Key Words: infant mortality, very low birth weight infant, child nutrition sciences, neonatology, Peru
Abstract
OBJECTIVES
To determine the actual nutritional intake of very low birth weight infants and their growth outcome during the first month of life. Additionally, we identified factors that account for a negative neonatal outcome in this population.
METHODS
A case-series study was conducted in a tertiary hospital in Lima, Peru between 2011 and 2012 and the data was obtained from medical records. No feeding protocol was used during this study. Daily fluids, energy and protein intakes were documented and weekly weight z-scores were calculated. A logistic regression analysis was used to identify factors for an adverse outcome, defined as neonatal mortality or extra-uterine growth restriction, during the first 28 days of life.
RESULTS
After applying selection criteria, 76 participants were included. The nutritional intakes were similar to standard values seen in the literature, but protein intakes were suboptimal in all of the four weeks. Birth weight z-score was associated with an adverse outcome (p=0.035). It was determined that having a birth weight z-score under -1.09 predicted a negative outcome with an area under the curve of 96.8% [93.5%, 100%] with a 95% confidence interval.
CONCLUSION
Protein intakes are widely deficient in the population of this study. Nevertheless, an adverse outcome during the neonatal period is more associated with a poor birth weight z-score than nutrition-related factors.
Introduction
Adequate nutrition is essential for optimum growth in very low birth weight infants. Despite recent research in this area, extra-uterine growth restriction presents an ongoing challenge [1] due to immature gut motility and the subsequent risk of necrotizing enterocolitis with “aggressive” feeding [2]. Inadequate nutrition leads to poor growth [3],[4] in the short term and impaired neurological development [5],[6] in the long term. Studies have also shown that very low birth weight infants are likely to develop hypertension, insulin resistance and diminished glucose tolerance by adulthood [7] and may never reach adult growth as compared with their non-very low birth weight peers [8].
In contrast, adequate nutrition has been associated with lower rates of death and short-term morbidity, without increasing the incidence of necrotizing enterocolitis [9]. The Cochrane Collaboration found that the risk of necrotizing enterocolitis in very low birth weight infants is not affected by delaying the introduction of progressive enteral feeds, nor by delaying advancement of feeds or the use of early trophic feedings [10],[11],[12]. As to long term complications, it has been recently proposed that nutrition acts as a protective factor via the microbiome-gut-brain axis, which may explain why suboptimal nutrition may affect neurodevelopment negatively [13].
Very low birth weight nutrition management is being practiced heterogeneously at distinct neonatal intensive care units [14]. Several reports have been made regarding nutritional intakes and growth outcome, [3],[4],[15],[16],[17],[18],[19] but more evidence is needed to come to any management conclusions [19]. Thus, we will try to explore this area, by describing and evaluating the current nutritional management, and its associated growth outcomes, in a resource-limited setting.
Methods
Ethics statement
Ethical approval for this protocol was obtained from the ethics committee at Universidad Peruana Cayetano Heredia in Lima, Peru.
Design
This is a retrospective cohort done in the neonatal intensive care unit of Hospital Nacional Cayetano Heredia in Lima, Peru. No standardized nutrition protocol for very low birth weight infants had been implemented at the time of the study. Inclusion criteria: Infants born during the years 2011 and 2012 with a birth weight of 1500 grams or less. Exclusion criteria: Length of stay in the hospital less than seven days; lack of weight information on the days 7, 14, 21 or 28 (+/-1 day) and participants without available medical records.
Study variables
In January 2013 medical records for participants meeting selection criteria were reviewed. For those who met the criteria we reviewed hospital course and measurements data including sex, gestational age, weight, enteral feedings, fluids, energy and proteins for the first 28 days or until discharge. The nutrient content of maternal milk was assumed to have 0.9 g / 100ml and 67 kcal / 100ml, which is consistent with literature values [20]. The formula used for premature babies contained 24 cal/oz.
Weight was recorded in grams and collected at days 0, 7, 14, 21 and 28. If weight from that day was not found, the weight from +/-1 day was used. All weights were then converted into Fenton and Kim 2013 weight z-scores [21]. This helped define intrauterine growth restriction as a weight z-score at birth ≤ -2, and extra-uterine growth restriction as weight z-score of ≤ -2 at 28 days of life. For those patients that were discharged before 28 days of life, their discharge weight z-score was used. The outcome evaluates mortality or extra-uterine growth restriction.
The day in which the participant started enteral feedings was documented, as well as the day in which their enteral nutrition reached 50% and 100% of their total nutrition. Parenteral and enteral intakes of volume, energy and proteins were collected daily for each participant. The day the participant starts enteral feedings is defined as the day the participant tolerates oral feeds, even though most of the participant’s feedings might still be parenteral nutrition.
Comorbidities were tabulated for necrotizing enterocolitis, sepsis and mechanical ventilation. Necrotizing enterocolitis was defined as a Bell stage of 2 or above with clinical and radiological findings [22]. A sepsis diagnosis was made clinically but confirmed microbiologically, to be included in the analysis. Mechanical ventilation is considered if the patient required assisted breathing.
R version 3.0.2 was used for statistical analysis. Graphics were created using the package of ggplot2 for R as well as the pROC package. Box plot graphs were created to visually evaluate nutritional intakes and weight z-scores during the first 28 days of life. One box plot was graphed per week.
A multivariable logistic model was used to evaluate our final outcome (mortality or extra-uterine growth restriction). The variables in the model included: birth weight z-score, protein and calories in the first week of life, the day enteral feeds started, and the presence of necrotizing enterocolitis, sepsis and mechanical ventilation. Nutritional intakes in the other weeks of life did not affect the outcome, thus were not included in the model. A significance level less than 0.05 was used in our statistical tests.
We used our models to predict, within a 95% confidence interval (CI), and to evaluate the area under the curve. Youden Index, sensitivity and specificity were calculated using the package Optimal Cutpoints version 1.1-3 in R.
Results
We had 115 very low birth weight infants born in 2011 and 2012 with an incidence of 10.9 and 15.2 per every 1,000 births, respectively. From this total, 39 were excluded: 28 due to hospital length of stay less than 1 week, 2 for lacking weight information and 9 because of unavailable medical records. Thus, 76 participants were included in this study. It should be mentioned that 75% of participants with less than a week of stay were extremely low birth weight.
This study consisted of 52.6% of males, with a median birth weight of 1290 grams (range: 560-1500g) and median gestational age of 32 weeks (range: 24-36 weeks). Intra uterine growth restriction was seen in 23.7% of participants. By the twenty-eighth day of life, 9 participants were discharged and 6 had died. Extra-uterine growth restriction was presented in 63.2% of participants. From those who died during the study, half were extremely low birth weight with the most common cause of death being septic shock in 50% of participants. In addition, 6.6% of the study participants experienced necrotizing enterocolitis, 23.7% had sepsis, and 42.1% required mechanical ventilation. From those with necrotizing enterocolitis, all were Bell Stage III with diagnosis as early as day 3 and as late as day 13 (median day 5). None had intra uterine growth restriction and only one presented extra-uterine growth restriction. Necrotizing enterocolitis itself did not appear to cause an effect on producing extra-uterine growth restriction or death.
All infants started their feeding with parenteral nutrition, while enteral nutrition began in the first couple of days. Parenteral nutrition was given until the infant received 100 ml/kg/day enterally. Concerning nutritional intakes, daily fluids, energy and protein of the first week of life can be seen in (Table 1) and weekly averages are shown in (Figure 1.) Proteins (p=0.18) and calories (p=0.46) intake in the first week of life were not significant in relation to an adverse outcome, as defined earlier. Protein intakes during this study were always below 3.5 g/kg/day. Regarding enteral feedings, these started with a median of 2 days (range: 1 to 12 days) and achieved 100% by a median of 11 days (range: 5 to 28 days). However, 23.7% of participants regressed after achieving full enteral nutrition.
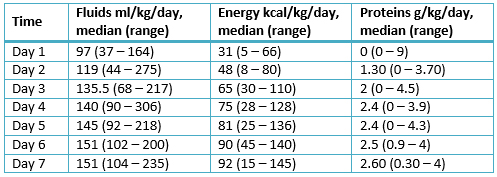
Table 1: First week nutritional intakes
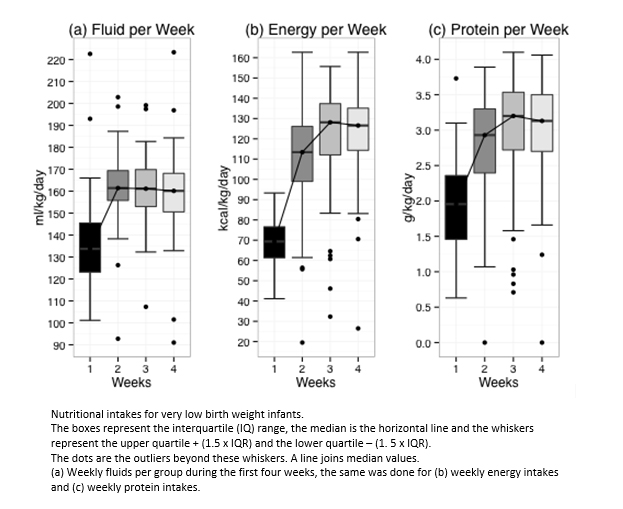
Figure 1: Weekly nutritional intakes
In relation to the weight z-scores, their medians were always negative, starting with a birth weight z-score of -1.43 (range: -4.41 to 1.00) and reaching minimum of -2.48 (range: -4.66 to -0.98) at 28 days of life, as shown in (Figure 2). Birth weight z-score was the factor most strongly associated with neonatal death or extra-uterine growth restriction (p=0.035) during their first 28 days of life. This was the only variable that showed statistical significance in our analysis (Table 2).
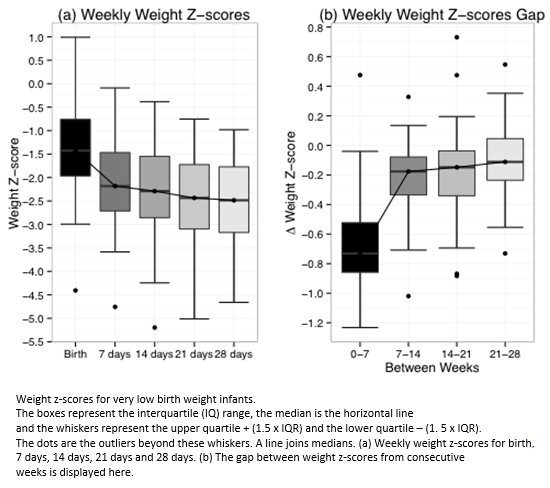
Figure 2: Weight Z – Scores
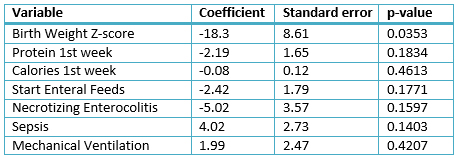
Table 2: Logistic multivariable regression for a negative outcome at 28 days
Multivariable logistic regression analysis demonstrates that the probability of a negative outcome dramatically increases as a birth weight z-score falls below -1.09 (Figure 3). When evaluating birth weight z-score alone and outcome. As mentioned before, a negative outcome is considered as death or extra-uterine growth restriction in the first 28 days of life. Its appropriate receiver operating characteristic (ROC), we find an area under the curve of 96.8% [93.5%, 100%]. This provides a sensitivity of 96% [79.64%, 99.99%] and specificity of 90% [78.59%, 96.74%] with -1.09 as the cutoff, with a Youden Index of 0.862 (Figure 4).
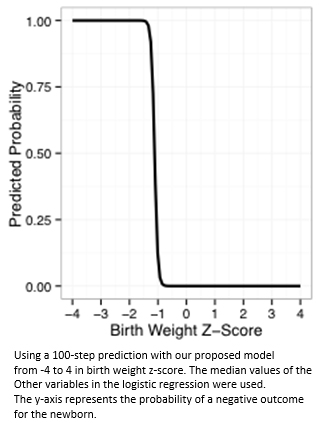
Figure 3: Logistic model prediction of birth weight z- Score
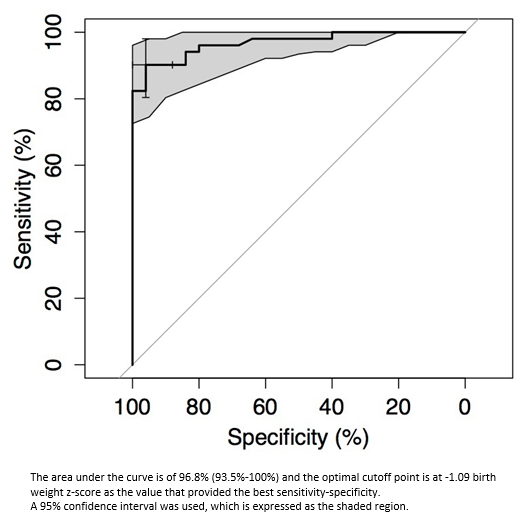
Figure 4: ROC Curve
Discussion
When comparing our nutritional intakes with the literature [23],[24],[25],[26],[27] fluids and energy intakes almost met the established values, however protein intakes were suboptimal in all four weeks. Despite having no feeding regimen and subpar protein intakes. However, nutritional intakes were not as important as birth weight z-score for predicting a negative outcome (death or extra-uterine growth restriction). Moreover, the sensitivity and specificity obtained show that having a z-score below -1.09 at birth is a good predictor for neonatal death or extra-uterine growth restriction during their first month.
Some limitations of this study include that data was obtained retrospectively, and this study was not able to obtain information regarding crown-heel length or head circumference. This study focuses on the neonatal outcomes during their first 28 days of life, however some outcomes from this early period are not seen until later in life. In contrast, this study benefits from the availability of having daily nutritional intake information for every participant. Another important strength is the fact that no feeding protocol was established, at the time of the study, thus the study group reflects a “naïve” population. Additionally, as it has already been stated, this publication represents the first report regarding nutritional intakes in very low birth weight infants from Peru.
Regarding nutritional intakes, our findings are similar to those found two decades ago in a study conducted in the USA [15] and to a study conducted a decade ago in Argentina [3]. Our data is worrisome since deficient protein intakes during the first week of life are associated with poor neurological outcomes at 18 months [6]. Furthermore, our population shows birth weight z-scores lower than those reported in other neonatal intensive care units [17],[28],[29]. In agreement with previous reports, we found that birth weight z-scores were the most important risk factor for adverse growth outcomes. Specifically, poor birth weight is the best predictor for mortality in a limited medical setting [30].
In Latin America poor prenatal control compliance, low socioeconomic status, unplanned pregnancy and subpar nutritional status have been previously associated with low birth weight [31],[32]. This is reflected with our poor birth weight z-scores which is very distinct from what has been published elsewhere [17],[28]. We hope this will help clinicians understand the clinical risk that lies on these patients. Moreover, we also hope that policymakers from low- and middle-income countries (LMIC) focus on maternal nutrition, if we ever hope to improve the negative neonatal outcome we face day to day.
Conclusion
Future studies should design interventions to improve birth weight with the hopes of reducing neonatal mortality and extra-uterine growth restriction. Multicenter studies should be done in low- and middle-income countries to confirm if birth weight z-score is even a better indicator for a negative outcome than birth weight per se. We found that birth weight z-score has a bigger weigh regarding an unfavorable outcome by 28 days, than nutritional intakes. Finally, we emphasize that improving maternal health and nutritional status should improve a neonate’s health status at birth and thus produce better overall outcomes.
Notes
From the editor
The authors originally submitted this article in Spanish and subsequently translated it into English. The Journal has not copyedited this version.
Ethical aspects
The Journal has evidence that the research protocol which originates this article, had the approval of the Institutional Research Ethics Committee of the Universidad Peruana Cayetano Heredia, Lima, Peru.
Conflicts of interests
The authors completed the ICMJE conflict of interest declaration form and declare not having received funding for the preparation of this report, not having any financial relationships with organizations that could have interests in the published article in the last three years, and not having other relations or activities that might influence the article´s content. Forms can be requested to the responsible author or the editorial direction of the Journal.
Financing
The authors declare that the study was self-financed by the authors and no money was received from external sources.
Acknowledgements
The authors greatly appreciate the comments provided by Doctor Ekhard Ziegler, Doctor Robert H. Gilman, Doctor Chris Meinzen. Doctor Diego Proaño, Jose Carlos Tapia, Enrico Medina, Neil Beaton, Michael Rogers, Lionel Jensen and Eloy F. Ruiz while proofreading this manuscript.
 Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.
Esta obra de Medwave está bajo una licencia Creative Commons Atribución-NoComercial 3.0 Unported. Esta licencia permite el uso, distribución y reproducción del artículo en cualquier medio, siempre y cuando se otorgue el crédito correspondiente al autor del artículo y al medio en que se publica, en este caso, Medwave.

OBJETIVOS
Determinar las ingestas nutricionales en los recién nacidos de muy bajo peso al nacer y su respectivo crecimiento en el primer mes de vida. Adicionalmente, identificar factores para un desenlace negativo en el periodo neonatal de esta población.
METODOS
Estudio de serie de casos desarrollado en un hospital de tercer nivel en Lima, Perú desde 2011 a 2012. La información se obtuvo de las historias médicas. No se utilizó un protocolo de nutrición durante el estudio. La ingesta diaria del volumen, la energía y las proteínas fue registrada al igual que el puntaje z del peso de manera semanal. Se utilizó regresión logística para identificar factores asociados a un desenlace adverso, que se define como mortalidad neonatal o restricción de crecimiento extrauterino en los primeros 28 días de vida.
RESULTADOS
Luego del criterio de selección, se incluyeron a 76 participantes. Las ingestas nutricionales fueron similares a los valores descritos en la literatura, pero la ingesta proteica fue sub óptima durante las cuatro semanas. El puntaje z del peso al nacer se asocia con un desenlace adverso (p=0,035). Se determinó que un puntaje z menor de 1,09 predice un desenlace negativo con un área bajo la curva ROC de 96,8% (93,5%, 100%), con un intervalo de confianza del 95%.
CONCLUSIÓN
Las ingestas proteicas fueron sumamente deficientes en este estudio. Sin embargo, un desenlace adverso se asocia más a un pobre puntaje z al nacer que a factores relacionados a la nutrición.
 Authors:
Álvaro Proaño[1], Romina Elena Aragón[1], Fabiola Rivera[2], Jaime Zegarra[1,2,3]
Authors:
Álvaro Proaño[1], Romina Elena Aragón[1], Fabiola Rivera[2], Jaime Zegarra[1,2,3]
Affiliation:
[1] Facultad de Medicina Alberto Hurtado, Universidad Peruana Cayetano Heredia, Lima, Perú
[2] Unidad de Neonatología, Clínica San Felipe, Lima, Perú
[3] Unidad de Cuidados Intensivos Neonatología, Hospital Nacional Cayetano Heredia, Lima, Perú
E-mail: alvaro.proano.f@upch.pe
Author address:
[1] Avenida El Polo 740
Edificio C
Oficina 313
Santiago de Surco
Lima
Peru

Citation: Proaño , Aragón RE, Rivera F, Zegarra J. Nutritional intake and weight z-scores in very low birth weight infants in Peru. Medwave 2016 Mar;16(2):e6414 doi: 10.5867/medwave.2016.02.6414
Submission date: 17/12/2015
Acceptance date: 15/3/2016
Publication date: 29/3/2016
Origin: not requested
Type of review: reviewed by two external peer reviewers, double-blind

Comments (0)
We are pleased to have your comment on one of our articles. Your comment will be published as soon as it is posted. However, Medwave reserves the right to remove it later if the editors consider your comment to be: offensive in some sense, irrelevant, trivial, contains grammatical mistakes, contains political harangues, appears to be advertising, contains data from a particular person or suggests the need for changes in practice in terms of diagnostic, preventive or therapeutic interventions, if that evidence has not previously been published in a peer-reviewed journal.
No comments on this article.
To comment please log in
 Medwave provides HTML and PDF download counts as well as other harvested interaction metrics.
Medwave provides HTML and PDF download counts as well as other harvested interaction metrics. There may be a 48-hour delay for most recent metrics to be posted.

- Corpeleijn WE, Vermeulen MJ, van den Akker CH, van Goudoever JB. Feeding very-low-birth-weight infants: our aspirations versus the reality in practice. Ann Nutr Metab. 2011;58 Suppl 1:20-9. | CrossRef | PubMed |
- Bozzetti V, Tagliabue PE, Visser GH, van Bel F, Gazzolo D. Feeding issues in IUGR preterm infants. Early Hum Dev. 2013 Oct;89 Suppl 2:S21-3. | CrossRef | PubMed |
- Dinerstein A, Nieto RM, Solana CL, Perez GP, Otheguy LE, Larguia AM. Early and aggressive nutritional strategy (parenteral and enteral) decreases postnatal growth failure in very low birth weight infants. J Perinatol. 2006 Jul;26(7):436-42. | PubMed |
- Roggero P, Giannì ML, Orsi A, Amato O, Piemontese P, Liotto N, et al. Implementation of nutritional strategies decreases postnatal growth restriction in preterm infants. PLoS One. 2012;7(12):e51166. | CrossRef | PubMed |
- Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006 Apr;117(4):1253-61. | PubMed |
- Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009 May;123(5):1337-43. | CrossRef | PubMed |
- Eichenwald EC, Stark AR. Management and outcomes of very low birth weight. N Engl J Med. 2008 Apr 17;358(16):1700-11. | CrossRef | PubMed |
- Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E. Growth of very low birth weight infants to age 20 years. Pediatrics. 2003 Jul;112(1 Pt 1):e30-8. | PubMed |
- Ehrenkranz RA, Das A, Wrage LA, Poindexter BB, Higgins RD, Stoll BJ, et al. Early nutrition mediates the influence of severity of illness on extremely LBW infants. Pediatr Res. 2011 Jun;69(6):522-9. | CrossRef | PubMed |
- Morgan J, Bombell S, McGuire W. Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants. Cochrane Database Syst Rev. 2013 Mar 28;3:CD000504. | CrossRef | PubMed |
- Morgan J, Young L, McGuire W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2014;12:CD001970. | CrossRef | PubMed |
- Morgan J, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2013 Mar 28;3:CD001241. | CrossRef | PubMed |
- Keunen K, van Elburg RM, van Bel F, Benders MJ. Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatr Res. 2015 Jan;77(1-2):148-55. | CrossRef | PubMed |
- Dutta S, Singh B, Chessell L, Wilson J, Janes M, McDonald K, et al. Guidelines for feeding very low birth weight infants. Nutrients. 2015 Jan 8;7(1):423-42. | CrossRef | PubMed |
- Carlson SJ, Ziegler EE. Nutrient intakes and growth of very low birth weight infants. J Perinatol. 1998 Jul-Aug;18(4):252-8. | PubMed |
- Embleton NE, Pang N, Cooke RJ. Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics. 2001 Feb;107(2):270-3. | PubMed |
- Cormack BE, Bloomfield FH. Audit of feeding practices in babies<1200 g or 30 weeks gestation during the first month of life. J Paediatr Child Health. 2006 Jul-Aug;42(7-8):458-63. | PubMed |
- Grover A, Khashu M, Mukherjee A, Kairamkonda V. Iatrogenic malnutrition in neonatal intensive care units: urgent need to modify practice. JPEN J Parenter Enteral Nutr. 2008 Mar-Apr;32(2):140-4. | CrossRef | PubMed |
- Maas C, Poets CF, Franz AR. Avoiding postnatal undernutrition of VLBW infants during neonatal intensive care: evidence and personal view in the absence of evidence. Arch Dis Child Fetal Neonatal Ed. 2015 Jan;100(1):F76-81. | CrossRef | PubMed |
- Jenness R. The composition of human milk. Semin Perinatol. 1979 Jul;3(3):225-39. | PubMed |
- Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013 Apr 20;13:59. | CrossRef | PubMed |
- Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978 Jan;187(1):1-7. | PubMed |
- Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. 1. Guidelines on Paediatric Parenteral Nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), Supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005 Nov;41 Suppl 2:S1-87. | PubMed |
- Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010 Jan;50(1):85-91. | CrossRef | PubMed |
- Bolisetty S, Osborn D, Sinn J, Lui K; Australasian Neonatal Parenteral Nutrition Consensus Group. Standardised neonatal parenteral nutrition formulations - an Australasian group consensus 2012. BMC Pediatr. 2014 Feb 18;14:48. | CrossRef | PubMed |
- Embleton ND, Simmer K. Practice of parenteral nutrition in VLBW and ELBW infants. World Rev Nutr Diet. 2014;110:177-89. | CrossRef | PubMed |
- Koletzko B, Poindexter B, Uauy R. Recommended nutrient intake levels for stable, fully enterally fed very low birth weight infants. World Rev Nutr Diet. 2014;110:297-9. | CrossRef | PubMed |
- Krauel Vidal X, Figueras Aloy J, Natal Pujol A, Iglesias Platas I, Moro Serrano M, Fernández Pérez C, Martín-Ancel A. [Reduced postnatal growth in very low birth weight newborns with GE < or = 32 weeks in Spain]. An Pediatr (Barc). 2008 Mar;68(3):206-12. | PubMed |
- Graziano PD, Tauber KA, Cummings J, Graffunder E, Horgan MJ. Prevention of postnatal growth restriction by the implementation of an evidence-based premature infant feeding bundle. J Perinatol. 2015 Aug;35(8):642-9. | CrossRef | PubMed |
- Gooden M, Younger N, Trotman H. What is the best predictor of mortality in a very low birth weight infant population with a high mortality rate in a medical setting with limited resources? Am J Perinatol. 2014 Jun;31(6):441-6. | CrossRef | PubMed |
- Figueroa ML, Llosa L, Alvarez JO. [The nutritional and health status of the Latin American woman]. Arch Latinoam Nutr. 1988 Sep;38(3):705-22. | PubMed |
- Ticona-Rendón M, Pacora-Portella P, Huanco-Apaza D, Ticona-Vildoso M. [Intrauterine growth retardation in Peru: stressors and perinatal outcomes Hospital Ministry of Health]. Ginecol Obstet Mex. 2014 Nov;82(11):725-36. | PubMed |
 Corpeleijn WE, Vermeulen MJ, van den Akker CH, van Goudoever JB. Feeding very-low-birth-weight infants: our aspirations versus the reality in practice. Ann Nutr Metab. 2011;58 Suppl 1:20-9.
| CrossRef | PubMed |
Corpeleijn WE, Vermeulen MJ, van den Akker CH, van Goudoever JB. Feeding very-low-birth-weight infants: our aspirations versus the reality in practice. Ann Nutr Metab. 2011;58 Suppl 1:20-9.
| CrossRef | PubMed | Bozzetti V, Tagliabue PE, Visser GH, van Bel F, Gazzolo D. Feeding issues in IUGR preterm infants. Early Hum Dev. 2013 Oct;89 Suppl 2:S21-3. | CrossRef | PubMed |
Bozzetti V, Tagliabue PE, Visser GH, van Bel F, Gazzolo D. Feeding issues in IUGR preterm infants. Early Hum Dev. 2013 Oct;89 Suppl 2:S21-3. | CrossRef | PubMed | Dinerstein A, Nieto RM, Solana CL, Perez GP, Otheguy LE, Larguia AM. Early and aggressive nutritional strategy (parenteral and enteral) decreases postnatal growth failure in very low birth weight infants. J Perinatol. 2006 Jul;26(7):436-42. | PubMed |
Dinerstein A, Nieto RM, Solana CL, Perez GP, Otheguy LE, Larguia AM. Early and aggressive nutritional strategy (parenteral and enteral) decreases postnatal growth failure in very low birth weight infants. J Perinatol. 2006 Jul;26(7):436-42. | PubMed | Roggero P, Giannì ML, Orsi A, Amato O, Piemontese P, Liotto N, et al. Implementation of nutritional strategies decreases postnatal growth restriction in preterm infants. PLoS One. 2012;7(12):e51166. | CrossRef | PubMed |
Roggero P, Giannì ML, Orsi A, Amato O, Piemontese P, Liotto N, et al. Implementation of nutritional strategies decreases postnatal growth restriction in preterm infants. PLoS One. 2012;7(12):e51166. | CrossRef | PubMed | Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006 Apr;117(4):1253-61. | PubMed |
Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006 Apr;117(4):1253-61. | PubMed | Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009 May;123(5):1337-43. | CrossRef | PubMed |
Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009 May;123(5):1337-43. | CrossRef | PubMed | Eichenwald EC, Stark AR. Management and outcomes of very low birth weight. N Engl J Med. 2008 Apr 17;358(16):1700-11. | CrossRef | PubMed |
Eichenwald EC, Stark AR. Management and outcomes of very low birth weight. N Engl J Med. 2008 Apr 17;358(16):1700-11. | CrossRef | PubMed | Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E. Growth of very low birth weight infants to age 20 years. Pediatrics. 2003 Jul;112(1 Pt 1):e30-8.
| PubMed |
Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, Borawski E. Growth of very low birth weight infants to age 20 years. Pediatrics. 2003 Jul;112(1 Pt 1):e30-8.
| PubMed | Ehrenkranz RA, Das A, Wrage LA, Poindexter BB, Higgins RD, Stoll BJ, et al. Early nutrition mediates the influence of severity of illness on extremely LBW infants. Pediatr Res. 2011 Jun;69(6):522-9. | CrossRef | PubMed |
Ehrenkranz RA, Das A, Wrage LA, Poindexter BB, Higgins RD, Stoll BJ, et al. Early nutrition mediates the influence of severity of illness on extremely LBW infants. Pediatr Res. 2011 Jun;69(6):522-9. | CrossRef | PubMed | Morgan J, Bombell S, McGuire W. Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants. Cochrane Database Syst Rev. 2013 Mar 28;3:CD000504. | CrossRef | PubMed |
Morgan J, Bombell S, McGuire W. Early trophic feeding versus enteral fasting for very preterm or very low birth weight infants. Cochrane Database Syst Rev. 2013 Mar 28;3:CD000504. | CrossRef | PubMed | Morgan J, Young L, McGuire W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2014;12:CD001970. | CrossRef | PubMed |
Morgan J, Young L, McGuire W. Delayed introduction of progressive enteral feeds to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2014;12:CD001970. | CrossRef | PubMed | Morgan J, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2013 Mar 28;3:CD001241. | CrossRef | PubMed |
Morgan J, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2013 Mar 28;3:CD001241. | CrossRef | PubMed | Keunen K, van Elburg RM, van Bel F, Benders MJ. Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatr Res. 2015 Jan;77(1-2):148-55. | CrossRef | PubMed |
Keunen K, van Elburg RM, van Bel F, Benders MJ. Impact of nutrition on brain development and its neuroprotective implications following preterm birth. Pediatr Res. 2015 Jan;77(1-2):148-55. | CrossRef | PubMed | Dutta S, Singh B, Chessell L, Wilson J, Janes M, McDonald K, et al. Guidelines for feeding very low birth weight infants. Nutrients. 2015 Jan 8;7(1):423-42. | CrossRef | PubMed |
Dutta S, Singh B, Chessell L, Wilson J, Janes M, McDonald K, et al. Guidelines for feeding very low birth weight infants. Nutrients. 2015 Jan 8;7(1):423-42. | CrossRef | PubMed | Carlson SJ, Ziegler EE. Nutrient intakes and growth of very low birth weight infants. J Perinatol. 1998 Jul-Aug;18(4):252-8. | PubMed |
Carlson SJ, Ziegler EE. Nutrient intakes and growth of very low birth weight infants. J Perinatol. 1998 Jul-Aug;18(4):252-8. | PubMed | Embleton NE, Pang N, Cooke RJ. Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics. 2001 Feb;107(2):270-3. | PubMed |
Embleton NE, Pang N, Cooke RJ. Postnatal malnutrition and growth retardation: an inevitable consequence of current recommendations in preterm infants? Pediatrics. 2001 Feb;107(2):270-3. | PubMed | Cormack BE, Bloomfield FH. Audit of feeding practices in babies<1200 g or 30 weeks gestation during the first month of life. J Paediatr Child Health. 2006 Jul-Aug;42(7-8):458-63. | PubMed |
Cormack BE, Bloomfield FH. Audit of feeding practices in babies<1200 g or 30 weeks gestation during the first month of life. J Paediatr Child Health. 2006 Jul-Aug;42(7-8):458-63. | PubMed | Grover A, Khashu M, Mukherjee A, Kairamkonda V. Iatrogenic malnutrition in neonatal intensive care units: urgent need to modify practice. JPEN J Parenter Enteral Nutr. 2008 Mar-Apr;32(2):140-4. | CrossRef | PubMed |
Grover A, Khashu M, Mukherjee A, Kairamkonda V. Iatrogenic malnutrition in neonatal intensive care units: urgent need to modify practice. JPEN J Parenter Enteral Nutr. 2008 Mar-Apr;32(2):140-4. | CrossRef | PubMed | Maas C, Poets CF, Franz AR. Avoiding postnatal undernutrition of VLBW infants during neonatal intensive care: evidence and personal view in the absence of evidence. Arch Dis Child Fetal Neonatal Ed. 2015 Jan;100(1):F76-81. | CrossRef | PubMed |
Maas C, Poets CF, Franz AR. Avoiding postnatal undernutrition of VLBW infants during neonatal intensive care: evidence and personal view in the absence of evidence. Arch Dis Child Fetal Neonatal Ed. 2015 Jan;100(1):F76-81. | CrossRef | PubMed | Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013 Apr 20;13:59.
| CrossRef | PubMed |
Fenton TR, Kim JH. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013 Apr 20;13:59.
| CrossRef | PubMed | Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978 Jan;187(1):1-7. | PubMed |
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978 Jan;187(1):1-7. | PubMed | Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. 1. Guidelines on Paediatric Parenteral Nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), Supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005 Nov;41 Suppl 2:S1-87. | PubMed |
Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R. 1. Guidelines on Paediatric Parenteral Nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), Supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005 Nov;41 Suppl 2:S1-87. | PubMed | Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010 Jan;50(1):85-91. | CrossRef | PubMed |
Agostoni C, Buonocore G, Carnielli VP, De Curtis M, Darmaun D, Decsi T, et al. Enteral nutrient supply for preterm infants: commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2010 Jan;50(1):85-91. | CrossRef | PubMed | Bolisetty S, Osborn D, Sinn J, Lui K; Australasian Neonatal Parenteral Nutrition Consensus Group. Standardised neonatal parenteral nutrition formulations - an Australasian group consensus 2012. BMC Pediatr. 2014 Feb 18;14:48.
| CrossRef | PubMed |
Bolisetty S, Osborn D, Sinn J, Lui K; Australasian Neonatal Parenteral Nutrition Consensus Group. Standardised neonatal parenteral nutrition formulations - an Australasian group consensus 2012. BMC Pediatr. 2014 Feb 18;14:48.
| CrossRef | PubMed | Embleton ND, Simmer K. Practice of parenteral nutrition in VLBW and ELBW infants. World Rev Nutr Diet. 2014;110:177-89. | CrossRef | PubMed |
Embleton ND, Simmer K. Practice of parenteral nutrition in VLBW and ELBW infants. World Rev Nutr Diet. 2014;110:177-89. | CrossRef | PubMed | Koletzko B, Poindexter B, Uauy R. Recommended nutrient intake levels for stable, fully enterally fed very low birth weight infants. World Rev Nutr Diet. 2014;110:297-9. | CrossRef | PubMed |
Koletzko B, Poindexter B, Uauy R. Recommended nutrient intake levels for stable, fully enterally fed very low birth weight infants. World Rev Nutr Diet. 2014;110:297-9. | CrossRef | PubMed | Krauel Vidal X, Figueras Aloy J, Natal Pujol A, Iglesias Platas I, Moro Serrano M, Fernández Pérez C, Martín-Ancel A. [Reduced postnatal growth in very low birth weight newborns with GE < or = 32 weeks in Spain]. An Pediatr (Barc). 2008 Mar;68(3):206-12.
| PubMed |
Krauel Vidal X, Figueras Aloy J, Natal Pujol A, Iglesias Platas I, Moro Serrano M, Fernández Pérez C, Martín-Ancel A. [Reduced postnatal growth in very low birth weight newborns with GE < or = 32 weeks in Spain]. An Pediatr (Barc). 2008 Mar;68(3):206-12.
| PubMed | Graziano PD, Tauber KA, Cummings J, Graffunder E, Horgan MJ. Prevention of postnatal growth restriction by the implementation of an evidence-based premature infant feeding bundle. J Perinatol. 2015 Aug;35(8):642-9. | CrossRef | PubMed |
Graziano PD, Tauber KA, Cummings J, Graffunder E, Horgan MJ. Prevention of postnatal growth restriction by the implementation of an evidence-based premature infant feeding bundle. J Perinatol. 2015 Aug;35(8):642-9. | CrossRef | PubMed | Gooden M, Younger N, Trotman H. What is the best predictor of mortality in a very low birth weight infant population with a high mortality rate in a medical setting with limited resources? Am J Perinatol. 2014 Jun;31(6):441-6. | CrossRef | PubMed |
Gooden M, Younger N, Trotman H. What is the best predictor of mortality in a very low birth weight infant population with a high mortality rate in a medical setting with limited resources? Am J Perinatol. 2014 Jun;31(6):441-6. | CrossRef | PubMed | Figueroa ML, Llosa L, Alvarez JO. [The nutritional and health status of the Latin American woman]. Arch Latinoam Nutr. 1988 Sep;38(3):705-22. | PubMed |
Figueroa ML, Llosa L, Alvarez JO. [The nutritional and health status of the Latin American woman]. Arch Latinoam Nutr. 1988 Sep;38(3):705-22. | PubMed | Ticona-Rendón M, Pacora-Portella P, Huanco-Apaza D, Ticona-Vildoso M. [Intrauterine growth retardation in Peru: stressors and perinatal outcomes Hospital Ministry of Health]. Ginecol Obstet Mex. 2014 Nov;82(11):725-36. | PubMed |
Ticona-Rendón M, Pacora-Portella P, Huanco-Apaza D, Ticona-Vildoso M. [Intrauterine growth retardation in Peru: stressors and perinatal outcomes Hospital Ministry of Health]. Ginecol Obstet Mex. 2014 Nov;82(11):725-36. | PubMed |Systematization of initiatives in sexual and reproductive health about good practices criteria in response to the COVID-19 pandemic in primary health care in Chile
Clinical, psychological, social, and family characterization of suicidal behavior in Chilean adolescents: a multiple correspondence analysis








