Key Words: elderly, dementia, cognitive decline, Peruvian
Abstract
INTRODUCTION
It is estimated that major neurocognitive disorders will affect 115.4 million people by 2050, representing a significant financial burden for society. Likewise, functional dependence for basic or instrumental activities of daily life is usually a consequence of the greater prevalence of disabling pathologies, and of the progressive decrease of the physiological reserve due to aging.
OBJECTIVES
To determine the ratio between the functional test and prediction of deterioration of cognitive function in geriatric patients. To determine which factors are associated with decreased cognitive functions in elderly patients
METHODS
This is a retrospective cohort study. We included participants who attended the Geriatrics Outpatient Services of the Naval Medical Center of Peru from 2010 to 2014. Two groups were formed, the first comprised those who presented physiological loss of cognitive functions, defined as the decrease less than 4.1 points in the score of the Mini Mental State Examination during follow-up and a second group who had a pathological loss of cognitive functions, defined as a decrease of 4.2 points in average or more in the Mini Mental State Examination score during follow-up. Patients were followed for four years, performing functional evaluations, as well as collecting data on comorbidities and sociodemographic factors.
RESULTS
We included 368 patients, whose mean age was 75.8 years and 50.91% male. Female gender (53.72%), poor education (62.81%), and comorbidities were statistically more frequent in the pathological cognitive decline group. Functional assessment variables had a worse disease progress through follow-up in the group with pathological disease progress of the Mini Mental State Examination score, including Timed Up & Go Test
CONCLUSIONS
Score values of Timed Up & Go Test manage to predict the risk of a pathological decrease in Mini Mental State Examination regardless of sociodemographic factors, comorbidities, and functional assessment.
Introduction
Major neurocognitive disorders are defined as the deterioration of one or more cognitive domains that interfere with functional independence in daily activities [1]. There are 35.6 million people living with cognitive impairment worldwide and it seems this figure will rise to 65.7 million in 2030 and 115.4 million in 2050 [2]. These disorders also represent a significant financial burden on society, similar to that caused by cardiovascular disease and cancer [3].
Mini-Mental State Examination is still the most widely used cognitive test in the world, known to detect a suspected cognitive impairment, determine the impairment severity and be useful for follow-up over time. It evaluates different cognitive domains such as orientation, registration or encoding memory, attention and calculation, recall, language and praxis [4]. There are different versions of the test, validated in multiple countries and languages, each one adapted to the reality of each country and with its own cut-off points [5].
On the other hand, functional impairment for basic or instrumental activities of daily life is usually a consequence of the higher prevalence of disabling pathologies and of the progressive decrease in the physiological reserve due to aging [6]. Functional dependency in older adults can be measured through different scores (Barthel, Lawton) [7],[8], but in recent years, performance-based instruments have been developed that assess physical performance and predict frailty, mortality, dysmobility and disability [9],[10], being an important part of the functional assessment. The most commonly used are the Timed Up&Go test [11], the Short physical performance battery [12] and gait speed.
There is evidence that tests that include gait speed are able to determine an increased risk of neurocognitive disorders in the older adults. In relation to this, there are known cut-off points for gait speed that can guide the clinician who evaluates this type of patients. However, Timed Up&Go test, which, in addition to gait assessment, evaluates the ability of getting up from a chair, does not have enough scientific evidence to associate it with a high incidence of neurocognitive disorders [13],[14]. Additionally, most studies that highlight the association between slow gait speed and high risk of neurocognitive disorders, define the presence of cognitive impairment with static cutoff points from different questionnaires, having found very little evidence of variations in the Mini-Mental State Examination score as a definition of new cases of neurocognitive disorders [15],[16].
Therefore, evaluating altered values in Timed Up&Go test and its association with decreased Mini-Mental State Examination score time will contribute to the physical, functional and mental evaluation of this population, facilitating the stratification of risk of neurocognitive disorders and decision making by health personnel.
Methods
Study design
This is a retrospective cohort study.
Population: Outpatient participants attended at the Geriatrics Service of Peruvian Naval Medical Center from 2010 to 2014 who accepted to participate in the study [17].
Inclusion criteria: Cognitively healthy patients, who presented a score of Mini Mental State Examination of 25 or more and a Pfeiffer test with three errors or less.
Exclusion criteria: Patients with a diagnosis of cerebrovascular disease, Parkinson's disease or other neurodegenerative disease (amyotrophic lateral sclerosis, Parkinson plus, Huntington), alcoholism, vitamin B12 deficiency, folic acid deficiency, hypothyroidism, use of antidementials and / or antipsychotics or that the patient has not agreed to participate in the study.
Sample
Our study population was that of 1,277 elderly patients of the ambulatory care levels of the Geriatrics Service of the Naval Medical Center, participants of a cohort study [17]. Only 368 participants met the inclusion / exclusion criteria. Of these, 21 participants did not have complete follow-up data and 17 participants died during the study, so their data were excluded. Therefore, the final sample size was of 330 participants.
Patients, recruited since January 2010, were followed annually, measuring functional scores, cognitive and sociodemographic variables. We calculated a power of 91% to find an average variation of the Mini Mental State Examination score of 5 points in both groups [18].
Variables
Decrease in the Mini Mental State Examination score
We used the Peruvian version of the Mini Mental State Examination [19] (score of 0-30) to define the evolution of cognitive problems. Annual variations of the Mini Mental State Examination score were followed. Two categories were created:
a) Physiological reduction of cognitive functions, defined as the decrease of 4.1 points or less in the Mini Mental State Examination score during follow-up.
b) Pathological decrease in cognitive functions, defined as the decrease of 4.2 points on average or more in the Mini Mental State Examination score during follow-up [15],[16].
Functional tests: performed at the day clinic of Geriatrics Service of the Naval Medical Center.
Timed Up & Go Test: the participant was asked to take a seat in a chair with braces, 45.8 cm high. Later he was given the following indications: "Take a seat in the chair, with your back on the backrest and your arms on the braces. When you hear 'ready', get up and walk to the line drawn on the floor at your usual speed, then turn and come back to sit on the chair again ". The stopwatch was started by saying the word "ready" and stopped when the patient sat down. The distance between the chair and the floor line was 3 meters. This variable was recorded as numerical, without cut-off points [20].
Short Physical Performance Battery: score of 0-12, three tests of 0-4 points each:
a) Balance: the participant was invited to stand with his or her feet parallel and in semi-tandem position, if he or she kept the balance properly for 10 seconds, a point was considered for each position. By inviting the participant to maintain balance in tandem position, he was given a point if he managed to stay 3-9 seconds and two points if he reached 10 seconds;
b) Gait: the participants were invited to walk four meters at a normal speed. A score was assigned according to the time obtained by each patient. Four points: <4.82 s, 3 points: 4.82-6.20 s, 2 points: 6.21-8.7 s, 1 point: > 8.7 s and 0 points: participant was unable to complete the test; and
c) Chair test: The participant was invited to get up and sit down from a chair without braces five times, with arms crossed over the chest (44.3 cm high). A score was assigned according to the time the participant took to perform the test. Four points: ≤ 11.19 s, 3 points: 11.20-13.69 s, 2 points: 13.70-16.79 s, 1-point: > 16.70 s and 0 points: the participant was not able to complete the test. The variable was recorded as numerical (0-12), without cut-off points [21].
Barthel index: this is a questionnaire about 10 basic activities of daily life (BADL) (feeding, shower, dressing, use of the toilet, transfer bed-armchair, mobility, use of stairs, toilet, urinary and fecal continence) with a total score ranging 0-100. It was analyzed as a numerical variable [22].
Lawton index: this a questionnaire on eight instrumental activities of daily life (IADL) (telephone use, shopping, preparing food, taking care of the house, means of transport, laundry, medication and use of money). Score from 0 to 8, analyzed as numerical variable [23].
Sociodemographic variables: age in years according to clinical history, sex of the participant according to phenotype and education according to clinical history report.
Comorbidities: a history of depression, arterial hypertension, type 2 diabetes, heart failure and chronic obstructive pulmonary disease were collected when present, from the geriatric clinical histories.
Ethical aspects
The present work has the approval of the Ethics Committee of the Naval Medical Center. We preserved the integrity and fundamental rights of patients subject to research, in accordance with the guidelines of good clinical practice and ethics in biomedical research.
Statistical analysis: The bivariate analysis was performed comparing 2 groups, according to the variable outcome: decrease of the score of Mini Mental State Examination (physiological vs. pathological). Student´s t test was used for the numerical variables and chi2 for the categorical variables. Subsequently, a Cox regression model was developed, including follow-up time, annual functional and cognitive evaluations, adjusting the final model for sociodemographic variables, comorbidities and functional assessment to predict deterioration of cognitive functions according to the Mini Mental State Examination.
Results
We found a mean age of 75.8 years, a greater presence of male participants (50.91%) and participants with complete school studies (60.30%). At the start of follow-up, arterial hypertension was present in 26.67% of patients, type 2 diabetes in 15.45%, chronic obstructive pulmonary disease in 10.90%, heart failure in 8.79% and depression in 30%. Likewise, we obtained an average of Barthel Index’s score of 89.81, of Lawton Index of 5.34, of the Short Physical Performance Battery of 8.63, of the Timed Up & Go Test of 12.73 seconds and an average of the score of the Mini Mental State Examination of 27.73 points. In the bivariate analysis we only included the initial comparison vs. after four years of following for the numerical variables, since the prevalence of sociodemographic variables and pathological backgrounds varied very little and were not the main objective of our study (Table 1).
Table 1 also shows the bivariate analysis regarding the groups with pathological and physiological decrease of the Mini Mental State Examination score. When comparing the mean age and its variation after four years in both study groups, no significant differences were found.
Regarding gender, there is a higher frequency of females in the group with pathological decrease of Mini Mental State Examination score, with statistically significant differences. Similarly results were observed with education, where we see a clear association between poor education and pathological progression of neurocognitive disorders.
Regarding comorbidities, we see a statistically significant association of our response variable with arterial hypertension, type 2 diabetes, heart failure and depression. There is a higher prevalence of these comorbidities in the group with pathological decrease of the Mini Mental State Examination score, except for chronic obstructive pulmonary disease.
Additionally, the averages of the functional scales demonstrate an inadequate physical performance in the group with pathological evolution of the Mini Mental State Examination score, in addition to a marked deterioration after four years of follow-up. Differences were statistically significant for all variables.
After developing a Cox regression model estimate, the hazard ratios (HR) were calculated to compare the risks of suffering a pathological decrease in the Mini Mental State Examination score. As in the bivariate analysis, no differences were found with respect to age, but significant differences were found for sex and educational level, where being female and having low schooling were statistically associated with our outcome variable. In the crude analysis, statistical significance was found for all the variables except for age and chronic obstructive pulmonary disease. Despite this, it was decided to include the variable age in the final model, since it was considered a known confounder. In the multivariate model, with adjusted hazard ratios, we found statistical significance in relation to all covariates except for age, finding that the hazard ratio of having a pathological decrease vs a physiological one in the Mini-Mental State Examination score is 1.73 (95% CI: 1.41 to 1.96), in relation to the Timed Up & Go test expressed in seconds. Additionally, multicollinearity was discarded between the Barthel index, Lawton index, Short Physical Performance Battery and Timed Up & Go test, using the variance inflation factor.
Discussion
The main objective of the study was to determine the relationship between Timed Up & Go test and the progression of neurocognitive disorders. We found that Timed Up & Go test was significantly associated with a pathological decrease in the Mini-Mental State Examination score, taking into account functional assessments, comorbidities and sociodemographic factors in the analysis. We found a significantly higher Timed Up & Go test average score (meaning a poorer physical performance) in the group with pathological decrease in Mini-Mental State Examination score than in the group with physiological decrease after 4 years of follow-up.
In addition, other instruments of functionality in older adults were evaluated, finding an unfavorable evolution for basic activities (Barthel index) and instrumental activities (Lawton index) more pronounced in the pathological decrease group of the Mini-Mental State Examination score. Something similar occurred when evaluating the Short Physical Performance Battery where there was a decrease in the average score in both groups, but more evident in the group with a pathological decrease of the Mini-Mental State Examination score.
A validation study of Timed Up & Go test for predicting falls mentions a close relationship between this test and cognitive problems [11]. However, in studies regarding minimal cognitive impairment, poor performance in Timed Up & Go test was not statistically significant [24]. However, intervention studies with rehabilitation programs show improvements in Timed Up & Go test in patients with cognitive impairment [11], demonstrating that it is a useful tool in monitoring the evolution of this group of patients [18].
In relation to the valuation of activities of daily living, there is evidence that a loss of independence for basic and instrumental activities is associated with cognitive impairment, especially measured by Lawton's score [7]. In this regard, a systematic review concludes that dependence for instrumental activities predicts cognitive impairment, but dependence on basic activities do not [25]. In general, in patients with cognitive impairment, the use of scales to measure basic and instrumental dependencies of daily life is usually recommended, since both help in the evaluation of this category of patients [26], and is also part of the criteria recommended by DSMV (Diagnostic and Statistical Manual of Mental Disorders) [27]. In relation to Short Physical Performance Battery, the consulted literature reveals that there is a worse physical and muscular performance in patients with neurocognitive disorders, mainly in terms of gait evaluation [8],[26],[28]. These findings are consistent with what we found in our analysis.
In our study, we found an association between high blood pressure, type-2 diabetes mellitus, heart failure and depression with a pathological decrease in the Mini-Mental State Examination score. Our results resemble similar publications, where the cited co-morbidities are associated with increased presence, increased risk or greater severity of neurocognitive disorders [1],[29],[30],[31],[32],[33]. In the literature we consulted, we found that most studies determine an association between chronic obstructive pulmonary disease and neurocognitive disorders [34]. However, there is evidence that the association between chronic obstructive pulmonary disease and cognitive impairment may be influenced by inflammatory factors, hypoxemia and depression, as well as co-morbidities, so this association is controversial. On the other hand, a recent study of risk factors for neurocognitive disorders identifies smoking as the most important risk factor and not chronic obstructive pulmonary disease [34].
Additionally, we explored the association with sociodemographic factors and observed an increased risk of neurocognitive disorders in women with a low level of education [35]. In the literature we consulted, age is often a risk factor for cognitive impairment [15], but our results do not match those findings, although there is evidence that in retired military personnel exposed to different lifestyles, the effect of age at risk for cognitive impairment would be controversial [36].
The particularity of the participants included in this study, retired military patients and their families, raises the possibility that our results may not be extrapolated to the general population; in relation to this, we found evidence that retired military personnel, because they have a lifetime financial compensation, have a better quality of life. However, there are articles with similar populations with potentially comparable results with older adult populations in our environment [37]. After an extensive review of the literature, we found that some variables should have been added to the analysis, such as smoking, obesity, dyslipidemia, sleep disorders and physical activity. However, the variables chronic obstructive pulmonary disease and the Short Physical Performance Battery scores were included in the analysis, so there may be an indirect statistical adjustment in relation to tobacco use and physical activity.
Finally, we realize that the average age of our participants is lower than that of similar cognitive impairment studies; this could be due to the fact that our sampling was based on the role of the Peruvian Naval Medical Center and not on a randomization.
Although there are few publications that support Timed Up & Go test [24] role as a predictor of poor evolution of the Mini Mental State Examination score, we have found literature that indicates that a correct intervention in physical matters in patients with cognitive impairment could achieve improvements in Timed Up & Go test [12]
Conclusions
Our results support the hypothesis that Timed Up & Go test values predict the risk of pathological decrease in Mini-Mental State Examination score, regardless of socio-demographic factors, comorbidities, and functional valuation. We recommend studies of intervention in physical activity, sarcopenia, and functionality to reduce the risk of neurocognitive disorders in older adults.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal is aware that the Ethics and Research Committee of the Naval Medical Center was informed about this study and its possible publication in a biomedical journal.
Declaration of conflicts of interest
The authors have completed the ICMJE Conflicts of Interest declaration form, and declare that they have not received funding for the report; have no financial relationships with organizations that might have an interest in the published article in the last three years; and have no other relationships or activities that could influence the published article. Forms can be requested by contacting the author responsible or the editorial management of the Journal.
Financing
The authors state that there were no external sources of funding.
Editor's note
The principal or responsible author asserts that this manuscript is an honest, accurate and transparent transcription of the study being reported; that no important aspects of the study have been omitted; and that discrepancies between the study results and those anticipated (if relevant) have been recorded and explained.

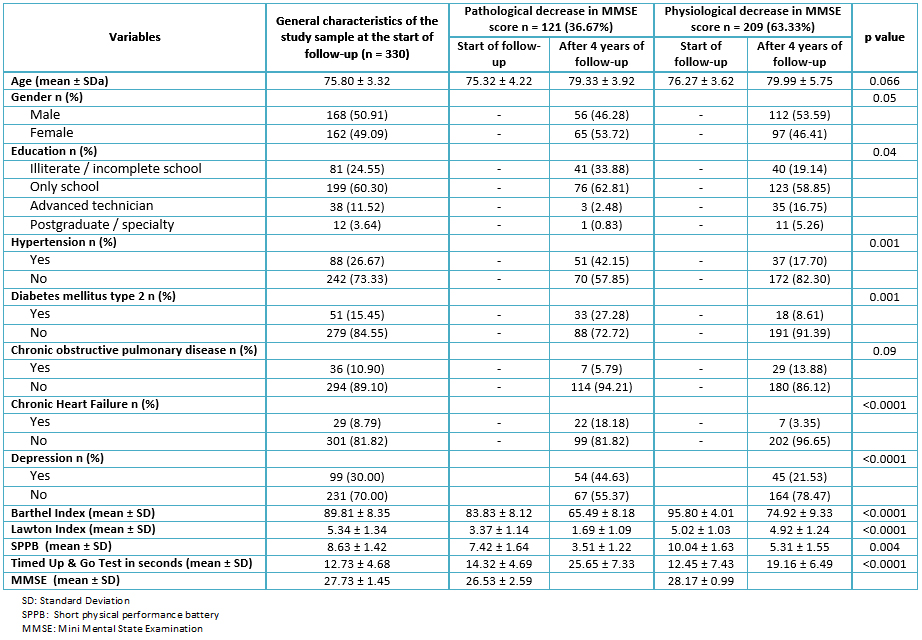 Table 1. Bivariate analysis based on decreased cognitive functions after 4 years of follow-up (n = 330)
Table 1. Bivariate analysis based on decreased cognitive functions after 4 years of follow-up (n = 330)

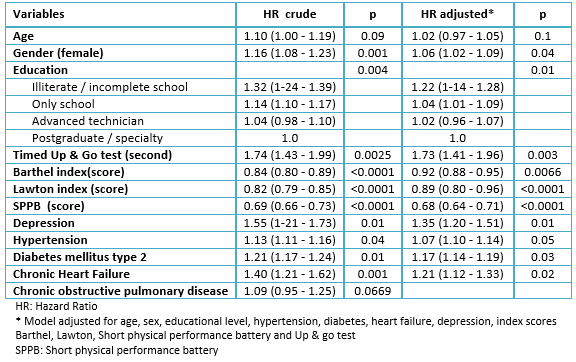 Table 2. Cox Regression for Prediction of Pathological Decrease in Mini Mental State Examination Score (n = 330)
Table 2. Cox Regression for Prediction of Pathological Decrease in Mini Mental State Examination Score (n = 330)
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
Se estima que los trastornos neurocognitivos mayores afectarán a 115,4 millones de personas en 2050, lo que representa una carga financiera importante para la sociedad. Asimismo, la dependencia funcional para actividades básicas o instrumentales de la vida diaria suele ser consecuencia de la mayor prevalencia de patologías discapacitantes, y de la progresiva disminución de la reserva fisiológica propia del envejecimiento.
OBJETIVOS
Se persiguen dos objetivos: determinar la relación entre los test funcionales y la predicción de deterioro de funciones cognitivas en pacientes geriátricos; y establecer qué factores están asociados a disminución de las funciones cognitivas en pacientes geriátricos.
MÉTODOS
Estudio de tipo cohorte retrospectiva. Incluimos participantes que acudieron a los servicios ambulatorios de geriatría del Centro Médico Naval de Perú desde 2010 hasta 2014. Se formaron dos grupos, el primero con los que presentaron pérdida fisiológica de funciones cognitivas, definida como la disminución menor a 4,1 puntos en el puntaje del Mini Mental State Examination durante el seguimiento y otro con una pérdida patológica de funciones cognitivas, definida como la disminución de 4,2 puntos en promedio o más en el puntaje de esta misma encuesta durante el seguimiento. Los pacientes fueron seguidos por cuatro años, período en el que se les efectuaron evaluaciones funcionales y se recogieron datos de comorbilidades y factores sociodemográficos.
RESULTADOS
Se incluyeron 368 pacientes, cuya media de edad fue de 75,8 años y 50,91% fueron hombres. El género femenino (53,72%), la presencia de un bajo grado de instrucción (62,81%) y la presencia de comorbilidades fueron más prevalentes en el grupo con disminución de Mini Mental State Examination patológico. Las variables de evaluación funcional, incluyendo al Timed Up & Go Test, presentaron promedios inadecuados durante el seguimiento de cuatro años en el grupo con evolución patológica del puntaje del Mini Mental State Examination, en comparación con el grupo sano.
CONCLUSIONES
Los valores del puntaje del Timed Up & Go Test logran predecir el riesgo de una disminución patológica del Mini Mental State Examination, independientemente de factores sociodemográficos, comorbilidades y valoración funcional.
 Authors:
Gustavo Alberto Sandival Ampuero[1], Fernando M. Runzer-Colmenares[2,3], José F. Parodi[2]
Authors:
Gustavo Alberto Sandival Ampuero[1], Fernando M. Runzer-Colmenares[2,3], José F. Parodi[2]
Affiliation:
[1] Facultad de Medicina Humana, Universidad Nacional Federico Villarreal, Lima, Perú
[2] Centro de Investigación del Envejecimiento (CIEN), Facultad de Medicina Humana, Universidad de San Martin de Porres, Lima, Perú
[3] Unidad de geriatría, Centro Médico Naval, Callao, Perú
E-mail: gsandival19@gmail.com
Author address:
[1] Avenida Garcia Villon Manzana c6
Lote 7, Cercado de Lima
Lima
Perú

Citation: Sandival Ampuero GA, Runzer-Colmenares FM, Parodi JF. Functional assessment as a predictor of cognitive impairment: a retrospective cohort study. Medwave 2017 Nov-Dic;17(9):e7099 doi: 10.5867/medwave.2017.09.7099
Submission date: 3/6/2017
Acceptance date: 9/11/2017
Publication date: 12/12/2017
Origin: not requested
Type of review: reviewed by five external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003 Feb;51(2):169-77. | PubMed |
- Duthey B, Background Paper 6,11 Alzheimer Disease and other Dementias. Update on 2004. Who. 2013;(February):1-77. | Link |
- Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013 Apr 4;368(14):1326-34. | CrossRef | PubMed |
- Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189-98. | PubMed |
- Biundo R, Weis L, Bostantjopoulou S, Stefanova E, Falup-Pecurariu C, Kramberger MG, et al. MMSE and MoCA in Parkinson's disease and dementia with Lewy bodies: a multicenter 1-year follow-up study. J Neural Transm (Vienna). 2016 Apr;123(4):431-8. | CrossRef | PubMed |
- Reig-Ferrer A, Cabrero-García J, Lizán Tudela L. [Assessment of functional capacity, psychological well-being and mental health in primary care]. Aten Primaria. 2009 Sep;41(9):515-9. | CrossRef | PubMed |
- Jefferson AL, Byerly LK, Vanderhill S, Lambe S, Wong S, Ozonoff A, et al. Characterization of activities of daily living in individuals with mild cognitive impairment. Am J Geriatr Psychiatry. 2008 May;16(5):375-83. | CrossRef | PubMed |
- McGough EL, Logsdon RG, Kelly VE, Teri L. Functional mobility limitations and falls in assisted living residents with dementia: physical performance assessment and quantitative gait analysis. J Geriatr Phys Ther. 2013 Apr-Jun;36(2):78-86. | CrossRef | PubMed |
- Inzitari M, Calle A, Esteve A, Casas Á, Torrents N, Martínez N. [Do you measure gait speed in your daily clinical practice? A review]. Rev Esp Geriatr Gerontol. 2017 Jan - Feb;52(1):35-43. | CrossRef | PubMed |
- Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016 Dec 22;14(1):215. | CrossRef | PubMed |
- Schoene D, Wu SM, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, Lord SR. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013 Feb;61(2):202-8. | CrossRef | PubMed |
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994 Mar;49(2):M85-94. | PubMed |
- Quan M, Xun P, Chen C, Wen J, Wang Y, Wang R, et al. Walking Pace and the Risk of Cognitive Decline and Dementia in Elderly Populations: A Meta-analysis of Prospective Cohort Studies. J Gerontol A Biol Sci Med Sci. 2017 Feb;72(2):266-270. | CrossRef | PubMed |
- Beauchet O, Annweiler C, Callisaya ML, De Cock AM, Helbostad JL, Kressig RW, et al. Poor Gait Performance and Prediction of Dementia: Results From a Meta-Analysis. J Am Med Dir Assoc. 2016 Jun 1;17(6):482-90. | CrossRef | PubMed |
- Jacqmin-Gadda H, Fabrigoule C, Commenges D, Dartigues JF. A 5-year longitudinal study of the Mini-Mental State Examination in normal aging. Am J Epidemiol. 1997 Mar 15;145(6):498-506. | PubMed |
- Burns A, Jacoby R, Levy R. Progression of cognitive impairment in Alzheimer's disease. J Am Geriatr Soc. 1991 Jan;39(1):39-45. | PubMed |
- Runzer-Colmenares FM, Samper-Ternent R, Al Snih S, Ottenbacher KJ, Parodi JF, Wong R. Prevalence and factors associated with frailty among Peruvian older adults. Arch Gerontol Geriatr. 2014 Jan-Feb;58(1):69-73. | CrossRef | PubMed |
- Thomas VS, Hageman PA. Can neuromuscular strength and function in people with dementia be rehabilitated using resistance-exercise training? Results from a preliminary intervention study. J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):746-51. | PubMed |
- Custodio N, Montesinos R, Escobar J. Prevalencia de demencia en una población urbana de Lima-Perú : estudio puerta a puerta Dementia prevalence in a Lima . Peru urban community : door-to-door study. 2008;69(4):233–8. | Link |
- Lin MR, Hwang HF, Hu MH, Wu HD, Wang YW, Huang FC. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004 Aug;52(8):1343-8. | PubMed |
- Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):728-33. | PubMed |
- Millán-Calenti JC, Tubío J, Pita-Fernández S, González-Abraldes I, Lorenzo T, Fernández-Arruty T, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010 May-Jun;50(3):306-10. | CrossRef | PubMed |
- Lund R, Nilsson CJ, Avlund K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing. 2010 May;39(3):319-26. | CrossRef | PubMed |
- Mirelman A, Weiss A, Buchman AS, Bennett DA, Giladi N, Hausdorff JM. Association between performance on Timed Up and Go subtasks and mild cognitive impairment: further insights into the links between cognitive and motor function. J Am Geriatr Soc. 2014 Apr;62(4):673-8. | CrossRef | PubMed |
- Mariani E, Monastero R, Mecocci P. Mild cognitive impairment: a systematic review. J Alzheimers Dis. 2007 Aug;12(1):23-35. | PubMed |
- Jean L, Bergeron ME, Thivierge S, Simard M. Cognitive intervention programs for individuals with mild cognitive impairment: systematic review of the literature. Am J Geriatr Psychiatry. 2010 Apr;18(4):281-96. | CrossRef | PubMed |
- Narrow WE, Clarke DE, Kuramoto SJ, Kraemer HC, Kupfer DJ, Greiner L, et al. DSM-5 field trials in the United States and Canada, Part III: development and reliability testing of a cross-cutting symptom assessment for DSM-5. Am J Psychiatry. 2013 Jan;170(1):71-82. | CrossRef | PubMed |
- Cobo CMS, Pérez V, Hermosilla C, Nuñez MJ, Lorena P De. Prevalence of Sarcopenia in Elderly With Dementia Institutionalized : a Multicenter Study. J Aging Res Clin Pract. 2015;2040(12):24-7. | Link |
- Qiu C, Winblad B, Marengoni A, Klarin I, Fastbom J, Fratiglioni L. Heart failure and risk of dementia and Alzheimer disease: a population-based cohort study. Arch Intern Med. 2006 May 8;166(9):1003-8. | PubMed |
- Formiga F, Fort I, Robles MJ, Riu S, Sabartes O, Barranco E, et al. Comorbidity and clinical features in elderly patients with dementia: differences according to dementia severity. J Nutr Health Aging. 2009 May;13(5):423-7. | PubMed |
- Sharp SI, Aarsland D, Day S, Sønnesyn H; Alzheimer's Society Vascular Dementia Systematic Review Group, Ballard C. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011 Jul;26(7):661-9. | CrossRef | PubMed |
- Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012 May;42(5):484-91. | CrossRef | PubMed |
- Buntinx F, Kester A, Bergers J, Knottnerus JA. Is depression in elderly people followed by dementia? A retrospective cohort study based in general practice. Age Ageing. 1996 May;25(3):231-3. | PubMed |
- Singh B, Parsaik AK, Mielke MM, Roberts RO, Scanlon PD, Geda YE, et al. Chronic obstructive pulmonary disease and association with mild cognitive impairment: the Mayo Clinic Study of Aging. Mayo Clin Proc. 2013 Nov;88(11):1222-30. | CrossRef | PubMed |
- Schoenhofen E, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011 Oct-Dec;25(4):289-304. | CrossRef | PubMed |
- Mueller SG, Schuff N, Yaffe K, Madison C, Miller B, Weiner MW. Hippocampal atrophy patterns in mild cognitive impairment and Alzheimer's disease. Hum Brain Mapp. 2010 Sep;31(9):1339-47. | CrossRef | PubMed |
- Rosenheck RA, Dausey DJ, Frisman L, Kasprow W. Outcomes after initial receipt of social security benefits among homeless veterans with mental illness. Psychiatr Serv. 2000 Dec;51(12):1549-54. | PubMed |
 Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003 Feb;51(2):169-77. | PubMed |
Haan MN, Mungas DM, Gonzalez HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older latinos: the influence of type 2 diabetes mellitus, stroke and genetic factors. J Am Geriatr Soc. 2003 Feb;51(2):169-77. | PubMed | Duthey B, Background Paper 6,11 Alzheimer Disease and other Dementias. Update on 2004. Who. 2013;(February):1-77. | Link |
Duthey B, Background Paper 6,11 Alzheimer Disease and other Dementias. Update on 2004. Who. 2013;(February):1-77. | Link | Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013 Apr 4;368(14):1326-34. | CrossRef | PubMed |
Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. N Engl J Med. 2013 Apr 4;368(14):1326-34. | CrossRef | PubMed | Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189-98. | PubMed |
Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975 Nov;12(3):189-98. | PubMed | Biundo R, Weis L, Bostantjopoulou S, Stefanova E, Falup-Pecurariu C, Kramberger MG, et al. MMSE and MoCA in Parkinson's disease and dementia with Lewy bodies: a multicenter 1-year follow-up study. J Neural Transm (Vienna). 2016 Apr;123(4):431-8. | CrossRef | PubMed |
Biundo R, Weis L, Bostantjopoulou S, Stefanova E, Falup-Pecurariu C, Kramberger MG, et al. MMSE and MoCA in Parkinson's disease and dementia with Lewy bodies: a multicenter 1-year follow-up study. J Neural Transm (Vienna). 2016 Apr;123(4):431-8. | CrossRef | PubMed | Reig-Ferrer A, Cabrero-García J, Lizán Tudela L. [Assessment of functional capacity, psychological well-being and mental health in primary care]. Aten Primaria. 2009 Sep;41(9):515-9. | CrossRef | PubMed |
Reig-Ferrer A, Cabrero-García J, Lizán Tudela L. [Assessment of functional capacity, psychological well-being and mental health in primary care]. Aten Primaria. 2009 Sep;41(9):515-9. | CrossRef | PubMed | Jefferson AL, Byerly LK, Vanderhill S, Lambe S, Wong S, Ozonoff A, et al. Characterization of activities of daily living in individuals with mild cognitive impairment. Am J Geriatr Psychiatry. 2008 May;16(5):375-83. | CrossRef | PubMed |
Jefferson AL, Byerly LK, Vanderhill S, Lambe S, Wong S, Ozonoff A, et al. Characterization of activities of daily living in individuals with mild cognitive impairment. Am J Geriatr Psychiatry. 2008 May;16(5):375-83. | CrossRef | PubMed | McGough EL, Logsdon RG, Kelly VE, Teri L. Functional mobility limitations and falls in assisted living residents with dementia: physical performance assessment and quantitative gait analysis. J Geriatr Phys Ther. 2013 Apr-Jun;36(2):78-86. | CrossRef | PubMed |
McGough EL, Logsdon RG, Kelly VE, Teri L. Functional mobility limitations and falls in assisted living residents with dementia: physical performance assessment and quantitative gait analysis. J Geriatr Phys Ther. 2013 Apr-Jun;36(2):78-86. | CrossRef | PubMed | Inzitari M, Calle A, Esteve A, Casas Á, Torrents N, Martínez N. [Do you measure gait speed in your daily clinical practice? A review]. Rev Esp Geriatr Gerontol. 2017 Jan - Feb;52(1):35-43. | CrossRef | PubMed |
Inzitari M, Calle A, Esteve A, Casas Á, Torrents N, Martínez N. [Do you measure gait speed in your daily clinical practice? A review]. Rev Esp Geriatr Gerontol. 2017 Jan - Feb;52(1):35-43. | CrossRef | PubMed | Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016 Dec 22;14(1):215. | CrossRef | PubMed |
Pavasini R, Guralnik J, Brown JC, di Bari M, Cesari M, Landi F, et al. Short Physical Performance Battery and all-cause mortality: systematic review and meta-analysis. BMC Med. 2016 Dec 22;14(1):215. | CrossRef | PubMed | Schoene D, Wu SM, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, Lord SR. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013 Feb;61(2):202-8. | CrossRef | PubMed |
Schoene D, Wu SM, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, Lord SR. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013 Feb;61(2):202-8. | CrossRef | PubMed | Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994 Mar;49(2):M85-94. | PubMed |
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994 Mar;49(2):M85-94. | PubMed | Quan M, Xun P, Chen C, Wen J, Wang Y, Wang R, et al. Walking Pace and the Risk of Cognitive Decline and Dementia in Elderly Populations: A Meta-analysis of Prospective Cohort Studies. J Gerontol A Biol Sci Med Sci. 2017 Feb;72(2):266-270. | CrossRef | PubMed |
Quan M, Xun P, Chen C, Wen J, Wang Y, Wang R, et al. Walking Pace and the Risk of Cognitive Decline and Dementia in Elderly Populations: A Meta-analysis of Prospective Cohort Studies. J Gerontol A Biol Sci Med Sci. 2017 Feb;72(2):266-270. | CrossRef | PubMed | Beauchet O, Annweiler C, Callisaya ML, De Cock AM, Helbostad JL, Kressig RW, et al. Poor Gait Performance and Prediction of Dementia: Results From a Meta-Analysis. J Am Med Dir Assoc. 2016 Jun 1;17(6):482-90. | CrossRef | PubMed |
Beauchet O, Annweiler C, Callisaya ML, De Cock AM, Helbostad JL, Kressig RW, et al. Poor Gait Performance and Prediction of Dementia: Results From a Meta-Analysis. J Am Med Dir Assoc. 2016 Jun 1;17(6):482-90. | CrossRef | PubMed | Jacqmin-Gadda H, Fabrigoule C, Commenges D, Dartigues JF. A 5-year longitudinal study of the Mini-Mental State Examination in normal aging. Am J Epidemiol. 1997 Mar 15;145(6):498-506. | PubMed |
Jacqmin-Gadda H, Fabrigoule C, Commenges D, Dartigues JF. A 5-year longitudinal study of the Mini-Mental State Examination in normal aging. Am J Epidemiol. 1997 Mar 15;145(6):498-506. | PubMed | Burns A, Jacoby R, Levy R. Progression of cognitive impairment in Alzheimer's disease. J Am Geriatr Soc. 1991 Jan;39(1):39-45. | PubMed |
Burns A, Jacoby R, Levy R. Progression of cognitive impairment in Alzheimer's disease. J Am Geriatr Soc. 1991 Jan;39(1):39-45. | PubMed | Runzer-Colmenares FM, Samper-Ternent R, Al Snih S, Ottenbacher KJ, Parodi JF, Wong R. Prevalence and factors associated with frailty among Peruvian older adults. Arch Gerontol Geriatr. 2014 Jan-Feb;58(1):69-73. | CrossRef | PubMed |
Runzer-Colmenares FM, Samper-Ternent R, Al Snih S, Ottenbacher KJ, Parodi JF, Wong R. Prevalence and factors associated with frailty among Peruvian older adults. Arch Gerontol Geriatr. 2014 Jan-Feb;58(1):69-73. | CrossRef | PubMed | Thomas VS, Hageman PA. Can neuromuscular strength and function in people with dementia be rehabilitated using resistance-exercise training? Results from a preliminary intervention study. J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):746-51. | PubMed |
Thomas VS, Hageman PA. Can neuromuscular strength and function in people with dementia be rehabilitated using resistance-exercise training? Results from a preliminary intervention study. J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):746-51. | PubMed | Custodio N, Montesinos R, Escobar J. Prevalencia de demencia en una población urbana de Lima-Perú : estudio puerta a puerta Dementia prevalence in a Lima . Peru urban community : door-to-door study. 2008;69(4):233–8. | Link |
Custodio N, Montesinos R, Escobar J. Prevalencia de demencia en una población urbana de Lima-Perú : estudio puerta a puerta Dementia prevalence in a Lima . Peru urban community : door-to-door study. 2008;69(4):233–8. | Link | Lin MR, Hwang HF, Hu MH, Wu HD, Wang YW, Huang FC. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004 Aug;52(8):1343-8. | PubMed |
Lin MR, Hwang HF, Hu MH, Wu HD, Wang YW, Huang FC. Psychometric comparisons of the timed up and go, one-leg stand, functional reach, and Tinetti balance measures in community-dwelling older people. J Am Geriatr Soc. 2004 Aug;52(8):1343-8. | PubMed | Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):728-33. | PubMed |
Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003 Aug;58(8):728-33. | PubMed | Millán-Calenti JC, Tubío J, Pita-Fernández S, González-Abraldes I, Lorenzo T, Fernández-Arruty T, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010 May-Jun;50(3):306-10. | CrossRef | PubMed |
Millán-Calenti JC, Tubío J, Pita-Fernández S, González-Abraldes I, Lorenzo T, Fernández-Arruty T, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010 May-Jun;50(3):306-10. | CrossRef | PubMed | Lund R, Nilsson CJ, Avlund K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing. 2010 May;39(3):319-26. | CrossRef | PubMed |
Lund R, Nilsson CJ, Avlund K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing. 2010 May;39(3):319-26. | CrossRef | PubMed | Mirelman A, Weiss A, Buchman AS, Bennett DA, Giladi N, Hausdorff JM. Association between performance on Timed Up and Go subtasks and mild cognitive impairment: further insights into the links between cognitive and motor function. J Am Geriatr Soc. 2014 Apr;62(4):673-8. | CrossRef | PubMed |
Mirelman A, Weiss A, Buchman AS, Bennett DA, Giladi N, Hausdorff JM. Association between performance on Timed Up and Go subtasks and mild cognitive impairment: further insights into the links between cognitive and motor function. J Am Geriatr Soc. 2014 Apr;62(4):673-8. | CrossRef | PubMed | Mariani E, Monastero R, Mecocci P. Mild cognitive impairment: a systematic review. J Alzheimers Dis. 2007 Aug;12(1):23-35. | PubMed |
Mariani E, Monastero R, Mecocci P. Mild cognitive impairment: a systematic review. J Alzheimers Dis. 2007 Aug;12(1):23-35. | PubMed | Jean L, Bergeron ME, Thivierge S, Simard M. Cognitive intervention programs for individuals with mild cognitive impairment: systematic review of the literature. Am J Geriatr Psychiatry. 2010 Apr;18(4):281-96. | CrossRef | PubMed |
Jean L, Bergeron ME, Thivierge S, Simard M. Cognitive intervention programs for individuals with mild cognitive impairment: systematic review of the literature. Am J Geriatr Psychiatry. 2010 Apr;18(4):281-96. | CrossRef | PubMed | Narrow WE, Clarke DE, Kuramoto SJ, Kraemer HC, Kupfer DJ, Greiner L, et al. DSM-5 field trials in the United States and Canada, Part III: development and reliability testing of a cross-cutting symptom assessment for DSM-5. Am J Psychiatry. 2013 Jan;170(1):71-82. | CrossRef | PubMed |
Narrow WE, Clarke DE, Kuramoto SJ, Kraemer HC, Kupfer DJ, Greiner L, et al. DSM-5 field trials in the United States and Canada, Part III: development and reliability testing of a cross-cutting symptom assessment for DSM-5. Am J Psychiatry. 2013 Jan;170(1):71-82. | CrossRef | PubMed | Cobo CMS, Pérez V, Hermosilla C, Nuñez MJ, Lorena P De. Prevalence of Sarcopenia in Elderly With Dementia Institutionalized : a Multicenter Study. J Aging Res Clin Pract. 2015;2040(12):24-7. | Link |
Cobo CMS, Pérez V, Hermosilla C, Nuñez MJ, Lorena P De. Prevalence of Sarcopenia in Elderly With Dementia Institutionalized : a Multicenter Study. J Aging Res Clin Pract. 2015;2040(12):24-7. | Link | Qiu C, Winblad B, Marengoni A, Klarin I, Fastbom J, Fratiglioni L. Heart failure and risk of dementia and Alzheimer disease: a population-based cohort study. Arch Intern Med. 2006 May 8;166(9):1003-8. | PubMed |
Qiu C, Winblad B, Marengoni A, Klarin I, Fastbom J, Fratiglioni L. Heart failure and risk of dementia and Alzheimer disease: a population-based cohort study. Arch Intern Med. 2006 May 8;166(9):1003-8. | PubMed | Formiga F, Fort I, Robles MJ, Riu S, Sabartes O, Barranco E, et al. Comorbidity and clinical features in elderly patients with dementia: differences according to dementia severity. J Nutr Health Aging. 2009 May;13(5):423-7. | PubMed |
Formiga F, Fort I, Robles MJ, Riu S, Sabartes O, Barranco E, et al. Comorbidity and clinical features in elderly patients with dementia: differences according to dementia severity. J Nutr Health Aging. 2009 May;13(5):423-7. | PubMed | Sharp SI, Aarsland D, Day S, Sønnesyn H; Alzheimer's Society Vascular Dementia Systematic Review Group, Ballard C. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011 Jul;26(7):661-9. | CrossRef | PubMed |
Sharp SI, Aarsland D, Day S, Sønnesyn H; Alzheimer's Society Vascular Dementia Systematic Review Group, Ballard C. Hypertension is a potential risk factor for vascular dementia: systematic review. Int J Geriatr Psychiatry. 2011 Jul;26(7):661-9. | CrossRef | PubMed | Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012 May;42(5):484-91. | CrossRef | PubMed |
Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012 May;42(5):484-91. | CrossRef | PubMed | Buntinx F, Kester A, Bergers J, Knottnerus JA. Is depression in elderly people followed by dementia? A retrospective cohort study based in general practice. Age Ageing. 1996 May;25(3):231-3. | PubMed |
Buntinx F, Kester A, Bergers J, Knottnerus JA. Is depression in elderly people followed by dementia? A retrospective cohort study based in general practice. Age Ageing. 1996 May;25(3):231-3. | PubMed | Singh B, Parsaik AK, Mielke MM, Roberts RO, Scanlon PD, Geda YE, et al. Chronic obstructive pulmonary disease and association with mild cognitive impairment: the Mayo Clinic Study of Aging. Mayo Clin Proc. 2013 Nov;88(11):1222-30. | CrossRef | PubMed |
Singh B, Parsaik AK, Mielke MM, Roberts RO, Scanlon PD, Geda YE, et al. Chronic obstructive pulmonary disease and association with mild cognitive impairment: the Mayo Clinic Study of Aging. Mayo Clin Proc. 2013 Nov;88(11):1222-30. | CrossRef | PubMed | Schoenhofen E, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011 Oct-Dec;25(4):289-304. | CrossRef | PubMed |
Schoenhofen E, Gatz M. Relationship between education and dementia: an updated systematic review. Alzheimer Dis Assoc Disord. 2011 Oct-Dec;25(4):289-304. | CrossRef | PubMed | Mueller SG, Schuff N, Yaffe K, Madison C, Miller B, Weiner MW. Hippocampal atrophy patterns in mild cognitive impairment and Alzheimer's disease. Hum Brain Mapp. 2010 Sep;31(9):1339-47. | CrossRef | PubMed |
Mueller SG, Schuff N, Yaffe K, Madison C, Miller B, Weiner MW. Hippocampal atrophy patterns in mild cognitive impairment and Alzheimer's disease. Hum Brain Mapp. 2010 Sep;31(9):1339-47. | CrossRef | PubMed | Rosenheck RA, Dausey DJ, Frisman L, Kasprow W. Outcomes after initial receipt of social security benefits among homeless veterans with mental illness. Psychiatr Serv. 2000 Dec;51(12):1549-54. | PubMed |
Rosenheck RA, Dausey DJ, Frisman L, Kasprow W. Outcomes after initial receipt of social security benefits among homeless veterans with mental illness. Psychiatr Serv. 2000 Dec;51(12):1549-54. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








