Key Words: breastfeeding, knowledge, healthcare providers
Abstract
INTRODUCTION
Healthcare provider’s knowledge has been identified as a factor associated with clinical practice skills and exclusive breastfeeding prevalence.
OBJECTIVES
To evaluate the level of knowledge and training in breastfeeding of healthcare provider’s that work in family healthcare centers of Maipu, Chile, (midwifes, physicians, nurses and nutritionists). To determine association among level of knowledge, profession and breastfeeding training.
METHODS
Quantitative, cross-sectional, analytical study. Participants were healthcare professionals regularly participating in healthy child exams of six month old babies. We used a validated survey based on the “Ten steps for successful breastfeeding”. Statistical analyses included frequencies, percentages, measures of central tendency as well as the association among level of knowledge, profession and training in breastfeeding.
RESULTS
Results showed that of the total number of participants (n=78), 42.2% classified as “average”, 3.8% as “poor” and near 50% as “good” or “very good” knowledge. Nutritionists obtained the best scores in knowledge about breastfeeding with 50% of “very good”, followed by nurses and midwifes, with 39% and 35% respectively. On the other hand, most physicians obtained “good” (65.4%) and only 7.7% “very good”. Only 33% had had breastfeeding training at some point of their lives, and 6.4% had had one training session in the last year. We highlight that 34.6 to 42.3% of those who obtained “good” and “very good” scores had had breastfeeding training. Knowledge level was directly associated with breastfeeding training (p=0.033) and healthcare profession (p=0.019).
CONCLUSION
Healthcare professionals have different levels of breastfeeding knowledge. Breastfeeding training sessions significantly increase knowledge, which could improve breastfeeding prevalence.
Introduction
Maternal breastfeeding is one of the most promoted public health actions worldwide, in part because its practice promotes the health and well-being of the mother-child dyad [1],[2]. Exclusive breastfeeding is defined as the single intake of breast milk, without associated liquid or solids, except for the administration of oral rehydration solutions or vitamins, minerals or drugs in the form of drops or syrups [3]. The World Health Organization (WHO) recommends the start of exclusive breastfeeding from the first hours of life up to six months [4].
In 1990, the Baby-friendly Hospital Initiative (BFHI) and the Ten Steps to Successful Breastfeeding were established through the Innocenti Declaration, product of the joint work between WHO and UNICEF in Florence. The following strategies aim to promote early breastfeeding and to ensure compliance with international marketing codes for breastmilk substitutes in all maternity services [5]:
- Have a written policy on breastfeeding that is systematically brought to the attention of all health personnel.
- Train all hospital staff so that they are able to implement the aforementioned policy.
- Inform all pregnant women about the benefits of breastfeeding and how to put it into practice.
- Help mothers initiate breastfeeding within a half-hour of birth.
- Show mothers how to breastfeed and how to keep breastfeeding, even if they if they should be separated from their children.
- Do not give newborns anything but breast milk, without other food or drink, unless medically indicated
- Promote the establishment of a 24 hours shared room for the mother and her child.
- Encourage breastfeeding on demand.
- Do not give pacifiers to breastfed babies.
- Encourage the establishment of breastfeeding support groups and ensure mothers are contacted by them once they leave the hospital.
Globally, less than 40% of infants under six months of age receive exclusive breastfeeding, with a similar figure reporting in Latin America and the Caribbean (38%).
In Chile, the trend of exclusive breastfeeding in the sixth month of life has been increasing, from 16% in 1993, 46% in 2005 and 56.3% in 2013 [6]. However, despite this, there are still sectors with prevalence below the currently established target, especially in Maipú with one of the lowest prevalences of the Central Metropolitan Health Service (29.3%) [7].
From 1993 to 1997, Chile implemented a program at the Barros Lucco Trudeau Hospital, which included the diagnosis of breastfeeding practices, and systematic theoretical-practical training of health personnel. At the end of the program, a higher prevalence of exclusive breastfeeding was evidenced at the sixth month (1993: 47% versus 1997: 65%) as well as a decrease in costs in neonatology [8]. Currently in Chile, following the recommendations of the World Health Organization (WHO) and the United Nations International Children's Emergency Fund (UNICEF), the Health Department of Maipú has developed an annual training program in breastfeeding provided by the Central Metropolitan Health Service. Its objective is to advise health professionals to support mothers during the lactation period and to overcome problems derived from it (40 hours course), and also give advice for infant and small child feeding (five days course) [5],[9],[10]. The quotas are competitive among the different professionals and there is only one available spot for each health center, that is, five trained professionals per year.
Since breastfeeding education is one of the most important factors in achieving its success, and considering that Maipú has one of the lowest prevalences of breastfeeding at the national level, the objectives of this study were: to assess the level of knowledge in breastfeeding of professionals who participate in the healthy child control in the Family Health Centers (CESFAM) of Maipú (midwife, physician, nurse, nutritionist) and determine if there is any association between the level of knowledge in breastfeeding, the profession, and the presence or absence of breastfeeding training that professionals had at the time of the survey.
Methods
Quantitative, cross-sectional, analytical study. Participants were the professionals involved in the health check-up of the child until the sixth month of life: midwives, doctors, nurses and nutritionists, in the municipal Family Health Centers of Maipú. All participating physicians were general practitioners. In order to avoid duplication of responses, professionals working in more than one Family Health Center in Maipú were excluded.
The level of knowledge in breastfeeding was measured through a survey based on the "Ten Steps to Successful Breastfeeding" which has been used in previous studies [11],[12],[13]. The survey consists of 22 questions assessing the level of knowledge based on the percentage of correct answers (Table1).
Table 1. Level of knowledge in breastfeeding according to survey.
The first part includes work and personal background information such as: CESFAM in which the professional works at the time of the survey, sex, age, profession, years of work experience, seniority at CESFAM and training in breastfeeding.
The following are the questions evaluating knowledge in breastfeeding:
Multiple choice questions
- The amount of milk a woman is able to produce depends on:
- What advice would you give to the nursing mother who is breastfeeding and has to go to work after her post-natal rest, on how to feed her child?
- According to your criterion, the nursing mother should interrupt breastfeeding when she has:
- At how many months would you say a mother has to complete the weaning?
- Until what age do you consider that a child of a good nourished mother should be breastfed?
- Until what age do you consider that a child from a malnourished mother should be breastfed?
- Indicate which of these institutional practices promotes breastfeeding the most
- When is it proper to give formula to newborns?
Questions with answer yes / no / does not know
- Have you heard about the Baby-friendly Hospitals?
- Should the first intake of breast milk be immediately after delivery?
- Should the mother breastfeed every time the baby asks for it?
- Do you know the benefits that the Labor Code gives to working women who breastfeed?
- Have you had or known about any written communication about breastfeeding protection, promotion and support to breastfeeding?
- Have you received training on breastfeeding in the past year?
- Do baby bottles interfere with and make breastfeeding more difficult?
- Does the mother's emotion and stress negatively influence her milk production capacity?
- Is it important for the new-born to take colostrum?
- Will the mother produce more milk the more the infant sucks?
- Do breastfed children gain more weight than children who are fed with breast milk substitutes?
- Should the mother who is breastfeeding give the other foods first and then the breast?
- Is it preferable that weaning occurs abruptly?
- Does your health centre have educational activities for postpartum breastfeeding mothers?
The study was approved by the health department of Maipú, and the Ethics Committee of Universidad del Desarrollo – Clínica Alemana.
Data collection was done by the researcher, through interviews with each professional who agreed to participate in the study, signing an informed consent, which guaranteed the confidentiality and privacy of information, and emphasized voluntary participation. Data were entered into an Excel spreadsheet and subsequently the SPSS version 21 program [14] was used for statistical analysis.
To characterize the professionals surveyed, a descriptive analysis was carried out using percentages for the following variables: CESFAM in which the professional works, sex, profession; and means for the variables age and years of work experience. Frequency tables were used to determine the level of knowledge according to the proportion of correct answers for each profession in the survey.
The chi-square statistical test was applied to assess the association between level of knowledge and the variables profession and training status of professionals in breastfeeding. Statistical significance level was 0.05.
Results
In the five family health centers of Maipú there are 106 professionals who participate in the control of the child up to six months. Of these, 86 met the inclusion / exclusion criteria. The response rate was 90.6% (n = 78). Of the 78 surveys, 23% (n = 18) were performed at CESFAM Carlos Godoy, 23% (n = 18) in Dr. Iván Insunza, 22% (n = 17) in Dr. Clotario Blest, 15% (n = 12) in Dr. Luis Ferrada and 17% (n = 13) in President Michelle Bachelet.
The mean age of the participants was 35 years ± 7.7 with 76% women (n = 59). The professionals had an average of 9± 6.6 years of work experience, with the physicians having the lowest mean and the nurses the highest mean, with 7 and 12 years respectively. The proportion of participants for each of the professions are shown in Figure1.
Figure 1. Percentage distribution of professionals surveyed.
Level of knowledge, profession and training status
Overall, the results of the survey on level of knowledge in breastfeeding based on the "Ten Steps to Successful Breastfeeding", describe that the majority of professionals (42.2%) achieved a "average" qualification, followed by 29.5% "very good", 24.4% "good" and 3.8% "bad".
Regarding the level of knowledge of professionals, the most outstanding are the nutritionists, who have the highest percentage of "good" and "very good" qualifications (71.4%), followed by a professional midwife with a 70%, and professional nurse with a 66.7% for both qualifications. Medical professionals qualifications were mainly concentrated in the concept of "average" (65.4%), doubling the results obtained by the other professionals in the same concept (Figure 2).
Figure 2. Percentage distribution of concept of qualification, according to profession.
Regarding training, 66.7% of the surveyed professionals reported not having received formal training in breastfeeding since their graduation and 33.3% (n = 26) had at least one training session in breastfeeding. It should be noted that only five professionals (6.4%) reported having received training in breastfeeding in the last year. The professionals who participated most in breastfeeding training were nutritionists (57.1%), followed by midwives (45%), nurses (33.3%), and finally physicians (11.5% %). Of the trained professionals, 76.9% obtained a level of knowledge categorized as "good" and "very good", while those not trained only 42.3% (Table 2). Statistical analysis shows that there is an association between level of knowledge and profession (p = 0.019) and between the level of knowledge and training in breastfeeding (p = 0.033).
Table 2. Concept of qualification, according to training.
Discussion
The present study demonstrates that the different health professionals who work in the family health centers of Maipú have different levels of knowledge in breastfeeding, which could be explained by different curricular structures of the training grids in undergraduate training. Although breastfeeding is a cross-cutting issue in health care, this is not reflected in the basic training of the careers involved in the care of the mother-child dyad. The higher level of knowledge in breastfeeding found in nutritionists and midwives could be explained because during their formation these contents are addressed in greater depth and extension than in other professionals, since they are directly related to the specialized competencies required for the development of the profession such as nutrition and childcare, respectively.
Although nutritionists and midwives have a high average knowledge (“good” or “very good”), it is higher in those cases who have taken breastfeeding courses as well as in the other professionals surveyed. Thus, the results obtained, support the importance of training in this subject, pointing out that one of the most successful interventions to promote breastfeeding and its maintenance over time is the support of professionals towards the dyad [9],[15].
There are several trainings designed with variable duration times nationally and internationally; the most recommended is the one prepared by WHO - UNICEF and the "Initiative Hospital Friend of the Child and the Mother", however the training received by professionals of Maipú, has been limited to the one that the health service to which they belong imparts and which is carried out only once a year. On the other hand, the practice of replicating the training received by the practitioner to the rest of the health team is not established either. This may be a breastfeeding awareness event, as well as perhaps a non-formal training that should replicate the knowledge acquired. Studies carried out by Molina [12] and Feldman et al., [16] show that professionals with training in breastfeeding issues and who carry out promotional activities in their workplaces, have more knowledge about this which improves patterns of practice and confidence in the management of breastfeeding.
There are no previous reports comparing the degree of knowledge of the different primary health care professionals such as those covered in this research. It is for this reason that when comparing the results obtained with others of similar characteristics, it should be taken into account that the participants of studies carried out in other countries such as those of Rodríguez et al., [13] Hurtado et al., and Molina [12], are professionals who belong to a level of specialized maternity care (secondary and tertiary level in Chile). Differences in the study population can influence the results because the professionals surveyed work at different levels of care and present different levels of knowledge and specialty in their disciplines.
The absence of international evidence at the primary health level regarding the issue, could be explained by the differences in the protocols of care in the children's program determined by the authority of each country, as well as the training of professionals involved in it. For example, in the case of Chile, the professional care of newborns up to the first month of life is performed by midwives, a professional that is not formed in all countries. In Chile, no studies have been found that measure knowledge in breastfeeding in health professionals, there are only publications that refer to training of professionals in this field, applying this measure as one of the interventions for the promotion, practice and increase of prevalence of breastfeeding [8]. For the above mentioned, this study stands out for being innovative when focusing on an unexplored group in this area of health care at the national level.
The results found could be useful to direct interventions and training to professionals who presented poor results, since for the first time, it is possible to identify those who stand out for their high level of knowledge (nutritionists and midwives) as well as those who have a lower level (nurses and doctors), the latter in accordance with what has been described by Hurtado et al. [11] and Molina [12] in identifying a low level of knowledge in these professionals.
Conclusion
In conclusion, the improvement in the training of all professionals in the management and promotion of breastfeeding requires the support not only of the health care management entities, in terms of the promotion and access to training, but also of the authorities in order to increase the resources allocated to these trainings, as well as the scientific societies and entities that train health professionals, in order to regulate the formal contents in breastfeeding topics with a transversal vision, focused both on undergraduate training and continuing training of health professionals.
At the local level, a training plan should be considered for all professionals who join the family health centers and consider continuing training as well. Maintaining breastfeeding standards updated and available to all professionals, and activate training and maintenance of the breastfeeding committees in each establishment must also be considered. In these committees participants should be representatives of the different professions and replicate the good practices in all health service centers. Educational interventions covering these professionals significantly increase their knowledge in this matter, therefore, increasing these interventions would allow to improve the prevalence of breastfeeding further improving our country's indices which, although already high, are not uniformly reflected in some sectors.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
From the authors
Thesis work to obtain the degree of Magister in Public Health in Universidad Mayor.
Ethical aspects
The Journal is aware that the Ethics Committee of the University of Development - Clínica Alemana, Santiago, Chile, was informed of and approved this study and its possible publication in a biomedical dissemination journal.
Conflicts of Interest
The authors completed the ICMJE conflict of interest declaration form, and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Financing
The authors state there were no external funding for the conduction of the study.

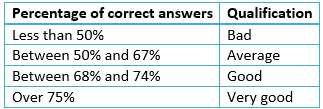 Table 1. Level of knowledge in breastfeeding according to survey.
Table 1. Level of knowledge in breastfeeding according to survey.

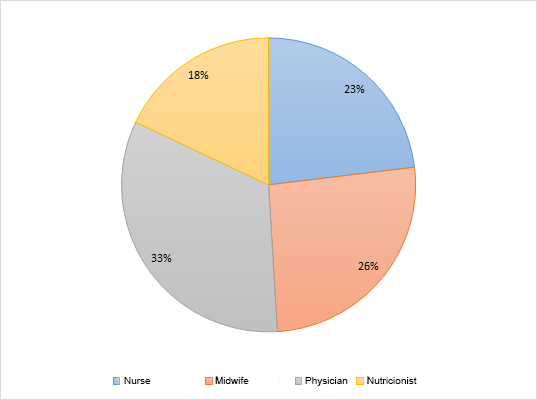 Figure 1. Percentage distribution of professionals surveyed.
Figure 1. Percentage distribution of professionals surveyed.

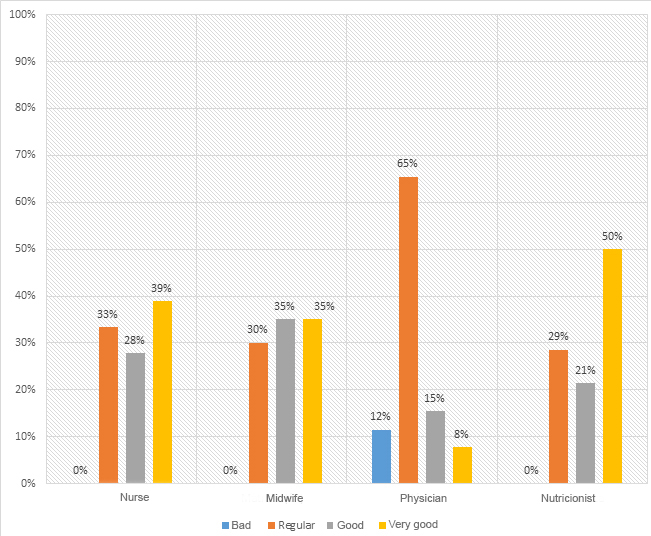 Figure 2. Percentage distribution of concept of qualification, according to profession.
Figure 2. Percentage distribution of concept of qualification, according to profession.

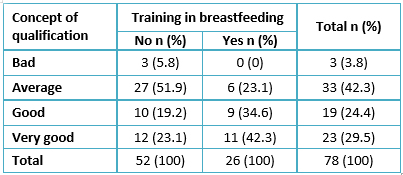 Table 2. Concept of qualification, according to training.
Table 2. Concept of qualification, according to training.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

INTRODUCCIÓN
El conocimiento sobre lactancia materna de profesionales de la salud ha sido asociado a diferencias en la práctica y prevalencia de lactancia materna exclusiva.
OBJETIVOS
Evaluar nivel de conocimientos sobre lactancia materna en los profesionales que participan del control de salud del niño en los centros de salud familiar de la comuna de Maipú (matrona o matrón, médico, enfermera o enfermero, nutricionista); y determinar si existe asociación entre el nivel de conocimientos, la profesión y el estado de capacitación en lactancia materna en el momento de la encuesta.
MÉTODOS
Estudio de tipo cuantitativo, transversal y analítico. Los participantes fueron profesionales de salud que regularmente son parte del control de niño sano hasta el sexto mes de vida. Se aplicó una encuesta basada en los “Diez pasos para una lactancia materna exitosa”. El análisis descriptivo consideró frecuencias, porcentajes y medidas de tendencia central, así como la asociación entre nivel de conocimiento, profesión y estado de capacitación.
RESULTADOS
De un total de 78 participantes, 42,2% logró un concepto de calificación “regular”, sólo el 3,8% obtuvo el concepto “malo” y más del 50% de los profesionales obtuvieron calificación “bueno” y “muy bueno”. Los profesionales que obtuvieron mejor calificación por sus conocimientos en lactancia materna fueron nutricionistas con 50% de “muy bueno”, seguido por enfermeras(os) y matronas(es) con 39% y 35% respectivamente. Por otra parte, el 65,4% de los médicos obtuvo calificación “regular” y sólo un 7,7% “muy bueno”. Del total de los profesionales, sólo el 33% contaba con capacitación en lactancia materna (histórico) y 6,4% recibió capacitación en este tema durante el último año, destacando que el 34,6 y 42,3% de aquellos que obtuvieron conceptos “bueno” y “muy bueno” corresponden a profesionales capacitados. Se encontró asociación estadísticamente significativa entre el nivel de conocimiento en lactancia materna, profesión (p=0,019) y presencia de capacitación (p=0,033).
CONCLUSIONES
Los profesionales de salud presentan distintos niveles de conocimientos en lactancia materna. Las capacitaciones en esta temática incrementan significativamente los conocimientos, lo que podría mejorar la prevalencia en lactancia materna.
 Authors:
Laura Medel Marambio [1 ], Dafna Benadof [1,2 ], Carol Toro Huerta [1 ]
Authors:
Laura Medel Marambio [1 ], Dafna Benadof [1,2 ], Carol Toro Huerta [1 ]
Affiliation:
[1] Escuela de Salud Pública, Universidad Mayor, Santiago, Chile
[2] Facultad de Odontología, Universidad Andrés Bello, Santiago, Chile
E-mail: dafna.benadof@unab.cl
Author address:
[1] Echaurren 237
Santiago
Región Metropolitana
Chile

Citation: Medel Marambio L , Benadof D , Toro Huerta C . Breastfeeding knowledge of health professionals working in municipal healthcare centers in Maipu. Medwave 2017 Abr;17(2):e6891 doi: 10.5867/medwave.2017.03.6891
Submission date: 28/11/2016
Acceptance date: 22/2/2017
Publication date: 6/4/2017
Origin: no solicitado
Type of review: reviewed by four external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Ministerio de Salud, Manual de Lactancia Materna: Contenidos técnicos para profesionales de la salud, Chile. 2010. | Link |
- Oddy WH. The impact of breastmilk on infant and child health. Breastfeed Rev. 2002 Nov;10(3):5-18. | PubMed |
- Burgess A, Glasauer P. Guía de nutrición de la familia. Roma, FAO 2006:69-77. | Link |
- Organización Mundial de la Salud. Estrategia Mundial para la alimentación del lactante y pequeño. Ginebra. OMS/UNICEF; 2003. | Link |
- Declaración de Innocenti: sobre la protección, Promoción y Apoyo de la Lactancia Materna. OMS - UNICEF. Florencia , Agosto. 1990. [on line] | Link |
- Atalah E. Current status of breastfeeding in Chile. Medwave 2006 Jun;6(5):e3528 | Link |
- Datos estadísticos del Servicio de Salud Metropolitano Central. Julio de 2014.
- Ossandón M, llabaca J, Gajardo C, Castillo N, Namur L. Fomento de la lactancia materna, programa Iniciativa Hospital Amigo del Niño y la Madre, en Hospital Barros Luco Trudeau. Rev Chil Pediatr. 2000;71(2):98-106. | CrossRef |
- World Health Organizatipn. Breastfeeding counselling: A training course. Trainer’s Guide. 1993. who.int [on line]. | Link |
- Organización Mundial de la Salud. La Alimentación del lactante y del niño pequeño: Capítulo Modelo para libros de textos dirigidos a estudiantes de medicina y otras carreras de la salud. OMS; 2010. | Link |
- Hurtado VJG, Aguilar TE, Ochoa LAA, Moreno SGA, Álvarez HG. Saberes de médicos y enfermeras de un hospital, acerca de las bondades de la lactancia. Rev Mex Pediatr. 2014;81(2):56-60. | Link |
- Molina T. Informe sobre conocimiento de los residentes de pediatría en el manejo de la lactancia materna. Asociación Española de Pediatría. Ann Pediatría, 2003;58(3):263-267. | Link |
- Rodríguez F, Borace R, López A. Conocimientos, actitudes y prácticas del personal multidisplinario de salud y la promoción realizada a las madres con respecto a la lactancia materna en dos maternidades. Panamá: Instituto conmemorativo Gorgas de estudios de la salud; 2006: [on line] | Link |
- IBM Corp. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp.;2012. | Link |
- Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database Syst Rev. 2007 Jan 24;(1):CD001141. | CrossRef | PubMed |
- Feldman-Winter L, Barone L, Milcarek B, Hunter K, Meek J, Morton J, et al. Residency curriculum improves breastfeeding care. Pediatrics. 2010 Aug;126(2):289-97. | CrossRef | PubMed |
 Ministerio de Salud, Manual de Lactancia Materna: Contenidos técnicos para profesionales de la salud, Chile. 2010. | Link |
Ministerio de Salud, Manual de Lactancia Materna: Contenidos técnicos para profesionales de la salud, Chile. 2010. | Link | Oddy WH. The impact of breastmilk on infant and child health. Breastfeed Rev. 2002 Nov;10(3):5-18. | PubMed |
Oddy WH. The impact of breastmilk on infant and child health. Breastfeed Rev. 2002 Nov;10(3):5-18. | PubMed | Organización Mundial de la Salud. Estrategia Mundial para la alimentación del lactante y pequeño. Ginebra. OMS/UNICEF; 2003. | Link |
Organización Mundial de la Salud. Estrategia Mundial para la alimentación del lactante y pequeño. Ginebra. OMS/UNICEF; 2003. | Link | Declaración de Innocenti: sobre la protección, Promoción y Apoyo de la Lactancia Materna. OMS - UNICEF. Florencia , Agosto. 1990. [on line] | Link |
Declaración de Innocenti: sobre la protección, Promoción y Apoyo de la Lactancia Materna. OMS - UNICEF. Florencia , Agosto. 1990. [on line] | Link | Datos estadísticos del Servicio de Salud Metropolitano Central. Julio de 2014.
Datos estadísticos del Servicio de Salud Metropolitano Central. Julio de 2014.  Ossandón M, llabaca J, Gajardo C, Castillo N, Namur L. Fomento de la lactancia materna, programa Iniciativa Hospital Amigo del Niño y la Madre, en Hospital Barros Luco Trudeau. Rev Chil Pediatr. 2000;71(2):98-106. | CrossRef |
Ossandón M, llabaca J, Gajardo C, Castillo N, Namur L. Fomento de la lactancia materna, programa Iniciativa Hospital Amigo del Niño y la Madre, en Hospital Barros Luco Trudeau. Rev Chil Pediatr. 2000;71(2):98-106. | CrossRef | World Health Organizatipn. Breastfeeding counselling: A training course. Trainer’s Guide. 1993. who.int [on line]. | Link |
World Health Organizatipn. Breastfeeding counselling: A training course. Trainer’s Guide. 1993. who.int [on line]. | Link | Organización Mundial de la Salud. La Alimentación del lactante y del niño pequeño: Capítulo Modelo para libros de textos dirigidos a estudiantes de medicina y otras carreras de la salud. OMS; 2010. | Link |
Organización Mundial de la Salud. La Alimentación del lactante y del niño pequeño: Capítulo Modelo para libros de textos dirigidos a estudiantes de medicina y otras carreras de la salud. OMS; 2010. | Link | Hurtado VJG, Aguilar TE, Ochoa LAA, Moreno SGA, Álvarez HG. Saberes de médicos y enfermeras de un hospital, acerca de las bondades de la lactancia. Rev Mex Pediatr. 2014;81(2):56-60. | Link |
Hurtado VJG, Aguilar TE, Ochoa LAA, Moreno SGA, Álvarez HG. Saberes de médicos y enfermeras de un hospital, acerca de las bondades de la lactancia. Rev Mex Pediatr. 2014;81(2):56-60. | Link | Molina T. Informe sobre conocimiento de los residentes de pediatría en el manejo de la lactancia materna. Asociación Española de Pediatría. Ann Pediatría, 2003;58(3):263-267. | Link |
Molina T. Informe sobre conocimiento de los residentes de pediatría en el manejo de la lactancia materna. Asociación Española de Pediatría. Ann Pediatría, 2003;58(3):263-267. | Link | Rodríguez F, Borace R, López A. Conocimientos, actitudes y prácticas del personal multidisplinario de salud y la promoción realizada a las madres con respecto a la lactancia materna en dos maternidades. Panamá: Instituto conmemorativo Gorgas de estudios de la salud; 2006: [on line] | Link |
Rodríguez F, Borace R, López A. Conocimientos, actitudes y prácticas del personal multidisplinario de salud y la promoción realizada a las madres con respecto a la lactancia materna en dos maternidades. Panamá: Instituto conmemorativo Gorgas de estudios de la salud; 2006: [on line] | Link |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








