Key Words: transcultural studies, measures, physical functioning, mobility limitation, critical care
Abstract
Background
The Functional Status Score for the Intensive Care Unit (FSS-ICU) is a valid and reliable instrument to measure physical functioning in the intensive care unit setting. Translation and cross-cultural adaptation in Chile has not been published for the FSS-ICU.
Aim
To translate and cross-culturally adapt all associated documents of the original FSS-ICU for Chile.
Method
The Spanish version of FSS-ICU, available at www.ImproveLTO.com, was used as the starting point. This version was previously translated, with the original FSS-ICU developers, following established guidelines for this process. The Chilean pocket card version was newly developed based on the English version at www.ImproveLTO.com. Cognitive interviews were conducted for the adaptation of the FSS-ICU and pocket card version to assess understanding of relevant stakeholders (i.e., Chilean intensive care unit physiotherapists). Adaptations to the translation were made when agreement among the physiotherapists was less than 80%.
Results
Cognitive interviews of the Chilean FSS-ICU (85 items) and pocket card version (18 items) were performed with 30 Chilean physiotherapists from 18 hospitals (14 public and 4 private). During the interviews, modest adaptations mainly made in the general guidelines and specific instructions for three items of the FSS-ICU and two items of the pocket card. Finally, the frequently asked questions, pocket card and full version of the FSS-ICU were developed. The original developers accepted all adaptations.
Conclusions
The Chilean version of the FSS-ICU was easy to understand by the physiotherapists. The FSS-ICU is freely available for non-commercial clinical and research use by Chilean Spanish-speakers.
Introduction
Advances in critical care medicine have contributed to the increased survival of critically ill patients[1]. Survivors commonly experience new or worsening impairments in their cognitive, mental and/or physical functioning after intensive care unit discharge[2],[3], known as Post Intensive Care Syndrome[2]. This syndrome is associated with higher healthcare costs and impaired quality of life[4],[5]. Evidence suggests that early physical therapy and exercise interventions in the intensive care unit is safe and can improve the strength and mobility status of survivors[6],[7],[8]. However, at present, there are important challenges in assessing physical functioning in the intensive care unit[9],[10],[11].
There is a growing interest in creating and adapting physical functioning measurement instruments for use in critically ill patients[10],[12]. The available evidence highlights many instruments designed for use in the intensive care unit[13],[14]. At present, four intensive care unit physical functioning measurement instruments are recommended based on their psychometric properties[10],[11]: Physical Functional in Intensive Care Unit Test-scored; Chelsea Critical Care Physical Assessment Tool; Intensive Care Unit Mobility scale; and Functional Status Score for the Intensive Care Unit (FSS-ICU). In contrast to the other instruments, the FSS-ICU measures functional activities exclusively, and scores the level of physical assistance for each activity, including walking. More specifically, the FSS-ICU[15],[16] measures the level of physical assistance in five functional activities relevant to the intensive care unit setting (rolling, supine to sit transfer, sit to stand transfer, sitting at the edge of the bed, and walking). The FSS-ICU is a valid instrument based on an international psychometric evaluation[12],[16]. The inter-rater reliability is greater than 0.98[17],[18],[19] and it has construct validity with the Physical Functional in Intensive Care Unit Test-scored (Spearman rho = 0.85 to 0.87) and the Intensive Care Unit Mobility scale (Spearman rho = 0.46 to 0.95), among other measures[12],[16]. During early phases of critical illness, the FSS-ICU can predict the recovery of patients’ ability to walk[20], with a 1-point increase in the FSS-ICU total score being associated with a 6-hour reduction in hospital stay (p < 0.01) and an increase discharge to home (Odds Ratio 1.11; 95% Confidence Interval: 1.06 to 1.17)[16]. The FSS-ICU does not require additional equipment and can be easily integrated into routine clinical care by intensive care unit physiotherapists, which contributed to our interest in selecting this instrument for adaptation for Chile[10],[16].
Translation and cross-cultural adaptation is recommended to preserve the semantic, conceptual, experiential and idiomatic equivalence between the original version and the translated version of a measurement instrument[21]. Although there is a FSS-ICU Spanish version available, cross-cultural adaptation has not been published[22]. Hence, the aim of this project was to translate and cross-culturally adapt all documents related to the original FSS-ICU (full version, pocket card, and Frequently Asked Questions) to create a complete Chilean Spanish version.
Method
Study design
The translation and cross-cultural adaptation methodology for this project was based on guidelines recommended by Beaton et al.[21]. We contacted, via email, Dale Needham, MD, PhD (corresponding author of the original version of the FSS-ICU) who authorized the cross-cultural adaptation process in Chile. The present study respected ethical standards in accordance with the Declaration of Helsinki and was approved by the Research Ethics Committee of the Facultad de Medicina de la Clínica Alemana de Santiago Universidad del Desarrollo (Nº 2017-104).
Description of the Functional Status Score for the Intensive Care Unit
The FSS-ICU is designed to measure physical functioning in the intensive care unit, and quantifies the level of physical assistance required by the patient in five specific tasks: rolling, supine to sit transfer, sit to stand transfer, sitting at the edge of bed, and walking[15],[16].This measure can be incorporated into clinical evaluations routinely performed by a physiotherapist with little added time required, or as a stand-alone research evaluation with an estimated time for completion of 10 to 30 minutes (depending on the patient's functional status)[16]. Each activity is scored using an eight-point ordinal scale ranging from 0 (unable to perform) to 7 (complete independence). The total score is a sum of the individual scores for each of the five activities, with a range from 0 to 35 points, where a higher score indicates greater functional independence[16].
Documents
The existing FSS-ICU Spanish version v29.08.16, available at www.ImproveLTO.com/instruments/ (ImproveLTO Spanish version), was used as a starting point for this project. This FSS-ICU Spanish was previously translated with the original developers of the FSS-ICU[22], based on the first four recommended stages from Beaton et al.[21]: two independent translations into Chilean Spanish (Stage I), synthesis of these first Chilean Spanish versions (Stage II), two independent translations into English (Stage III) and review of all documents by an expert review committee (Stage IV). The expert review committee for this project discussed and resolved any ambiguities from the forward and backward synthesis to derive the final FSS-ICU Chilean Spanish version In addition, the original pocket card (English language), available at www.ImproveLTO.com/instruments/ was also used for this project. The pocket card was translated and reviewed by an expert committee composed by a moderator, language professional, methodologist, critical care physiotherapy specialist, co-authors of the study and the translators. This expert committee met in-person to translate and review the pocket card version using the Spanish version of improveLTO.com as a reference.
Cognitive interviews (Stage V)
The purpose of the cognitive interviews was to test the understanding and interpretation of the instrument by the stakeholders, which corresponds to Stage V of the guidelines from Beaton et al.[21]. Thirty physiotherapists from public and private hospitals in Chile were selected and invited by email to participate in this stage. The selection criteria for the physiotherapists were as follows: 1) physiotherapy degree from a university recognized by the Chilean state, 2) at least one year of clinical work experience in the intensive care unit, and 3) existing knowledge of the FSS-ICU. Once the first contact was made, two co-authors (ACM and FGS) conducted interviews with each physiotherapist.
The interviews were structured according to the following three stages: 1) Reading the FSS-ICU: the interviewed physiotherapists were asked to read the complete FSS-ICU measure; 2) Scoring the FSS-ICU: they were shown a video of a patient evaluated with the FSS-ICU that included the five activities, with each physiotherapist scoring it according to the video, using the pocket version and the full version of the FSS-ICU; and 3) Cognitive interview: cognitive questions were asked to examine for possible semantic and conceptual uncertainties that arose when reading and scoring the instrument[23],[24]. The methodology used was Think-aloud and verbal probing, as described by Miller et al.[25] and Willis et al.[26],[27], through face-to-face semi-structured interviews. Interpretation of the general guidelines, specific instructions, activities and scores for different clinical scenarios were explored. In each interview, an audio recording was made as documentation of the cognitive interview, and all concerns and questions of the physiotherapists interviewed were collected to build the Frequently Asked Questions (when the questions were repeated by at least three physiotherapists).
After every ten interviews, a consensus meeting was held between two co-authors (ACM and FGS) and a methodologist (JL) to define when to make adaptations. This allowed the FSS-ICU to be retested in the following ten interviews. The role of the methodologist was to monitor if the adaptations maintained the essence of the original FSS-ICU. After every block of 10 interviews and consensus meeting the adaptations were made, and the new version was tested in the following ten physiotherapists until completing 30 cognitive interviews. The patient who was filmed and all the participating physiotherapists signed an informed consent and confidentiality agreement, respectively.
Final report to the authors (Stage VI)
A report of the cross-cultural adaptation process was sent to the senior authors of the original English FSS-ICU and the Portuguese translation/adaptation (DMN and FSG, respectively) to receive their feedback and approval. These senior authors monitored the adaptation process in order to preserve the original structure and essence of the FSS-ICU, and ensure that the process was consistent with that used for the FSS-ICU Brazilian version[19].
Data analysis
To analyze results, the existing Spanish version of the FSS-ICU and the pre-final Chilean Spanish pocket card were divided into 85 and 18 items, respectively (including the general guidelines, specific instructions, activities, and scores of the FSS-ICU).
Content validity is the degree to which an instrument has an appropriate sample of items for the construct being measured and is an important procedure in scale development. In this study, the Content Validity Index for Scales[28] methodology was used to assess the agreement of the pre-final Chilean Spanish pocket card among the participants of the expert committee.
The interviews participants used two criteria -“agree” and “do not agree” - to rate the equivalence of each item. Adaptations of the documents were made when agreement among the physiotherapists was less than 80%. The agreement for each item was calculated as follows: multiplying the number of physiotherapists who agreed by 100, and dividing it by the total number of participating physiotherapists. Agreement was considered acceptable if 80% or greater[28].
Results
The expert committee consisted of ten professionals with a median (inter-quartile range) number of years of professional experience of 20 (16 to 21) (Table 1). The translation and review of the Chilean pocket card reported a Content Validity Index for Scales = 0.97 among the participants of the experts committee.
Thirty physiotherapists were interviewed to perform Stage V during a one-month period from May 25 to June 22, 2018. These participants had a median (inter-quartile range) age of 32.5 (30 to 36) years, a median of 6 (4.25 to 9.75) years of experience in the intensive care unit, and 33% had specialization in critical care physiotherapy from the National Association of Accreditation of Specialist Physiotherapists (Table 2). The 18 hospitals in which the physiotherapists worked included public (14) and private (4) facilities. The cognitive interviews had median duration of 51.5 (41.0 to 61.0) minutes. During the Stage V, adaptations were made in 3 of 85 items of the existing Spanish version of the FSS-ICU (Table 3), and in 2 of 18 items in the pre-final Chilean Spanish pocket version (Table 4). These adaptations corresponded mainly to items in the instructions and general guidelines. At the end of the interviews and consensus, all items obtained 100% agreement among the physiotherapists for the full Chilean version, the Chilean pocket card version, and an update of the Spanish Frequently Asked Questions of the FSS-ICU, all freely available for non-commercial use from www.ImproveLTO.com.
Discussion
In Chile, the translation and cross-cultural adaptation process is frequently used to adapt Spanish measurement instruments from original English language instrument[29],[30],[31],[32],[33],[34]. The present study was based on the international recommendations of Beaton et al.[21], as well as the translation and adaptation process used to create the Brazilian version of the FSS-ICU[19]. This recommended process allows the comparison of the same measurement instrument in different countries and cultures, and avoids possible comprehension problems that could occur with literal translations[35].
Despite frequent application of this translation and cross-cultural adaptation process, there is heterogeneity in the recommendations available[36]. However, Epstein et al.[37] reported that the expert committee and cognitive interviews are essential stages of this process. In the present work, these two stages were conducted yielding relevant insights regarding application of the FSS-ICU, which allowed expansion of the existing English-language Frequently Asked Questions in creating the Spanish Frequently Asked Questions as a complementary document for the Chilean FSS-ICU.
Stage V of the cross-cultural adaptation process is a pre-test of the translate/adapted instrument, with a recommendation for including at least 30 subjects[21]. In the pre-test of the Brazilian FSS-ICU, two qualified physiotherapists with standardized training in FSS-ICU tested the pre-final version in a total of 30 critically ill patients[19]. On the other hand, the pre-test conducted in the present study was based on cognitive interviews in 30 ICU physiotherapists, who applied the full FSS-ICU and its pocket card version. This cognitive interview is a strategy that increases face validity of an instrument, and has become a key qualitative method for the pre-test and evaluation of questionnaires[26],[27]. This issue is especially relevant since the FSS-ICU is a performance-based evaluation instrument in which interpretation of patient peformance by the evaluator is important in contrast to a patient-reported instrument in which interpretation of the patient’s perspective is the focus. For this reason, in the present study, the cognitive interviews allowed the Spanish FSS-ICU to be refined based on verbal reports and experience of the 30 intensive care unit physiotherapists.
The FSS-ICU is one recommended instrument for evaluating physical functioning in intensive care unit[10],[11]. The FSS-ICU measures the physical assistance level in five activities, including walking, and has psychometric evaluations that enforce the robustness of this instrument for use in clinical practice and research in critically ill patients[16],[17]. This recommendation for use of the FSS-ICU justifies efforts to translate and adapt the original instrument in countries with other languages and cultures.
This study has potential limitations. For instance, the Chilean FSS-ICU was not applied in face-to-face evaluations of intensive care unit patients, but was evaluated in a more standardized manner using a video of its application with a critically ill patient. Another limitation of this study was that the final document was not re-tested again; however, the final agreement was 100% in the items that needed adaptations. Moreover, all physiotherapists included in the study belong to four regions of Chile; hence, the linguistic differences of other Chilean regions were not considered in the process.
This study is part of the validation process of the FSS-ICU in Chile. This first step allows the instrument to be available to measure its psychometric properties, such as interobserver reliability and construct validity.
In conclusion, the Chilean version of the FSS-ICU can be used to assess the physical functioning. The FSS-ICU is freely available for non-commercial clinical and research use by Chilean Spanish-speakers, minimizing misinterpretation of the original FSS-ICU. However, despite this translation/adaptation, training may be valuable to ensure correct implementation of this instrument. Future research should evaluate the psychometric properties of this version of the FSS-ICU in Chile.
Notes
From the editor
The authors originally submitted this article in English.
Contributor roles
FGS, ACM, JL: Conceptualization, FGS, ACM, JL: Formal analysis, JL, VHC, TGP: Funding acquisition, FGS, ACM, JL, DMN, FSG: Investigation, FGS, ACM, JL, DMN, FSG: Methodology, FGS, ACM: Project administration, JL, VHC, TGP: Resources, JL, DMN, FSG: Supervision, FGS, ACM, JL, DMN, FSG: Visualization, FGS, ACM, JL: Writing – original draft, FGS, ACM, JL, VHC, TGP, DMN, FSG: Writing – review & editing.
Acknowledgments
The authors thank all those who participated in the cognitive interviews for their voluntary contribution to the study. We also thank the School of Physical Therapy, Clínica Alemana Universidad del Desarrollo, the Physical Medicine and Rehabilitation Department of the Clínica Alemana de Santiago and the Program of Master in Physical Therapy and Rehabilitation of the Universidad del Desarrollo for the support for this study.
Competing interests
The authors have completed the ICMJE conflict of interest declaration form, and declare that they have not received funding for the completion of the report; have no financial relationships with organizations that might have an interest in the published article in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the responsible author or the editorial board of the Journal.
Funding
This study received financial support from the School of Physical Therapy, Clínica Alemana Universidad del Desarrollo, and from the Departamento Científico Docente, Clínica Alemana de Santiago. The funders had no role in the design of the study, the collection and analysis of data, the decision to publish or in the preparation of the manuscript.

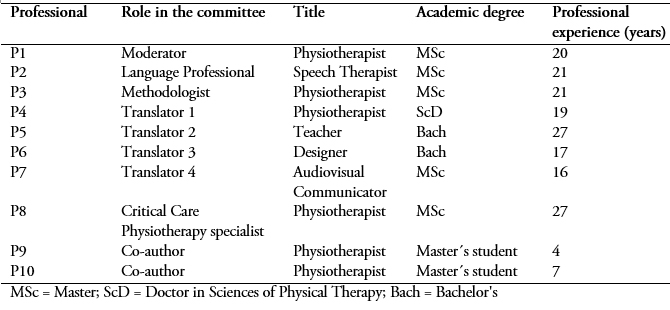 Table 1. Characteristics of the expert committee that translated and reviewed the pre-final version of the pocket card.
Table 1. Characteristics of the expert committee that translated and reviewed the pre-final version of the pocket card.

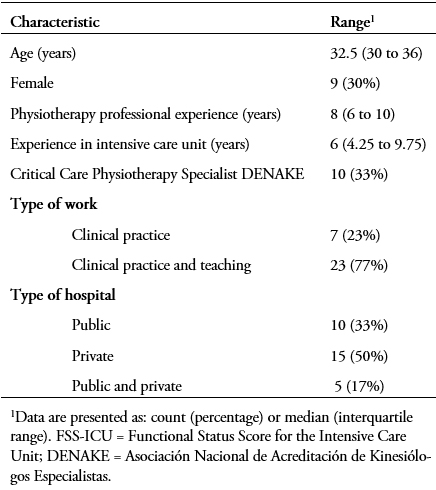 Table 2. Characteristics of the physiotherapist interviewed during cognitive interviews of the Chilean FSS-ICU (n = 30).
Table 2. Characteristics of the physiotherapist interviewed during cognitive interviews of the Chilean FSS-ICU (n = 30).

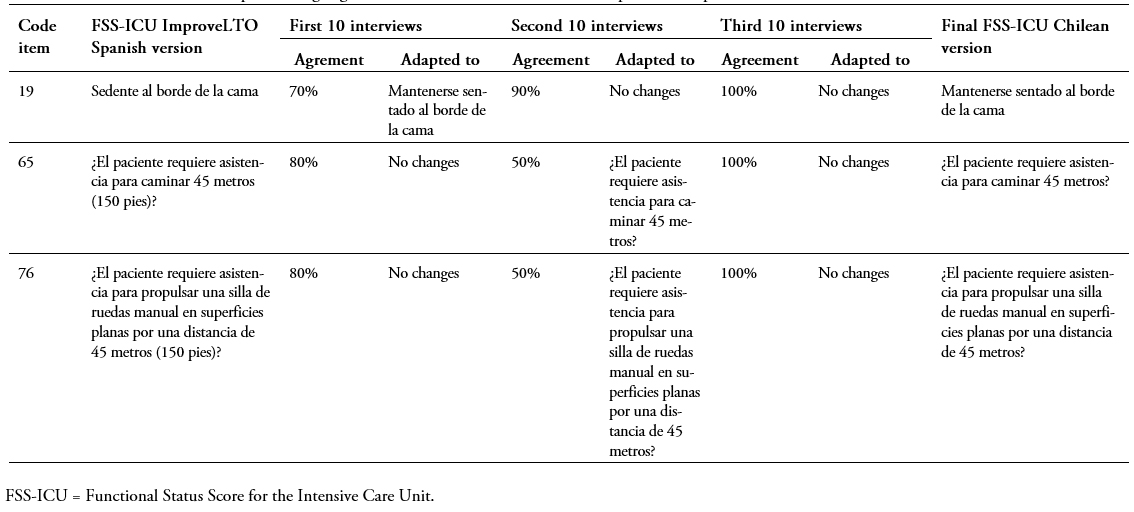 Table 3. Results of the items adapted during cognitive interviews of the full FSS-ICU ImproveLTO Spanish versión
Table 3. Results of the items adapted during cognitive interviews of the full FSS-ICU ImproveLTO Spanish versión

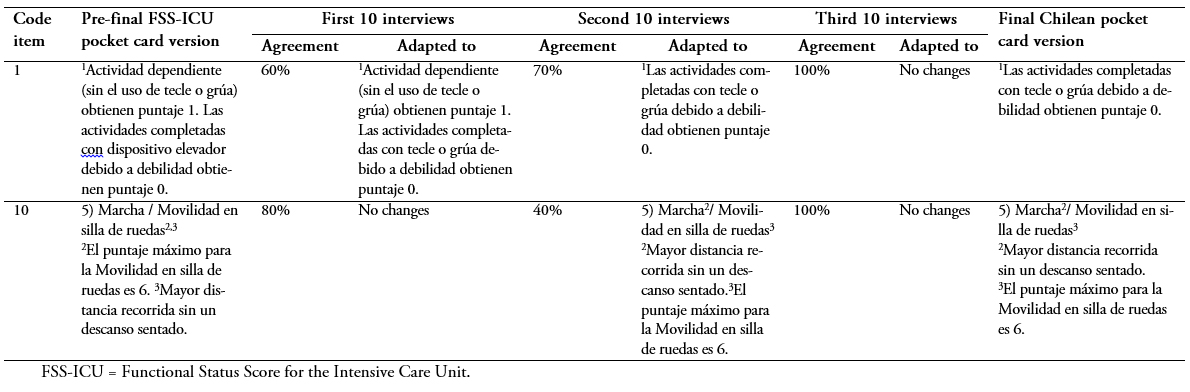 Table 4. Results of the items adapted during cognitive interviews of the pre-final FSS-ICU pocket card version.
Table 4. Results of the items adapted during cognitive interviews of the pre-final FSS-ICU pocket card version.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

Introducción
La Functional Status Score for the Intensive Care Unit (FSS-ICU) es un instrumento válido y confiable para medir funcionamiento físico en unidades de cuidados intensivos. Sin embargo, la traducción y adaptación transcultural de la FSS-ICU en Chile no ha sido publicada.
Objetivo
Traducir y adaptar transculturalmente todos los documentos asociados de la FSS ICU original para Chile.
Método
Se utilizó como punto de partida la versión en español de FSS-ICU, disponible en www.ImproveLTO.com. Esta versión se tradujo previamente con los desarrolladores originales de la FSS-ICU, siguiendo las recomendaciones establecidas para este proceso. La versión de bolsillo chilena se desarrolló recientemente en base a la versión original en inglés. Se realizaron entrevistas cognitivas a kinesiólogos de la unidad de cuidados intensivos para evaluar la comprensión de la FSS-ICU y versión de bolsillo. Las adaptaciones se realizaron cuando el acuerdo entre los kinesiólogos fue inferior al 80%.
Resultados
Se realizaron las entrevistas cognitivas de la FSS-ICU en español (85 ítems) y versión de bolsillo (18 ítems) en 30 kinesiólogos chilenos provenientes de 18 diferentes hospitales (14 públicos y 4 privados). Durante las entrevistas se realizaron adaptaciones principalmente en las guías generales e instrucciones específicas para tres ítems de la FSS-ICU y dos elementos de la versión de bolsillo. Finalmente, se desarrollaron las preguntas frecuentes, la versión de bolsillo y la versión completa de la FSS-ICU. Todas las adaptaciones fueron aceptadas por los desarrolladores originales.
Conclusiones
La versión chilena de la FSS-ICU fue fácil de entender por los kinesiólogos. La FSS-ICU está disponible gratis para uso clínico e investigación no comercial en Chile.
 Authors:
Felipe González-Seguel[1,2], Agustín Camus-Molina[1,2], Jaime Leppe[2], Viviane Hidalgo-Cabalín[1], Tania Gutiérrez-Panchana[1], Dale M. Needham[3], Fernando S. Guimarães[4]
Authors:
Felipe González-Seguel[1,2], Agustín Camus-Molina[1,2], Jaime Leppe[2], Viviane Hidalgo-Cabalín[1], Tania Gutiérrez-Panchana[1], Dale M. Needham[3], Fernando S. Guimarães[4]
Affiliation:
[1] Servicio de Medicina Física y Rehabilitación, Departamento de Medicina Interna, Facultad de Medicina, Clínica Alemana Universidad del Desarrollo, Santiago, Chile
[2] Programa de Magíster en Terapia Física y Rehabilitación, Carrera de Kinesiología, Facultad de Medicina, Clínica Alemana Universidad del Desarrollo, Santiago, Chile
[3] Pulmonary & Critical Care Medicine and Physical Medicine & Rehabilitation, Johns Hopkins University, Baltimore, Maryland, United States
[4] Faculdade de Medicina da Universidade Federal do Rio Janeiro, Departamento de Fisioterapia, Rio Janeiro, Brasil
E-mail: feligonzalezs@udd.cl
Author address:
[1] Departamento de Medicina Interna
Facultad de Medicina
Clínica Alemana Universidad del Desarrollo
Vitacura 5951
Vitacura
Santiago
Chile

Citation: González-Seguel F, Camus-Molina A, Leppe J, Hidalgo-Cabalín V, Gutiérrez-Panchana T, Needham DM, et al. Chilean version of the Functional Status Score for the Intensive Care Unit: a translation and cross-cultural adaptation. Medwave 2019;19(1):e7439 doi: 10.5867/medwave.2019.01.7439
Submission date: 11/9/2018
Acceptance date: 20/12/2018
Publication date: 7/1/2019
Origin: not requested
Type of review: reviewed by two external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Spragg RG, Bernard GR, Checkley W, Curtis JR, Gajic O, Guyatt G, et al . Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010 May 15;181(10):1121-7. | CrossRef | PubMed |
- Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012 Feb;40(2):502-9. | CrossRef | PubMed |
- Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011 Apr 7;364(14):1293-304. | CrossRef | PubMed |
- Alvear V S, Canteros J, Rodríguez P. [Calculation of costs per inpatient day in an intensive care unit]. Rev Med Chil. 2010 May;138(5):558-66. | CrossRef | PubMed |
- Ruhl AP, Huang M, Colantuoni E, Karmarkar T, Dinglas VD, Hopkins RO, et al. Healthcare utilization and costs in ARDS survivors: a 1-year longitudinal national US multicenter study. Intensive Care Med. 2017 Jul;43(7):980-991. | CrossRef | PubMed |
- Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009 May 30;373(9678):1874-82. | CrossRef | PubMed |
- Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016 Oct 1;388(10052):1377-1388. | CrossRef | PubMed |
- Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017 Feb;43(2):171-183. | CrossRef | PubMed |
- Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of Early Rehabilitation during Intensive Care Unit Stay on Functional Status: Systematic Review and Meta-Analysis. PLoS One. 2015 Jul 1;10(7):e0130722. | CrossRef | PubMed |
- Parry SM, Huang M, Needham DM. Evaluating physical functioning in critical care: considerations for clinical practice and research. Crit Care. 2017 Oct 4;21(1):249. | CrossRef | PubMed |
- Parry SM, Nydahl P, Needham DM. Implementing early physical rehabilitation and mobilisation in the ICU: institutional, clinician, and patient considerations. Intensive Care Med. 2018 Apr;44(4):470-473. | CrossRef | PubMed |
- Parry SM, Denehy L, Beach LJ, Berney S, Williamson HC, Granger CL. Functional outcomes in ICU – what should we be using? – an observational study. Crit Care. 2015 Mar 29;19:127. | CrossRef | PubMed |
- Parry SM, Granger CL, Berney S, Jones J, Beach L, El-Ansary D, et al. Assessment of impairment and activity limitations in the critically ill: a systematic review of measurement instruments and their clinimetric properties. Intensive Care Med. 2015 May;41(5):744-62. | CrossRef | PubMed |
- Libuy MH, Szita CP, Hermosilla PJ, Arellano SD, Rodríguez-Núñez I, Báez RC. [Validity of scales for the functional assessment of critically ill patients]. Rev Med Chil. 2017 Sep;145(9):1137-1144. | CrossRef | PubMed |
- Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010 Jun;25(2):254-62. | CrossRef | PubMed |
- Huang M, Chan KS, Zanni JM, Parry SM, Neto SG, Neto JA, et al. Functional Status Score for the ICU: An International Clinimetric Analysis of Validity, Responsiveness, and Minimal Important Difference. Crit Care Med. 2016 Dec;44(12):e1155-e1164. | PubMed |
- Hiser S, Toonstra A, Friedman LA, Colantuoni E, Connolly B, Needham DM. Interrater Reliability of the Functional Status Score for the Intensive Care Unit. J Acute Care Phys Ther. Oct 2018;9(4):186-192. | CrossRef |
- Ragavan VK, Greenwood KC, Bibi K. The Functional Status Score for the Intensive Care Unit Scale. J Acute Care Phys Ther 2016;7:93-100. | CrossRef |
- Silva VZM da, Araújo Neto JA de, Cipriano Júnior G, et al. Brazilian version of the Functional Status Score for the ICU: translation and cross-cultural adaptation. Rev Bras Ter Intensiva 2017;29:34-8. | CrossRef | Link |
- Mehrholz J, Mückel S, Oehmichen F, Pohl M. First results about recovery of walking function in patients with intensive care unit-acquired muscle weakness from the General Weakness Syndrome Therapy (GymNAST) cohort study. BMJ Open. 2015 Dec 23;5(12):e008828. | CrossRef | PubMed |
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000 Dec 15;25(24):3186-91. | PubMed |
- Guimarães FS, González-Seguel FA, Zanni JM, et al. The spanish translation and cross-cultural adaptation of the Functional Status Score for the Intensive Care Unit (FSS-ICU). In: Poster presented at: World Confederation for Physical Therapy Congress. Cape Town: 2-4 ;July 2017.
- Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs. 2003 Apr;42(1):57-63. | PubMed |
- Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993 Dec;46(12):1417-32. | PubMed |
- Miller K, Willson S, Chepp V, et al. Cognitive Interviewing Methodology. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2014. | CrossRef | Link |
- Willis G, Lawrence D, Thompson F, et al. The Use of Cognitive Interviewing to Evaluate Translated Survey Questions : Lessons Learned;2005:1-9. | CrossRef | Link |
- Willis GB, Miller K. Cross-Cultural Cognitive Interviewing. Field methods 2011;23:331-41. | CrossRef | Link |
- Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006 Oct;29(5):489-97. | PubMed |
- Merellano-Navarro E, Lapierre M, García-Rubio J, et al. Traducción y adaptación cultural del cuestionario de independencia física Composite Physical Function para su uso en Chile. Rev Med Chil 2015;143:1314-9. | CrossRef |
- Alarcon M AM, Muñoz NS. Medición en salud: Algunas consideraciones metodológicas. Rev Med Chil 2008;136:125–30. | CrossRef | Link |
- Binfa L, Cancino V, Ugarte I, Mella M, Cavada G. [Cultural adaptation and translation of the Woman Abuse Screening Tool]. Rev Med Chil. 2018 Mar;146(3):331-340. | CrossRef | PubMed |
- Villoria E, Lara L. Assessment of the Hospital Anxiety and Depression Scale for cancer patients. Rev Med Chil. 2018 Mar;146(3):300-307. | CrossRef | PubMed |
- Borghero F, Martínez V, Zitko P, Vöhringer PA, Cavada G, Rojas G. [Screening depressive episodes in adolescents. Validation of the Patient Health Questionnaire-9 (PHQ-9)]. Rev Med Chil. 2018 Apr;146(4):479-486. | CrossRef | PubMed |
- Sepúlveda P R, Molina G. T, Molina C. R, et al. Adaptación transcultural y validación de un instrumento de calidad de vida relacionada con la salud en adolescentes chilenos. Rev Med Chil 2013;141:1283-92. | CrossRef | Link |
- Breugelmans R. Dangers in using translated medical questionnaires: the importance of conceptual equivalence across languages and cultures in patient-reported outcome measures. Chest. 2009 Oct;136(4):1175-1177. | CrossRef | PubMed |
- Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005 Mar-Apr;8(2):94-104. | PubMed |
- Epstein J, Santo RM, Guillemin F. A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. J Clin Epidemiol 2015;68:435–41. | CrossRef |
 Spragg RG, Bernard GR, Checkley W, Curtis JR, Gajic O, Guyatt G, et al . Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010 May 15;181(10):1121-7. | CrossRef | PubMed |
Spragg RG, Bernard GR, Checkley W, Curtis JR, Gajic O, Guyatt G, et al . Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010 May 15;181(10):1121-7. | CrossRef | PubMed | Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012 Feb;40(2):502-9. | CrossRef | PubMed |
Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012 Feb;40(2):502-9. | CrossRef | PubMed | Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011 Apr 7;364(14):1293-304. | CrossRef | PubMed |
Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011 Apr 7;364(14):1293-304. | CrossRef | PubMed | Alvear V S, Canteros J, Rodríguez P. [Calculation of costs per inpatient day in an intensive care unit]. Rev Med Chil. 2010 May;138(5):558-66. | CrossRef | PubMed |
Alvear V S, Canteros J, Rodríguez P. [Calculation of costs per inpatient day in an intensive care unit]. Rev Med Chil. 2010 May;138(5):558-66. | CrossRef | PubMed | Ruhl AP, Huang M, Colantuoni E, Karmarkar T, Dinglas VD, Hopkins RO, et al. Healthcare utilization and costs in ARDS survivors: a 1-year longitudinal national US multicenter study. Intensive Care Med. 2017 Jul;43(7):980-991. | CrossRef | PubMed |
Ruhl AP, Huang M, Colantuoni E, Karmarkar T, Dinglas VD, Hopkins RO, et al. Healthcare utilization and costs in ARDS survivors: a 1-year longitudinal national US multicenter study. Intensive Care Med. 2017 Jul;43(7):980-991. | CrossRef | PubMed | Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009 May 30;373(9678):1874-82. | CrossRef | PubMed |
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009 May 30;373(9678):1874-82. | CrossRef | PubMed | Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016 Oct 1;388(10052):1377-1388. | CrossRef | PubMed |
Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016 Oct 1;388(10052):1377-1388. | CrossRef | PubMed | Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017 Feb;43(2):171-183. | CrossRef | PubMed |
Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017 Feb;43(2):171-183. | CrossRef | PubMed | Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of Early Rehabilitation during Intensive Care Unit Stay on Functional Status: Systematic Review and Meta-Analysis. PLoS One. 2015 Jul 1;10(7):e0130722. | CrossRef | PubMed |
Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of Early Rehabilitation during Intensive Care Unit Stay on Functional Status: Systematic Review and Meta-Analysis. PLoS One. 2015 Jul 1;10(7):e0130722. | CrossRef | PubMed | Parry SM, Huang M, Needham DM. Evaluating physical functioning in critical care: considerations for clinical practice and research. Crit Care. 2017 Oct 4;21(1):249.
| CrossRef | PubMed |
Parry SM, Huang M, Needham DM. Evaluating physical functioning in critical care: considerations for clinical practice and research. Crit Care. 2017 Oct 4;21(1):249.
| CrossRef | PubMed | Parry SM, Nydahl P, Needham DM. Implementing early physical rehabilitation and mobilisation in the ICU: institutional, clinician, and patient considerations. Intensive Care Med. 2018 Apr;44(4):470-473. | CrossRef | PubMed |
Parry SM, Nydahl P, Needham DM. Implementing early physical rehabilitation and mobilisation in the ICU: institutional, clinician, and patient considerations. Intensive Care Med. 2018 Apr;44(4):470-473. | CrossRef | PubMed | Parry SM, Denehy L, Beach LJ, Berney S, Williamson HC, Granger CL. Functional outcomes in ICU – what should we be using? – an observational study. Crit Care. 2015 Mar 29;19:127. | CrossRef | PubMed |
Parry SM, Denehy L, Beach LJ, Berney S, Williamson HC, Granger CL. Functional outcomes in ICU – what should we be using? – an observational study. Crit Care. 2015 Mar 29;19:127. | CrossRef | PubMed | Parry SM, Granger CL, Berney S, Jones J, Beach L, El-Ansary D, et al. Assessment of impairment and activity limitations in the critically ill: a systematic review of measurement instruments and their clinimetric properties. Intensive Care Med. 2015 May;41(5):744-62. | CrossRef | PubMed |
Parry SM, Granger CL, Berney S, Jones J, Beach L, El-Ansary D, et al. Assessment of impairment and activity limitations in the critically ill: a systematic review of measurement instruments and their clinimetric properties. Intensive Care Med. 2015 May;41(5):744-62. | CrossRef | PubMed | Libuy MH, Szita CP, Hermosilla PJ, Arellano SD, Rodríguez-Núñez I, Báez RC. [Validity of scales for the functional assessment of critically ill patients]. Rev Med Chil. 2017 Sep;145(9):1137-1144. | CrossRef | PubMed |
Libuy MH, Szita CP, Hermosilla PJ, Arellano SD, Rodríguez-Núñez I, Báez RC. [Validity of scales for the functional assessment of critically ill patients]. Rev Med Chil. 2017 Sep;145(9):1137-1144. | CrossRef | PubMed | Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010 Jun;25(2):254-62. | CrossRef | PubMed |
Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010 Jun;25(2):254-62. | CrossRef | PubMed | Huang M, Chan KS, Zanni JM, Parry SM, Neto SG, Neto JA, et al. Functional Status Score for the ICU: An International Clinimetric Analysis of Validity, Responsiveness, and Minimal Important Difference. Crit Care Med. 2016 Dec;44(12):e1155-e1164. | PubMed |
Huang M, Chan KS, Zanni JM, Parry SM, Neto SG, Neto JA, et al. Functional Status Score for the ICU: An International Clinimetric Analysis of Validity, Responsiveness, and Minimal Important Difference. Crit Care Med. 2016 Dec;44(12):e1155-e1164. | PubMed | Hiser S, Toonstra A, Friedman LA, Colantuoni E, Connolly B, Needham DM. Interrater Reliability of the Functional Status Score for the Intensive Care Unit. J Acute Care Phys Ther. Oct 2018;9(4):186-192. | CrossRef |
Hiser S, Toonstra A, Friedman LA, Colantuoni E, Connolly B, Needham DM. Interrater Reliability of the Functional Status Score for the Intensive Care Unit. J Acute Care Phys Ther. Oct 2018;9(4):186-192. | CrossRef | Ragavan VK, Greenwood KC, Bibi K. The Functional Status Score for the Intensive Care Unit Scale. J Acute Care Phys Ther 2016;7:93-100. | CrossRef |
Ragavan VK, Greenwood KC, Bibi K. The Functional Status Score for the Intensive Care Unit Scale. J Acute Care Phys Ther 2016;7:93-100. | CrossRef | Silva VZM da, Araújo Neto JA de, Cipriano Júnior G, et al. Brazilian version of the Functional Status Score for the ICU: translation and cross-cultural adaptation. Rev Bras Ter Intensiva 2017;29:34-8. | CrossRef | Link |
Silva VZM da, Araújo Neto JA de, Cipriano Júnior G, et al. Brazilian version of the Functional Status Score for the ICU: translation and cross-cultural adaptation. Rev Bras Ter Intensiva 2017;29:34-8. | CrossRef | Link | Mehrholz J, Mückel S, Oehmichen F, Pohl M. First results about recovery of walking function in patients with intensive care unit-acquired muscle weakness from the General Weakness Syndrome Therapy (GymNAST) cohort study. BMJ Open. 2015 Dec 23;5(12):e008828. | CrossRef | PubMed |
Mehrholz J, Mückel S, Oehmichen F, Pohl M. First results about recovery of walking function in patients with intensive care unit-acquired muscle weakness from the General Weakness Syndrome Therapy (GymNAST) cohort study. BMJ Open. 2015 Dec 23;5(12):e008828. | CrossRef | PubMed | Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000 Dec 15;25(24):3186-91. | PubMed |
Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000 Dec 15;25(24):3186-91. | PubMed | Guimarães FS, González-Seguel FA, Zanni JM, et al. The spanish translation and cross-cultural adaptation of the Functional Status Score for the Intensive Care Unit (FSS-ICU). In: Poster presented at: World Confederation for Physical Therapy Congress. Cape Town: 2-4 ;July 2017.
Guimarães FS, González-Seguel FA, Zanni JM, et al. The spanish translation and cross-cultural adaptation of the Functional Status Score for the Intensive Care Unit (FSS-ICU). In: Poster presented at: World Confederation for Physical Therapy Congress. Cape Town: 2-4 ;July 2017.  Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs. 2003 Apr;42(1):57-63. | PubMed |
Drennan J. Cognitive interviewing: verbal data in the design and pretesting of questionnaires. J Adv Nurs. 2003 Apr;42(1):57-63. | PubMed | Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993 Dec;46(12):1417-32. | PubMed |
Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993 Dec;46(12):1417-32. | PubMed | Miller K, Willson S, Chepp V, et al. Cognitive Interviewing Methodology. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2014. | CrossRef | Link |
Miller K, Willson S, Chepp V, et al. Cognitive Interviewing Methodology. Hoboken, NJ, USA: John Wiley & Sons, Inc; 2014. | CrossRef | Link | Willis G, Lawrence D, Thompson F, et al. The Use of Cognitive Interviewing to Evaluate Translated Survey Questions : Lessons Learned;2005:1-9. | CrossRef | Link |
Willis G, Lawrence D, Thompson F, et al. The Use of Cognitive Interviewing to Evaluate Translated Survey Questions : Lessons Learned;2005:1-9. | CrossRef | Link | Willis GB, Miller K. Cross-Cultural Cognitive Interviewing. Field methods 2011;23:331-41. | CrossRef | Link |
Willis GB, Miller K. Cross-Cultural Cognitive Interviewing. Field methods 2011;23:331-41. | CrossRef | Link | Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006 Oct;29(5):489-97. | PubMed |
Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health. 2006 Oct;29(5):489-97. | PubMed | Merellano-Navarro E, Lapierre M, García-Rubio J, et al. Traducción y adaptación cultural del cuestionario de independencia física Composite Physical Function para su uso en Chile. Rev Med Chil 2015;143:1314-9. | CrossRef |
Merellano-Navarro E, Lapierre M, García-Rubio J, et al. Traducción y adaptación cultural del cuestionario de independencia física Composite Physical Function para su uso en Chile. Rev Med Chil 2015;143:1314-9. | CrossRef | Alarcon M AM, Muñoz NS. Medición en salud: Algunas consideraciones metodológicas. Rev Med Chil 2008;136:125–30. | CrossRef | Link |
Alarcon M AM, Muñoz NS. Medición en salud: Algunas consideraciones metodológicas. Rev Med Chil 2008;136:125–30. | CrossRef | Link | Binfa L, Cancino V, Ugarte I, Mella M, Cavada G. [Cultural adaptation and translation of the Woman Abuse Screening Tool]. Rev Med Chil. 2018 Mar;146(3):331-340. | CrossRef | PubMed |
Binfa L, Cancino V, Ugarte I, Mella M, Cavada G. [Cultural adaptation and translation of the Woman Abuse Screening Tool]. Rev Med Chil. 2018 Mar;146(3):331-340. | CrossRef | PubMed | Villoria E, Lara L. Assessment of the Hospital Anxiety and Depression Scale for cancer patients. Rev Med Chil. 2018 Mar;146(3):300-307. | CrossRef | PubMed |
Villoria E, Lara L. Assessment of the Hospital Anxiety and Depression Scale for cancer patients. Rev Med Chil. 2018 Mar;146(3):300-307. | CrossRef | PubMed | Borghero F, Martínez V, Zitko P, Vöhringer PA, Cavada G, Rojas G. [Screening depressive episodes in adolescents. Validation of the Patient Health Questionnaire-9 (PHQ-9)]. Rev Med Chil. 2018 Apr;146(4):479-486. | CrossRef | PubMed |
Borghero F, Martínez V, Zitko P, Vöhringer PA, Cavada G, Rojas G. [Screening depressive episodes in adolescents. Validation of the Patient Health Questionnaire-9 (PHQ-9)]. Rev Med Chil. 2018 Apr;146(4):479-486. | CrossRef | PubMed | Sepúlveda P R, Molina G. T, Molina C. R, et al. Adaptación transcultural y validación de un instrumento de calidad de vida relacionada con la salud en adolescentes chilenos. Rev Med Chil 2013;141:1283-92. | CrossRef | Link |
Sepúlveda P R, Molina G. T, Molina C. R, et al. Adaptación transcultural y validación de un instrumento de calidad de vida relacionada con la salud en adolescentes chilenos. Rev Med Chil 2013;141:1283-92. | CrossRef | Link | Breugelmans R. Dangers in using translated medical questionnaires: the importance of conceptual equivalence across languages and cultures in patient-reported outcome measures. Chest. 2009 Oct;136(4):1175-1177. | CrossRef | PubMed |
Breugelmans R. Dangers in using translated medical questionnaires: the importance of conceptual equivalence across languages and cultures in patient-reported outcome measures. Chest. 2009 Oct;136(4):1175-1177. | CrossRef | PubMed | Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005 Mar-Apr;8(2):94-104. | PubMed |
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005 Mar-Apr;8(2):94-104. | PubMed | Epstein J, Santo RM, Guillemin F. A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. J Clin Epidemiol 2015;68:435–41. | CrossRef |
Epstein J, Santo RM, Guillemin F. A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. J Clin Epidemiol 2015;68:435–41. | CrossRef |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








