio nacional.
Conclusiones
La prevalencia por diabetes mellitus tipo 2 en población menor de 30 años atendida en el Ministerio de Salud de Perú se ha incrementado en más de 10 veces durante el periodo 2005 a 2018. La región Costa y las ciudades con mayor densidad poblacional tuvieron mayor prevalencia. Se necesita enfocar y mejorar las estrategias de control de los factores de riesgo en la población juvenil como la obesidad e inadecuados estilos de vida y un tamizaje a menor edad en la población de riesgo.
 Autores:
Maycol Suker Ccorahua-Ríos[1], Noé Atamari-Anahui [2], Iveth Miranda-Abarca[1], Andy Bryan Campero-Espinoza[1], Evelina Andrea Rondón-Abuhadba[3], César Johan Pereira-Victorio[4]
Autores:
Maycol Suker Ccorahua-Ríos[1], Noé Atamari-Anahui [2], Iveth Miranda-Abarca[1], Andy Bryan Campero-Espinoza[1], Evelina Andrea Rondón-Abuhadba[3], César Johan Pereira-Victorio[4]
Affiliation:
[1] ASOCIEMH CUSCO, Escuela Profesional de Medicina Humana, Facultad de Ciencias de la Salud, Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú
[2] Universidad San Ignacio de Loyola, Vicerrectorado de Investigación, Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Lima, Perú
[3] Escuela Profesional de Medicina Humana, Facultad de Ciencias de la Salud, Universidad Nacional de San Antonio Abad del Cusco, Cusco, Perú
[4] Universidad Continental, Lima, Perú
E-mail: noe.atamari@gmail.com
Author address:
[1] Avenida La Fontana 550
La Molina
Lima, Perú

Citation: Ccorahua-Ríos MS, Atamari-Anahui N, Miranda-Abarca I, Campero-Espinoza AB, Rondón-Abuhadba EA, Pereira-Victorio CJ. Type 2 diabetes mellitus prevalence between 2005 and 2018 in population under 30 using data from the Ministry of Health of Peru . Medwave 2019;19(10):e7723 doi: 10.5867/medwave.2019.10.7723
Submission date: 18/8/2019
Acceptance date: 24/10/2019
Publication date: 13/11/2019
Origin: not commissioned
Type of review: reviewed by three external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- International Diabetes Federation. IDF Diabetes atlas. 8th ed. 2017 [on line]. | Link |
- Arredondo A, Azar A, Recamán AL. Diabetes, a global public health challenge with a high epidemiological and economic burden on health systems in Latin America. Glob Public Health. 2018 Jul;13(7):780-787. | CrossRef | PubMed |
- Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018 Apr;138:271-281. | CrossRef | PubMed |
- Amed S, Islam N, Sutherland J, Reimer K. Incidence and prevalence trends of youth-onset type 2 diabetes in a cohort of Canadian youth: 2002-2013. Pediatr Diabetes. 2018 Jun;19(4):630-636. | CrossRef | PubMed |
- Baron P, Márquez E. Diabetes mellitus tipo 2 en niños y adolescentes. Med Interna México. 2010;26(1):36-47. | Link |
- De Ferranti SD, Osganian SK. Epidemiology of paediatric metabolic syndrome and type 2 diabetes mellitus. Diab Vasc Dis Res. 2007 Dec;4(4):285-96. | PubMed |
- Licea ME, Bustamante M, Lemane M. Diabetes tipo 2 en niños y adolescentes : aspectos clínico-epidemiológicos, patogénicos y terapéuticos. Rev Cuba Endocrinol. 2008;19(1). | Link |
- Kaufman FR. Type 2 diabetes in children and youth. Endocrinol Metab Clin North Am. 2005 Sep;34(3):659-76, ix-x. | PubMed |
- Calero Bernal ML, Varela Aguilar JM. Infant-juvenile type 2 diabetes. Rev Clin Esp. 2018 Oct;218(7):372-381. | CrossRef | PubMed |
- Pinto M, Seclén S, Cabello E. Diabetes tipo 2 en niños. Reporte de caso. Rev Medica Hered. 2016;21(2):103-6. | Link |
- Ministerio de Salud del Perú. Resolución Ministerial N°961. Lima: MINSA; 2014:21. | Link |
- Instituto Nacional de Estadística e Informática. Población afiliada a algún seguro de Salud. Lima: INEI; 2018:36. | Link |
- Villena JE. Diabetes Mellitus in Peru. Ann Glob Health. 2015 Nov-Dec;81(6):765-75. | CrossRef | PubMed |
- Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005-2014. Rev Panam Salud Publica. 2018;42(e50):1-7. | CrossRef |
- Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018 Jan;6(1):69-80. | CrossRef | PubMed |
- Manrique-Hurtado H, Aro-Guardia P, Pinto-Valdivia M. Diabetes tipo 2 en niños. Serie de casos. Rev Medica Hered. 2016;26(1):5. | Link |
- Carrillo-Larco RM, Bernabé-Ortiz A. [Type 2 diabetes mellitus in peru: a systematic review of prevalence and incidence in the general population]. Rev Peru Med Exp Salud Publica. 2019 Jan-Mar;36(1):26-36. | CrossRef | PubMed |
- Ruiz-Alejos A, Carrillo-Larco RM, Miranda JJ, Anderson CAM, Gilman RH, Smeeth L, et al. Addressing the impact of urban exposure on the incidence of type 2 diabetes mellitus: The PERU MIGRANT Study. Sci Rep. 2018 Apr 3;8(1):5512. | CrossRef | PubMed |
- Seclen SN, Rosas ME, Arias AJ, Medina CA. Elevated incidence rates of diabetes in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2017 Jul 19;5(1):e000401. | CrossRef | PubMed |
- Ahmad O, Boschi-Pinto C, Lopez A, Murray C, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva Switzerland: WHO; 2000:14.
- Ministerio de Salud del Perú. Guía de Práctica Clínica para el Diagnóstico, Tratamiento y Control de la Diabetes Mellitus Tipo 2 en el Primer Nivel de Atención. 1ra ed. Dirección de Prevención de Enfermedades No Transmisibles y Oncológicas, editor. Lima: MINSA;2016:10-66. | Link |
- Herrera-Añazco P, Atamari-Anahui N, Flores-Benites V. Numero de nefrólogos, servicios de hemodiálsis y tendencia de la prevalencia de enfermedad renal cronica en el Minisiterio de Salud de Perú. Rev Peru Med Exp Salud Publica. 2019;36(1):62-7. | CrossRef |
- Atamari-Anahui N, Ccorahua-Rios MS, Condori-Huaraka M, Huamanvilca-Yepez Y, Amaya E, Herrera-Añazco P. Epidemiology of chronic kidney disease in Peru and its relation to social determinants of health. Int Health. 2019 Oct 31. pii: ihz071. | CrossRef | PubMed |
- Atamari-Anahui N, Alva-Díaz C, Vera-Monge V, Taype-Rondan A. Tendencia de mortalidad por enfermedad cerebrovascular registrada por el Ministerio de Salud de Perú, 2005-2015. Neurol Arg. 2019. | CrossRef |
- Curioso WH. [eHealth in Peru: implementation of policies to strengthen health information systems]. Rev Panam Salud Publica. 2014 May-Jun;35(5-6):437-41. | PubMed |
- Del Aguila Villar CM. Obesidad en el niño: factores de riesgo y estrategias para su prevención en Perú. Rev Peru Med Exp Salud Pública. 2018;34(1):113. | CrossRef |
- Miranda JJ, Wells JC, Smeeth L. [Transitions in context: findings related to rural-to-urban migration and chronic non-communicable diseases in Peru]. Rev Peru Med Exp Salud Publica. 2012 Jul-Sep;29(3):366-72. | PubMed |
- Pettitt DJ, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence JM, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014 Feb;37(2):402-8. | CrossRef | PubMed |
- Instituto Nacional de Estadística e Informática. Usuarios de consulta externa de los establecimientos de salud. Inst Nac Estad E Informática. 2014;1:23-62. | Link |
- Curioso WH, Pardo K, Valeriano L. [Use of health facilities of the Ministry of Health of Peru, 2009-2011]. Rev Peru Med Exp Salud Publica. 2013 Apr;30(2):175-80. | PubMed |
- Calagua-Quispe M, Falen-Boggio J, del Águila-Villar C, Lu-de Lama R, Rojas-Gabulli M. Características clínicas y bioquímicas de la diabetes mellitus tipo 2 ( DMt2 ) en el Instituto Nacional de Salud del Niño. Fac Med. 2012;73(2):141-6. | Link |
- Mejia CR, Paucar-Tito L, Morales-Concha L, Atamari-Anahui N, Rondón-Abuhadba EA, Ordoñez-Linares ME. Association between hospitalization stay and diabetic foot: an analytical cross-sectional study in three Peruvian hospitals. Medwave. 2018;18(7):e7336. | CrossRef |
- Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave. 2017 Dec 5;17(9):e7097. | CrossRef | PubMed |
- Pinhas-Hamiel O, Zeitler P. Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet. 2007 May 26;369(9575):1823-1831. | CrossRef | PubMed |
- Gutiérrez C, Romaní Romaní F, Wong P, Del Carmen Sara J. Brecha entre cobertura poblacional y prestacional en salud: un reto para la reforma de salud en el Perú. An Fac Med. 2018;79(1):65. | CrossRef |
 Arredondo A, Azar A, Recamán AL. Diabetes, a global public health challenge with a high epidemiological and economic burden on health systems in Latin America. Glob Public Health. 2018 Jul;13(7):780-787. | CrossRef | PubMed |
Arredondo A, Azar A, Recamán AL. Diabetes, a global public health challenge with a high epidemiological and economic burden on health systems in Latin America. Glob Public Health. 2018 Jul;13(7):780-787. | CrossRef | PubMed | Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018 Apr;138:271-281. | CrossRef | PubMed |
Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, et al. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018 Apr;138:271-281. | CrossRef | PubMed | Amed S, Islam N, Sutherland J, Reimer K. Incidence and prevalence trends of youth-onset type 2 diabetes in a cohort of Canadian youth: 2002-2013. Pediatr Diabetes. 2018 Jun;19(4):630-636. | CrossRef | PubMed |
Amed S, Islam N, Sutherland J, Reimer K. Incidence and prevalence trends of youth-onset type 2 diabetes in a cohort of Canadian youth: 2002-2013. Pediatr Diabetes. 2018 Jun;19(4):630-636. | CrossRef | PubMed | Baron P, Márquez E. Diabetes mellitus tipo 2 en niños y adolescentes. Med Interna México. 2010;26(1):36-47. | Link |
Baron P, Márquez E. Diabetes mellitus tipo 2 en niños y adolescentes. Med Interna México. 2010;26(1):36-47. | Link | De Ferranti SD, Osganian SK. Epidemiology of paediatric metabolic syndrome and type 2 diabetes mellitus. Diab Vasc Dis Res. 2007 Dec;4(4):285-96. | PubMed |
De Ferranti SD, Osganian SK. Epidemiology of paediatric metabolic syndrome and type 2 diabetes mellitus. Diab Vasc Dis Res. 2007 Dec;4(4):285-96. | PubMed | Licea ME, Bustamante M, Lemane M. Diabetes tipo 2 en niños y adolescentes : aspectos clínico-epidemiológicos, patogénicos y terapéuticos. Rev Cuba Endocrinol. 2008;19(1). | Link |
Licea ME, Bustamante M, Lemane M. Diabetes tipo 2 en niños y adolescentes : aspectos clínico-epidemiológicos, patogénicos y terapéuticos. Rev Cuba Endocrinol. 2008;19(1). | Link | Kaufman FR. Type 2 diabetes in children and youth. Endocrinol Metab Clin North Am. 2005 Sep;34(3):659-76, ix-x. | PubMed |
Kaufman FR. Type 2 diabetes in children and youth. Endocrinol Metab Clin North Am. 2005 Sep;34(3):659-76, ix-x. | PubMed | Calero Bernal ML, Varela Aguilar JM. Infant-juvenile type 2 diabetes. Rev Clin Esp. 2018 Oct;218(7):372-381. | CrossRef | PubMed |
Calero Bernal ML, Varela Aguilar JM. Infant-juvenile type 2 diabetes. Rev Clin Esp. 2018 Oct;218(7):372-381. | CrossRef | PubMed | Pinto M, Seclén S, Cabello E. Diabetes tipo 2 en niños. Reporte de caso. Rev Medica Hered. 2016;21(2):103-6. | Link |
Pinto M, Seclén S, Cabello E. Diabetes tipo 2 en niños. Reporte de caso. Rev Medica Hered. 2016;21(2):103-6. | Link | Instituto Nacional de Estadística e Informática. Población afiliada a algún seguro de Salud. Lima: INEI; 2018:36. | Link |
Instituto Nacional de Estadística e Informática. Población afiliada a algún seguro de Salud. Lima: INEI; 2018:36. | Link | Villena JE. Diabetes Mellitus in Peru. Ann Glob Health. 2015 Nov-Dec;81(6):765-75. | CrossRef | PubMed |
Villena JE. Diabetes Mellitus in Peru. Ann Glob Health. 2015 Nov-Dec;81(6):765-75. | CrossRef | PubMed | Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005-2014. Rev Panam Salud Publica. 2018;42(e50):1-7. | CrossRef |
Atamari-Anahui N, Ccorahua-Rios MS, Taype-Rondan A, Mejia CR. Mortalidad atribuida a diabetes mellitus registrada en el Ministerio de Salud de Perú, 2005-2014. Rev Panam Salud Publica. 2018;42(e50):1-7. | CrossRef | Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018 Jan;6(1):69-80. | CrossRef | PubMed |
Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018 Jan;6(1):69-80. | CrossRef | PubMed | Manrique-Hurtado H, Aro-Guardia P, Pinto-Valdivia M. Diabetes tipo 2 en niños. Serie de casos. Rev Medica Hered. 2016;26(1):5. | Link |
Manrique-Hurtado H, Aro-Guardia P, Pinto-Valdivia M. Diabetes tipo 2 en niños. Serie de casos. Rev Medica Hered. 2016;26(1):5. | Link | Carrillo-Larco RM, Bernabé-Ortiz A. [Type 2 diabetes mellitus in peru: a systematic review of prevalence and incidence in the general population]. Rev Peru Med Exp Salud Publica. 2019 Jan-Mar;36(1):26-36. | CrossRef | PubMed |
Carrillo-Larco RM, Bernabé-Ortiz A. [Type 2 diabetes mellitus in peru: a systematic review of prevalence and incidence in the general population]. Rev Peru Med Exp Salud Publica. 2019 Jan-Mar;36(1):26-36. | CrossRef | PubMed | Ruiz-Alejos A, Carrillo-Larco RM, Miranda JJ, Anderson CAM, Gilman RH, Smeeth L, et al. Addressing the impact of urban exposure on the incidence of type 2 diabetes mellitus: The PERU MIGRANT Study. Sci Rep. 2018 Apr 3;8(1):5512. | CrossRef | PubMed |
Ruiz-Alejos A, Carrillo-Larco RM, Miranda JJ, Anderson CAM, Gilman RH, Smeeth L, et al. Addressing the impact of urban exposure on the incidence of type 2 diabetes mellitus: The PERU MIGRANT Study. Sci Rep. 2018 Apr 3;8(1):5512. | CrossRef | PubMed | Seclen SN, Rosas ME, Arias AJ, Medina CA. Elevated incidence rates of diabetes in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2017 Jul 19;5(1):e000401. | CrossRef | PubMed |
Seclen SN, Rosas ME, Arias AJ, Medina CA. Elevated incidence rates of diabetes in Peru: report from PERUDIAB, a national urban population-based longitudinal study. BMJ Open Diabetes Res Care. 2017 Jul 19;5(1):e000401. | CrossRef | PubMed | Ahmad O, Boschi-Pinto C, Lopez A, Murray C, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva Switzerland: WHO; 2000:14.
Ahmad O, Boschi-Pinto C, Lopez A, Murray C, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva Switzerland: WHO; 2000:14.  Ministerio de Salud del Perú. Guía de Práctica Clínica para el Diagnóstico, Tratamiento y Control de la Diabetes Mellitus Tipo 2 en el Primer Nivel de Atención. 1ra ed. Dirección de Prevención de Enfermedades No Transmisibles y Oncológicas, editor. Lima: MINSA;2016:10-66. | Link |
Ministerio de Salud del Perú. Guía de Práctica Clínica para el Diagnóstico, Tratamiento y Control de la Diabetes Mellitus Tipo 2 en el Primer Nivel de Atención. 1ra ed. Dirección de Prevención de Enfermedades No Transmisibles y Oncológicas, editor. Lima: MINSA;2016:10-66. | Link | Herrera-Añazco P, Atamari-Anahui N, Flores-Benites V. Numero de nefrólogos, servicios de hemodiálsis y tendencia de la prevalencia de enfermedad renal cronica en el Minisiterio de Salud de Perú. Rev Peru Med Exp Salud Publica. 2019;36(1):62-7. | CrossRef |
Herrera-Añazco P, Atamari-Anahui N, Flores-Benites V. Numero de nefrólogos, servicios de hemodiálsis y tendencia de la prevalencia de enfermedad renal cronica en el Minisiterio de Salud de Perú. Rev Peru Med Exp Salud Publica. 2019;36(1):62-7. | CrossRef | Atamari-Anahui N, Ccorahua-Rios MS, Condori-Huaraka M, Huamanvilca-Yepez Y, Amaya E, Herrera-Añazco P. Epidemiology of chronic kidney disease in Peru and its relation to social determinants of health. Int Health. 2019 Oct 31. pii: ihz071. | CrossRef | PubMed |
Atamari-Anahui N, Ccorahua-Rios MS, Condori-Huaraka M, Huamanvilca-Yepez Y, Amaya E, Herrera-Añazco P. Epidemiology of chronic kidney disease in Peru and its relation to social determinants of health. Int Health. 2019 Oct 31. pii: ihz071. | CrossRef | PubMed | Atamari-Anahui N, Alva-Díaz C, Vera-Monge V, Taype-Rondan A. Tendencia de mortalidad por enfermedad cerebrovascular registrada por el Ministerio de Salud de Perú, 2005-2015. Neurol Arg. 2019. | CrossRef |
Atamari-Anahui N, Alva-Díaz C, Vera-Monge V, Taype-Rondan A. Tendencia de mortalidad por enfermedad cerebrovascular registrada por el Ministerio de Salud de Perú, 2005-2015. Neurol Arg. 2019. | CrossRef | Curioso WH. [eHealth in Peru: implementation of policies to strengthen health information systems]. Rev Panam Salud Publica. 2014 May-Jun;35(5-6):437-41. | PubMed |
Curioso WH. [eHealth in Peru: implementation of policies to strengthen health information systems]. Rev Panam Salud Publica. 2014 May-Jun;35(5-6):437-41. | PubMed | Del Aguila Villar CM. Obesidad en el niño: factores de riesgo y estrategias para su prevención en Perú. Rev Peru Med Exp Salud Pública. 2018;34(1):113. | CrossRef |
Del Aguila Villar CM. Obesidad en el niño: factores de riesgo y estrategias para su prevención en Perú. Rev Peru Med Exp Salud Pública. 2018;34(1):113. | CrossRef | Miranda JJ, Wells JC, Smeeth L. [Transitions in context: findings related to rural-to-urban migration and chronic non-communicable diseases in Peru]. Rev Peru Med Exp Salud Publica. 2012 Jul-Sep;29(3):366-72. | PubMed |
Miranda JJ, Wells JC, Smeeth L. [Transitions in context: findings related to rural-to-urban migration and chronic non-communicable diseases in Peru]. Rev Peru Med Exp Salud Publica. 2012 Jul-Sep;29(3):366-72. | PubMed | Pettitt DJ, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence JM, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014 Feb;37(2):402-8. | CrossRef | PubMed |
Pettitt DJ, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence JM, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014 Feb;37(2):402-8. | CrossRef | PubMed | Instituto Nacional de Estadística e Informática. Usuarios de consulta externa de los establecimientos de salud. Inst Nac Estad E Informática. 2014;1:23-62. | Link |
Instituto Nacional de Estadística e Informática. Usuarios de consulta externa de los establecimientos de salud. Inst Nac Estad E Informática. 2014;1:23-62. | Link | Curioso WH, Pardo K, Valeriano L. [Use of health facilities of the Ministry of Health of Peru, 2009-2011]. Rev Peru Med Exp Salud Publica. 2013 Apr;30(2):175-80. | PubMed |
Curioso WH, Pardo K, Valeriano L. [Use of health facilities of the Ministry of Health of Peru, 2009-2011]. Rev Peru Med Exp Salud Publica. 2013 Apr;30(2):175-80. | PubMed | Calagua-Quispe M, Falen-Boggio J, del Águila-Villar C, Lu-de Lama R, Rojas-Gabulli M. Características clínicas y bioquímicas de la diabetes mellitus tipo 2 ( DMt2 ) en el Instituto Nacional de Salud del Niño. Fac Med. 2012;73(2):141-6. | Link |
Calagua-Quispe M, Falen-Boggio J, del Águila-Villar C, Lu-de Lama R, Rojas-Gabulli M. Características clínicas y bioquímicas de la diabetes mellitus tipo 2 ( DMt2 ) en el Instituto Nacional de Salud del Niño. Fac Med. 2012;73(2):141-6. | Link | Mejia CR, Paucar-Tito L, Morales-Concha L, Atamari-Anahui N, Rondón-Abuhadba EA, Ordoñez-Linares ME. Association between hospitalization stay and diabetic foot: an analytical cross-sectional study in three Peruvian hospitals. Medwave. 2018;18(7):e7336. | CrossRef |
Mejia CR, Paucar-Tito L, Morales-Concha L, Atamari-Anahui N, Rondón-Abuhadba EA, Ordoñez-Linares ME. Association between hospitalization stay and diabetic foot: an analytical cross-sectional study in three Peruvian hospitals. Medwave. 2018;18(7):e7336. | CrossRef | Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave. 2017 Dec 5;17(9):e7097. | CrossRef | PubMed |
Atamari-Anahui N, Martinez-Ninanqui FW, Paucar-Tito L, Morales-Concha L, Miranda-Chirau A, Gamarra-Contreras MA, et al. Factors associated to inpatient mortality rates in type-2-diabetic patients: a cross-sectional analytical study in three Peruvian hospitals. Medwave. 2017 Dec 5;17(9):e7097. | CrossRef | PubMed | Pinhas-Hamiel O, Zeitler P. Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet. 2007 May 26;369(9575):1823-1831. | CrossRef | PubMed |
Pinhas-Hamiel O, Zeitler P. Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet. 2007 May 26;369(9575):1823-1831. | CrossRef | PubMed | Gutiérrez C, Romaní Romaní F, Wong P, Del Carmen Sara J. Brecha entre cobertura poblacional y prestacional en salud: un reto para la reforma de salud en el Perú. An Fac Med. 2018;79(1):65. | CrossRef |
Gutiérrez C, Romaní Romaní F, Wong P, Del Carmen Sara J. Brecha entre cobertura poblacional y prestacional en salud: un reto para la reforma de salud en el Perú. An Fac Med. 2018;79(1):65. | CrossRef |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








